Infections in Pregnancy: A Comprehensive Guide for Nursing Students
Essential knowledge for identifying, managing, and preventing infections during pregnancy
Table of Contents
Introduction to Infections in Pregnancy
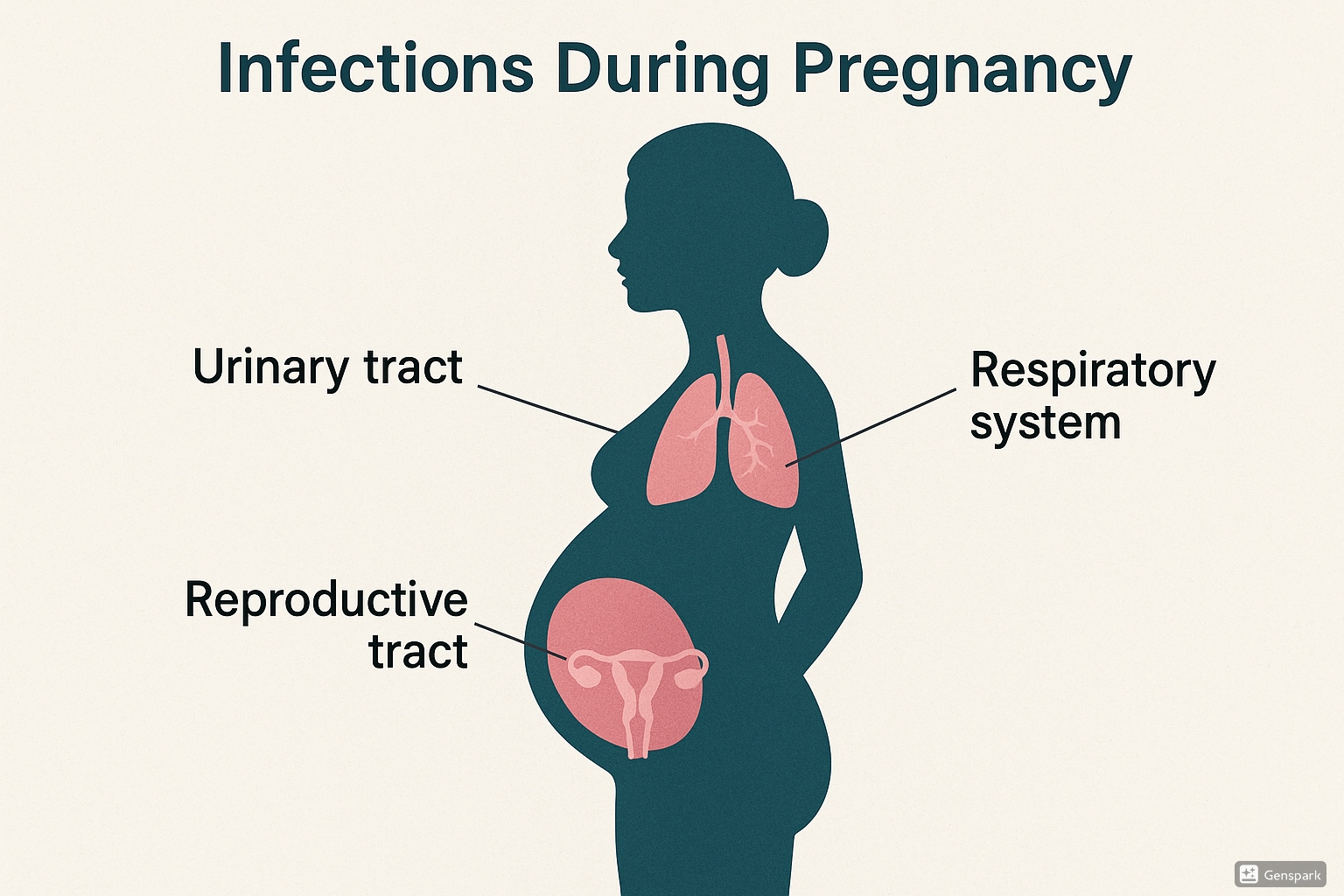
Pregnancy creates a unique physiological state that can alter a woman’s susceptibility to various infections. The immune system undergoes significant changes to accommodate the developing fetus, which can sometimes increase vulnerability to infections. Additionally, anatomical and physiological alterations during pregnancy can create conditions favorable for certain pathogens to thrive.
