First Aid Management of Unconsciousness
Comprehensive Nursing Education Notes
Professional first aid assessment and management of unconscious patients
Table of Contents
Introduction & Overview
Key Learning Objectives
- Understand the pathophysiology of unconsciousness
- Perform systematic assessment of unconscious patients
- Implement evidence-based first aid interventions
- Apply nursing process to unconscious patient care
- Recognize emergency situations requiring immediate intervention
Unconsciousness represents a state of altered consciousness where an individual cannot be aroused by verbal or physical stimuli and lacks awareness of themselves and their environment. As a nurse, understanding the first aid management of unconscious patients is crucial for providing immediate, life-saving interventions while preventing further complications.
Why This Matters
- • Unconsciousness can be life-threatening
- • Immediate assessment prevents complications
- • Proper positioning prevents aspiration
- • Early intervention improves outcomes
Nursing Scope
- • Primary survey and assessment
- • Airway management and positioning
- • Vital signs monitoring
- • Safety and environmental management
Critical Alert
Never assume an unconscious person is “just sleeping” or under the influence of substances. Always treat unconsciousness as a medical emergency until proven otherwise through systematic assessment.
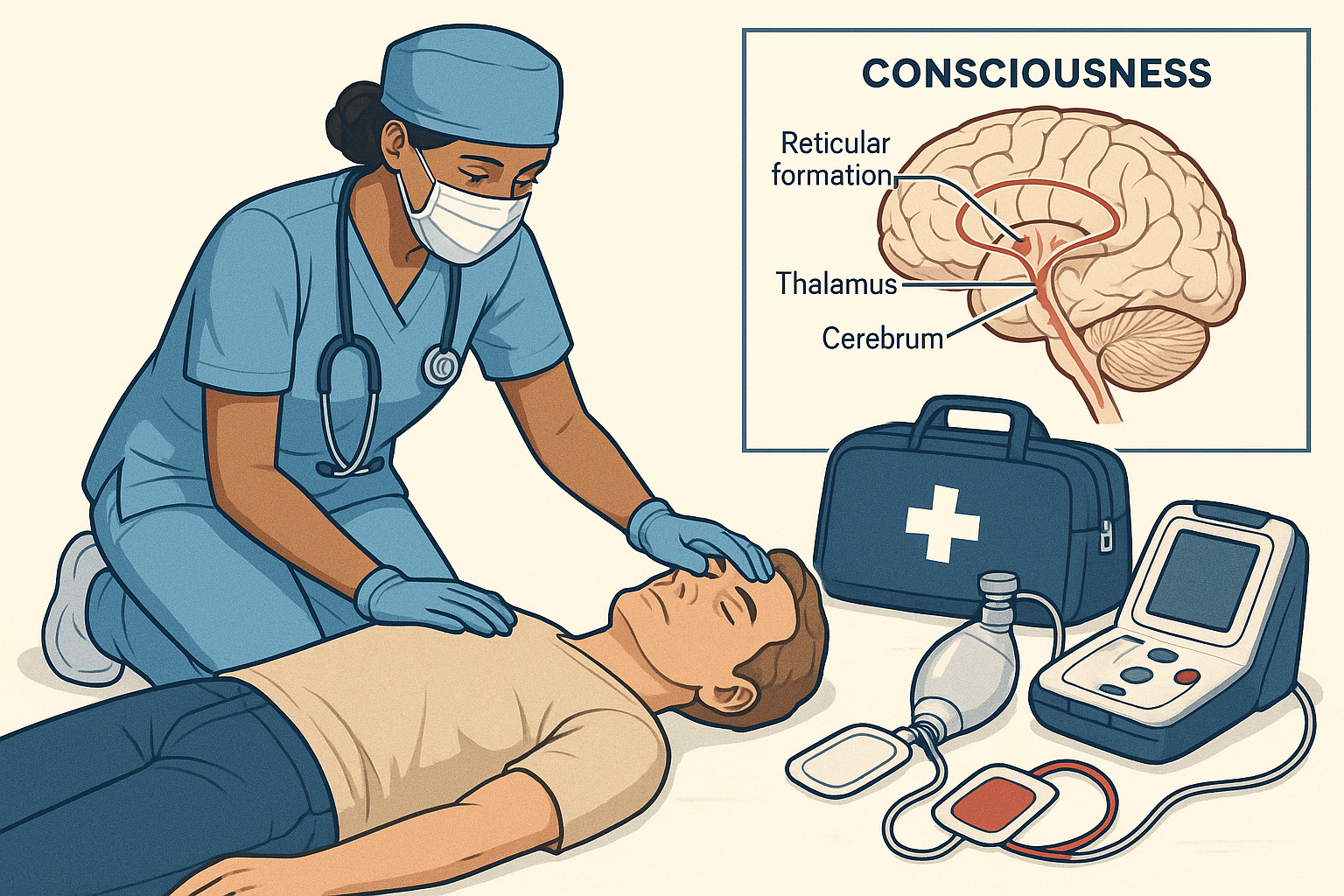
Pathophysiology of Consciousness
Consciousness depends on the interaction between the cerebral cortex and the reticular activating system (RAS) in the brainstem. Understanding this relationship is fundamental to recognizing why unconsciousness occurs and how to manage it effectively.
