Pregnancy Diagnosis: Signs, Differential Diagnosis, and Confirmatory Tests
Comprehensive nursing notes for accurate pregnancy diagnosis
Table of Contents
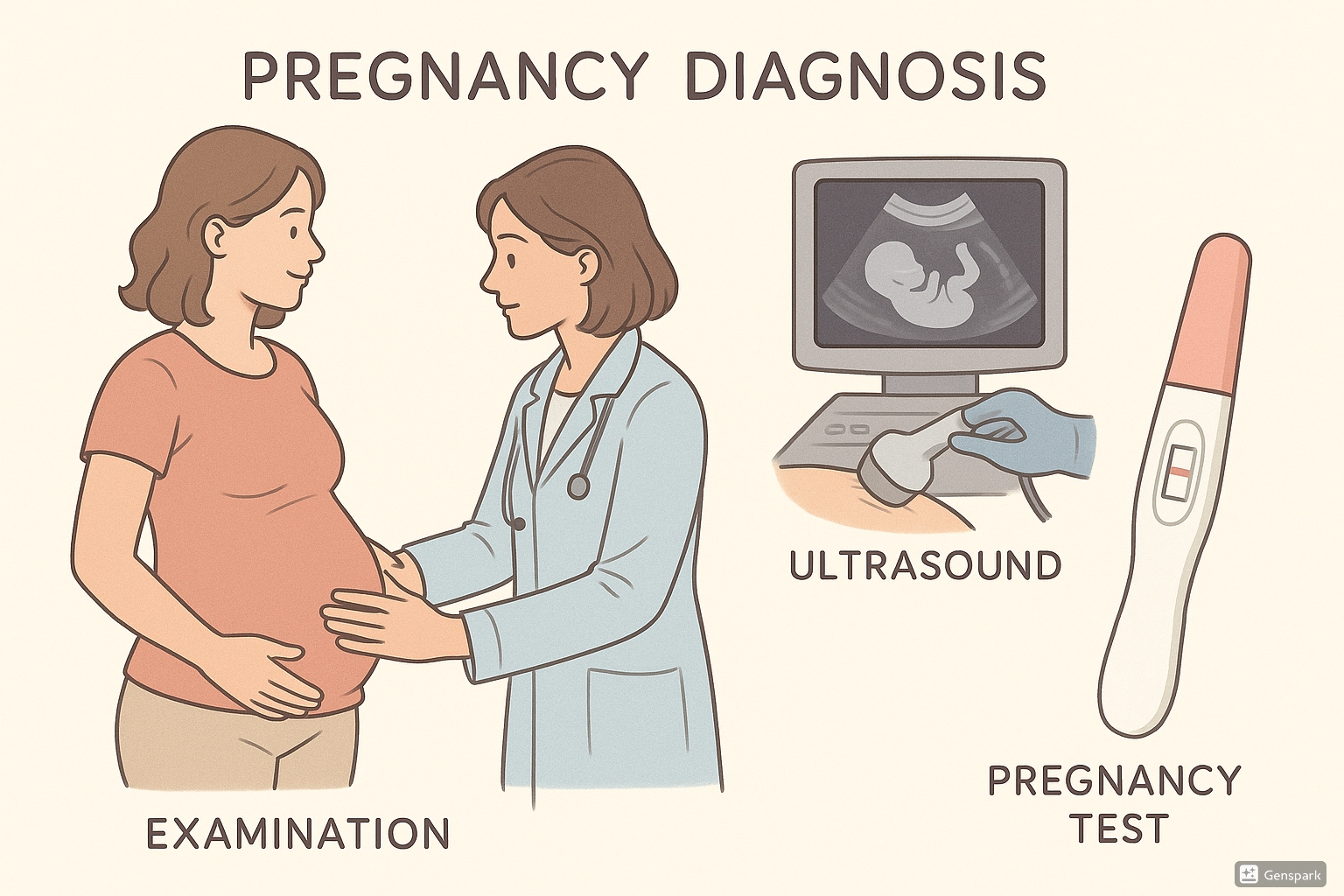
Fig. 1: Overview of pregnancy diagnosis methods including clinical examination, diagnostic tests and ultrasound confirmation
1. Introduction to Pregnancy Diagnosis
1.1 Definition & Importance
Pregnancy diagnosis is the process of confirming that conception has occurred and that a woman is carrying a developing embryo or fetus. Accurate and timely pregnancy diagnosis forms the cornerstone of obstetric care and is essential for appropriate prenatal management, ensuring optimal outcomes for both mother and baby.