Infections in pregnancy represent a significant concern as they can affect both maternal and fetal health. Some infections may be asymptomatic in the mother but can cross the placenta and cause serious congenital issues. Early detection, appropriate treatment, and preventive measures are crucial aspects of prenatal care that nursing professionals must be well-versed in.
Important Concept
Maternal infections can be transmitted to the fetus in three primary ways:
- Transplacental transmission (hematogenous spread)
- Ascending infection from the vagina through the cervix
- During delivery through contact with maternal blood or vaginal secretions
Urinary Tract Infections in Pregnancy
Urinary Tract Infections (UTIs) are among the most common infections in pregnancy, affecting 2-10% of pregnant women. The increased prevalence is due to several pregnancy-related changes:
- Urinary stasis due to progesterone-induced smooth muscle relaxation
- Mechanical compression of the ureters by the enlarging uterus
- Increased bladder volume and decreased bladder tone
- Glycosuria and aminoaciduria providing a favorable medium for bacterial growth
Types of UTIs in Pregnancy
| Type | Characteristics | Clinical Manifestations | Management | Complications if Untreated |
|---|---|---|---|---|
| Asymptomatic Bacteriuria (ASB) | Bacterial colonization without symptoms | No symptoms; detected through routine urine cultures | 7-day course of antibiotics (commonly nitrofurantoin, amoxicillin, or cephalexin) | 30% progress to pyelonephritis if untreated |
| Acute Cystitis | Infection of the bladder | Dysuria, urgency, frequency, suprapubic pain, hematuria | 7-14 day antibiotic regimen; increased fluid intake | Pyelonephritis, preterm labor |
| Pyelonephritis | Upper urinary tract infection affecting kidneys | Fever, chills, flank pain, nausea/vomiting, costovertebral angle tenderness | Hospitalization, IV antibiotics, hydration; oral antibiotics after improvement | Sepsis, preterm birth, low birth weight, respiratory distress |
Memory Aid: “DIAPER” for UTI Risk Factors in Pregnancy
- D: Diabetes & Dilated collecting system
- I: Immunosuppression
- A: Anatomical abnormalities
- P: Previous UTIs
- E: Elevated bladder pressure from the growing uterus
- R: Reflux (vesicoureteral)
Diagnostic Approaches for UTIs
Proper diagnosis of infections in pregnancy like UTIs requires:
- Clean-catch midstream urine specimen
- Urinalysis (pyuria, bacteriuria, nitrites, leukocyte esterase)
- Urine culture and sensitivity (gold standard)
- Complete blood count to assess inflammatory response
Nursing Tip
When collecting urine samples from pregnant women, provide clear instructions on proper cleansing techniques and how to obtain a clean-catch midstream specimen to reduce contamination. Remember to process samples within 1 hour or refrigerate to prevent bacterial overgrowth.
Bacterial Infections in Pregnancy
Bacterial infections in pregnancy can cause significant maternal morbidity and adverse fetal outcomes. Timely identification and appropriate antimicrobial therapy are essential for preventing complications.
