Minor Disorders of Newborn and Its Management
Comprehensive Nursing Care Guide for Neonatal Disorders
Table of Contents
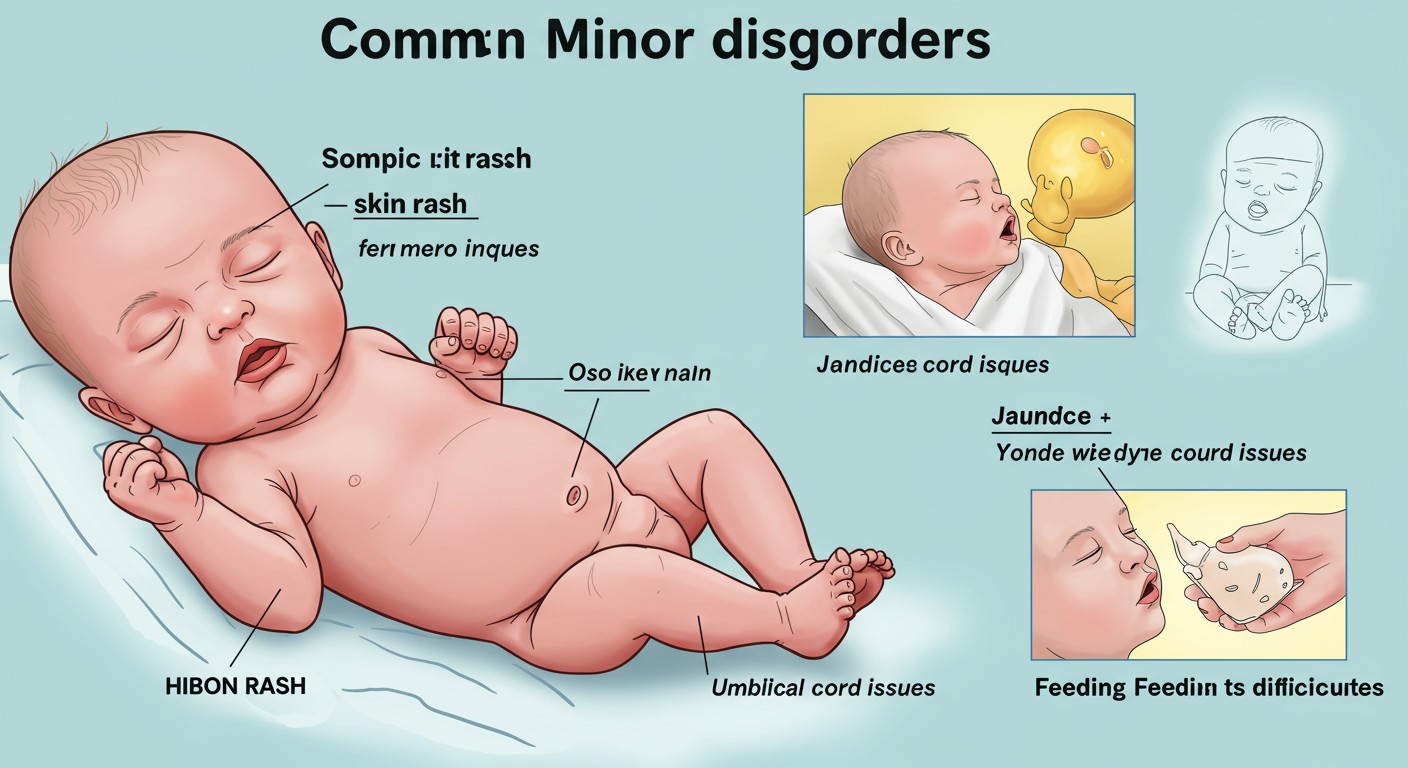
Introduction to Neonatal Disorders
The first 28 days of life, known as the neonatal period, is a critical time of adaptation for newborns. During this transition from intrauterine to extrauterine life, newborns may experience various minor disorders that require careful assessment and management. Understanding these common neonatal disorders is essential for nursing professionals to provide timely and appropriate care.
Most neonatal disorders are transient and self-limiting but require vigilant monitoring to prevent progression to more serious conditions. Early identification and proper management are crucial components of newborn care that directly impact long-term outcomes and family adjustment.
Key Concept:
While most minor disorders of newborns resolve spontaneously, proper nursing assessment and intervention can significantly reduce parental anxiety, prevent complications, and ensure optimal neonatal development.
