Vasa Previa
Comprehensive Guide for Nursing Students
Table of Contents
Introduction
Vasa previa is a rare but serious obstetric complication with potentially devastating consequences if not detected and managed properly. As future nursing professionals, understanding vasa previa is crucial for providing optimal care for at-risk patients and participating effectively in the multidisciplinary care team.
This condition occurs when fetal blood vessels, unprotected by the umbilical cord or placental tissue, run through the fetal membranes and cross over or are in close proximity to the internal cervical os. These exposed vessels are at risk of rupture during labor, which can lead to rapid fetal exsanguination and death if not promptly addressed.
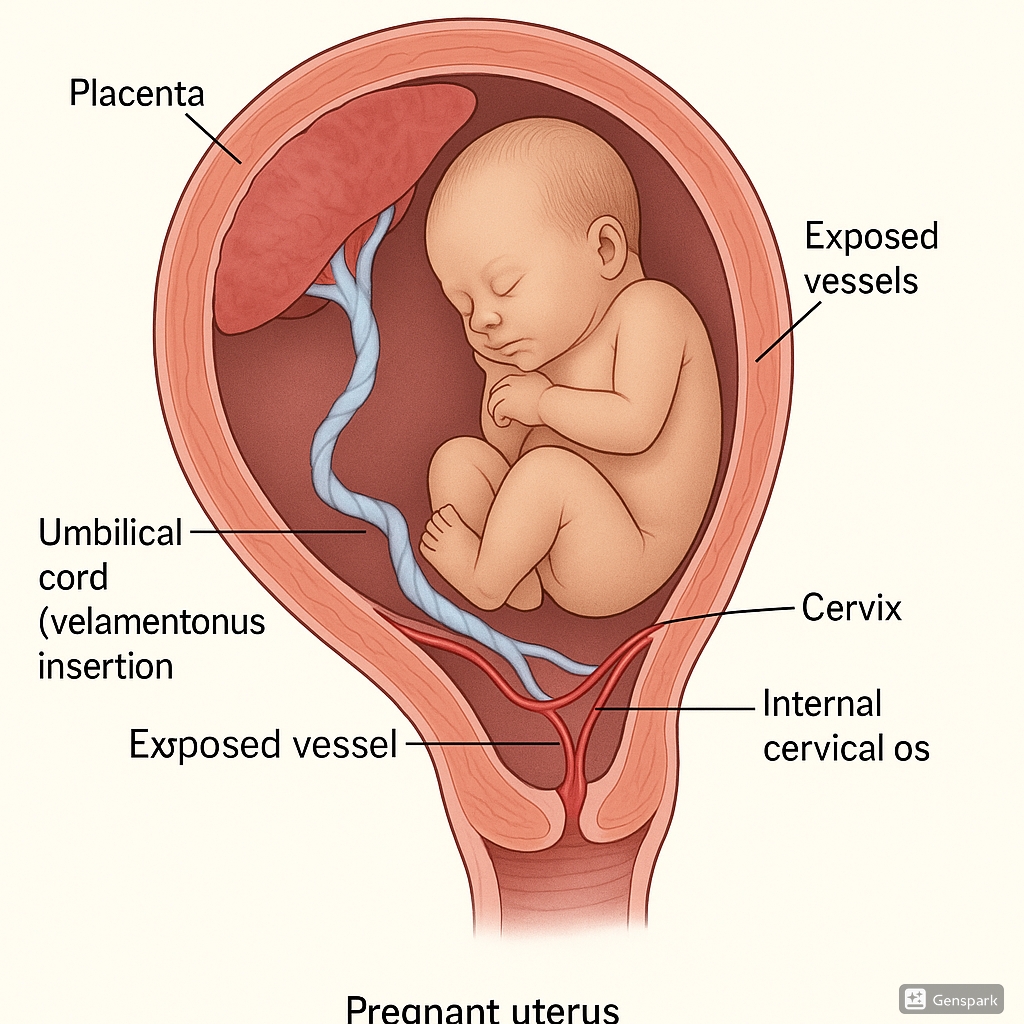
Fig. 1: Anatomical illustration of vasa previa showing exposed fetal vessels crossing the cervical os.