Clinical Significance:
- Early pregnancy diagnosis allows for timely initiation of prenatal care
- Enables early detection of complications such as ectopic pregnancy or gestational trophoblastic disease
- Facilitates accurate dating of the pregnancy, which is crucial for monitoring fetal growth and development
- Allows women to make informed decisions about their pregnancy
1.2 Diagnostic Approach
The approach to pregnancy diagnosis involves assessing a combination of signs and symptoms that range from less reliable (presumptive) to absolutely definitive (positive) indicators. Healthcare providers typically follow a systematic approach when confirming pregnancy.
Classification of Pregnancy Signs
Presumptive Signs
Least reliable
Subjective & objective symptoms
Probable Signs
More reliable
Observable anatomical changes
Positive Signs
Definitive confirmation
Direct evidence of fetus
2. Presumptive Signs of Pregnancy
Presumptive signs are the least reliable indicators of pregnancy diagnosis. They are considered subjective as they can often be attributed to conditions other than pregnancy. These signs typically appear during the first 8-12 weeks of gestation.
2.1 Subjective Symptoms
| Symptom | Description | Onset | Notes for Nursing Assessment |
|---|---|---|---|
| Amenorrhea | Absence of menstruation | After conception | Document LMP (Last Menstrual Period); can be caused by stress, hormonal imbalances, excessive exercise |
| Nausea and vomiting | “Morning sickness” (can occur any time of day) | 2-8 weeks | Assess severity, hydration status; can be caused by gastrointestinal disorders |
| Breast changes | Tenderness, tingling, heaviness | 3-4 weeks | Can be premenstrual symptoms or due to hormonal contraception |
| Fatigue | Unusual tiredness | 1-12 weeks | Nonspecific; many medical conditions cause fatigue |
| Urinary frequency | Increased urination | 2-8 weeks | Rule out UTI; can be caused by diabetes, diuretics |
| Food aversions/cravings | Changes in food preferences | 4-8 weeks | Highly subjective; varies greatly among women |
2.2 Objective Symptoms
Observable Changes
- Skin pigmentation changes (linea nigra, chloasma)
- Spider angiomas
- Striae gravidarum (stretch marks)
- Weight gain
Physiological Changes
- Increased basal body temperature
- Slight blood pressure changes
- Melasma (the “mask of pregnancy”)
- Palmar erythema
Important Nursing Consideration:
Presumptive signs alone are never sufficient for confirming a pregnancy diagnosis. They should prompt further investigation using more reliable tests and assessments.
Mnemonic: “PREGNANT” for Remembering Presumptive Signs
- P: Period stopped (amenorrhea)
- R: Restroom visits increase (urinary frequency)
- E: Enlargement and tenderness of breasts
- G: Gastric disturbances (nausea, vomiting)
- N: Nipples darken
- A: Appetite changes (cravings/aversions)
- N: Nausea (morning sickness)
- T: Tiredness (fatigue)
3. Probable Signs of Pregnancy
Probable signs provide stronger evidence of pregnancy than presumptive signs. These signs are objectively verified by the healthcare provider during examination. While highly suggestive of pregnancy, they still do not provide absolute confirmation for pregnancy diagnosis.
3.1 Anatomical Changes
| Sign | Description | Timing | Assessment Notes |
|---|---|---|---|
| Goodell’s Sign | Softening of the cervix | 4-6 weeks | Detected during vaginal examination; cervix feels softer than usual |
| Chadwick’s Sign | Bluish-purple discoloration of vagina and cervix | 6-8 weeks | Due to increased vascularity and venous congestion |
| Hegar’s Sign | Softening of the isthmus of uterus (lower uterine segment) | 6-8 weeks | Requires bimanual examination technique |
| Braxton Hicks contractions | Irregular, painless uterine contractions | After 1st trimester | Becomes more noticeable in 2nd and 3rd trimesters |
3.2 Palpable Changes
Uterine Changes During Early Pregnancy
8 Weeks
Size of a chicken egg
Barely palpable above symphysis pubis
12 Weeks
Size of a grapefruit
Palpable just above symphysis pubis
16 Weeks
Halfway to umbilicus
Distinct enlargement noticeable
- Ballottement: The technique where the fetus can be bounced away and felt to rebound when the uterus is tapped during examination (16-28 weeks)
- Uterine enlargement: Progressive growth of the uterus in a characteristic pattern
- Piskacek’s sign: Asymmetrical enlargement of the uterus due to implantation
- McDonald’s sign: Ease of flexing the body of the uterus against the cervix
Nursing Assessment Tip:
When documenting probable signs, always correlate findings with the woman’s reported last menstrual period (LMP) and any presumptive symptoms. Systematic pregnancy diagnosis requires comprehensive assessment across all categories of signs.
4. Positive Signs of Pregnancy
Positive signs offer definitive proof of pregnancy and are considered diagnostic. These signs provide direct evidence of the presence of a fetus and form the most reliable basis for pregnancy diagnosis.