Common Bacterial Infections During Pregnancy
| Infection | Causative Agent | Clinical Features | Maternal/Fetal Effects | Management |
|---|---|---|---|---|
| Group B Streptococcus (GBS) | Streptococcus agalactiae | Often asymptomatic; can cause UTI, chorioamnionitis | Neonatal meningitis, pneumonia, sepsis; preterm birth | Universal screening at 35-37 weeks; intrapartum antibiotic prophylaxis (penicillin or ampicillin) |
| Listeriosis | Listeria monocytogenes | Flu-like symptoms, fever, gastrointestinal symptoms | Miscarriage, stillbirth, preterm birth, neonatal sepsis | IV ampicillin ± gentamicin; avoidance of high-risk foods |
| Bacterial Vaginosis (BV) | Polymicrobial (Gardnerella vaginalis, Prevotella, Mobiluncus) | Thin, grayish discharge with “fishy” odor | Preterm birth, PROM, chorioamnionitis | Oral metronidazole or clindamycin |
| Syphilis | Treponema pallidum | Primary: Chancre; Secondary: Rash; Latent: Asymptomatic | Congenital syphilis, stillbirth, hydrops fetalis | Penicillin G (no adequate alternative in pregnancy) |
| Gonorrhea | Neisseria gonorrhoeae | Often asymptomatic; vaginal discharge, dysuria | Preterm labor, PROM, neonatal conjunctivitis | Ceftriaxone IM; partner treatment essential |
| Chlamydia | Chlamydia trachomatis | Often asymptomatic; mucopurulent discharge | Preterm birth, neonatal conjunctivitis, pneumonia | Azithromycin or amoxicillin; partner treatment |
Memory Aid: “TORCH-B” for Bacterial TORCH Infections
While TORCH typically refers to Toxoplasmosis, Other (syphilis), Rubella, Cytomegalovirus, and Herpes, you can remember key bacterial infections with “TORCH-B”:
- Treponema pallidum (Syphilis)
- Oral bacteria like Fusobacterium (periodontal disease)
- Rickettsia (Q fever)
- Chlamydia trachomatis
- Hemophilus influenzae
- Bacteria like Listeria, Group B Strep
Tuberculosis in Pregnancy
Maternal tuberculosis (TB) is a significant concern in infections in pregnancy, especially in high-prevalence areas:
- Diagnostic challenges: Avoid X-rays when possible; IGRA or tuberculin skin tests are not affected by pregnancy
- Treatment: Isoniazid, rifampin, and ethambutol are generally safe; streptomycin is contraindicated
- Congenital TB is rare but has high mortality if untreated
- Nursing considerations: Monitor for hepatotoxicity, ensure adequate vitamin B6 supplementation with isoniazid
Important Consideration
Never delay treatment of active TB during pregnancy. The risks of untreated TB far outweigh the potential risks of first-line anti-tuberculosis medications. Prompt treatment protects both the mother and the fetus.
Protozoal Infections in Pregnancy
Protozoal infections in pregnancy can cause significant maternal and fetal morbidity. These single-celled parasites can cross the placenta and infect the developing fetus, resulting in congenital disorders.
Common Protozoal Infections During Pregnancy
| Infection | Causative Agent | Transmission | Clinical Manifestations | Fetal Effects | Management |
|---|---|---|---|---|---|
| Toxoplasmosis | Toxoplasma gondii | Undercooked meat, cat feces, contaminated soil | Often asymptomatic; flu-like symptoms, lymphadenopathy | Hydrocephalus, intracranial calcifications, chorioretinitis, mental retardation | Spiramycin (prevention of transmission); pyrimethamine + sulfadiazine + folinic acid after 18 weeks for confirmed fetal infection |
| Malaria | Plasmodium species (P. falciparum most severe) | Anopheles mosquito bite | Cyclical fever, chills, headache, nausea/vomiting | Intrauterine growth restriction, preterm birth, stillbirth, congenital malaria | Preventive measures; chloroquine (sensitive areas); artemisinin-based treatment in 2nd/3rd trimester; quinine + clindamycin in 1st trimester |
| Trichomoniasis | Trichomonas vaginalis | Sexual transmission | Frothy, malodorous vaginal discharge; vulvovaginal irritation | Preterm birth, premature rupture of membranes, low birth weight | Metronidazole (safe in all trimesters); treat partners; retest after treatment |