Definition & Pathophysiology
Definition
Vasa previa is defined as the presence of unprotected fetal blood vessels running through the fetal membranes (amnion and chorion) and crossing over or in close proximity (within 2 cm) to the internal cervical os.
Pathophysiology
Vasa previa develops due to abnormal placentation and umbilical cord insertion. The condition is typically associated with one of two primary anatomical variations:
- Velamentous cord insertion: Instead of inserting directly into the placenta, the umbilical cord inserts into the fetal membranes, leaving vessels unprotected as they travel through the membranes to reach the placenta.
- Placental morphological abnormalities: Including bilobed placenta, succenturiate lobes, or multilobed placenta where vessels connect separate placental lobes by traversing through the membranes.
In normal placentation, the umbilical cord inserts directly into the placenta with vessels protected by Wharton’s jelly. In vasa previa, the vessels lack this protective covering, making them vulnerable to compression, rupture, and subsequent hemorrhage.
Memory Aid: “VEIN”
Velamentous insertion → vessels traverse through membranes
Exposed vessels without Wharton’s jelly protection
Internal os proximity increases risk
Nonprotected fetal blood supply
Epidemiology & Risk Factors
Prevalence
Vasa previa is a relatively rare condition, with reported prevalence ranging from approximately:
- 1 in 2,000 to 1 in 6,000 pregnancies in the general population
- However, incidence rises to approximately 1 in 300 pregnancies conceived through in vitro fertilization (IVF)
Risk Factors
| Risk Factor | Description | Relative Risk |
|---|---|---|
| In Vitro Fertilization (IVF) | Assisted reproductive technology increases risk significantly | High |
| Placental Abnormalities | Bilobed or succenturiate lobe placenta | High |
| Velamentous Cord Insertion | Umbilical cord inserts into membranes rather than placenta | High |
| Low-lying Placenta | Placenta positioned close to cervical os in second trimester | Moderate |
| Placenta Previa | Placenta covering internal os | Moderate |
| Multiple Gestations | Twin or higher-order pregnancies | Moderate |
| Previous Uterine Surgery | Including cesarean sections, D&C, myomectomy | Lower |
Memory Aid: “VIPP MLT”
Velamentous cord insertion
In vitro fertilization
Placental abnormalities (bilobed, succenturiate)
Placenta previa history
Multiple gestations
Low-lying placenta
Traumatic uterine procedures
Classification of Vasa Previa
Vasa previa can be classified into different types based on the underlying anatomical abnormalities:
| Type | Description | Associated Features |
|---|---|---|
| Type I | Vessels running between velamentous cord insertion and placenta | Associated with velamentous cord insertion |
| Type II | Vessels connecting lobes of bilobed or succenturiate lobe placenta | Associated with placental morphological abnormalities |
| Type III (Emerging classification) | Vessels present without velamentous insertion or abnormal placenta | May have central cord insertion with aberrant vessels on membranes |
Clinical Pearl
While most vasa previa cases are associated with either velamentous cord insertion or placental abnormalities, recent literature describes Type III cases where neither is present, but vessels still traverse the membranes near the cervical os.
Clinical Presentation
The clinical presentation of vasa previa varies depending on whether it is diagnosed antenatally or presents during labor.
Asymptomatic (Antenatal)
Most cases of vasa previa are asymptomatic during pregnancy and are identified through routine ultrasound screening or targeted assessment due to risk factors.
Symptomatic (During Labor)
When vasa previa is undiagnosed before labor, clinical presentation may include:
- Painless vaginal bleeding – Typically occurs after rupture of membranes or during labor due to vessel rupture
- Rapid fetal heart rate abnormalities – Including variable or prolonged decelerations, bradycardia, or sinusoidal pattern
- Signs of fetal distress – Disproportionate to the amount of visible bleeding
- Fetal shock and anemia – Due to acute blood loss
Warning Signs
The amount of visible vaginal bleeding may appear minimal despite significant fetal blood loss. This is a critical point for nursing assessment – fetal distress disproportionate to visible maternal bleeding should raise immediate concern for vasa previa.