Objectives of Neonatal Disorder Management
- Early identification of physiological and pathological conditions
- Implementation of prompt and appropriate nursing interventions
- Prevention of complications through vigilant monitoring
- Providing education and reassurance to parents/caregivers
- Promoting newborn comfort and optimal development
Physiological Jaundice
Physiological jaundice is one of the most common neonatal disorders, affecting approximately 60% of term newborns and 80% of preterm newborns. It results from elevated serum bilirubin levels manifesting as yellowish discoloration of the skin and sclera.
Etiology
- Increased RBC breakdown (neonate has higher RBC count)
- Immature liver function with limited conjugation ability
- Increased enterohepatic circulation of bilirubin
- Decreased gut motility delaying bilirubin excretion
Clinical Manifestations
- Yellow discoloration of skin and sclera
- Appears after 24 hours of life in term babies
- Progresses in cephalocaudal direction (head to toe)
- Usually peaks by day 3-5 of life
- Resolves within 7-10 days in term infants
Kramer’s Rule for Jaundice Assessment
Visual assessment of jaundice progression by body region
Assessment
| Assessment Parameter | Normal Findings | Concerning Findings |
|---|---|---|
| Onset | After 24 hours of life | Within first 24 hours (pathological) |
| Progression | Cephalocaudal (head to toe) | Rapid progression reaching extremities |
| Duration | Resolves within 7-10 days (term infants) | Persists beyond 2 weeks in term infants |
| Bilirubin levels | Peak typically < 12-15 mg/dL | Rising > 5 mg/dL in 24 hrs or > 20 mg/dL total |
| Behavior | Normal feeding and activity | Lethargy, poor feeding (sign of kernicterus) |
Management
Phototherapy
Primary treatment for moderate hyperbilirubinemia
- Converts bilirubin to water-soluble photoisomers
- Specific wavelength (blue-green spectrum, 460-490 nm)
- Requires full skin exposure except for eyes and genitalia
- Regular assessment of hydration status and body temperature
Supportive Care
- Promote frequent breastfeeding (8-12 times/day)
- Monitor weight, hydration, and urine output
- Avoid supplementing with water or dextrose water
- Serial bilirubin monitoring as per protocol
- Assess for signs of dehydration
JAUNDICE Mnemonic for Nursing Assessment
J – Jaundice progression (cephalocaudal)
A – Age at onset (after 24 hours is physiological)
U – Urination pattern (monitor output)
N – Nutrition status (feeding frequency)
D – Defecation (stool color and frequency)
I – Intensity of skin color (Kramer’s zones)
C – Clinical behavior (alertness, crying)
E – Evaluate risk factors (prematurity, ABO/Rh)
Nursing Considerations:
- Document the extent of jaundice using Kramer’s rule
- Position infant properly during phototherapy with eye protection
- Increase feeding frequency to promote meconium passage
- Monitor temperature every 2-4 hours during phototherapy
- Educate parents about the condition and its management
- Recognize the difference between physiological and pathological jaundice
Diaper Dermatitis
Diaper dermatitis, commonly known as diaper rash, is a common inflammatory condition affecting the skin in the diaper area. It’s one of the frequently encountered neonatal disorders that can cause discomfort and irritation.