Components of Consciousness
Arousal (Wakefulness)
Controlled by the reticular activating system in the brainstem, extending from medulla to thalamus
Awareness (Content)
Mediated by the cerebral cortex, particularly the association areas
Physiological Requirements
- Glucose: 5.5 mmol/L minimum
- Oxygen: Adequate cerebral perfusion
- Temperature: Normal range (36-37.5°C)
- Electrolytes: Sodium, calcium balance
- pH: 7.35-7.45 for optimal function
Memory Aid: CONSCIOUSNESS Mnemonic
C – Cerebral cortex (awareness)
O – Oxygen requirement
N – Neurological pathways
S – Sodium balance
C – Circulation (cerebral)
I – Intact brainstem
O – Optimal temperature
U – Undisturbed RAS
S – Sufficient glucose
N – Normal pH
E – Electrolyte balance
S – Synaptic transmission
S – Structural integrity
Clinical Pearls
- • Small brainstem lesions can cause profound unconsciousness
- • Bilateral cortical damage may preserve arousal but impair awareness
- • Metabolic causes often show fluctuating levels of consciousness
- • Structural causes typically show progressive deterioration
Causes of Unconsciousness
Understanding the various causes of unconsciousness helps nurses prioritize assessment and interventions. Causes can be broadly categorized into structural, metabolic, toxic, and psychiatric origins.
AEIOU-TIPS Mnemonic for Causes
Alcohol, Acidosis, Arrhythmias
Including diabetic ketoacidosis, uremic acidosis
Epilepsy, Electrolytes, Encephalitis
Post-ictal state, hyponatremia, hypercalcemia
Insulin, Infection, Intussusception
Hypoglycemia, hyperglycemia, sepsis
Opiates, Oxygen
Overdose, hypoxia, carbon monoxide
Uremia, Underdose
Renal failure, missed medications
Trauma, Temperature, Toxins
Head injury, hypothermia, poisoning
Infection
Meningitis, encephalitis, sepsis
Psychiatric, Poisoning
Conversion disorder, drug overdose
Stroke, Shock, Space-occupying lesion
CVA, hypovolemia, tumor, hematoma
Cardiovascular Causes
- • Cardiac arrest
- • Severe arrhythmias
- • Massive MI
- • Cardiogenic shock
- • Severe hypertension
Metabolic Causes
- • Hypoglycemia (<2.8 mmol/L)
- • Severe hyperglycemia
- • Hepatic encephalopathy
- • Uremic encephalopathy
- • Severe hypothermia
Neurological Causes
- • Stroke (brainstem)
- • Intracranial hemorrhage
- • Severe head trauma
- • Status epilepticus
- • Brain tumor
Time-Critical Causes
These conditions require immediate recognition and intervention:
- • Hypoglycemia (treat within minutes)
- • Cardiac arrest (CPR immediately)
- • Status epilepticus (anticonvulsants)
- • Opioid overdose (naloxone)
- • Severe hypoxia (oxygen/ventilation)
- • Increased ICP (positioning, osmotherapy)
Primary Assessment Techniques
Systematic assessment of an unconscious patient follows the ABCDE approach, with particular attention to life-threatening conditions that require immediate intervention.
