Table of Contents
Introduction to Uterine Inversion
Uterine inversion is a rare but serious obstetric emergency characterized by the turning inside-out of the uterus, where the fundus collapses into the uterine cavity, potentially extending through the cervix and into the vagina. This condition poses significant risk to maternal health due to severe hemorrhage and shock, necessitating immediate recognition and intervention to prevent maternal morbidity and mortality.
Key Facts About Uterine Inversion
- Occurs most commonly during the third stage of labor (immediately after childbirth)
- Can be complete or incomplete depending on the extent of fundal collapse
- Represents a true obstetric emergency requiring immediate intervention
- Associated with significant blood loss and hemodynamic instability
- Prompt recognition and management significantly improves outcomes
- Appropriate nursing care is essential throughout the management process
Throughout this comprehensive guide, we will explore the pathophysiology, clinical presentation, diagnosis, management, and nursing considerations for uterine inversion. As nursing professionals, developing a thorough understanding of this condition is essential for providing timely, evidence-based care to affected patients and potentially saving lives in emergency obstetric situations.
Epidemiology & Incidence
Uterine inversion is a rare obstetric emergency with variable reported incidence rates globally. Understanding the epidemiological aspects provides context for recognizing this condition in clinical practice.
| Region/Country | Incidence Rate | Notable Features |
|---|---|---|
| Global Range | 1 in 2,000 to 1 in 23,000 deliveries | Wide variation due to differences in obstetric practices |
| United States | Approximately 1 in 20,000 deliveries | Lower incidence likely due to modern obstetric practices |
| India | 3 times higher than US rates | Higher rates potentially related to obstetric management variations |
| Developed Countries | 1 in 8,000 to 1 in 20,000 deliveries | Decreased following implementation of active management of third stage labor |
| Developing Countries | Up to 1 in 2,000 deliveries | Higher rates potentially due to limited resources and training |
Epidemiological Insights
- The incidence has decreased fourfold after the introduction of active management during the third stage of labor
- Paradoxically, uterine inversion is observed more frequently in “low-risk” deliveries
- Mortality rates have decreased significantly with modern obstetric practices, from historical rates of 15% to less than 1% in developed countries
- Recurrence risk in subsequent pregnancies is not well-established, but isolated case reports suggest potential recurrence
Pathophysiology of Uterine Inversion
The pathophysiology of uterine inversion involves a complex interplay of mechanical forces, uterine relaxation, and anatomical factors. Understanding these mechanisms is crucial for nurses to comprehend why the condition develops and how interventions work.
Core Pathophysiological Mechanisms
- Excessive traction on umbilical cord
- Fundal pressure during placental delivery
- Abnormal attachment of placenta to uterine fundus
- Short umbilical cord creating downward traction
- Uterine atony (relaxed uterus)
- Abnormal thinning of uterine wall
- Weak or compromised myometrial tissue
- Congenital uterine anomalies
- Placenta accreta/increta/percreta
- Uterine overdistension
- Connective tissue disorders
- Previous uterine surgeries
Three-Step Pathophysiological Process
Uterine inversion typically develops through a sequence of events:
Step 1: Initial Dimpling
A portion of the uterine wall (typically the fundus) begins to indent or dimple inward into the uterine cavity, often where the placenta is attached.
Step 2: Uterine Relaxation
Relaxation of part or all of the uterine musculature allows the inward depression to continue without resistance from contracting muscles.
Step 3: Downward Traction
Simultaneous downward traction (from cord pulling, fundal pressure, or maternal pushing) causes the fundus to be pulled through the cervix.
Physiological Consequences
Hemodynamic Effects
- Hemorrhage: Occurs due to inability of the inverted uterus to contract properly and compress bleeding vessels
- Neurogenic Shock: Results from parasympathetic stimulation as the uterus stretches through the cervix
- Disproportionate Shock: The degree of shock often exceeds what would be expected from the visible blood loss alone
- Vagal Response: Stretching of uterine ligaments can trigger a vasovagal response leading to bradycardia and hypotension
Understanding these pathophysiological mechanisms helps nurses recognize the condition earlier, anticipate complications, and understand the rationale behind management approaches. The inverted uterus is unable to contract effectively, which leads to continued bleeding from the placental site and increases the risk for hemorrhagic shock.
