Rural Health Services in India
Organization, Staffing and Material Management
Table of Contents
Introduction to Rural Health Services in India
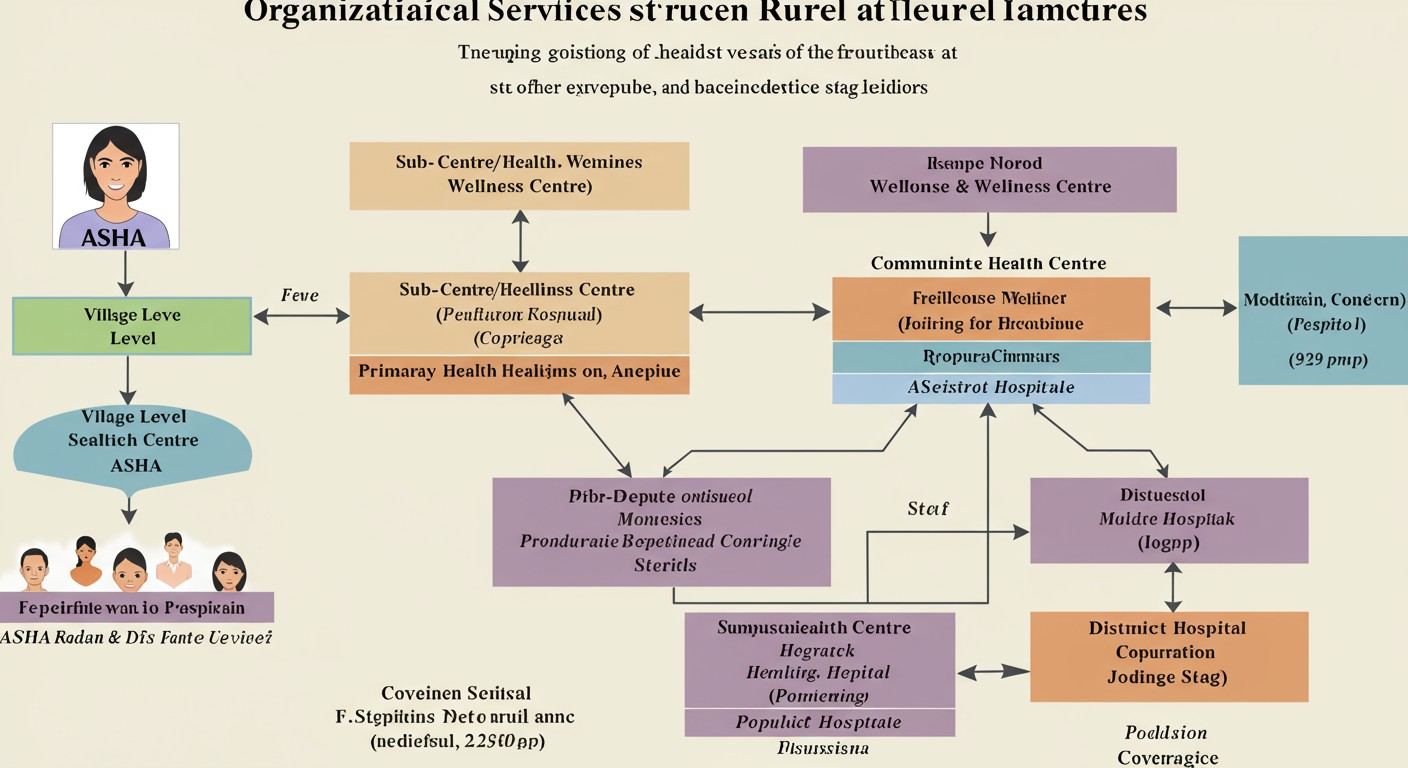
India’s rural health care system operates as a three-tier structure designed to provide accessible healthcare to the vast rural population. The system aims to bridge the gap between urban and rural healthcare by establishing a network of health facilities from village level to district hospitals.
The Rural Health Care System in India is designed based on population norms that vary between plain areas and hilly/tribal/difficult areas. The healthcare infrastructure is supported by various national health programs and initiatives like the National Health Mission (NHM), which aims to strengthen healthcare delivery at all levels.
Organizational Structure of Rural Health Services
The rural health infrastructure in India follows a hierarchical model with specific population coverage at each level:
| Health Facility Level | Plain Areas | Hilly/Tribal/Difficult Areas |
|---|---|---|
| Sub-Centre | 5,000 population | 3,000 population |
| Primary Health Centre | 30,000 population | 20,000 population |
| Community Health Centre | 1,20,000 population | 80,000 population |
Key Insight: The national average coverage differs from the recommended norms. A Sub-Centre typically covers about 5,624 people, a PHC covers 34,876 people, and a CHC covers 173,235 people based on current statistics.
Village Level Health Services
Accredited Social Health Activists (ASHAs)
At the grassroots level, each village or large habitation has a female Accredited Social Health Activist (ASHA) who serves as the first point of contact between the community and the public health system.