| Chagas Disease | Trypanosoma cruzi | Triatomine bug (“kissing bug”); congenital; blood transfusion | Acute: fever, malaise, edema; Chronic: cardiomyopathy | Congenital infection (2-10%); hepatosplenomegaly, meningoencephalitis | Screening in endemic areas; benznidazole may be used after 1st trimester; treatment of infant if infected |
Toxoplasmosis: Prevention and Screening
Toxoplasmosis is a significant concern among protozoal infections in pregnancy. Preventing primary infection during pregnancy is crucial:
- Cook meat to safe temperatures (145°F for whole cuts, 160°F for ground meat)
- Wash fruits and vegetables thoroughly
- Avoid changing cat litter or use gloves and wash hands thoroughly
- Keep cats indoors and feed them commercial food rather than raw meat
- Wear gloves when gardening and avoid soil potentially contaminated with cat feces
Memory Aid: “ABCDEF” for Classic Signs of Congenital Toxoplasmosis
- Abnormal CSF
- Brain calcifications
- Chorioretinitis
- Developmental delay
- Enlarged liver/spleen (hepatosplenomegaly)
- Fluid in brain (hydrocephalus)
Regional Consideration
Screening practices for toxoplasmosis vary by country. In the United States, universal screening is not recommended, while in France and Austria, monthly serological screening is standard practice for seronegative women during pregnancy. Nurses should be aware of local guidelines.
Fungal Infections in Pregnancy
Fungal infections in pregnancy are common due to the altered vaginal environment, increased glycogen content, and immunological changes that occur during gestation. While most fungal infections are not transmitted to the fetus, they can cause significant discomfort and complications for the mother.
Vulvovaginal Candidiasis
Vulvovaginal candidiasis (VVC) affects up to 30% of pregnant women, most commonly in the second trimester:
- Causative agent: Primarily Candida albicans (80-90%), followed by C. glabrata and other species
- Risk factors: Pregnancy, diabetes, antibiotic use, immunosuppression, tight-fitting clothing
- Clinical features: Thick, white “cottage cheese-like” discharge, intense vulvar pruritus, dysuria, dyspareunia
- Diagnosis: Clinical appearance, KOH microscopy showing pseudohyphae/yeast buds, pH typically normal (4.0-4.5)
- Treatment: Topical azoles (clotrimazole, miconazole) are first-line; oral fluconazole generally avoided in pregnancy
| Antifungal Agent | Pregnancy Category | Recommended Use in Pregnancy | Administration | Duration |
|---|---|---|---|---|
| Clotrimazole | B | Preferred option | Vaginal cream or suppository | 7 days |
| Miconazole | B | Preferred option | Vaginal cream or suppository | 7 days |
| Nystatin | B | Alternative option | Vaginal tablet | 14 days |
| Terconazole | C | Use with caution | Vaginal cream or suppository | 3-7 days |
| Fluconazole (oral) | D | Generally avoided; potential risk of birth defects with high doses/long-term use | Oral tablet | Single dose (150mg) |
Nursing Tip
When educating pregnant patients about vulvovaginal candidiasis prevention, remember the “Cotton, Cool, and Clean” principle: wear cotton underwear, avoid tight clothing, keep the genital area cool and dry, and maintain good hygiene without douching.
Other Fungal Infections
Although less common, other fungal infections in pregnancy require attention:
- Dermatophytoses (ringworm): Topical antifungals like clotrimazole and miconazole are preferred over oral options
- Onychomycosis: Generally treated after pregnancy due to need for long-term oral therapy
- Systemic fungal infections: Rare in pregnancy but may include:
- Histoplasmosis: Treatment with amphotericin B if severe; azoles avoided in first trimester
- Coccidioidomycosis: Higher risk of dissemination in pregnant women; amphotericin B for treatment
- Cryptococcosis: Amphotericin B + flucytosine for severe infection; consultation with infectious disease specialist required
Important Consideration
Systemic fungal infections during pregnancy require a multidisciplinary approach involving maternal-fetal medicine specialists, infectious disease experts, and neonatologists. The risk-benefit ratio of treatment must be carefully evaluated on an individual basis.
