Genitourinary Fistulas
Comprehensive Nursing Study Guide for Healthcare Professionals
Table of Contents
Introduction to Genitourinary Fistulas
Genitourinary fistulas represent abnormal communications between the urinary tract and other body systems, creating pathological connections that disrupt normal anatomical barriers. These complex medical conditions significantly impact patients’ quality of life and require comprehensive nursing knowledge for effective management.
Key Definition
A fistula is an abnormal passageway between two organs or between an organ and the body surface. In genitourinary fistulas, these connections involve the urinary system (bladder, urethra, ureters) and adjacent structures like the vagina, bowel, or skin.
Epidemiological Significance
Pathophysiology of Genitourinary Fistulas
Tissue Damage
Initial trauma or surgical injury creates tissue necrosis and compromises vascular supply
Inflammation
Inflammatory response leads to tissue breakdown and impaired healing processes
Fistula Formation
Abnormal communication develops between organs due to failed tissue repair
Cellular and Molecular Mechanisms
Tissue Ischemia
- Compromised blood supply
- Cellular hypoxia and death
- Impaired collagen synthesis
- Decreased wound healing capacity
Inflammatory Response
- Cytokine release and activation
- Neutrophil and macrophage infiltration
- Matrix metalloproteinase upregulation
- Tissue matrix degradation
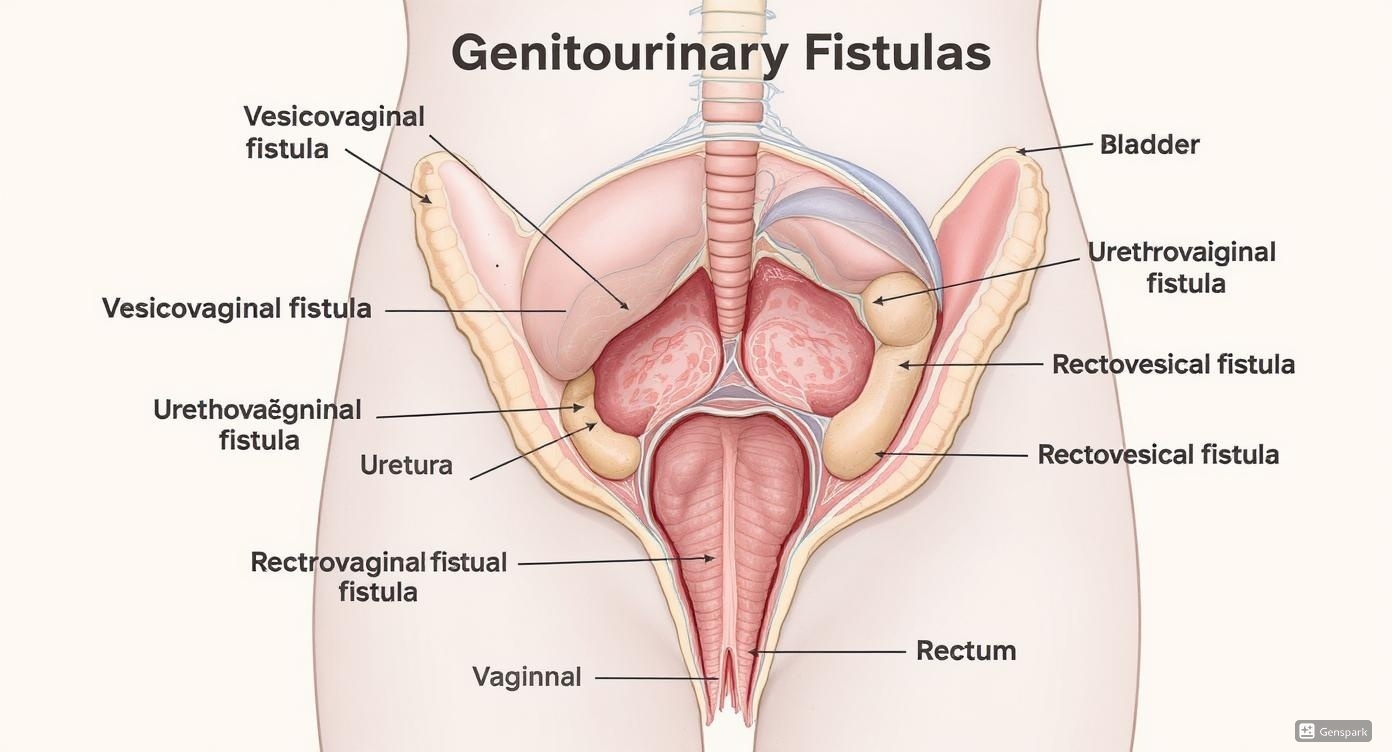
Types of Genitourinary Fistulas
Urogenital Fistulas
Vesicovaginal Fistula (VVF)
Most common type connecting bladder to vagina
Urethrovaginal Fistula
Connection between urethra and vagina
Ureterovaginal Fistula
Abnormal connection between ureter and vagina
Urologic and Other Fistulas
Rectovesical Fistula
Communication between rectum and bladder
Rectourethral Fistula
Connection between rectum and urethra
Colovesical Fistula
Link between colon and bladder
| Fistula Type | Location | Common Causes | Primary Symptoms |
|---|---|---|---|
| Vesicovaginal | Bladder-Vagina | Hysterectomy, prolonged labor | Continuous urinary leakage per vagina |
| Urethrovaginal | Urethra-Vagina | Urethral surgery, trauma | Urinary incontinence, dyspareunia |
| Rectovesical | Rectum-Bladder | Prostate surgery, radiation | Pneumaturia, fecaluria |
| Colovesical | Colon-Bladder | Diverticulitis, Crohn’s disease | Recurrent UTIs, pneumaturia |
Memory Aid: FISTULA Types
Causes and Risk Factors
Iatrogenic Causes
Gynecological Surgery
Hysterectomy accounts for 75% of vesicovaginal fistulas in developed countries
Urological Procedures
Transurethral resection, prostatectomy, urethral surgeries
Colorectal Surgery
Low anterior resection, abdominoperineal resection
Obstetric Causes
Prolonged Labor
Pressure necrosis from fetal head compression
Instrumental Delivery
Forceps or vacuum-assisted deliveries
Cesarean Section
Bladder injury during difficult procedures
Additional Risk Factors
Medical Conditions
- Inflammatory bowel disease
- Diverticular disease
- Pelvic malignancy
- Previous pelvic radiation
- Chronic infections
Patient Factors
- Advanced age
- Diabetes mellitus
- Smoking history
- Malnutrition
- Immunocompromised state
Geographic Factors
- Limited healthcare access
- Inadequate prenatal care
- Cultural practices
- Nutritional deficiencies
- Early marriage and pregnancy