ABCDE Assessment Protocol
A – AIRWAY
Assessment:
- • Look for visible obstruction
- • Listen for stridor or gurgling
- • Feel for air movement
- • Check for vomit or foreign objects
Interventions:
- • Head tilt-chin lift (if no trauma)
- • Jaw thrust (if cervical spine injury suspected)
- • Suction if secretions present
- • Recovery position if breathing adequately
B – BREATHING
Assessment:
- • Rate (normal 12-20/min)
- • Depth and pattern
- • Chest movement symmetry
- • Oxygen saturation
- • Skin color and temperature
Interventions:
- • High-flow oxygen (15L/min via mask)
- • Bag-mask ventilation if inadequate
- • Monitor oxygen saturation continuously
- • Prepare for intubation if needed
C – CIRCULATION
Assessment:
- • Pulse rate, rhythm, strength
- • Blood pressure
- • Capillary refill time
- • Skin color and warmth
- • Look for obvious bleeding
Interventions:
- • IV access (two large bore cannulas)
- • Control external bleeding
- • Fluid resuscitation if shocked
- • ECG monitoring
D – DISABILITY (Neurological)
Assessment:
- • Glasgow Coma Scale
- • Pupil size and reactivity
- • Limb movement and tone
- • Blood glucose level
Interventions:
- • Treat hypoglycemia immediately
- • Consider naloxone if opioid suspected
- • Prevent secondary brain injury
- • Maintain neutral cervical spine
E – EXPOSURE & Environment
Assessment:
- • Full body examination
- • Core temperature
- • Signs of trauma or injection sites
- • Medical alert jewelry
Interventions:
- • Maintain normothermia
- • Preserve dignity and privacy
- • Remove from hazardous environment
- • Document all findings
Glasgow Coma Scale (GCS) Assessment
Eye Opening (E)
Verbal Response (V)
Motor Response (M)
Total GCS Score: 3-15 (E + V + M)
Severe: 3-8 | Moderate: 9-12 | Mild: 13-15
Assessment Success Tips
- • Always assume cervical spine injury in trauma patients
- • Perform blood glucose test within first 5 minutes
- • Reassess vital signs every 5-10 minutes initially
- • Document time of each assessment and intervention
- • Consider reversible causes first (hypoglycemia, opioids)
First Aid Management Protocol
The first aid management of unconsciousness follows a structured approach prioritizing life-threatening conditions while preparing for advanced medical care.
FIRST AID Mnemonic for Unconscious Patients
Find and treat reversible causes
Hypoglycemia, opioid overdose, hypoxia
Immediately assess ABCDE
Systematic primary survey
Recovery position if breathing
Maintain airway, prevent aspiration
Stabilize cervical spine
If trauma suspected
Test blood glucose
Treat hypoglycemia immediately
Administer oxygen
High-flow if available
IV access and monitoring
Prepare for medications
Document and transport
Continuous monitoring
Step-by-Step First Aid Protocol
Step 1: Immediate Safety & Response (0-30 seconds)
Scene Safety:
- • Check for hazards (fire, electrical, traffic)
- • Ensure personal safety first
- • Move patient only if in immediate danger
- • Call for help immediately
Initial Response:
- • Shake shoulders gently and shout
- • Check for responsiveness to voice
- • If no response, assume unconscious
- • Activate emergency services (call 911/999)
Step 2: Airway Management (30-60 seconds)
No Trauma Suspected:
- • Head tilt-chin lift maneuver
- • Remove visible foreign objects
- • Suction secretions if available
- • Insert oropharyngeal airway if trained
Trauma Suspected:
- • Jaw thrust without head tilt
- • Maintain cervical spine immobilization
- • Log roll if positioning needed
- • Two-person technique preferred
Step 3: Breathing Assessment & Support (1-2 minutes)
Assessment:
- • Look for chest rise and fall
- • Listen for breath sounds
- • Feel for air movement (10 seconds)
- • Check oxygen saturation if available
Support:
- • High-flow oxygen (15L/min via mask)
- • Bag-mask ventilation if inadequate