4.1 Fetal Indicators
The Three Primary Positive Signs:
- Fetal heart tones: Detectable by Doppler ultrasound as early as 8-10 weeks, and by fetoscope at 18-20 weeks
- Fetal movements: Felt by examiner (not the mother) at around 18-20 weeks
- Visualization of the fetus: Through ultrasound imaging
| Positive Sign | Detection Method | Earliest Detection | Notes |
|---|---|---|---|
| Fetal heart activity | Transvaginal ultrasound | 5-6 weeks | Confirms viable pregnancy |
| Fetal heart tones | Doppler device | 8-10 weeks | 110-160 beats/minute |
| Fetal outline | Transabdominal ultrasound | 6-7 weeks | Can confirm location, number, and viability |
| Fetal movements (objective) | Examiner palpation | 18-20 weeks | Active fetal movement felt by examiner |
| Fetal parts | Leopold’s maneuvers | 22+ weeks | Systematic palpation to identify fetal position |
Timeline of Detectable Positive Signs
5-6 weeks
Fetal cardiac activity
8-10 weeks
Doppler heart tones
18-20 weeks
Objective fetal movement
22+ weeks
Palpable fetal parts
Mnemonic: “FETUS” for Positive Signs of Pregnancy
- F: Fetal heart tones (auscultated)
- E: Embryo/fetus visualized (ultrasound)
- T: Tactile fetal movements (felt by examiner)
- U: Ultrasound confirmation
- S: Skeletal parts of fetus (palpated)
5. Differential Diagnosis
Several conditions can mimic the signs and symptoms of pregnancy, creating diagnostic challenges for healthcare providers. Accurate pregnancy diagnosis requires careful consideration of these alternative explanations.
5.1 Conditions That Mimic Pregnancy
| Condition | Common Symptoms | Distinguishing Features |
|---|---|---|
| Pseudocyesis (False pregnancy) | Amenorrhea, abdominal enlargement, breast changes, nausea | No fetal heart tones, negative pregnancy tests, psychological factors often present |
| Ovarian tumors/cysts | Abdominal distension, pelvic pressure, menstrual irregularities | Usually unilateral enlargement, negative pregnancy tests |
| Uterine fibroids | Enlarged uterus, irregular uterine contour | Irregular uterine enlargement, no fetal heart tones |
| Hydatidiform mole | Amenorrhea, vaginal bleeding, exaggerated pregnancy symptoms | Extremely high hCG levels, characteristic “snowstorm” appearance on ultrasound |
| Menopause | Amenorrhea, mood changes, weight gain | Age-specific assessment, FSH levels elevated |
| Obesity with amenorrhea | Abdominal enlargement, missed periods | Negative pregnancy tests, hormonal evaluation |
5.2 Diagnostic Challenges
Clinical Scenarios Requiring Caution
- Irregular menstrual cycles
- Obesity (can make physical examination difficult)
- Hormonal contraceptive use (may mask usual signs)
- Perimenopausal women
- Multiple pregnancies (may have exaggerated signs)
Nursing Approach
- Obtain thorough health history
- Document chronological sequence of symptoms
- Use objective confirmatory tests
- Consider psychological factors
- Collaborate with healthcare team
Critical Consideration:
When symptoms suggest pregnancy but confirmatory tests are negative, further investigation is essential. Accurate pregnancy diagnosis may require multiple assessment methods and referral to specialists if diagnostic uncertainty persists.
6. Confirmatory Tests
Laboratory and imaging tests provide definitive confirmation of pregnancy and are essential components of modern pregnancy diagnosis. These tests have largely replaced the need to wait for positive signs to confirm pregnancy.
6.1 Hormonal Tests
Human Chorionic Gonadotropin (hCG):
This hormone is produced by the developing placenta shortly after implantation and is the basis for most pregnancy tests. hCG can be detected in urine or blood, with blood tests being more sensitive.