Etiology
- Prolonged exposure to moisture (urine and feces)
- Skin maceration from occlusive diapers
- Chemical irritation from fecal enzymes
- Increased skin pH from ammonia in urine
- Secondary fungal infections (Candida albicans)
- Friction between diaper and skin
Clinical Manifestations
- Erythema and inflammation in diaper area
- Shiny, glazed appearance of affected skin
- Possible papules, vesicles, or scaling
- Candidal infection: satellite lesions beyond main rash
- Discomfort, irritability during diaper changes
Types of Diaper Dermatitis
1. Irritant Contact Dermatitis
Most common type, caused by friction and chemical irritation
• Appears on convex surfaces and skin folds
• Spares the folds in severe cases
2. Candidal Diaper Dermatitis
Caused by Candida albicans overgrowth
• Bright red, sharply demarcated
• Satellite papules and pustules
• Often involves skin folds
3. Seborrheic Diaper Dermatitis
Part of generalized seborrheic dermatitis
• Yellow, greasy scales
• Often seen with cradle cap
Management
| Management Strategy | Implementation | Rationale |
|---|---|---|
| Preventive Measures |
|
Reduces skin exposure to moisture and irritants |
| Barrier Products |
|
Creates protective barrier between skin and irritants |
| Candidal Infection |
|
Treats underlying fungal infection |
| Severe Dermatitis |
|
Reduces inflammation and promotes healing |
Nursing Considerations:
- Assess characteristics and extent of the rash during each diaper change
- Document appearance, location, and progression of rash
- Educate parents on proper diaper changing technique
- Advise against use of baby wipes containing alcohol or fragrance
- Demonstrate application of prescribed medications or barrier creams
- Teach parents to recognize signs of worsening or secondary infection
DIAPER Mnemonic for Prevention
D – Dry skin thoroughly after cleaning
I – Inspect skin regularly for early signs
A – Air exposure to promote healing
P – Protect with barrier creams
E – Eliminate irritants (gentle cleansers only)
R – Regular diaper changes (every 2-3 hours)
Oral Thrush
Oral thrush (oropharyngeal candidiasis) is a common fungal infection in newborns caused by Candida albicans. It’s one of the frequent neonatal disorders that requires proper identification and management to prevent complications and discomfort during feeding.
Etiology
- Overgrowth of Candida albicans (commensal fungus)
- Immature immune system in newborns
- Transmission during vaginal delivery
- Transmission from caregivers or contaminated objects
- Recent antibiotic therapy (alters oral flora)
Clinical Manifestations
- White, curd-like patches on oral mucosa, tongue, and gums
- Patches that cannot be easily wiped off
- Underlying erythematous base when patches are removed
- Feeding difficulties or refusal to feed
- Irritability during and after feeding
- Possible concurrent diaper dermatitis (candidal)
Distinguishing Oral Thrush from Milk Residue
Oral Thrush
Cannot be easily wiped off
Bleeding or redness when scraped
Appears on tongue, buccal mucosa, palate
Associated with feeding difficulties
Milk Residue
Easily wiped away
No underlying redness
Usually on tongue only
No feeding difficulties
Management
| Intervention | Administration | Nursing Considerations |
|---|---|---|
| Nystatin oral suspension |
|
|
| Miconazole oral gel |
|
|
| Gentian violet (1%) |
|
|
Nursing Considerations:
- Assess oral cavity before and after feeding to differentiate thrush from milk residue
- Demonstrate medication administration technique to parents/caregivers
- Advise treating mother’s nipples if breastfeeding (to prevent reinfection)
- Teach proper hygiene and sterilization of feeding equipment
- Monitor infant’s feeding patterns and weight gain
- Assess for concurrent diaper dermatitis which may indicate systemic candidiasis
Practice Point:
Always instruct parents to complete the full course of antifungal treatment even if thrush appears to have resolved. Premature discontinuation often leads to recurrence that may be more difficult to treat.
Umbilical Cord Issues
The umbilical cord is a critical structure that requires proper care and monitoring after birth. Various umbilical cord issues are common neonatal disorders that nurses must be able to identify and manage appropriately to prevent infections and complications.
Normal Umbilical Cord Changes
- Moist and white/blue at birth
- Begins drying within 24 hours of birth
- Turns black and dry as it mummifies
- Separates naturally within 7-14 days
- Small amount of clear/bloody discharge during separation is normal
Common Umbilical Issues
-
Omphalitis (umbilical infection)
- Erythema and swelling around cord
- Purulent or foul-smelling discharge
- Warmth around umbilical area
- Potential systemic symptoms (fever, lethargy)
-
Umbilical Granuloma
- Small, pink, moist tissue at base after cord separation
- Persistent clear/yellow discharge
- No surrounding erythema or tenderness
-
Umbilical Hernia
- Protrusion at umbilicus during crying or straining
- Usually reducible and painless
- Most resolve spontaneously by age 4-5 years
Umbilical Cord Care Timeline
Birth to Day 1
• Moist, white-blue appearance
• Contains Wharton’s jelly
• Initial cord clamp in place
Days 2-3
• Begins drying and shrinking
• Turns brownish-black
• Cord clamp removed (when dry)
Days 5-7
• Continues mummification process
• Dry, black appearance
• Base may become moist as separation begins
Days 7-14
• Cord separation occurs
• Small amount of discharge normal
• Umbilical area continues healing
Management of Umbilical Issues
| Condition | Management | Nursing Considerations |
|---|---|---|
| Normal Cord Care |
|
|
| Omphalitis |
|
|
| Umbilical Granuloma |
|
|
| Umbilical Hernia |
|
|
UMBILICAL Mnemonic for Cord Assessment
U – Unusual odor (sign of infection)
M – Moisture level (should progressively dry)
B – Bleeding (small amount normal during separation)
I – Inflammation of surrounding skin
L – Lack of progressive drying
I – Integrity of surrounding skin
C – Color changes (normal: white → black)
A – Appearance of base after separation
L – Length of time for healing
Umbilical Cord Care Best Practices:
- World Health Organization (WHO) recommends “dry cord care” in most settings
- Keep cord clean and dry
- Expose to air when possible
- No routine application of antiseptics
- In areas with high infection rates, chlorhexidine application may be recommended
- Avoid traditional substances (oils, herbs, animal dung)
- Sponge baths until cord falls off
- Fold diaper below cord to prevent urine contamination
- Teach parents signs of infection requiring medical attention
Feeding Difficulties
Feeding difficulties are common neonatal disorders that can significantly impact growth, development, and parent-infant bonding. Early identification and management of feeding problems are essential aspects of neonatal nursing care.