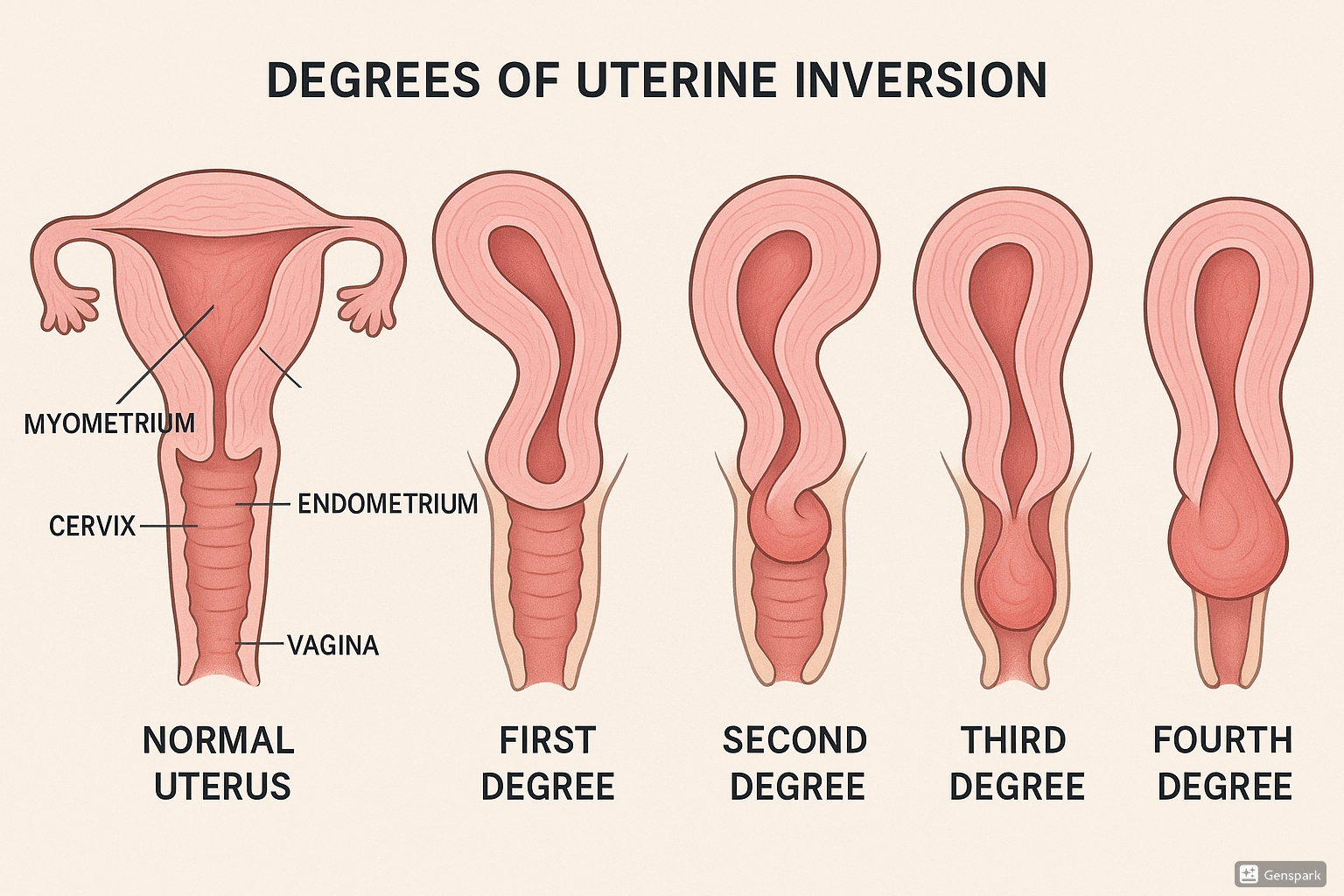
Classification & Grading of Uterine Inversion
Uterine inversion is classified according to both the timing of occurrence (temporal classification) and the degree or extent of the inversion (anatomical classification). Proper classification guides management decisions and helps in communicating the severity of the condition among healthcare providers.
Temporal Classification
| Classification | Timing | Clinical Significance |
|---|---|---|
| Acute | Within 24 hours after delivery | Most common form; true obstetric emergency requiring immediate intervention |
| Subacute | 24 hours to 4 weeks postpartum | Less common; may have delayed presentation but still requires urgent management |
| Chronic | More than 4 weeks after delivery | Rare; may present with chronic pelvic pain, abnormal bleeding, or discharge |
| Non-puerperal | Unrelated to pregnancy | Extremely rare; usually associated with tumors or masses distorting the uterus |
Anatomical Classification (Degrees of Inversion)
| Degree | Description | Clinical Features |
|---|---|---|
| First Degree (Incomplete) | Fundus inverts into the uterine cavity but remains above the internal cervical os | May be difficult to diagnose; often detected during bimanual examination |
| Second Degree (Complete) | Fundus passes through the cervical os into the vaginal canal | Fundus not palpable abdominally; mass felt in vaginal canal |
| Third Degree (Prolapsed) | Fundus extends to the vaginal introitus, visible at perineum | Visible mass at the vaginal opening; severe pain and shock |
| Fourth Degree (Total) | Complete inversion with vaginal walls included, entire uterus protrudes outside the body | Dramatic presentation with uterus and vagina completely exteriorized; extreme shock |
Clinical Relevance of Classification
- Prognostic Value: Higher degrees of inversion tend to correlate with more severe hemodynamic instability
- Management Approach: The degree of inversion guides the choice of reduction technique
- Time Sensitivity: Acute inversions are easier to reduce than subacute or chronic inversions
- Surgical Planning: More severe inversions may require advanced surgical interventions if manual reduction fails
Risk Factors for Uterine Inversion
While uterine inversion can occur unexpectedly in women with no identifiable risk factors, several conditions and practices are known to increase the likelihood of this complication. Understanding these risk factors helps healthcare providers identify patients who may benefit from preventive measures and vigilant monitoring.