Role and Responsibilities
- Acts as a bridge between ANM and the village
- Accountable to the Panchayat
- Promotes universal immunization
- Provides referral and escort services for RCH
- Facilitates construction of household toilets
- Prepares and implements Village Health Plan
Support and Resources
- Receives performance-based compensation
- Provided with a Drug Kit containing generic AYUSH and allopathic formulations
- Undergoes 23 days of induction training spread over 12 months
- Ongoing on-the-job training throughout the year
- Government of India bears the cost of training, incentives, and medical kits
Sub-Centre/Health & Wellness Centre (SC/HWC)
The Sub-Centre is the most peripheral and first contact point between the primary health care system and the community. The revised IPHS 2022 guidelines designate them as Health and Wellness Centres (HWCs) to provide comprehensive primary care.
Staffing Pattern
| Staff Position | Number (Existing Pattern) | Number (IPHS Recommended) |
|---|---|---|
| Health Worker (Female)/ANM | 1 | 2 |
| Additional Second ANM (on contract) | 1 | – |
| Health Worker (Male) | 1 | 1 |
| Voluntary Worker (Honorarium Rs.100/- p.m.) | 1 (optional) | 1 (optional) |
Resources and Material Management
Medical Supplies
- Basic drugs for minor ailments
- Essential drugs (both allopathic and AYUSH)
- Equipment kits provided by Ministry of Health & Family Welfare
Financial Resources
- Untied Fund of Rs. 10,000 per annum
- Joint Bank Account operated by ANM & Sarpanch
- 100% Central assistance for salary of ANMs and LHVs
- Rent at the rate of Rs. 3,000/- per annum
- Contingency at the rate of Rs. 3,200/- per annum
Primary Health Centre (PHC)
The Primary Health Centre (PHC) is the first contact point between the village community and a Medical Officer. PHCs provide integrated curative and preventive healthcare with emphasis on preventive and promotive aspects.
Staffing Pattern
| Staff Position | Number (Existing Pattern) | Number (IPHS Recommended) |
|---|---|---|
| Medical Officer | 1 | 3 (At least 1 female) |
| AYUSH Practitioner | NIL | 1 |
| Pharmacist | 1 | 2 |
| Nurse-Midwife (Staff Nurse) | 1 + 2 additional on contract | 5 |
| Health Worker (Female)/ANM | 1 | 1 |
| Health Educator | 1 | 1 |
| Health Assistant (Male) | 1 | 1 |
| Health Assistant (Female)/LHV | 1 | 1 |
| Upper Division Clerk | 1 | 1 |
| Lower Division Clerk | 1 | 1 |
| Laboratory Technician | 1 | 2 |
| Driver | 1 (Subject to vehicle availability) | Optional (vehicles may be outsourced) |
| Class IV | 4 | 4 |
| Account Manager | NIL | 1 |
Infrastructure and Resources
Physical Infrastructure
- 4-6 beds for patients
- Established and maintained by State Governments under MNP/BMS Programme
- 86.7% of PHCs are located in Government buildings
Functions
- Acts as a referral unit for 6 Sub-Centres
- Curative, preventive, promotive and Family Welfare Services
- 24-hour service in at least 50% PHCs (target under NHM)
- Regular supply of essential quality drugs and equipment
Community Health Centre (CHC)
The Community Health Centre (CHC) serves as a referral centre for 4 PHCs and provides specialized healthcare services. According to IPHS 2022 guidelines, CHCs are classified into Non-FRU CHCs and FRU-CHCs.
Types of CHCs (IPHS 2022)
Non-FRU CHC
- 30 essential beds
- Provides essential services including preventive, promotive, curative, palliative, and rehabilitative services
- Normal delivery and stabilization of common emergencies
FRU CHC
- 30-50 beds depending on location
- Specialized care through specialists
- Functional operation theatre
- Blood storage unit
- Elective and emergency surgical services
Staffing Pattern
| Staff Position | Number (Existing Pattern) | Number (IPHS Recommended Essential) |
|---|---|---|
| A. Clinical Manpower | ||
| Medical Officer | 4 | – |
| Block Health Officer | – | 1 |
| General Surgeon | Specialists among the 4 MOs | 1 |
| Physician | Specialists among the 4 MOs | 1 |
| Obstetrician/Gynaecologist | Specialists among the 4 MOs | 1 |
| Paediatrician | Specialists among the 4 MOs | 1 |
| Anaesthetist | – | 1 |
| Public Health Manager | – | 1 |
| Eye Surgeon | – | 1 |
| Dental Surgeon | – | 1 |
| General Duty Medical Officer | – | 6 |
| AYUSH Specialists/GDMO | – | 2 |
| B. Support Manpower | ||
| Staff Nurse | 7 | 19 |
| Public Health Nurse | – | 1 |
| ANM | – | 1 |
| Pharmacist/Compounder | 1 | 3 |
| Pharmacist-AYUSH | – | 1 |
| Laboratory Technician | 1 | 3 |
| Radiographer | 1 | 2 |
| Other support staff | 15 | 25+ |
Staffing Challenge: There is a significant shortfall in specialists at CHCs across India. As per data, there is a shortfall of 75% of Surgeons, 65.9% of Obstetricians & Gynaecologists, 80.1% of Physicians and 74.4% of Paediatricians. Overall, there is a shortfall of 63.9% specialists at the CHCs.