- • Rate: 10-12 breaths/minute for adults
- • Monitor chest rise with each breath
Step 4: Circulation & Neurological Check (2-3 minutes)
Circulation:
- • Check carotid pulse (central)
- • Assess skin color and temperature
- • Look for obvious bleeding
- • Apply direct pressure to wounds
Neurological:
- • Check pupil size and reactivity
- • Test blood glucose immediately
- • Assess limb movement
- • Glasgow Coma Scale assessment
Step 5: Treat Reversible Causes (3-5 minutes)
Hypoglycemia:
- • If BGL <4.0 mmol/L
- • IV glucose 25g (50ml of 50%)
- • Or glucagon 1mg IM
- • Recheck in 10 minutes
Opioid Overdose:
- • Pinpoint pupils
- • Respiratory depression
- • Naloxone 0.4-2mg IV/IM
- • Repeat every 2-3 minutes
Seizure:
- • Post-ictal state
- • Protect from injury
- • Check for status epilepticus
- • Prepare anticonvulsants
Step 6: Positioning & Protection (Ongoing)
If Breathing Adequately:
- • Recovery position (left lateral)
- • Ensure airway remains open
- • Monitor for vomiting
- • Prevent pressure sores
If Trauma Suspected:
- • Maintain spinal immobilization
- • Log roll with adequate personnel
- • Use spinal board if available
- • Cervical collar application
Time-Critical Actions
Within 1 minute:
- • Call for emergency services
- • Secure airway
- • Check breathing
Within 5 minutes:
- • Blood glucose test
- • Treat hypoglycemia
- • Administer naloxone if indicated
Comprehensive Nursing Interventions
Beyond first aid, nurses must provide comprehensive care addressing physiological, safety, and psychological needs of unconscious patients and their families.
Assessment
Continuous monitoring and evaluation
Diagnosis
Identify nursing problems
Planning
Set goals and interventions
Implementation
Execute nursing care
Priority Nursing Diagnoses for Unconscious Patients
High Priority
- 1 Ineffective airway clearance related to decreased level of consciousness
- 2 Risk for aspiration related to impaired swallowing and gag reflex
- 3 Impaired gas exchange related to altered breathing pattern
- 4 Risk for injury related to altered level of consciousness
Medium Priority
- 5 Impaired skin integrity related to immobility
- 6 Risk for infection related to invasive procedures
- 7 Imbalanced nutrition related to inability to eat
- 8 Anxiety (family) related to patient condition
System-Based Nursing Interventions
Respiratory System Management
Continuous Assessment:
- • Respiratory rate, depth, and pattern every 15 minutes initially
- • Oxygen saturation monitoring (maintain >95%)
- • Auscultate lung fields every 2-4 hours
- • Monitor for signs of respiratory distress
- • Assess airway patency continuously
Interventions:
- • Position to optimize ventilation (semi-Fowler’s if no spinal injury)
- • Suction airway as needed (limit to 15 seconds)
- • Provide chest physiotherapy every 2 hours
- • Turn patient every 2 hours to prevent atelectasis
- • Maintain artificial airway if present
Neurological System Monitoring
Neurological Assessments:
- • Glasgow Coma Scale every 15 minutes initially
- • Pupil size, shape, and reactivity
- • Motor response and reflexes
- • Vital sign trends (Cushing’s triad)
- • Signs of increased intracranial pressure
Neuroprotective Measures:
- • Maintain head of bed 15-30° (unless contraindicated)
- • Keep head in neutral position
- • Minimize stimulation during acute phase
- • Control fever aggressively
- • Monitor blood glucose closely
Cardiovascular System Support
Monitoring:
- • Continuous cardiac monitoring
- • Blood pressure every 15 minutes initially
- • Pulse quality and rhythm
- • Capillary refill and peripheral perfusion
- • Fluid balance (I&O)
Interventions:
- • Maintain adequate perfusion pressure
- • IV access and fluid management
- • Sequential compression devices for DVT prevention
- • Monitor for arrhythmias
- • Administer vasoactive drugs as ordered
