HIV in Pregnancy
Comprehensive Guide for Nursing Students
Table of Contents
1. Introduction to HIV in Pregnancy
Human Immunodeficiency Virus (HIV) infection during pregnancy presents unique challenges for healthcare providers, particularly nurses who play a crucial role in the management and care of affected mothers and their babies. HIV in pregnancy requires a comprehensive understanding of the virus, its transmission dynamics, and the specific interventions needed to minimize mother-to-child transmission (MTCT).
HIV is a retrovirus that attacks the body’s immune system, specifically CD4+ T cells, which are vital in fighting infections. If left untreated, HIV can progress to Acquired Immunodeficiency Syndrome (AIDS), characterized by severe immunodeficiency and opportunistic infections.
Memory Aid: H.I.V.
H – High-risk scenarios require testing
I – Infection can cross the placenta
V – Viral load monitoring is essential
2. Epidemiology and Global Impact
Globally, HIV continues to be a significant public health concern, particularly affecting pregnant women and their children. According to recent data:
- In 2023, approximately 39.9 million people were living with HIV globally, with 65% in the WHO African Region.
- Mother-to-child transmission rates have decreased substantially from >20% to around 1.9% in countries with effective PMTCT programs.
- Without any intervention, the risk of vertical transmission during pregnancy, delivery, or breastfeeding can be as high as 25-30%.
- With appropriate interventions, including antiretroviral therapy (ART), the risk can be reduced to less than 1%.
The epidemiological landscape of HIV in pregnancy varies significantly across regions, with higher prevalence rates in resource-limited settings where access to preventive measures and treatment may be constrained.
3. Pathophysiology of HIV in Pregnancy
Understanding the pathophysiology of HIV in pregnancy is crucial for nursing care planning and intervention. Key aspects include:
Maternal Impact
- Accelerated CD4+ T cell depletion
- Increased risk of opportunistic infections
- Potential for obstetric complications
- Physiological changes affecting drug metabolism
Fetal Impact
- Risk of transplacental transmission
- Potential for fetal growth restriction
- Increased risk of preterm birth
- Development of fetal HIV infection