Common Feeding Issues in Newborns
-
Poor Latch (Breastfeeding)
- Difficulty attaching to breast
- Shallow latch causing nipple pain
- Clicking sounds during feeding
- Insufficient milk transfer
-
Ineffective Sucking
- Weak or disorganized suck
- Inability to maintain rhythmic sucking
- Fatigue during feeding
- Commonly seen in preterm or neurologically impaired infants
-
Regurgitation/Reflux
- Frequent spitting up after feeds
- May be accompanied by irritability
- Arching of back during/after feeding
- Usually physiologic but may be pathologic
-
Anatomical Issues
- Ankyloglossia (tongue-tie)
- Cleft lip/palate
- Micrognathia
Signs of Adequate Feeding in Newborns
Breastfeeding
Audible swallowing
Rhythmic sucking with pauses
Relaxed arms and hands
Breast softening during feed
Satisfied after feeding
Formula Feeding
Steady sucking pattern
Minimal air swallowing
Appropriate volume intake
Completes feeding in 20-30 min
Content after feeding
Output Indicators of Adequate Intake
Urine
- 6+ wet diapers daily after day 4
- Pale yellow color
Stool
- 3+ stools daily by day 4
- Yellow, seedy (breastfed)
- Yellow to tan (formula)
Assessment
| Assessment Parameter | Indicators of Concern | Assessment Techniques |
|---|---|---|
| Oral Structure |
|
|
| Feeding Behavior |
|
|
| Growth Parameters |
|
|
| Hydration Status |
|
|
Management Strategies
Breastfeeding Issues
Poor Latch
- Position infant with ear, shoulder, and hip in alignment
- Support breast in “C” hold, away from areola
- Wait for wide mouth opening before bringing baby to breast
- Ensure asymmetric latch with more areola visible above upper lip
- Break suction and reposition if painful
Low Milk Supply
- Increase frequency of breastfeeding (8-12 times/day)
- Ensure proper breast drainage with compression
- Consider supplementary nursing system if needed
- Pump after feeding to increase stimulation
- Assess for medical causes of low supply
Tongue-Tie
- Refer for evaluation by healthcare provider
- May require frenotomy if significantly affecting feeding
- Modify positioning to accommodate restricted tongue movement
Formula Feeding Issues
Bottle Refusal
- Try different nipple shapes or flow rates
- Ensure proper positioning (semi-upright)
- Warm formula to body temperature
- Try paced bottle feeding technique
- Feed when showing early hunger cues
Excessive Gas/Colic
- Burp frequently during and after feeds
- Consider anti-colic bottles
- Hold upright for 20-30 minutes after feeding
- Consider formula change if symptoms persist
- Rule out milk protein sensitivity
Reflux Management
- Smaller, more frequent feeds
- Upright positioning during and after feeds
- Avoid overfeeding
- Consider thickened formula if recommended
- Elevate head of crib/bassinet (if recommended)
Nursing Considerations for Feeding Difficulties:
- Assess every feeding in hospital setting
- Document intake, output, and feeding behaviors
- Provide consistent and evidence-based education to parents
- Recognize cultural practices related to infant feeding
- Refer to lactation consultant for breastfeeding issues
- Connect parents with community resources for ongoing support
- Provide emotional support to parents experiencing feeding challenges
- Follow up with at-risk infants after discharge
FEEDS Mnemonic for Feeding Assessment
F – Frequency and duration of feeding sessions
E – Engagement of infant during feeding
E – Elimination patterns (urine and stool)
D – Discomfort signs during or after feeding
S – Swallowing effectiveness and coordination
Erythema Toxicum Neonatorum
Erythema Toxicum Neonatorum (ETN) is one of the most common benign skin neonatal disorders, affecting approximately 30-70% of full-term newborns. This self-limiting condition requires proper identification to distinguish it from more serious skin disorders.