Skin Integrity and Mobility
Pressure Injury Prevention:
- • Turn and reposition every 2 hours
- • Use pressure-relieving mattresses
- • Inspect skin every shift for breakdown
- • Keep skin clean and dry
- • Heel protectors and positioning devices
Range of Motion:
- • Passive ROM exercises every 4 hours
- • Position limbs in functional alignment
- • Use splints to prevent contractures
- • Collaborate with physiotherapy
- • Monitor for muscle atrophy
Elimination Management
Urinary Management:
- • Insert urinary catheter if indicated
- • Monitor urine output (>0.5ml/kg/hr)
- • Assess for urinary tract infections
- • Maintain catheter hygiene
- • Consider intermittent catheterization
Bowel Management:
- • Assess bowel sounds every 4 hours
- • Monitor for fecal impaction
- • Provide bowel care as needed
- • Consider bowel regimen
- • Document bowel movements
Nursing Excellence Tips
- • Always explain procedures to unconscious patients – they may hear you
- • Provide comfort measures: soft music, familiar voices, gentle touch
- • Maintain patient dignity and privacy during care
- • Communicate regularly with family members
- • Document detailed assessments and interventions
- • Collaborate with interdisciplinary team members
Special Considerations
Certain populations and situations require modified approaches to the management of unconsciousness. Understanding these variations is crucial for safe, effective care.
Pediatric Patients
- Airway: Proportionally larger tongue, smaller airway
- Breathing: Higher respiratory rate (20-30/min)
- Circulation: Higher heart rate (100-160 bpm)
- Glucose: More prone to hypoglycemia
- Temperature: Heat loss more rapid
- Positioning: Neutral head position
Elderly Patients
- Medications: Polypharmacy interactions common
- Comorbidities: Multiple underlying conditions
- Skin: More fragile, higher pressure injury risk
- Cognition: Baseline dementia may confound assessment
- Mobility: Higher risk of complications from immobility
- Frailty: Lower physiological reserve
Pregnant Patients
- Positioning: Left lateral tilt to prevent supine hypotension
- Airway: Increased risk of aspiration
- Circulation: Increased blood volume and cardiac output
- Fetal monitoring: Assess fetal heart rate if viable
- Medications: Consider teratogenic effects
- Trauma: Placental abruption risk
Scenario-Specific Considerations
Diabetic Emergencies
Hypoglycemia (<4.0 mmol/L)
Signs:
- • Rapid onset
- • Diaphoresis
- • Normal or rapid breathing
- • Normal skin turgor
Treatment:
- • 50ml of 50% glucose IV
- • Or 1mg glucagon IM
- • Recheck BGL in 10 minutes
- • Provide complex carbs when conscious
Hyperglycemia (>15 mmol/L)
Signs:
- • Gradual onset
- • Kussmaul breathing
- • Dehydration
- • Ketone odor
Treatment:
- • IV fluid resuscitation
- • Insulin therapy (hospital setting)
- • Monitor electrolytes
- • Urgent medical transport
Substance-Related Unconsciousness
Opioid Overdose
Signs:
- • Pinpoint pupils
- • Respiratory depression
- • Bradycardia
- • Cyanosis
Treatment:
- • Naloxone 0.4-2mg IV/IM/IN
- • Repeat every 2-3 minutes
- • Support ventilation
- • Monitor for re-sedation
Alcohol Intoxication
Signs:
- • Alcohol odor
- • Ataxia, slurred speech
- • Hypothermia
- • Hypoglycemia
Treatment:
- • Thiamine 100mg IV first
- • Then glucose if hypoglycemic
- • Warming measures
- • Monitor for withdrawal
Stimulant Overdose
Signs:
- • Hyperthermia
- • Hypertension
- • Tachycardia
- • Agitation/seizures
Treatment:
- • Cooling measures
- • Benzodiazepines for agitation
- • IV fluids
- • Monitor cardiac rhythm
Trauma-Related Unconsciousness
Spinal Injury Precautions
- • Maintain cervical spine immobilization at all times
- • Use jaw thrust instead of head tilt-chin lift
- • Log roll with minimum 3-4 people
- • Apply cervical collar when available