Pregnancy itself does not typically accelerate HIV disease progression in women who are on effective antiretroviral therapy. However, untreated HIV infection during pregnancy can lead to various adverse outcomes for both mother and child.
Memory Aid: P.A.T.H.
P – Placental barrier can be breached by HIV
A – Advanced disease increases transmission risk
T – T-cell depletion affects maternal immune function
H – Higher viral load correlates with higher transmission risk
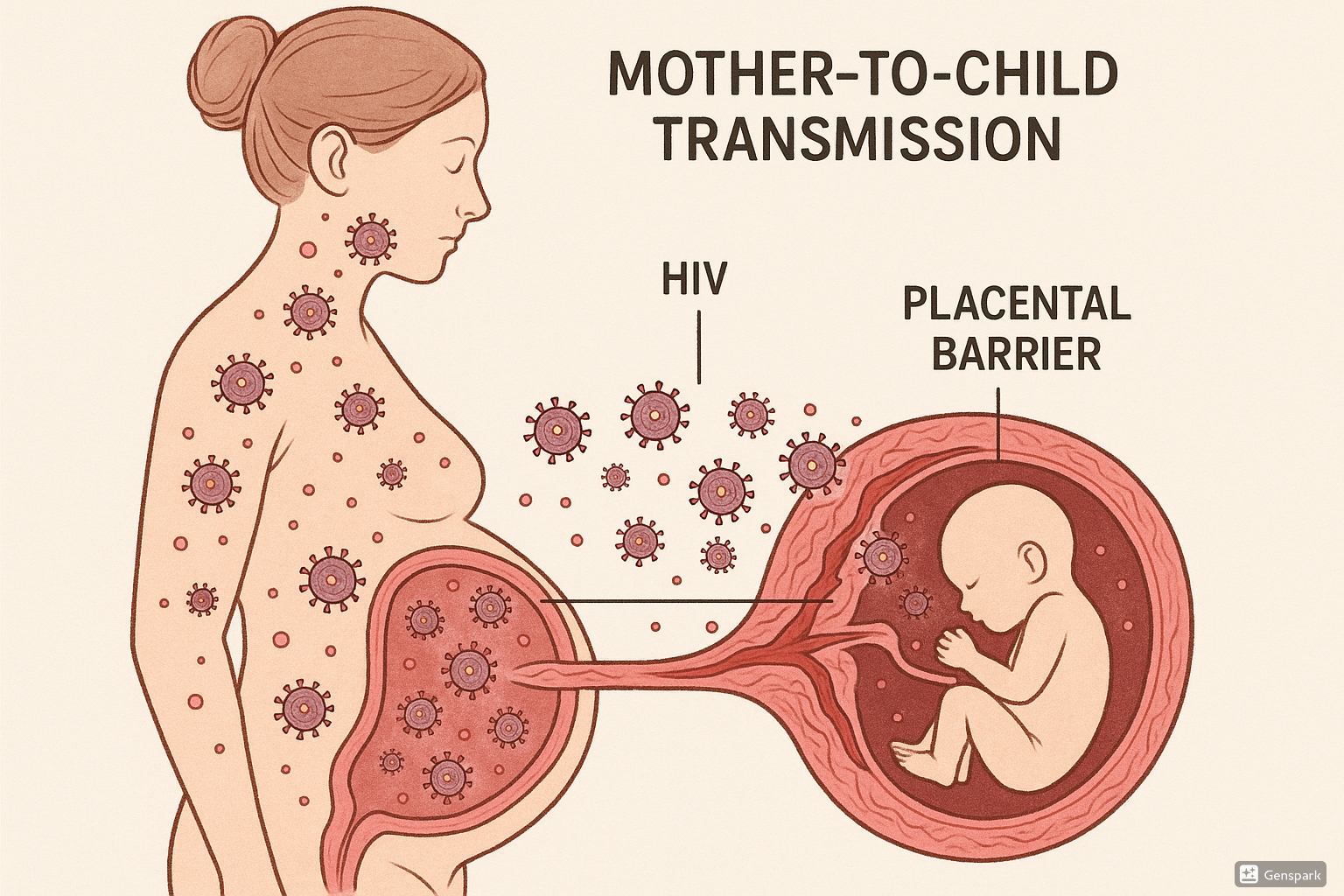
4. Mother-to-Child Transmission (MTCT)
Mother-to-child transmission (MTCT), also known as vertical transmission, refers to the transmission of HIV from an HIV-positive mother to her child during pregnancy, labor, delivery, or breastfeeding. Understanding the mechanisms of transmission is essential for implementing effective preventive strategies.
Transmission Timing and Mechanisms:
| Timing | Mechanism | Risk Contribution |
|---|---|---|
| In utero (intrauterine) | Transplacental transmission, microtransfusions across the placenta | 5-10% of MTCT cases |
| Intrapartum (during labor and delivery) | Exposure to maternal blood and genital secretions, ascending infection | 10-15% of MTCT cases |
| Postpartum (breastfeeding) | Transmission through breast milk containing HIV | 5-15% additional risk |
Early intrauterine transmission appears to be rare, with most in utero infections occurring late in pregnancy. The risk of transmission is significantly higher during labor and delivery due to maternal blood and secretions exposure.
5. Risk Factors for MTCT
Several factors increase the risk of mother-to-child transmission of HIV. Understanding these risk factors is crucial for identifying high-risk pregnancies and implementing appropriate interventions.
Maternal Factors
- High maternal viral load (>1,000 copies/mL)
- Low CD4+ T cell count (<500 cells/mm³)
- Advanced HIV disease or AIDS
- Primary HIV infection during pregnancy
- Poor adherence to antiretroviral therapy
- Concurrent sexually transmitted infections
Obstetric and Neonatal Factors
- Prolonged rupture of membranes (>4 hours)
- Invasive obstetric procedures
- Vaginal delivery (when viral load is high)
- Preterm birth
- Breastfeeding
- Acute chorioamnionitis
Clinical Alert
The single most important determinant of MTCT risk is maternal plasma viral load. Achieving viral suppression through ART is critical for prevention.