Diagnostic Approaches
Antenatal Diagnosis
Prenatal diagnosis of vasa previa is crucial for improving outcomes. Current expert consensus recommends screening all pregnancies at the mid-trimester (18-24 weeks) anatomy scan.
Ultrasound Modalities
| Diagnostic Method | Description | Value |
|---|---|---|
| Transvaginal Ultrasound | Gold standard; allows direct visualization of vessels over cervix | Primary Method |
| Color Doppler Imaging | Visualizes blood flow in vessels crossing over cervix | Essential Component |
| Pulsed Wave Doppler | Confirms fetal origin by showing fetal heart rate pattern | Confirmatory |
| 3D Ultrasound | Provides spatial relationship between vessels and cervix | Adjunctive |
| MRI | Used in unclear cases or for enhanced visualization | Secondary |
Ultrasound Diagnostic Criteria
- Visualization of vessels crossing over or within 2 cm of the internal cervical os
- Vessels running through membranes rather than within placental tissue or umbilical cord
- Color Doppler confirmation of blood flow
- Pulsed Doppler showing blood flow rate consistent with fetal heart rate
Intrapartum Diagnosis
When vasa previa is suspected during labor due to vaginal bleeding and fetal distress, several tests can confirm the fetal origin of blood:
| Test | Description | Time Required |
|---|---|---|
| Apt Test (Alkali Denaturation Test) |
Distinguishes fetal from maternal hemoglobin based on resistance to alkali denaturation. Fetal hemoglobin remains pink while maternal hemoglobin turns brownish-yellow. | 2-5 minutes |
| Ogita Test | Modified alkali denaturation test with improved sensitivity and specificity | 2-5 minutes |
| Kleihauer-Betke Test | Detects fetal hemoglobin-containing cells in maternal blood | 30-60 minutes |
| Hemoglobin Electrophoresis | Separates fetal from adult hemoglobin | ~60 minutes |
Memory Aid: “PACT for Vasa Previa”
Pink remains in fetal blood (Apt test)
Alkali denaturation differentiates blood source
Color Doppler confirms vessel location
Transvaginal ultrasound is the gold standard
Clinical Pearl
While diagnostic tests can confirm vasa previa, in most intrapartum cases with suspected fetal bleeding, immediate emergency cesarean delivery should not be delayed for test results if significant fetal heart rate abnormalities are present.
Management & Treatment
Management of vasa previa differs significantly based on whether it is diagnosed antenatally or presents during labor as an emergency. The primary goal is to prevent vessel rupture and fetal exsanguination.
Antenatal Management
- Serial ultrasound monitoring – To confirm persistence of vasa previa and assess fetal growth
- Patient education – About the condition, warning signs, and management plan
- Activity modification – Pelvic rest (no sexual intercourse) and limited physical activity
- Antenatal corticosteroids – Between 28-32 weeks to promote fetal lung maturity
-
Hospitalization – Current guidelines recommend:
- Consideration of hospitalization between 30-34 weeks
- Individualized timing based on risk factors and access to healthcare
- Fetal monitoring – Regular non-stress tests and biophysical profiles during hospitalization
-
Planned cesarean delivery – Current guidelines recommend:
- Delivery at 34-36 weeks for uncomplicated cases
- Earlier delivery if signs of labor, bleeding, or fetal compromise
Intrapartum Management (Emergency)
When vasa previa is diagnosed during labor or with rupture of membranes:
- Emergency cesarean delivery – Immediate delivery is indicated
- Rapid IV access – Two large-bore IV lines for potential resuscitation
- Blood products – Preparation of O-negative blood for potential neonatal transfusion
- Neonatal resuscitation team – Advanced preparation for potential neonatal compromise
Emerging Treatment Options
Recent advancements in management include:
- Fetoscopic laser ablation – In select cases, laser treatment of vessels crossing the cervical os has been performed to potentially allow vaginal delivery
- Expectant management with close surveillance – For cases diagnosed after 35 weeks with planned immediate cesarean delivery at onset of labor
Critical Management Point
Vaginal examination should be avoided in known or suspected cases of vasa previa, as it may disrupt the fetal vessels. Digital examinations should be performed only in controlled settings with immediate cesarean delivery capability.