Patient-Related Factors
Uterine Conditions
- Uterine atony or relaxation
- Uterine anomalies or congenital weakness
- Previous uterine surgery
- Multiparity with thinned uterine walls
- Adenomyosis
Placental Factors
- Fundal implantation of placenta
- Abnormal placental adherence (accreta, increta, percreta)
- Placenta previa
- Retained placenta
Connective Tissue Disorders
- Marfan syndrome
- Ehlers-Danlos syndrome
Labor and Delivery Factors
Management Practices (Modifiable)
- Excessive traction on the umbilical cord
- Fundal pressure (Credé maneuver) before placental separation
- Manual removal of placenta with excessive force
- Mismanagement of third stage of labor
- Use of uterine-relaxing agents
Labor Characteristics
- Prolonged labor causing uterine fatigue
- Rapid labor and delivery
- Precipitous delivery
- Short umbilical cord
- Fetal macrosomia with uterine overdistension
Previous History
- Prior uterine inversion
- Previous complicated third stage
- History of postpartum hemorrhage
Important Nursing Considerations
Despite the identified risk factors, it’s crucial to note that approximately 50% of uterine inversions occur in women with no recognizable risk factors. This highlights the importance of all obstetric nurses being prepared to identify and respond to this emergency regardless of a patient’s risk profile.
Risk Factor Assessment Tool
Nursing staff should consider documenting the following when assessing risk:
- Location of placental implantation (especially fundal attachment)
- Uterine tone assessment throughout labor
- Presence of connective tissue disorders
- Previous obstetric history, including third stage complications
- Fetal size and amniotic fluid volume
Clinical Presentation of Uterine Inversion
Recognizing the clinical presentation of uterine inversion is crucial for prompt diagnosis and management. The clinical manifestations vary based on the degree of inversion and the time elapsed since occurrence, but typically include several characteristic signs and symptoms that should trigger immediate action.
Cardinal Signs and Symptoms
| Clinical Feature | Description | Nursing Implications |
|---|---|---|
| Severe Lower Abdominal Pain | Sudden onset, excruciating pain described as tearing or ripping sensation in lower abdomen and pelvis | Distinguish from normal afterpains; assess pain quality and timing relative to delivery |
| Hemorrhage | Brisk, profuse vaginal bleeding that may be unresponsive to uterotonic agents | Quantify blood loss; prepare for fluid resuscitation; monitor vital signs closely |
| Absent Fundus | Inability to palpate uterine fundus on abdominal examination | Perform systematic abdominal palpation; document fundal height findings |
| Visible/Palpable Mass | Presence of a mass in the vagina or protruding through the introitus (in 3rd/4th degree inversion) | Avoid manipulation of visible mass; document appearance accurately |
| Hemodynamic Instability | Disproportionate shock relative to visible blood loss; includes hypotension, tachycardia, pallor, and diaphoresis | Monitor vital signs every 2-5 minutes; prepare for rapid fluid resuscitation; position for shock |
| Vagal Response | Bradycardia despite hypovolemia, due to parasympathetic stimulation from stretched pelvic ligaments | Anticipate need for atropine; monitor ECG; recognize this paradoxical response |
Presentation Based on Degree of Inversion
- May have minimal or no symptoms
- Subtle lower abdominal discomfort
- Uterus feels “different” on fundal palpation
- Depression or dimpling at fundus
- Often only detected during careful bimanual examination
- Moderate to severe pelvic pain
- Increased vaginal bleeding
- Fundus not palpable abdominally
- Mass felt within vaginal canal
- Early signs of hemodynamic instability
- Excruciating pain
- Significant hemorrhage
- Mass visible at vaginal introitus
- Pronounced hemodynamic instability
- Profound shock often present
- Dramatic presentation with exteriorized uterus
- Extreme pain if patient conscious
- Severe hemorrhagic and neurogenic shock
- Risk of tissue trauma and necrosis
- Life-threatening emergency
Red Flag Signs Requiring Immediate Action
- Sudden hemodynamic collapse shortly after delivery
- Failure to palpate uterine fundus after delivery
- Continuous heavy bleeding despite contracted uterus
- Appearance of a red, bleeding mass at the vaginal opening
- Severe pelvic pain with bearing-down sensation
- Bradycardia in the context of hypovolemia
Diagnosis of Uterine Inversion
Uterine inversion is primarily a clinical diagnosis that requires rapid recognition based on characteristic findings. Prompt identification is essential as delays in diagnosis can significantly increase morbidity and mortality.
Diagnostic Approaches
Primary Clinical Assessment
- Abdominal Examination: Absence of palpable uterine fundus or depression in the fundal area
- Vaginal Examination: Presence of a firm, round mass in the vagina or at the cervix
- Visual Inspection: In third or fourth degree inversion, direct visualization of reddish-purple mass at introitus
- Placental Assessment: Determine if placenta is still attached to the inverted fundus
Bimanual Examination Technique
A careful bimanual examination can confirm the diagnosis when the abdominal hand cannot palpate the fundus while the vaginal hand encounters a mass. This examination should be gentle to avoid worsening the inversion or increasing blood loss.
Supporting Diagnostic Methods
- Ultrasonography: May show absence of normal uterine fundus with a invagination or depression
- MRI: Rarely used in acute settings but helpful in diagnosing chronic or non-puerperal inversion
- Laboratory Tests: Not diagnostic but essential for management
- Complete blood count
- Coagulation profile
- Blood typing and crossmatching
- Basic metabolic panel
Important Note
Imaging studies should never delay emergency management when clinical diagnosis is clear. Treatment should be initiated immediately based on clinical findings.