Clinical Manifestations
Urinary Symptoms
Continuous Urinary Leakage
Most characteristic symptom of vesicovaginal fistulas
Urinary Frequency and Urgency
Due to reduced functional bladder capacity
Dysuria and Burning Sensation
Associated with recurrent urinary tract infections
Gynecological Symptoms
Vaginal Discharge
May contain urine, causing odor and irritation
Dyspareunia
Painful intercourse due to anatomical distortion
Vulvar Dermatitis
Chronic exposure to urine causes skin breakdown
Symptom Severity Assessment
with exertion
affecting daily activities
requiring pads
social isolation
| Fistula Type | Pathognomonic Signs | Associated Symptoms | Physical Findings |
|---|---|---|---|
| Vesicovaginal | Continuous clear fluid per vagina | Normal voiding may be preserved | Visible opening on speculum exam |
| Rectovesical | Pneumaturia, fecaluria | Recurrent UTIs, abdominal pain | Gas bubbles in urine |
| Urethrovaginal | Urinary incontinence | Difficulty with catheterization | Anterior vaginal wall defect |
| Colovesical | Pneumaturia, particulate urine | Altered bowel habits | Colonic contents in urine |
Diagnostic Procedures and Assessment
Physical Examination
Speculum Examination
Visual inspection for fistula opening
Digital Examination
Palpation for defects and tissue quality
Three-Swab Test
Differentiates vesical from ureteral fistulas
Laboratory Studies
Urinalysis
Assess for infection, blood, protein
Urine Culture
Identify causative organisms and sensitivities
Creatinine Studies
Vaginal fluid creatinine vs serum levels
Advanced Imaging Modalities
Cystography
Contrast study showing bladder outline and leakage
IVP/CTU
Evaluates upper urinary tract involvement
MRI
Detailed soft tissue visualization
Step-by-Step Diagnostic Approach
Treatment Options and Management Strategies
Conservative Management
Immediate Post-operative Period
- Continuous bladder drainage for 2-4 weeks
- Large bore catheter (16-20 Fr) placement
- Suprapubic catheterization if urethral route contraindicated
- Small fistulas (<1cm) may heal spontaneously
Adjunctive Therapies
- Anticholinergic medications for bladder spasms
- Prophylactic antibiotics
- Nutritional support and optimization
- Smoking cessation counseling
Surgical Interventions
Timing Considerations
- Wait 3-6 months for tissue healing
- Ensure absence of infection and inflammation
- Optimize patient nutritional status
- Early repair (<72 hours) in select cases
Surgical Approaches
- Transvaginal approach (most common)
- Transabdominal approach for complex cases
- Laparoscopic/robotic techniques
- Combined approaches for extensive fistulas
| Procedure | Approach | Success Rate | Indications | Complications |
|---|---|---|---|---|
| Latzko Procedure | Transvaginal | 95-98% | Small, supratrigonal VVF | Vaginal shortening |
| O’Conor Procedure | Transabdominal | 90-95% | Complex, large fistulas | Bladder dysfunction |
| Martius Flap | Transvaginal with graft | 85-90% | Recurrent fistulas | Graft necrosis |
| Ureteral Reimplantation | Transabdominal | 90-95% | Ureterovaginal fistulas | Ureteral stricture |
Treatment Decision Algorithm
Small Fistulas (<1cm)
- • Conservative management first
- • Continuous catheter drainage
- • Monitor for 6-8 weeks
- • Surgery if no improvement
Medium Fistulas (1-2.5cm)
- • Trial of conservative therapy