Nursing Care Plans
Comprehensive nursing care for patients with vasa previa focuses on vigilant monitoring, patient education, and preparation for potential emergencies.
Nursing Diagnoses
| Nursing Diagnosis | Related Factors |
|---|---|
| Risk for Fetal Bleeding | Exposed fetal vessels, potential vessel rupture |
| Anxiety | High-risk pregnancy, prolonged hospitalization |
| Risk for Ineffective Coping | Extended hospitalization, activity limitations |
| Deficient Knowledge | Unfamiliarity with condition and management plan |
| Risk for Impaired Family Processes | Hospitalization separation, concern for pregnancy outcome |
Nursing Interventions
| Phase | Nursing Interventions | Rationale |
|---|---|---|
| Antepartum | Provide comprehensive patient education about vasa previa, including warning signs of bleeding or labor | Promotes early recognition of complications and improves compliance with care plan |
| Perform regular electronic fetal monitoring (daily or twice daily NSTs) | Detects early signs of fetal compromise | |
| Implement activity restrictions and enforce pelvic rest | Minimizes risk of vessel rupture and premature labor | |
| Administer antenatal corticosteroids as prescribed | Promotes fetal lung maturity prior to planned preterm delivery | |
| Intrapartum (Emergency) | Establish large-bore IV access (preferably two lines) | Provides route for rapid fluid or blood administration |
| Apply continuous electronic fetal monitoring | Allows prompt detection of fetal distress | |
| Avoid vaginal examinations unless in OR with immediate cesarean capability | Prevents iatrogenic vessel rupture | |
| Collect blood samples for Apt test or other fetal hemoglobin tests if bleeding occurs | Helps distinguish fetal from maternal bleeding | |
| Prepare for emergency cesarean delivery | Facilitates rapid intervention to prevent fetal death | |
| Postpartum | Monitor for postpartum hemorrhage | Risk may be increased with placental anomalies |
| Support mother-infant bonding, especially with NICU admission | Promotes parental attachment when separation occurs | |
| Provide emotional support and referrals for psychological services if needed | Addresses potential trauma from high-risk pregnancy and delivery |
Documentation
Thorough nursing documentation should include:
- Electronic fetal monitoring results with interpretation
- Assessment of vaginal bleeding (if present) – amount, color, presence of clots
- Patient’s understanding of condition and compliance with activity restrictions
- Response to corticosteroids and other medications
- Emotional status and coping mechanisms
Patient Education
Key Teaching Points for Patients with Vasa Previa
- Explanation of condition in clear, non-technical language
- Importance of activity restrictions and pelvic rest
- Warning signs requiring immediate medical attention:
- Any vaginal bleeding
- Rupture of membranes
- Regular uterine contractions
- Decreased fetal movement
- Rationale for hospitalization and planned cesarean delivery
- Potential need for NICU care if delivered preterm
Complications
Vasa previa carries significant risks for both maternal and fetal complications, particularly when undiagnosed before labor.