Differential Diagnosis
Several conditions may present with symptoms similar to uterine inversion and should be considered in the diagnostic process:
| Differential Diagnosis | Distinguishing Features |
|---|---|
| Uterine Prolapse | Cervical os visible at the apex of the prolapsed tissue; uterine fundus still palpable abdominally |
| Retained Placenta | Fundus remains palpable; no mass in vagina except placental tissue; cervix may be visible around placental tissue |
| Fibroid Polyp | Usually smaller and more firm; fundus palpable abdominally; longer history of symptoms |
| Uterine Atony | Uterus palpable but soft/boggy; normal position of fundus; responds to massage and uterotonics |
| Cervical or Vaginal Tears | Bleeding may be present but fundus palpable; no mass in vagina; inspection reveals lacerations |
INVERTED Diagnostic Assessment Mnemonic
- I – Inspect for visible mass at vaginal introitus
- N – Note vital signs, especially signs of shock
- V – Verify absence of fundus on abdominal palpation
- E – Evaluate blood loss and hemodynamic stability
- R – Recognize pain disproportionate to visible findings
- T – Track onset relative to delivery and placental expulsion
- E – Examine carefully with bimanual technique
- D – Determine if placenta is still attached to inverted fundus
Management Approaches for Uterine Inversion
Management of uterine inversion requires a prompt, systematic approach focused on restoring normal uterine anatomy, managing shock, and preventing complications. The rapid implementation of appropriate interventions significantly impacts maternal outcomes.
Immediate Actions
- Call for emergency assistance (obstetric, anesthesia, and additional nursing support)
- Establish large-bore IV access (preferably two lines) for fluid resuscitation
- Begin rapid crystalloid infusion and prepare for blood product administration
- Monitor vital signs continuously
- Administer oxygen via face mask at 10-15 L/min
- Discontinue any oxytocin infusion immediately
- Position patient appropriately (lithotomy position if manual reduction will be attempted)
- Insert indwelling urinary catheter to monitor output
Management Decision Tree
Placenta Management
If placenta is still attached:
- Do NOT attempt to remove placenta before uterine replacement
- Placental removal before reduction may increase bleeding
- Replace uterus with placenta still attached when possible
- After uterine replacement, allow for spontaneous placental separation or careful manual removal
If placenta is already detached:
- Proceed directly to uterine replacement
- Be prepared for potential significant hemorrhage
Hemodynamic Status
If patient is hemodynamically stable:
- Attempt manual replacement first
- Consider uterine relaxants to facilitate reduction
- May have time for hydrostatic methods if manual fails
If patient is hemodynamically unstable:
- Simultaneous resuscitation and replacement attempts
- May need immediate surgical intervention
- Consider immediate transfer to operating room
- Prepare for possible blood transfusion
Reduction Techniques
Johnson’s Method:
- Place patient in lithotomy position
- Insert hand into vagina with palm toward inverted fundus
- Direct pressure upward toward umbilicus along axis of vagina
- Hold pressure steadily until reduction occurs
- Once reduced, maintain hand position until uterus contracts
First-line approach; most effective when performed immediately
O’Sullivan’s Method:
- Patient in lithotomy position with elevated hips
- Insert a large-volume douche system into posterior vagina
- Create water-tight seal at vaginal introitus with hands
- Infuse 2-3L warm sterile saline rapidly
- Hydrostatic pressure pushes fundus back into position
Second-line approach if manual reduction fails
Common Approaches:
- Huntington Procedure: Laparotomy with clamps on round ligaments to apply upward traction
- Haultain Procedure: Posterior uterine incision to release constriction ring, followed by manual replacement
- Laparoscopic-Assisted: Minimally invasive option in stable patients
Required when non-surgical methods fail or in subacute/chronic cases
Pharmacological Interventions
| Medication Type | Examples | Use | Considerations |
|---|---|---|---|
| Uterine Relaxants (to facilitate reduction) |
– Nitroglycerin (50-100 mcg IV) – Terbutaline (0.25 mg IV/SC) – Magnesium sulfate (4-6g IV over 20 min) – Halogenated anesthetics |
Administered before reduction attempts to relax uterine muscle and facilitate replacement | May worsen hypotension; use with caution in hemodynamically unstable patients |
| Uterotonics (after reduction) |
– Oxytocin (10-40 units IV infusion) – Methylergonovine (0.2mg IM) – Carboprost (250 mcg IM) – Misoprostol (800-1000 mcg rectal) |
Administered after successful reduction to contract uterus and prevent recurrence | Never give before reduction; start immediately after successful repositioning |
| Hemodynamic Support |
– Fluid resuscitation – Vasopressors (phenylephrine, ephedrine) – Atropine (for bradycardia) – Tranexamic acid (1g IV) |
Manage shock and maintain adequate perfusion during resuscitation | Consider balanced approach to fluid resuscitation; monitor for coagulopathy |
| Antibiotic Prophylaxis |
– Broad-spectrum antibiotics – Usually ampicillin + gentamicin or similar combination |
Prevent infection, especially after prolonged inversion or surgical reduction | Start early, particularly with prolonged manual manipulation or surgical intervention |
Post-Reduction Management
Post-Reduction Protocol
- Administer uterotonic agents immediately after successful reduction
- Maintain manual uterine compression for 3-5 minutes to ensure contraction
- Continue close monitoring of vital signs and uterine tone
- Assess for continued bleeding and respond appropriately
- Monitor fluid balance and maintain adequate urine output
- Consider ICU admission for 24 hours for unstable patients
- Continue thromboprophylaxis and antibiotic therapy as indicated
- Provide emotional support and clear communication to the patient and family
Keys to Successful Management
- Early Recognition: Prompt identification is the most crucial factor in successful management
- Team Approach: Coordinated effort between obstetric, anesthesia, and nursing staff
- Sequential Escalation: Progress logically through management options based on response
- Simultaneous Processes: Address hemodynamic stability while working toward uterine replacement
- Communication: Clear, calm communication among team members during the emergency
Nursing Care Plan for Uterine Inversion
Nursing care is fundamental in the management of uterine inversion, from early identification through emergency management and recovery. A structured care plan ensures comprehensive patient care throughout this obstetric emergency.