| Test Type | Earliest Detection | Accuracy | Considerations |
|---|---|---|---|
| Urine qualitative hCG | 12-14 days after conception | 97-99% with correct use |
|
| Serum qualitative hCG | 8-10 days after conception | >99% |
|
| Serum quantitative hCG (Beta hCG) | 8-10 days after conception | >99% |
|
hCG Levels in Normal Pregnancy
hCG levels rise rapidly during the first trimester, peak around 8-12 weeks, then decline and plateau for the remainder of pregnancy
6.2 Imaging Studies
Transvaginal Ultrasound
- Earliest detection: Gestational sac at 4-5 weeks
- Fetal pole: Visible by 5-6 weeks
- Cardiac activity: Detectable by 6 weeks
- Benefits: High resolution for early pregnancy, can detect ectopic pregnancy
- Limitations: More invasive, requires specialized training
Transabdominal Ultrasound
- Earliest detection: Gestational sac at 5-6 weeks
- Fetal pole: Visible by 6-7 weeks
- Cardiac activity: Detectable by 7-8 weeks
- Benefits: Non-invasive, provides overall view
- Limitations: Lower resolution for early pregnancy, affected by maternal habitus
First Trimester Ultrasound Information:
Beyond confirming pregnancy, early ultrasound provides critical information for pregnancy diagnosis and management:
- Confirmation of intrauterine pregnancy location
- Assessment of embryonic/fetal viability
- Accurate dating of the pregnancy
- Detection of multiple pregnancies
- Evaluation of maternal structures (ovaries, cervix)
- Screening for anomalies
7. Nursing Assessment & Care
Nurses play a crucial role in pregnancy diagnosis through systematic assessment, patient education, and coordination of care. A comprehensive nursing approach ensures accurate diagnosis and appropriate early pregnancy management.
Initial Assessment
- Comprehensive health history
- Menstrual history (LMP, cycle regularity)
- Sexual and contraceptive history
- Review of systems focused on presumptive signs
- Medical, surgical, and obstetric history
- Family history of genetic conditions
Physical Examination
- Vital signs with baseline weight
- General appearance assessment
- Breast examination for changes
- Abdominal assessment (inspection, auscultation, palpation)
- Pelvic examination (if indicated and qualified)
- Assessment for edema
Diagnostic Coordination
- Collection of urine for pregnancy testing
- Blood draw for serum testing
- Preparation for ultrasound procedures
- Documentation and reporting of results
- Referral coordination for prenatal care
- Follow-up planning
Mnemonic: “PREGNANT CARE” for Nursing Assessment
- P: Previous pregnancies and outcomes
- R: Risk factor identification
- E: Evaluate signs and symptoms
- G: Gather laboratory evidence
- N: Note psychological response
- A: Assess dating accuracy
- N: Nutritional status evaluation
- T: Test results communication
- C: Care coordination initiation
- A: Anticipatory guidance
- R: Resources and referrals
- E: Education about next steps
Patient Education Topics Following Pregnancy Diagnosis:
- Expected progression of pregnancy
- Normal vs. concerning symptoms
- Nutritional requirements
- Folic acid supplementation
- Lifestyle modifications (smoking, alcohol, caffeine)
- Prenatal care schedule
- Available prenatal testing options
- Warning signs requiring immediate attention
- Community resources and support
- Emotional and psychological adaptations
8. Global Best Practices
Around the world, various approaches to pregnancy diagnosis have been developed to address different healthcare contexts, cultural considerations, and resource availability. Learning from global best practices can enhance nursing care.
Point-of-Care Testing in Low-Resource Settings
Many developing countries have implemented community health worker programs that utilize rapid, low-cost pregnancy tests to bring pregnancy diagnosis services directly to remote communities. These programs typically:
- Train community health workers to perform and interpret basic tests
- Establish clear referral pathways for positive results
- Combine pregnancy testing with basic health education
- Use mobile technology to track and follow up with pregnant women
Midwifery-Led Care Models
Countries like the Netherlands, New Zealand, and Sweden utilize midwifery-led care models that emphasize:
- Early confirmation of pregnancy by trained midwives
- Continuity of care from pregnancy diagnosis through postnatal period
- Integration of physical and emotional assessment
- Risk stratification to determine appropriate care pathways
- Reduced medical interventions for low-risk pregnancies
- Strong emphasis on community-based care
Telemedicine for Rural Pregnancy Diagnosis
Australia, Canada, and parts of Scandinavia have pioneered telehealth approaches for remote pregnancy diagnosis and early prenatal care:
- Remote consultation with specialists after local confirmation of pregnancy
- Transmission of ultrasound images from remote clinics to central hospitals
- Digital recording and monitoring of early pregnancy symptoms
- Virtual support groups for newly diagnosed pregnant women
- Centralized electronic health records accessible across care settings
Cultural Sensitivity in Pregnancy Confirmation
Many healthcare systems are adapting their approaches to pregnancy diagnosis to respect cultural diversity:
- Involving family members in diagnosis discussions when culturally appropriate
- Providing language-appropriate educational materials
- Respecting traditional pregnancy diagnosis practices while ensuring medical accuracy
- Training healthcare providers in culturally competent communication
- Creating welcoming clinical environments for diverse populations
Implementation Considerations for Nursing Practice:
When adapting global best practices for pregnancy diagnosis, nurses should consider:
- Local resource availability and constraints
- Existing healthcare infrastructure and referral systems
- Cultural context and community preferences
- Evidence-based practices appropriate for the setting
- Sustainability and scalability of implemented approaches