Etiology
- Exact cause remains unknown
- Theories include:
- Response to skin colonization by normal flora
- Immune system activation against hair follicles
- Transient inflammatory response during skin adaptation
- Histologically shows eosinophilic infiltration
- Not associated with any systemic illness
Clinical Manifestations
- Blotchy, erythematous macules and papules
- Small pustules with surrounding erythema (1-3 mm)
- Typically spares palms and soles
- Most common on trunk, face, extremities
- Appears within 24-72 hours after birth
- Lesions may come and go in different areas
- Resolves spontaneously within 5-7 days
- No associated systemic symptoms
Differential Diagnosis of Newborn Rashes
| Skin Condition | Appearance | Timing | Location |
|---|---|---|---|
| Erythema Toxicum | Yellow-white pustules with erythematous base | 24-72 hours after birth | Face, trunk, extremities (spares palms/soles) |
| Neonatal Acne | Red papules and pustules | 2-4 weeks of age | Face, especially cheeks and forehead |
| Miliaria (Heat Rash) | Small vesicles or papules | Any time | Skin folds, areas covered by clothing |
| Seborrheic Dermatitis | Greasy yellow scales | First 3 months | Scalp, face, behind ears, diaper area |
| Impetigo | Honey-colored crusted lesions | Any time | Face, extremities, areas with skin breakdown |
Note: Unlike more serious conditions, Erythema Toxicum is not associated with systemic symptoms and resolves spontaneously without treatment.
Assessment and Management
Assessment
- Document distribution and appearance of lesions
- Assess for systemic symptoms (should be none)
- Differentiate from other neonatal skin conditions
- Wright stain of pustule contents may show eosinophils (if performed)
- Monitor progression over time
Management
- No treatment required (self-limiting condition)
- Avoid topical medications or ointments on affected areas
- Gentle cleansing with water only
- Avoid harsh soaps or lotions
- Standard newborn skin care
Nursing Considerations:
- Primary role is parental education and reassurance
- Explain benign nature of the condition
- Emphasize that no treatment is necessary
- Teach proper skin care techniques
- Document appearance, distribution, and progression
- Reassure that condition will resolve without scarring
- Differentiate from conditions requiring medical intervention
Clinical Tip:
A simple bedside test can help differentiate Erythema Toxicum from more concerning rashes: If gently stroking the skin adjacent to a lesion produces additional lesions (positive Darier’s sign), further evaluation is needed as this suggests mastocytosis rather than ETN.
Milia
Milia are one of the most common benign skin neonatal disorders, appearing as small, white or yellow papules on a newborn’s face. They result from trapped keratin beneath the epidermis and require no treatment.
Etiology
- Retention of keratin within the dermis
- Trapped keratinized cells in pilosebaceous follicles
- Incomplete separation of epidermis during development
- Formation of tiny epidermal cysts
Clinical Manifestations
- Small (1-2 mm) white or yellowish papules
- Firm, pearly appearance
- Most commonly appear on:
- Nose
- Cheeks
- Chin
- Forehead
- May occasionally appear on upper trunk
- No surrounding erythema or inflammation
- Present at birth or develop in first few weeks
- Usually disappear spontaneously within 1-2 months
Types of Milia
Primary Milia
Most common form seen in newborns
Arise spontaneously from entrapped keratin
Typically resolve within weeks without treatment
No associated systemic conditions
Milia En Plaque
Rare variant not typically seen in newborns
Multiple lesions on an erythematous base
May require dermatology referral
Milia vs. Epstein Pearls
Milia
• On skin surface
• Face, especially nose
Epstein Pearls
• On oral mucosa
• Palate and gums
Both are keratin cysts and resolve spontaneously
Assessment and Management
| Assessment | Management | Parent Education |
|---|---|---|
|
|
|
Nursing Considerations:
- Focus on parental education and reassurance
- Address parental concerns about appearance
- Emphasize benign nature and self-resolving course
- Strongly discourage picking, squeezing, or applying treatments
- Teach standard newborn skin care practices
- Advise when to seek medical attention (signs of infection)
Important:
Parents should be strongly cautioned against attempting to express milia, as this can lead to skin damage, scarring, and potential infection. Reassure them that these lesions will resolve naturally without intervention.