Fetal/Neonatal Complications
| Complication | Description | Incidence |
|---|---|---|
| Fetal Exsanguination | Rapid blood loss through ruptured vessels | High in undiagnosed cases with vessel rupture |
| Fetal/Neonatal Death | Due to hemorrhage and hypovolemic shock | ~56% if undiagnosed; <3% with prenatal diagnosis |
| Severe Anemia | Even with successful delivery after bleeding | Common with vessel rupture |
| Prematurity-related Complications | Due to planned early delivery | Variable, based on gestational age at delivery |
| Hypoxic-Ischemic Encephalopathy | Secondary to acute blood loss and hypoxia | Possible in cases with significant bleeding |
Maternal Complications
While vasa previa primarily affects fetal outcomes, several maternal complications can occur:
- Psychological distress – Anxiety, depression related to high-risk pregnancy status
- Prolonged hospitalization – Physical and emotional effects
- Surgical complications – Related to cesarean delivery
- Postpartum hemorrhage – May be increased with placental abnormalities
- Post-traumatic stress disorder – Particularly after emergency situations
Memory Aid: “BLEED”
Blood loss (fetal exsanguination)
Life-threatening emergency (requires immediate delivery)
Early delivery complications (prematurity)
Emotional impact (maternal psychological effects)
Death risk dramatically reduced with prenatal diagnosis
Prevention Strategies
While vasa previa itself cannot be prevented, adverse outcomes can be significantly reduced through early identification and appropriate management.
Primary Prevention
Targets risk reduction and early detection:
-
Universal ultrasound screening at 18-24 weeks
- Assessment of placental cord insertion
- Evaluation of placental morphology
- Color Doppler assessment of cervical area
-
Targeted screening for high-risk groups
- IVF pregnancies
- Multiple gestations
- Second-trimester low-lying placenta or placenta previa
- Previous uterine surgery
Secondary Prevention
Focuses on preventing complications once vasa previa is diagnosed:
- Follow-up ultrasound assessments – To confirm persistence or resolution of vasa previa
- Activity modification and pelvic rest – To reduce risk of premature labor or vessel rupture
- Hospitalization at appropriate gestational age – For close monitoring
- Planned cesarean delivery – Before onset of labor
- Avoidance of vaginal examinations – To prevent vessel disruption
Clinical Pearl
The mortality rate for undiagnosed vasa previa is approximately 56%, while prenatal diagnosis with planned management reduces this to less than 3%. This dramatic improvement underscores the critical importance of prenatal screening and proper management.
Best Practices & Recent Updates
Current Best Practices
Recent guidelines from professional organizations and expert consensus statements have established the following best practices:
Best Practice #1: Universal Screening
Expert consensus now recommends that all pregnancies should be screened for vasa previa at the second-trimester anatomy scan (18-24 weeks) by identifying placental cord insertion and using color Doppler over the cervix.
Best Practice #2: Individualized Hospitalization Timing
Current guidelines support a more nuanced approach to hospitalization timing. While most authorities recommend admission between 30-34 weeks, the exact timing should be individualized based on risk factors, distance from a tertiary care center, and patient circumstances.
Best Practice #3: Optimized Delivery Timing
Expert consensus from 2025 suggests that the optimal timing for planned cesarean delivery in uncomplicated vasa previa cases is between 34 weeks and 35 weeks 6 days. This timing balances the risks of prematurity with the risks of emergency delivery due to spontaneous labor.
Recent Updates (2023-2025)
-
Expanded Classification System
The recognition of Type III vasa previa (occurring without velamentous insertion or abnormal placental morphology) has expanded our understanding of the condition’s pathophysiology.
-
Emerging Interventional Approaches
Limited case reports have described successful fetoscopic laser ablation of vasa previa vessels, potentially allowing vaginal delivery in select cases. This remains experimental and is not standard practice.
-
Refined Risk Assessment
Research has identified specific ultrasound markers that may predict resolution or persistence of vasa previa identified in the second trimester, allowing more tailored management approaches.
Areas of Ongoing Research
- Optimal timing of delivery based on individualized risk factors
- Cost-effectiveness of universal screening versus targeted high-risk screening
- Development of predictive models for vasa previa resolution
- Role of cell-free fetal DNA testing in diagnosing vasa previa rupture
- Long-term outcomes of children born after vasa previa
Case Studies
Case Study 1: Prenatal Diagnosis and Management
Patient Profile: 33-year-old G2P1, conceived through IVF
Presentation: Routine 20-week anatomy scan showed a succenturiate lobe placenta with vessels crossing near the cervical os.