6. Diagnosis and Screening
Early diagnosis and routine screening for HIV during pregnancy are cornerstones of effective prevention strategies. Current guidelines recommend:
Screening Recommendations:
- Universal HIV screening for all pregnant women as early as possible in pregnancy, ideally during the first prenatal visit
- Repeat testing in the third trimester (28-32 weeks) for women at high risk or in high-prevalence areas
- Rapid HIV testing during labor for women with unknown HIV status
- Opt-out approach to remove stigma associated with HIV testing
Diagnostic testing for HIV typically involves a two-step process:
Initial Screening
- Fourth-generation HIV antigen/antibody combination immunoassays
- Rapid HIV antibody tests (for point-of-care testing)
- Results typically available within minutes to hours
Confirmatory Testing
- HIV-1/HIV-2 antibody differentiation immunoassay
- HIV RNA PCR testing (viral load)
- Determines HIV type and viral load
Nursing Alert
The differential diagnosis for acute HIV infection in pregnancy can include infectious mononucleosis, syphilis, rubella, toxoplasmosis, and other viral syndromes. Always consider HIV in pregnant women presenting with flulike symptoms.
7. Nursing Assessment and Diagnosis
Comprehensive nursing assessment is crucial for developing appropriate care plans for pregnant women with HIV. Key aspects of the assessment include:
Nursing Assessment Components:
- Complete health history, including HIV diagnosis, treatment history, and adherence
- Current antiretroviral therapy regimen and adherence patterns
- Psychosocial assessment, including support systems and coping mechanisms
- Risk factors for opportunistic infections and other complications
- Laboratory data: CD4+ count, viral load, complete blood count, liver and kidney function
- Mental health screening for anxiety, depression, and stigma-related concerns
Common nursing diagnoses for pregnant women with HIV include:
Physical Health Diagnoses
- Risk for infection related to immunosuppression
- Ineffective protection related to compromised immune system
- Imbalanced nutrition: less than body requirements
- Fatigue related to disease process
- Risk for impaired fetal development
Psychosocial Diagnoses
- Anxiety related to pregnancy outcomes and HIV status
- Fear related to potential infant infection
- Deficient knowledge about HIV management in pregnancy
- Risk for ineffective coping related to diagnosis
- Risk for interrupted family processes
Memory Aid: N.U.R.S.E.
N – Nutrition status assessment for both mother and fetus
U – Understanding level of HIV knowledge and prevention strategies
R – Risk factor identification for MTCT
S – Support system evaluation
E – Emotional health assessment
8. Antiretroviral Therapy in Pregnancy
Antiretroviral therapy (ART) is the cornerstone of HIV management during pregnancy, playing a crucial role in preventing mother-to-child transmission and maintaining maternal health.
Current Guidelines
All pregnant individuals with HIV should initiate antiretroviral therapy as early in pregnancy as possible, regardless of their CD4+ count or HIV RNA level, to maximize health outcomes and prevent vertical transmission.
Current Preferred Antiretroviral Regimens:
| Scenario | Recommended Regimen | Notes |
|---|---|---|
| Treatment-naïve, newly diagnosed | Dolutegravir-based regimens with dual-NRTI backbone | Data supports safety at all stages of pregnancy |
| Already on effective ART | Continue current regimen if virally suppressed | Avoid regimen switches when possible |
| First trimester options | Dolutegravir + tenofovir disoproxil fumarate/emtricitabine or abacavir/lamivudine | Current evidence shows no increased risk of neural tube defects |
| Alternative options | Raltegravir-based regimens, atazanavir/ritonavir-based regimens | For those with contraindications to preferred regimens |
Recent updates in ART guidelines for pregnancy include:
- Dolutegravir is now considered safe for use throughout pregnancy, including conception and first trimester
- Bictegravir/FTC/TAF is now included as an acceptable regimen for pregnant individuals
- Cobicistat-boosted regimens (elvitegravir, darunavir, atazanavir) are generally avoided due to pharmacokinetic concerns in pregnancy
Memory Aid: A.R.T.