Mongolian Spots
Mongolian spots (congenital dermal melanocytosis) are common benign birthmarks that present as blue-gray macules on the skin. These represent one of the most common pigmentary neonatal disorders, particularly in infants with darker skin tones.
Etiology
- Result from entrapment of melanocytes in the dermis
- Melanocytes fail to reach the epidermis during embryonic migration
- Genetic factors influence prevalence
- Higher prevalence in certain ethnicities:
- African (90-95%)
- Asian (80-90%)
- Hispanic (70-80%)
- Caucasian (1-10%)
Clinical Manifestations
- Blue-gray or blue-green macules or patches
- Non-blanching
- May vary in size from a few cm to covering large areas
- Most commonly found in:
- Sacral region (most common)
- Buttocks
- Lower back
- Shoulders
- Present at birth
- Usually fade gradually over years
- Most resolve by school age, but some may persist into adulthood
- No associated symptoms
Distinguishing Mongolian Spots from Bruising
Clinical Significance in Child Protection
Mongolian spots can be mistaken for bruising, potentially leading to unwarranted child abuse investigations. Careful documentation is essential for preventing such misunderstandings.
| Feature | Mongolian Spots | Bruises |
|---|---|---|
| Present at birth | Yes | No (except birth trauma) |
| Color change | Stable over weeks/months | Changes over days |
| Location | Sacrum, buttocks, shoulders | Variable, often on bony prominences |
| Borders | Diffuse, irregular | Often more defined |
| Tenderness | None | Often present |
| Texture | Same as surrounding skin | May be raised or swollen |
Assessment and Management
Assessment
- Document location, size, color, and appearance
- Photograph lesions (with parental consent)
- Include a measuring device for scale
- Maintain in medical record
- Distinguish from other skin lesions or bruising
- Assess for other birthmarks or skin findings
- Comprehensive skin assessment
Management
- No medical treatment required
- Maintain normal skin care
- Provide thorough documentation in medical record
- Provide a letter to parents describing the condition
- Consider referral if spots are:
- Unusually extensive
- In atypical locations (face, arms)
- Associated with other congenital anomalies
Nursing Considerations:
- Thorough documentation is essential for preventing misunderstandings about potential abuse
- Provide culturally sensitive education about the benign nature of these birthmarks
- Emphasize the natural resolution over time
- Provide a written description for parents to share with future healthcare providers
- Include information about Mongolian spots in discharge teaching
- Address any parental concerns about cosmetic appearance
Documentation Tip:
For effective documentation of Mongolian spots, use the “DESCRIBE” approach: Document size, color, region, irregular borders, birth-presence, expected resolution, and provide education to parents. This comprehensive documentation helps prevent misidentification as bruising in future healthcare encounters.
Cephalohematoma
Cephalohematoma is a common birth-related neonatal disorder characterized by a collection of blood between the periosteum and the skull bone. It’s important for nursing professionals to understand its characteristics, progression, and management to provide appropriate care and parental education.