Nursing Assessment
| Assessment Parameter | Assessment Techniques | Critical Findings |
|---|---|---|
| Vital Signs |
– Continuous monitoring – Assess every 2-5 minutes during emergency – Document trends |
– Tachycardia or bradycardia – Hypotension – Decreased oxygen saturation – Tachypnea |
| Blood Loss |
– Quantify using calibrated drapes – Count saturated pads – Visual estimation |
– Blood loss >500mL in vaginal delivery – Continuous bleeding – Large clots |
| Uterine Assessment |
– Abdominal palpation – Visual inspection of perineum – Observe for fundal height |
– Absence of palpable fundus – Mass visible at introitus – Depression at fundal area |
| Pain Assessment |
– Standardized pain scale – Observe behavioral indicators – Patient self-reporting |
– Severe, acute abdominal pain – Bearing down sensation – Pain disproportionate to clinical situation |
| Perfusion Status |
– Capillary refill – Skin color and temperature – Level of consciousness |
– Delayed capillary refill (>3 seconds) – Pallor, diaphoresis – Altered mental status |
| Fluid Balance |
– Intake/output monitoring – Urinary catheter output – IV fluid administration records |
– Oliguria (<30mL/hr) – Fluid overload signs – Imbalanced I/O ratio |
Nursing Diagnoses
Risk for Deficient Fluid Volume
Related to: Excessive blood loss secondary to uterine inversion
Nursing Interventions:
- Establish and maintain large-bore IV access (preferably two lines)
- Administer fluid resuscitation as ordered (crystalloids and/or blood products)
- Monitor vital signs continuously, especially blood pressure and heart rate
- Accurately measure blood loss using calibrated drapes and weighing pads
- Monitor lab values (Hgb, Hct, coagulation studies)
- Position patient appropriately for shock management
Acute Pain
Related to: Tissue trauma from uterine inversion
Nursing Interventions:
- Assess pain using standardized scale and observe for nonverbal indicators
- Administer analgesics as ordered and assess effectiveness
- Provide emotional support during procedures
- Implement non-pharmacological pain management strategies when appropriate
- Document pain character, location, intensity, and response to interventions
- Prepare for pain management needs during and after reduction procedures
Decreased Cardiac Output
Related to: Hypovolemia and neurogenic shock
Nursing Interventions:
- Monitor ECG continuously and observe for arrhythmias
- Administer oxygen as ordered to improve tissue oxygenation
- Position patient to optimize cardiac output (supine with legs elevated)
- Administer medications to support blood pressure as ordered
- Monitor for signs of adequate tissue perfusion (capillary refill, urine output)
- Prepare for potential transfer to higher level of care
Anxiety
Related to: Emergency situation and perceived threat to health
Nursing Interventions:
- Provide clear, concise explanations about procedures and care
- Maintain calm, reassuring presence during emergency interventions
- Include support person when appropriate
- Use therapeutic communication techniques
- Assess need for pharmacological anxiety management
- Provide privacy and maintain dignity during interventions
Risk for Infection
Related to: Tissue trauma and invasive procedures
Nursing Interventions:
- Implement strict aseptic technique during all procedures
- Administer prophylactic antibiotics as ordered
- Monitor for signs of infection (temperature, pulse, pain, discharge)
- Ensure proper perineal care and hygiene
- Document characteristics of lochia
- Educate patient on signs of infection to report
Interrupted Breastfeeding
Related to: Maternal medical emergency
Nursing Interventions:
- Assess mother’s desire and ability to breastfeed
- Coordinate with lactation specialist for support
- Assist with breast pump if direct breastfeeding is not possible
- Educate about medication effects on breastfeeding
- Support skin-to-skin contact when mother is stable
- Facilitate breastfeeding as soon as maternal condition permits
Emergency Nursing Interventions
URGENT Care Mnemonic for Uterine Inversion
- U – Understand the emergency and activate rapid response team
- R – Resuscitate with IV fluids and blood products as needed
- G – Gather equipment and medications for reduction attempts
- E – Evaluate vital signs and monitor continuously
- N – Notify appropriate providers (obstetrics, anesthesia)
- T – Treat pain and anxiety appropriately
- C – Communicate clearly with patient and healthcare team
- A – Anticipate needs for surgical intervention
- R – Restore normal uterine position through appropriate techniques
- E – Ensure post-reduction monitoring and uterine contraction
Post-Reduction Nursing Care
- Monitor vital signs every 15 minutes for 2 hours, then every 30 minutes for 2 hours
- Continue IV fluid management as ordered
- Assess for continued signs of hemorrhage
- Monitor urine output hourly until stable
- Assess laboratory values as ordered
- Perform fundal checks every 15 minutes for first 2 hours
- Assess uterine tone and location
- Monitor lochia amount, color, and consistency
- Administer uterotonic medications as ordered
- Document fundal height and position
- Assess pain using standardized scale
- Administer analgesics as ordered
- Monitor effectiveness of pain interventions
- Implement non-pharmacological comfort measures
- Document pain characteristics and response to therapy