A – Adherence is critical for viral suppression
R – Regimen selection based on safety, potency, and resistance profile
T – Timing matters; earlier initiation improves outcomes
9. Prevention Strategies (PMTCT)
Prevention of Mother-to-Child Transmission (PMTCT) encompasses a comprehensive approach that extends beyond antiretroviral therapy. The WHO’s four-pronged approach to PMTCT includes:
Prong 1 & 2
- Prong 1: Primary prevention of HIV infection among women of childbearing age
- Prong 2: Preventing unintended pregnancies among women living with HIV
Prong 3 & 4
- Prong 3: Preventing HIV transmission from a woman living with HIV to her infant
- Prong 4: Providing appropriate treatment, care, and support to mothers living with HIV, their children, and families
Specific interventions for PMTCT during different phases include:
PMTCT Strategies Throughout Pregnancy and Beyond:
| Phase | Interventions |
|---|---|
| Antepartum |
|
| Intrapartum |
|
| Postpartum |
|
Critical Point
The success of PMTCT depends on a continuum of care that spans pre-conception through postpartum periods. Gaps at any point can increase transmission risk.
10. Nursing Care During Pregnancy
Nurses play a pivotal role in the prenatal care of women with HIV. Comprehensive nursing care encompasses multiple domains:
Clinical Management
- Facilitating regular prenatal visits (often more frequent than standard care)
- Monitoring medication adherence and potential side effects
- Assessing for signs of opportunistic infections
- Tracking viral load and CD4+ count results
- Coordinating care with HIV specialists and obstetricians
Education and Support
- Providing information about HIV and pregnancy
- Teaching medication administration and importance of adherence
- Discussing transmission prevention strategies
- Preparing for labor, delivery, and postpartum periods
- Addressing psychosocial concerns and stigma
Nursing interventions during the prenatal period include:
- Comprehensive education about HIV treatment and prevention of transmission
- Regular assessment of medication adherence and development of strategies to address barriers
- Monitoring for drug interactions and side effects
- Emotional support and counseling to address fears related to pregnancy outcomes and HIV status
- Referral to community resources and support groups for women with HIV
- Nutritional counseling to support maternal and fetal health
Memory Aid: C.A.R.E.
C – Consistent viral suppression monitoring
A – Adherence support for antiretroviral therapy
R – Referrals to specialized services
E – Education about prevention strategies
11. Labor and Delivery Management
Labor and delivery represent critical periods for MTCT risk. Nursing care during this phase focuses on implementing protective strategies while supporting the birthing process.
Mode of Delivery Considerations:
| Scenario | Recommendation | Rationale |
|---|---|---|
| Viral load <1,000 copies/mL | Vaginal delivery is appropriate | Low risk of transmission with suppressed viral load |
| Viral load >1,000 copies/mL at 36 weeks | Scheduled cesarean delivery at 38 weeks | Reduces exposure to maternal blood/secretions |
| Unknown viral load at delivery | Consider scheduled cesarean delivery | Precautionary approach |
Key nursing considerations during labor and delivery include:
- Ensuring continuation of maternal antiretroviral therapy during labor
- Implementing intravenous zidovudine during labor for women with viral load >1,000 copies/mL
- Minimizing invasive procedures (e.g., fetal scalp electrodes, artificial rupture of membranes)
- Avoiding prolonged rupture of membranes when possible
- Using proper personal protective equipment for all healthcare providers
- Preparing for immediate postpartum infant prophylaxis
Nursing Alert
Intravenous zidovudine is typically administered as a loading dose of 2 mg/kg over 1 hour, followed by continuous infusion of 1 mg/kg/hour until delivery for women with viral load >1,000 copies/mL or unknown viral load at the time of labor.
12. Postpartum and Neonatal Care
Postpartum and neonatal care focus on continuing prevention strategies, monitoring both mother and infant, and supporting transition to long-term care.
Maternal Postpartum Care
- Continuation of antiretroviral therapy
- Monitoring for postpartum complications
- Assessment of medication adherence
- Support for mental health concerns
- Counseling on contraception options
- Continuity of HIV care transitions
Neonatal Care
- Initiating ARV prophylaxis ideally within 6-12 hours of birth
- HIV testing with age-appropriate methods
- Monitoring for medication side effects
- Routine pediatric care and immunizations
- Growth and development monitoring
- PCP prophylaxis if indicated
Infant Feeding Recommendations:
| Setting | Recommendation | Rationale |
|---|---|---|
| Resource-rich settings | Complete avoidance of breastfeeding | Formula feeding is safe and available |
| Resource-limited settings | Exclusive breastfeeding for 6 months with maternal ART | Benefits of breastfeeding outweigh risks when safe alternatives unavailable |
| U.S. setting with fully suppressed viral load | Informed shared decision-making about breastfeeding | Risk less than 1% with undetectable viral load, but not zero |
Infant HIV testing schedule includes:
- HIV nucleic acid testing (NAT) at birth (within 24-48 hours)
- HIV NAT at 1-2 months of age
- HIV NAT at 4-6 months of age
- HIV antibody testing at 12-18 months to confirm serostatus
Memory Aid: N.E.O.N.