Etiology
- Results from traumatic birth process
- Caused by rupture of blood vessels between skull bone and periosteum
- Risk factors include:
- Prolonged labor
- Vacuum-assisted delivery
- Forceps delivery
- Large fetal head circumference
- Primiparity
- Cephalopelvic disproportion
Clinical Manifestations
- Soft, fluctuant swelling on the scalp
- Does not cross suture lines (limited by periosteal attachment at sutures)
- Usually unilateral, commonly over parietal bone
- May not be apparent immediately at birth
- Often becomes more prominent in first few days
- No skin discoloration initially
- No tenderness on palpation
- Usually resolves within 2 weeks to 3 months
- Possible calcification with prolonged cases
Cephalohematoma vs. Caput Succedaneum
| Feature | Cephalohematoma | Caput Succedaneum |
|---|---|---|
| Definition | Blood between periosteum and skull bone | Edema of scalp tissue |
| Crosses suture lines | No | Yes |
| Onset | May appear hours after birth | Present immediately at birth |
| Duration | Weeks to months | Days (usually 3-7 days) |
| Consistency | Fluctuant, doesn’t pit on pressure | Soft, pits on pressure |
| Complications | Jaundice, infection (rare), calcification | Rarely any complications |
Cross-Section Comparison
Cephalohematoma
Blood confined within suture lines
Caput Succedaneum
Edema crossing suture lines
Assessment and Management
| Assessment | Management | Complications to Monitor |
|---|---|---|
|
|
|
Monitoring for Complications
Hyperbilirubinemia
- Monitor for jaundice as blood reabsorbs
- Serial bilirubin levels if jaundice present
- Encourage frequent feeding to promote excretion
- Assess for signs of dehydration
Infection
- Monitor for:
- Increased swelling
- Redness or warmth
- Fever
- Increased irritability
- Maintain scalp hygiene
- Avoid pressure on affected area
Nursing Considerations:
- Document birth history and risk factors
- Measure and document size of cephalohematoma
- Monitor for signs of increased intracranial pressure
- Position infant to avoid pressure on affected area
- Educate parents about:
- Normal resolution timeline (weeks to months)
- Possible temporary “bump” appearance as edges reabsorb first
- Signs of infection requiring medical attention
- Jaundice monitoring
- Provide reassurance about long-term outcomes
Warning:
Never attempt to aspirate or drain a cephalohematoma, as this introduces risk of infection and is not medically indicated. The body will naturally reabsorb the blood over time.
Caput Succedaneum
Caput succedaneum is a common, benign neonatal disorder characterized by diffuse swelling of the scalp due to pressure during delivery. Unlike cephalohematoma, it involves soft tissue edema rather than a collection of blood and typically resolves within days without intervention.
Etiology
- Results from pressure on fetal head during labor
- Occurs when head is pressed against cervix for extended periods
- Risk factors include:
- Prolonged labor
- Prolonged rupture of membranes
- Vacuum-assisted delivery
- Nulliparity
- Cephalopelvic disproportion
- Can occur with both vaginal and cesarean deliveries
Clinical Manifestations
- Soft, diffuse swelling of scalp tissue
- Crosses suture lines (key distinguishing feature)
- Present immediately at birth
- May have associated ecchymosis or purpura
- Pits on pressure (due to edematous nature)
- Usually resolves within 3-7 days
- Typically does not cause pain or discomfort
- No neurological symptoms
Key Characteristics of Caput Succedaneum
Anatomical Involvement
Caput succedaneum involves only the superficial tissues:
Skin
Subcutaneous tissue
Connective tissue (fascia)
Does not involve periosteum or bone
Distributional Pattern
Crosses suture lines
Diffuse swelling not confined by suture lines
Resolution Timeline
Typically resolves completely within one week
Assessment and Management
| Assessment | Management | Parent Education |
|---|---|---|
|
|
|
Nursing Considerations:
- Document characteristics of caput succedaneum in initial assessment
- Differentiate from other scalp conditions (cephalohematoma, subgaleal hemorrhage)
- Monitor resolution during hospital stay
- Provide anticipatory guidance to parents
- Address parental concerns about appearance
- Include in discharge teaching with expected timeline
- Teach parents normal newborn scalp care
- Advise when to seek medical attention (persistence beyond 7 days)
Clinical Pearl:
While caput succedaneum itself is benign, it can occasionally mask an underlying subgaleal hemorrhage, which is a medical emergency. Be alert for signs such as increasing head circumference, progressive scalp swelling extending beyond normal caput distribution, pallor, or signs of hypovolemic shock, which would warrant immediate medical attention.
Prevention and Best Practices
While many neonatal disorders are transient and benign, implementing evidence-based preventive strategies and best practices can significantly reduce their incidence and severity. Nursing professionals play a crucial role in educating parents and implementing these preventative measures.
PREVENT Mnemonic for Neonatal Disorders
P – Proper skin care with gentle cleansers
R – Regular feedings to prevent hyperbilirubinemia
E – Early identification and management
V – Vigilant monitoring of skin changes
E – Education of parents on normal variants
N – Nurture bonding despite cosmetic concerns
T – Thorough documentation of findings
Best Practices for Common Neonatal Disorders
| Disorder | Preventive Strategies | Global Best Practices |
|---|---|---|
| Physiological Jaundice |
|