- Monitor temperature every 4 hours
- Administer antibiotics as ordered
- Ensure proper perineal hygiene
- Assess for signs of infection
- Document wound appearance if surgical intervention occurred
- Assess emotional status regularly
- Provide clear explanation of events
- Encourage expression of feelings
- Include support persons in care
- Consider referral to mental health services
- Screen for trauma symptoms
- Educate about warning signs requiring medical attention
- Provide verbal and written instructions
- Arrange appropriate follow-up appointments
- Discuss contraception and future pregnancy planning
- Connect to community resources if needed
Documentation Guidelines
Essential Documentation Elements
- Timing: Precise time of inversion identification, interventions, and reduction
- Assessment Findings: Detailed description of uterine inversion presentation
- Vital Signs: Sequential recordings throughout emergency and recovery
- Blood Loss: Quantitative measurement when possible
- Interventions: Detailed listing of all management techniques used
- Medications: All medications administered with doses, routes, times, and responses
- Team Members: Names of all healthcare providers involved
- Patient Response: Detailed description of patient’s condition after interventions
Complications of Uterine Inversion
Despite proper management, uterine inversion may lead to several serious complications. Understanding potential sequelae allows nurses to monitor for early warning signs and participate in prevention strategies.
Immediate Complications
Hemorrhagic Shock
Significant blood loss from inverted uterine surface and inability of uterus to contract properly can lead to severe hemorrhage and hypovolemic shock.
Nursing Implications:
- Vigilant monitoring of vital signs and perfusion
- Preparation for massive transfusion protocol
- Administration of fluid resuscitation and vasopressors
Neurogenic Shock
Parasympathetic stimulation from stretching of pelvic tissues and ligaments can cause bradycardia and hypotension disproportionate to blood loss.
Nursing Implications:
- Recognition of paradoxical bradycardia
- Preparation for atropine administration
- Management of both neurogenic and hypovolemic components
Acute Kidney Injury
Renal hypoperfusion secondary to shock can lead to acute tubular necrosis and kidney injury.
Nursing Implications:
- Close monitoring of urine output (goal >30 mL/hr)
- Tracking of fluid balance
- Monitoring BUN, creatinine, and electrolytes
Delayed Complications
Recurrent Uterine Inversion
Potential for recurrence of inversion in the immediate postpartum period if uterine tone remains poor.
Nursing Implications:
- Continued fundal assessment after initial reduction
- Ensuring adequate uterotonic medication administration
- Education on signs of recurrence
Puerperal Infection
Endometritis, myometritis, or parametritis may develop due to tissue damage and manipulation during reduction.
Nursing Implications:
- Monitoring for fever, abnormal lochia, and uterine tenderness
- Administration of prophylactic antibiotics
- Teaching infection prevention practices
Psychological Trauma
PTSD, postpartum depression, or anxiety related to the traumatic birth experience.
Nursing Implications:
- Screening for psychological symptoms
- Providing emotional support and debriefing
- Referral to mental health services when needed
- Including supportive persons in care planning
Long-Term Sequelae
| Complication | Description | Nursing Considerations |
|---|---|---|
| Sheehan’s Syndrome | Pituitary infarction due to severe hypotension, leading to panhypopituitarism | Monitor for signs of endocrine dysfunction (failure to lactate, amenorrhea, fatigue); facilitate endocrinology follow-up |
| Uterine Scarring | Formation of intrauterine adhesions or scarring, particularly after surgical reduction | Educate about potential impact on future fertility; ensure gynecological follow-up |
| Secondary Infertility | Difficulty conceiving due to uterine damage or sequelae of management | Provide information about fertility resources; offer compassionate counseling |
| Recurrence in Future Pregnancies | Increased risk of recurrent uterine inversion in subsequent deliveries | Educate about importance of prenatal care and delivery planning for future pregnancies |
| Chronic Pelvic Pain | Persistent pain related to tissue damage or surgical interventions | Assess pain management strategies; refer to pain specialist if persistent |
Mortality Risk
Historically, maternal mortality from uterine inversion was as high as 15%. With modern obstetric and resuscitative practices, mortality has decreased significantly to less than 1% in developed countries. However, delayed diagnosis and management still carry substantial mortality risk, primarily from hemorrhagic shock and its sequelae.
Key factors that influence mortality include:
- Time to diagnosis and initiation of treatment
- Availability of blood products for transfusion
- Access to surgical intervention when needed
- Pre-existing maternal health conditions
- Level of healthcare provider experience with this rare condition
Prevention Strategies for Uterine Inversion
While uterine inversion cannot always be predicted or prevented, several evidence-based practices can significantly reduce the risk. Nursing awareness and implementation of these strategies play a crucial role in prevention.