- • Early surgical consultation
- • Consider timing of repair
- • Simple surgical closure
Large Fistulas (>2.5cm)
- • Immediate surgical planning
- • Complex reconstruction needed
- • Tissue interposition grafts
- • Multidisciplinary approach
Comprehensive Nursing Interventions
Pre-operative Nursing Care
Assessment Priorities
- Comprehensive history of fistula development
- Assessment of urinary leakage patterns
- Evaluation of skin integrity and hygiene needs
- Psychosocial impact assessment
- Nutritional status evaluation
Patient Education
- Explanation of condition and treatment options
- Pre-operative preparation instructions
- Expected outcomes and realistic expectations
- Importance of smoking cessation
Post-operative Nursing Care
Immediate Post-op (0-24 hours)
- Monitor vital signs and pain levels
- Ensure catheter patency and drainage
- Assess surgical site for bleeding
- Monitor fluid balance and urine output
Ongoing Care (1-7 days)
- Prevention of catheter-related infections
- Management of bladder spasms
- Mobilization and deep breathing exercises
- Nutritional support and hydration
Evidence-Based Care Plan for Genitourinary Fistulas
| Nursing Diagnosis | Expected Outcomes | Interventions | Evaluation Criteria |
|---|---|---|---|
| Impaired Urinary Elimination | Patient will maintain continent urinary function | Monitor catheter drainage, assess for blockages | Clear urine output >30ml/hr |
| Risk for Infection | Patient will remain free from UTI | Maintain sterile catheter care, monitor vitals | Normal WBC, afebrile |
| Impaired Skin Integrity | Skin will remain intact and healthy | Frequent perineal care, barrier creams | No evidence of excoriation |
| Anxiety related to condition | Patient will verbalize reduced anxiety | Provide emotional support, education | Patient reports feeling calm |
Holistic Pain and Comfort Management
Pharmacological
- Multimodal analgesia approach
- Anticholinergics for bladder spasms
- Topical anesthetics for perineal discomfort
- Anti-inflammatory medications
Non-pharmacological
- Relaxation and breathing techniques
- Positioning for comfort
- Heat therapy for muscle spasms
- Distraction and music therapy
Environmental
- Quiet, comfortable room environment
- Privacy and dignity maintenance
- Family support encouragement
- Cultural sensitivity considerations
Complications and Long-term Sequelae
Infectious Complications
Urinary Tract Infections
Most common complication, occurring in 60-80% of patients
Pyelonephritis
Ascending infection can lead to kidney involvement
Sepsis
Life-threatening systemic inflammatory response
Surgical Complications
Recurrent Fistula Formation
Occurs in 5-15% of surgical repairs
Ureteral Injury
Risk during complex reconstructive procedures
Bladder Dysfunction
Urgency, frequency, or retention post-operatively
Psychosocial and Quality of Life Impact
Social Isolation
Embarrassment and odor lead to withdrawal from social activities
Sexual Dysfunction
Physical and psychological factors affecting intimacy
Work Impairment
Frequent bathroom needs and hygiene concerns
Depression
High rates of anxiety and depression reported
Prevention and Risk Reduction Strategies
Surgical Prevention
- Careful tissue handling during surgery
- Adequate visualization and exposure
- Identification of anatomical landmarks
- Use of cystoscopy when indicated