N – Neonatal prophylaxis starts within hours of birth
E – Early diagnosis with appropriate testing
O – Ongoing maternal therapy is continued
N – Nutrition counseling about feeding options
13. Best Practices and Updates
Staying current with best practices and recent updates is essential for providing quality nursing care. Here are three key developments in HIV management during pregnancy:
Best Practice #1: Dolutegravir Safety in Pregnancy
Recent evidence has established the safety of dolutegravir-based regimens throughout pregnancy, including at conception and in the first trimester. Current guidelines now recommend dolutegravir as a preferred agent in pregnancy due to its high efficacy, high barrier to resistance, and favorable safety profile. This represents a significant shift from previous concerns about neural tube defects.
Best Practice #2: U=U in Perinatal Context
The concept of “Undetectable = Untransmittable” (U=U) is now being applied to the perinatal context. With consistent maternal viral suppression throughout pregnancy and breastfeeding, the risk of transmission is reduced to less than 1%. This has implications for counseling and shared decision-making about mode of delivery and infant feeding options, though complete elimination of risk remains the goal in resource-rich settings.
Best Practice #3: Triple Elimination Initiative
WHO’s “Triple Elimination Initiative” encourages countries to simultaneously commit to eliminating mother-to-child transmission of HIV, syphilis, and hepatitis B. This comprehensive approach recognizes the overlapping risk factors and transmission routes of these infections and promotes integrated testing, treatment, and prevention strategies during prenatal care. Nurses should incorporate screening and management strategies for all three infections in their care plans.
Emerging Research
Current research is exploring long-acting injectable antiretroviral options that may benefit pregnant women with adherence challenges, though data on safety in pregnancy is still accumulating. Additionally, novel approaches to immune-based prevention strategies, including maternal vaccination, are under investigation.
14. References
- Centers for Disease Control and Prevention. (2025). HIV and breastfeeding. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/illnesses-conditions/hiv.html
- Clinicalinfo.HIV.gov. (2024). Recommendations for the use of antiretroviral drugs during pregnancy. https://clinicalinfo.hiv.gov/en/guidelines/perinatal/recommendations-arv-drugs-pregnancy-overview
- HIV.gov. (2025). Preventing perinatal transmission of HIV. https://www.hiv.gov/hiv-basics/hiv-prevention/reducing-mother-to-child-risk/preventing-mother-to-child-transmission-of-hiv
- American College of Obstetricians and Gynecologists. (2018). Labor and delivery management of women with human immunodeficiency virus infection. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/09/labor-and-delivery-management-of-women-with-human-immunodeficiency-virus-infection
- World Health Organization. (2023). Infant feeding for the prevention of mother-to-child transmission of HIV. https://www.who.int/tools/elena/interventions/hiv-infant-feeding
- Moses, S., et al. (2023). The vital role of public health nurses in perinatal HIV prevention and care. https://pmc.ncbi.nlm.nih.gov/articles/PMC10246483/
- Roth, C. (2021). HIV in pregnancy. Nursing for Women’s Health. https://www.nwhjournal.org/article/S1751-4851(15)00012-4/fulltext
- UNAIDS. (2023). Prevention of HIV transmission from mother to child. https://www.unaids.org/sites/default/files/media_asset/prevention_en_0.pdf
- World Health Organization. (2024). Triple elimination initiative of mother-to-child transmission of HIV, syphilis, and hepatitis B. https://www.who.int/initiatives/triple-elimination-initiative-of-mother-to-child-transmission-of-hiv-syphilis-and-hepatitis-b
- NIH. (2024). Management of infants born to mothers with HIV infection. https://clinicalinfo.hiv.gov/en/guidelines/perinatal/infant-feeding-individuals-hiv-united-states