Block Public Health Unit (BPHU)
According to IPHS 2022 guidelines, all CHCs at block headquarters level are to be developed as Block Public Health Units (BPHU) with four functional areas:
Clinical Service Delivery
Providing healthcare services as per IPHS standards for CHCs
Public Health Functions
Surveillance, preventive and health promotion activities
Block Public Health Laboratory
Serves both clinical and public health functions
HMIS Unit
Health Management Information System for data collection and reporting
Sub-District and District Hospitals
District Hospitals and Sub-District Hospitals form the apex of the rural healthcare pyramid, providing more advanced secondary care services and serving as referral centers for CHCs.
Sub-District Hospital
- 31-100 beds capacity
- Serves population of 1,00,000 – 5,00,000
- First referral unit for tehsil/taluk/block population
- Provides specialist services in Medicine, Surgery, Obstetrics & Gynecology, Pediatrics, Dental, and AYUSH
District Hospital
- 100-500 beds capacity based on district population
- Serves as the secondary level of health care
- Provides comprehensive secondary health care services
- Handles referrals from CHCs, PHCs, and Sub-centers
- Houses the office of Chief Medical Officer/Civil Surgeon
Material Management in Rural Health Services
Effective material management is crucial for the functioning of rural health facilities. It encompasses procurement, storage, distribution, and disposal of drugs, vaccines, and equipment.
Drug Management
Procurement and Supply
- Essential medicines should be available free of cost at all facilities
- Centralized drug purchasing and distribution system
- Indenting based on consumption patterns
- Stock rotation and FEFO (First Expiry First Out) principle
- Emergency procurement provisions to prevent stock-outs
Storage and Inventory
- Adequate and spacious stores away from patient traffic
- Proper ventilation and protection from moisture
- Compactor system compared to conventional racks
- Buffer stocks kept in separate spaces or cupboards
- Regular inspection of stored materials
- Computerized inventory management
Equipment Management
| Facility Level | Equipment Management Guidelines |
|---|---|
| Sub-Centre/HWC |
|
| PHC |
|
| CHC |
|
Biomedical Waste Management
All healthcare facilities must ensure proper collection, transportation, treatment, and disposal of bio-medical waste as per the latest Biomedical Waste Management Rules.
Waste Segregation
- Color-coded bins for different types of waste
- Specific containers for sharps
- Separate collection for infectious and non-infectious waste
Disposal Methods
- Tie-ups with authorized waste treatment facilities
- Deep burial pits for specific types of waste in rural areas
- Regular staff training on waste handling
- Maintenance of waste disposal records
Best Practices & Recent Updates in Rural Health Services
Best Practice 1: Digital Health Records and Telemedicine
Implementation of electronic health records and telemedicine services to bridge the gap between rural areas and specialized healthcare. The National Digital Health Mission aims to create a digital health ecosystem with a unique health ID for every citizen, improving healthcare delivery in remote areas.
Best Practice 2: Ayushman Bharat Health and Wellness Centres
Transforming Sub-Centres and PHCs into Health and Wellness Centres to provide comprehensive primary healthcare services. These centers focus on a wider range of services including non-communicable diseases, mental health, palliative care, geriatric care, and basic emergency services.
Best Practice 3: Block Public Health Units for Integrated Service Delivery
Establishment of Block Public Health Units at CHCs to integrate clinical services with public health functions, strengthening disease surveillance, and promoting decentralized planning. This approach enhances the response to disease outbreaks and improves routine health services.
Recent Updates in Staffing & Material Management
Staffing Updates
- Prioritized in-house hiring for clinical staff
- 15% leave and training reserves for all staff
- Multi-skilling of doctors to overcome specialist shortage
- Three-year minimum posting to ensure continuity
Material Management Updates
- Digitization of inventory and records
- Computerized prescription and dispensing systems
- Quality assurance protocols for equipment
- Enhanced biomedical waste management as per new rules
Performance Monitoring
- Implementation of quality standards (NQAS)
- Regular internal and external audits
- Patient feedback through Mera Aspataal initiative
- Performance-based incentives for healthcare workers
Conclusion
The rural health services in India are designed with a hierarchical structure to reach the vast rural population. From ASHAs at the village level to District Hospitals at the top, each tier has specific roles, staffing patterns, and material management requirements. Despite challenges like staff shortages and inadequate infrastructure in some areas, recent initiatives and best practices are strengthening the system to provide better healthcare services to rural communities.