Nursing Assessment and Interventions
Nursing professionals play a crucial role in preventing, identifying, and managing infections in pregnancy. A systematic approach to assessment and intervention is essential for optimal maternal and fetal outcomes.
Assessment Strategies
| Assessment Component | Key Elements | Nursing Considerations |
|---|---|---|
| History Taking |
|
Use non-judgmental approach; create privacy for sensitive questions; consider cultural factors affecting reporting |
| Physical Assessment |
|
Compare findings to baseline; remember physiologic changes of pregnancy may mask or mimic infection signs |
| Laboratory Monitoring |
|
Explain purpose of tests; ensure proper collection techniques; follow up on results promptly |
| Fetal Assessment |
|
Correlate maternal infection status with fetal well-being; recognize patterns suggesting fetal compromise |
Nursing Interventions for Infections in Pregnancy
| Intervention Category | Specific Actions |
|---|---|
| Infection Prevention Counseling |
|
| Medication Administration |
|
| Symptom Management |
|
| Education and Support |
|
Memory Aid: “INFECTIONS” Nursing Priority Framework
- Identify risk factors early
- Note maternal and fetal vital signs
- Facilitate appropriate specimen collection
- Educate about prevention strategies
- Coordinate multidisciplinary care
- Treatment administration and monitoring
- Implement comfort measures
- Observe for complications
- Nurture maternal-infant bonding despite isolation needs
- Support psychosocial needs
Documentation Focus
Comprehensive documentation for infections in pregnancy should include:
- Infection type, onset, and suspected source
- Maternal vital signs and symptoms, including temporal patterns
- Fetal assessment findings
- Treatment initiated, including timing of first doses
- Patient education provided and demonstrated understanding
- Response to interventions and any adverse reactions
Best Practices and Recent Updates
Current Best Practices for Managing Infections in Pregnancy
1. Universal GBS Screening with Risk-Based Approach
Recent updates recommend a combined approach to Group B Streptococcal prevention:
- Universal screening at 36-38 weeks (updated from previous 35-37 weeks window)
- Point-of-care molecular testing in labor for women with unknown GBS status
- Risk-based assessment when results unavailable (pre-term labor, prolonged rupture of membranes)
- New research supporting vaginal-rectal screening plus point-of-care testing for highest sensitivity
2. Expanded Zika Virus Testing and Management
Updated guidelines for managing Zika virus exposure during pregnancy:
- Extended testing window up to 12 weeks after possible exposure (increased from previous 8-week window)
- Integration of Zika virus nucleic acid testing (NAT) and serologic testing for comprehensive assessment
- Serial ultrasounds every 3-4 weeks for exposed pregnant women regardless of symptoms
- Enhanced postnatal monitoring protocols for infants born to mothers with possible exposure
3. Telehealth Monitoring for Mild to Moderate Infections
Emerging evidence supports remote monitoring for certain infections in pregnancy:
- Implementation of home monitoring protocols for uncomplicated UTIs with virtual follow-up
- Remote temperature and symptom tracking applications with alert thresholds
- Virtual consultation pathways for mild viral illness assessment
- Integration of laboratory services with telehealth platforms for seamless monitoring
- Clear escalation protocols for symptoms requiring in-person evaluation
Recent Alert
The CDC has updated recommendations regarding azithromycin use for chlamydial infections during pregnancy due to emerging resistance patterns. Current guidance emphasizes test-of-cure at 3-4 weeks after treatment completion for all pregnant women, not just those with persistent symptoms.
Research Update
Recent studies have shown promising results for using maternal blood tests to detect fetal cytomegalovirus infection non-invasively. Cell-free DNA testing may eventually provide an alternative to invasive amniocentesis for diagnosing congenital CMV, though this technology is still under investigation and not yet in clinical practice.