Active Management of Third Stage of Labor (AMTSL)
Core AMTSL Components
Evidence shows that proper active management of the third stage has reduced the incidence of uterine inversion fourfold:
- Prophylactic Uterotonic Administration: Oxytocin (10 IU IM/IV) after delivery of anterior shoulder or immediately after delivery of the infant
- Delayed Cord Clamping: Wait 1-3 minutes before clamping and cutting the umbilical cord
- Controlled Cord Traction: Apply gentle traction only with a contracted uterus while providing counter-traction abdominally
- Uterine Massage: After placenta delivery, massage uterus through abdomen until contracted
Best Practice Guidelines
Practices to Implement
- Administer uterotonics prophylactically after delivery of the anterior shoulder or baby
- Ensure placental separation before applying cord traction
- Use gentle controlled cord traction with counter-pressure on the uterus
- Maintain vigilance during the third stage, especially with high-risk patients
- Provide proper education and training for all delivery attendants
- Document placental location during prenatal ultrasounds
- Perform routine fundal assessment after delivery
- Recognize and manage uterine atony promptly
Practices to Avoid
- Excessive traction on umbilical cord before placental separation
- Fundal pressure (Credé maneuver) to hasten placental delivery
- Vigorous or forceful manual extraction of placenta
- Pulling on cord when uterus is not contracted
- Mismanagement of abnormal placentation
- Unyielding pressure on the uterine fundus
- Aggressive fundal manipulation during placental delivery
High-Risk Patient Management
| Risk Factor | Preventive Strategies |
|---|---|
| Fundal Placenta |
– Document placental location from ultrasound – Exercise extra caution during placental delivery – Consider allowing spontaneous placental separation without traction – Ensure uterine contraction before any placental manipulation |
| Connective Tissue Disorders |
– Document in birth plan – Consider prophylactic measures for third stage – Vigilant monitoring during third stage – Early and prolonged oxytocin administration |
| Previous Uterine Inversion |
– Document history prominently in chart – Consider managed third stage by experienced provider – Prophylactic uterotonics – Extended observation during third stage and immediate postpartum period |
| Uterine Anomalies |
– Prenatal documentation of any anomalies – Consider ultrasound guidance during third stage – Cautious management of placental delivery – Prepare team for possible complications |
| Prolonged Labor |
– Recognize risk of uterine fatigue – Early prophylactic uterotonics – Avoid excessive fundal pressure – Allow adequate time for uterine recovery before placental manipulation |
Interprofessional Team Readiness
Team Preparation Strategies
- Regular Simulation Drills: Practice emergency response to uterine inversion scenarios
- Protocol Development: Establish clear, facility-specific protocols for management
- Equipment Readiness: Ensure immediate availability of emergency supplies and medications
- Communication Systems: Develop efficient emergency notification processes
- Staff Education: Regular updates on recognition and management of rare obstetric emergencies
- Debriefing Sessions: Review cases of uterine inversion for quality improvement
PREVENT Uterine Inversion Mnemonic
- P – Patience during third stage; avoid rushing placental delivery
- R – Recognize risk factors in prenatal period
- E – Ensure uterine contraction before cord traction
- V – Verify placental separation before traction
- E – Evaluate fundal height regularly during third stage
- N – Never apply excessive cord traction or fundal pressure
- T – Timely administration of prophylactic uterotonics
Mnemonics & Memory Aids
Mnemonics and memory aids can help nursing students quickly recall important information about uterine inversion during clinical practice and examinations. These learning tools enhance retention of critical concepts related to this rare obstetric emergency.
INVERSION: Signs & Symptoms
- I – Intense pain in lower abdomen
- N – No fundus palpable abdominally
- V – Vaginal mass visible or palpable
- E – Extreme hemorrhage
- R – Rapid deterioration of vital signs
- S – Shock disproportionate to visible blood loss
- I – Immediate postpartum occurrence (typically)
- O – Obvious distress in patient
- N – Neurogenic shock symptoms (bradycardia)
UTERUS: Emergency Management
- U – Urgently call for help
- T – Tocolytic medications to relax uterus
- E – Establish IV access (large-bore)
- R – Replace uterus manually or with hydrostatic methods
- U – Uterotonics after reduction (not before)
- S – Stabilize hemodynamics with fluids/blood products
FUNDAL: Risk Factors
- F – Fundal placental implantation
- U – Uterine anomalies or weakness
- N – Non-contracted uterus during third stage
- D – Downward traction on umbilical cord
- A – Abnormal placentation (accreta)
- L – Long labor causing uterine fatigue
SHOCK: Complication Assessment
- S – Severe hemorrhage
- H – Hypotension and tachycardia (or bradycardia)
- O – Oxygen saturation decreased
- C – Cold, clammy skin
- K – Knowledge of both hypovolemic and neurogenic components
Degrees of Inversion Memory Aid
Remember the 4 Degrees with “ICPT” (Inside, Cervix, Perineum, Total):
1st Degree: Inside
Fundus inverts but stays inside the uterine cavity
2nd Degree: Cervix
Fundus passes through the cervix into vagina
3rd Degree: Perineum
Fundus reaches the perineum/introitus
4th Degree: Total
Total inversion with uterus and vagina outside body
Visual Memory Framework for Management
The “3R” Approach to Uterine Inversion
Recognize
- Absent fundus
- Vaginal mass
- Hemorrhage
- Shock
Resuscitate
- IV fluids
- Blood products
- Oxygen
- Treat shock
Replace
- Relax uterus
- Manual reduction
- Hydrostatic method
- Surgical approach
Self-Assessment Questions
Test your knowledge of uterine inversion with these practice questions designed to reinforce key concepts and clinical decision-making.