Management:
- Confirmation with transvaginal ultrasound and color Doppler at 24 weeks
- Patient education about condition and warning signs
- Activity restrictions and pelvic rest advised
- Antenatal corticosteroids at 28 weeks
- Hospitalization at 32 weeks for continuous monitoring
- Planned cesarean delivery at 34 weeks 2 days
Outcome:
- Healthy female infant delivered, weight 2180g
- Brief NICU stay for respiratory support (4 days)
- Mother and baby discharged on day 6 without complications
Learning Points:
- Early detection allows for planned management
- IVF pregnancy emphasized as risk factor
- Systematic approach significantly improved outcome
Case Study 2: Emergency Presentation
Patient Profile: 27-year-old G1P0 at 32 weeks gestation with no prior complications
Presentation: Presented to labor and delivery with sudden painless vaginal bleeding after spontaneous rupture of membranes.
Clinical Course:
- Initial examination showed minimal bleeding but severe fetal bradycardia (FHR 70s)
- Rapid clinical assessment suspected vasa previa
- Emergency cesarean delivery performed within 10 minutes of arrival
- Apt test later confirmed fetal hemoglobin in vaginal blood
- Placental examination revealed velamentous cord insertion
Outcome:
- Male infant delivered with Apgar scores 2, 5, and 7 at 1, 5, and 10 minutes
- Severe anemia (hemoglobin 6 g/dL) requiring multiple transfusions
- NICU stay of 21 days
- Long-term follow-up showing mild developmental delay at 2 years
Nursing Implications:
- Recognition of disproportionate fetal distress relative to visible bleeding
- Importance of rapid response and team communication
- Critical role of nurse in emergency triage and mobilization of resources
- Necessity of counseling and support during NICU stay
References
- Cleveland Clinic. (2022). Vasa Previa: Causes, Symptoms, Management & Treatment. https://my.clevelandclinic.org/health/diseases/23465-vasa-previa
- Society of Obstetricians and Gynaecologists of Canada. (2023). Guideline No. 439: Diagnosis and Management of Vasa Previa. Journal of Obstetrics and Gynaecology Canada, 45(5), 608-625. https://www.jogc.com/article/S1701-2163(23)00378-X/fulltext
- Gagnon, R. et al. (2022). Vasa Previa. PMC, National Center for Biotechnology Information. https://pmc.ncbi.nlm.nih.gov/articles/PMC10424826/
- Hasegawa, J. et al. (2023). Challenging common misconceptions in vasa previa screening and diagnosis. Ultrasound in Obstetrics & Gynecology, 53(1), 24-33. https://obgyn.onlinelibrary.wiley.com/doi/10.1002/uog.27567
- Ranzini, A., & Oyelese, Y. (2020). How to screen for vasa previa. Ultrasound in Obstetrics & Gynecology, 57(1), 32-37. https://obgyn.onlinelibrary.wiley.com/doi/full/10.1002/uog.23520
- Jauniaux, E., & Melcer, Y. (2024). Vasa previa in singleton pregnancies: diagnosis and clinical management. American Journal of Obstetrics & Gynecology. https://www.ajog.org/article/S0002-9378(24)00442-3/fulltext
- Boston Children’s Hospital. (2023). Vasa Previa. https://www.childrenshospital.org/conditions/vasa-previa
- Riley Children’s Health. (2023). Vasa Previa. https://www.rileychildrens.org/health-info/vasa-previa
- Maternal Fetal Medicine Associates. (2023). What You Need to Know About Vasa Previa. https://www.mfmnyc.com/blog/need-know-vasa-previa/
- Lecturio Nursing. (2024). Vasa Previa [Free Cheat Sheet]. https://www.lecturio.com/nursing/free-cheat-sheet/vasa-previa/
- Katz, J. et al. (2024). Evaluation of chemical tests for fetal bleeding from vasa previa. International Journal of Gynecology & Obstetrics. https://pubmed.ncbi.nlm.nih.gov/9003944/
- Ruiter, L. et al. (2025). The natural history and management of vasa previa: a single institution experience. BMC Pregnancy and Childbirth, 25, 123-130. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-025-07708-8