- Proper suture technique and materials
Patient Optimization
- Smoking cessation programs
- Nutritional optimization
- Diabetes management
- Treatment of active infections
- Correction of anemia
Memory Aid: COMPLICATIONS of Fistulas
Global Best Practices and Healthcare Innovations
Low-Resource Settings: Africa Initiative
Ethiopia: Hamlin Fistula Hospitals
The Hamlin Fistula Ethiopia program has treated over 60,000 women since 1974, providing free surgery and rehabilitation. Their approach emphasizes:
- Comprehensive care including social reintegration
- Training local surgeons and midwives
- Community education and prevention programs
- 90% success rate in fistula repair
Advanced Technology: Robotic Surgery
United States: Cleveland Clinic Innovation
Pioneering robotic-assisted fistula repairs with improved outcomes:
- Enhanced precision and 3D visualization
- Reduced operative time and blood loss
- Improved success rates (98% for simple cases)
- Faster patient recovery times
Training and Education Programs Worldwide
India: FOGSI Initiative
Federation of Obstetric and Gynecological Societies of India
- National training programs
- Standardized surgical techniques
- Quality assurance protocols
Bangladesh: Dhaka Model
Integrated community-based approach
- Mobile surgical units
- Community health worker training
- Follow-up and support networks
Nigeria: VVF Centers
Government-supported specialized centers
- Regional expertise development
- Free treatment programs
- Prevention education campaigns
International Collaboration and Support
WHO Global Initiatives
- Global strategy to end preventable maternal mortality
- Skilled birth attendant training programs
- Emergency obstetric care accessibility
- Quality improvement frameworks
Non-Governmental Organizations
- UNFPA: Supporting fistula treatment globally
- Fistula Foundation: Funding surgical missions
- EngenderHealth: Training healthcare providers
- Direct Relief: Medical supply donations
Key Takeaways for Nursing Practice
Early Recognition
Understanding the early signs and symptoms of genitourinary fistulas enables nurses to advocate for timely diagnosis and intervention, significantly improving patient outcomes and quality of life.
Holistic Care
Effective nursing management of fistulas requires addressing not only the physical symptoms but also the psychological, social, and cultural impacts on patients and their families.
Prevention Focus
Prevention through skilled birth attendance, proper surgical technique, and patient education remains the most effective strategy for reducing the global burden of genitourinary fistulas.
Evidence-Based Practice Points
Clinical Excellence
- Early catheter placement can prevent up to 85% of small fistulas
- Multidisciplinary team approach improves success rates
- Patient education reduces anxiety and improves compliance
- Regular follow-up prevents long-term complications
Quality Outcomes
- Proper surgical timing increases repair success to >90%
- Comprehensive care addresses quality of life issues
- Cultural sensitivity improves patient satisfaction
- Continuous education enhances nursing competency
This comprehensive guide serves as an educational resource for nursing students and healthcare professionals.
Always consult current clinical guidelines and institutional protocols for patient care decisions.