1. A nurse is assessing a patient who has just delivered a healthy newborn. The patient suddenly complains of severe pelvic pain, and the nurse notices significant bleeding. On abdominal palpation, the uterine fundus cannot be felt. What is the most likely diagnosis?
Answer: B. Uterine inversion
Explanation: The inability to palpate the uterine fundus abdominally, combined with severe pelvic pain and hemorrhage immediately after delivery, is characteristic of uterine inversion. Uterine rupture typically presents with pain and bleeding but would not have an absent fundus. Retained placenta would show a palpable but enlarged uterus. Uterine atony presents with a soft, boggy uterus that is palpable abdominally.
2. Which of the following is an appropriate initial nursing intervention when uterine inversion is suspected?
Answer: C. Activate emergency response and call for assistance
Explanation: The first appropriate intervention when uterine inversion is suspected is to activate the emergency response system and call for assistance. Administering oxytocin would worsen the condition by causing the uterus to contract around the inversion. Applying fundal pressure could exacerbate the inversion. Manual removal of the placenta before repositioning the uterus may increase bleeding.
3. A nurse is caring for a patient with a third-degree uterine inversion. The patient’s vital signs show a blood pressure of 80/40 mmHg and heart rate of 58 beats per minute. This combination of hypotension and bradycardia is most likely due to:
Answer: B. Neurogenic shock from parasympathetic response
Explanation: The paradoxical combination of hypotension with bradycardia (rather than tachycardia) is characteristic of neurogenic shock from a parasympathetic response. This occurs due to stretching of the pelvic tissues and ligaments during uterine inversion. The other shock states typically present with tachycardia alongside hypotension.
4. After successful manual reduction of a uterine inversion, which medication should the nurse anticipate administering immediately?
Answer: C. Oxytocin
Explanation: Immediately after successful reduction of a uterine inversion, uterotonic agents such as oxytocin should be administered to promote uterine contraction, control bleeding, and prevent recurrence of the inversion. Magnesium sulfate, terbutaline, and nifedipine are tocolytics that relax the uterus and would be used before reduction attempts, not after.
5. Which nursing intervention should be avoided in a patient with suspected uterine inversion?
Answer: C. Applying traction on the umbilical cord
Explanation: Applying traction on the umbilical cord should be avoided as it can cause or worsen uterine inversion. Establishing IV access, administering oxygen, and continuous vital sign monitoring are all appropriate interventions for a patient with suspected uterine inversion.
References
The following resources were used in the development of this comprehensive guide on uterine inversion:
- Wendel, M.P., Shnaekel, K.L., & Magann, E.F. (2018). Uterine inversion: A review of a life-threatening obstetrical emergency. Obstetrical & Gynecological Survey, 73(7), 411-417.
- Coad, S.L., Dahlgren, L.S., & Hutcheon, J.A. (2017). Risks and consequences of puerperal uterine inversion in the United States, 2004 through 2013. American Journal of Obstetrics and Gynecology, 217(3), 377.e1-377.e6.
- Pararajasingam, S.S., Tsen, L.C., & Onwochei, D.N. (2024). Uterine inversion. BJA Education, 24(5), 173-178.
- Baskett, T.F. (2002). Acute uterine inversion: A review of 40 cases. Journal of Obstetrics and Gynaecology Canada, 24(12), 953-956.
- Hostetler, D.R., & Bosworth, M.F. (2000). Uterine inversion: A life-threatening obstetric emergency. The Journal of the American Board of Family Practice, 13(2), 120-123.
- Bhalla, R., Wuntakal, R., Odejinmi, F., & Khan, R.U. (2009). An acute inversion of the uterus. The Obstetrician & Gynaecologist, 11, 13-18.
- Long, L., & Penna, L. (2017). Maternal collapse. Obstetrics, Gynaecology & Reproductive Medicine, 28(2), 46-52.
- Beringer, R.M., & Patteril, M. (2004). Puerperal uterine inversion and shock. British Journal of Anaesthesia, 92(3), 439-441.
- Brar, H.S., Greenspoon, J.S., Platt, J.D., & Paul, R.H. (1989). Acute puerperal uterine inversion. New approaches to management. Journal of Reproductive Medicine, 34(3), 173-177.
- MMBRACE-UK. (2020). Saving lives, improving mothers’ care. Lessons learned to inform maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2016-2018. Maternal, Newborn and Infant Clinical Outcome Review Programme.
- Burns, R., & Dent, K. (2022). Managing medical and obstetric emergencies and trauma: a practical approach. John Wiley & Sons Ltd, London, 829-837.
- Bienstock, J.L., Eke, A.C., & Hueppchen, N. (2021). Postpartum haemorrhage. New England Journal of Medicine, 383, 1635-1645.
- Drew, T., & Carvalho, J.C.A. (2022). Major obstetric haemorrhage. British Journal of Anaesthesia Education, 22, 238-244.