- • Maintain neutral spine alignment
- • Document neurological deficits
Head Injury Management
- • Monitor for signs of increased ICP
- • Cushing’s triad: hypertension, bradycardia, irregular breathing
- • Avoid neck flexion (impedes venous drainage)
- • Prevent hypoxia and hypotension
- • Monitor pupil changes closely
- • Prepare for possible neurosurgical intervention
RED FLAGS Mnemonic – Immediate Concerns
Respiratory failure
Apnea, severe bradypnea, cyanosis
Extreme bradycardia
Heart rate <50 bpm
Dilated/fixed pupils
Sign of brainstem compression
Fever >40°C
Hyperthermia, heat stroke
Low blood glucose
<2.8 mmol/L - treat immediately
Active bleeding
Major hemorrhage, shock
GCS drop >2 points
Deteriorating neurological status
Status epilepticus
Continuous seizure >5 minutes
Nursing Implementation in Practice
This section focuses on the practical application of unconsciousness management in various healthcare settings, emphasizing the unique role of nurses in different environments.
Emergency Department
- Triage: Category 1 – Immediate attention
- Assessment: Complete ABCDE within 5 minutes
- Interventions: Immediate airway management
- Monitoring: Continuous vital signs
- Team: Coordinate with emergency physician
- Family: Provide updates and support
Intensive Care Unit
- Monitoring: Advanced hemodynamic monitoring
- Interventions: Complex life support systems
- Assessment: Hourly neurological checks
- Prevention: VAP, pressure injury protocols
- Team: Multidisciplinary rounds
- Family: Communication and decision support
Community/Home Setting
- Recognition: Early identification of changes
- Response: Emergency service activation
- Support: Basic life support until help arrives
- Family: Education on warning signs
- Prevention: Risk factor modification
- Follow-up: Chronic condition management
Quality Indicators for Unconscious Patient Care
Process Indicators
- Time to ABCDE assessment: <5 minutes from arrival
- Time to glucose test: <5 minutes from identification
- Oxygen therapy initiation: <2 minutes if indicated
- Naloxone administration: <3 minutes if opioid suspected
Outcome Indicators
- Survival to discharge: Monitor by cause
- Neurological outcome: Glasgow Outcome Scale
- Pressure injury rates: <5% for unconscious patients
- HAI rates: Ventilator-associated pneumonia
Interprofessional Team Communication
SBAR Communication Framework
S – Situation: “Patient found unconscious, GCS 6”
B – Background: “45-year-old diabetic, last seen 2 hours ago”
A – Assessment: “BGL 1.8, responsive to glucose administration”
R – Recommendation: “Continue glucose monitoring, consider admission”
Emergency Physician
- • Clinical assessment findings
- • Response to interventions
- • Suspected diagnosis
- • Need for procedures
Laboratory
- • STAT glucose
- • Arterial blood gas
- • Toxicology screen
- • Basic metabolic panel
Radiology
- • CT head (if trauma)
- • Chest X-ray
- • C-spine (if indicated)
- • Urgent vs routine
Nursing Education and Competency Development
Core Competencies
- Assessment skills: Systematic ABCDE approach
- Airway management: Positioning, suctioning, adjuncts
- Monitoring skills: Vital signs, neurological assessment
- Emergency response: BLS, medication administration
- Documentation: Accurate, timely, legal requirements
Training Methods
- E-learning modules: Interactive case studies
- Simulation training: High-fidelity mannequins
- Certification courses: ACLS, PALS, TNCC
- Competency assessment: Annual skill validation
- Case review: Multidisciplinary debriefing
Family-Centered Care Implementation
Communication Strategies
- • Regular updates: Every 30 minutes during acute phase
- • Simple language: Avoid medical jargon
- • Active listening: Address family concerns and questions
- • Cultural sensitivity: Respect religious and cultural practices
- • Realistic expectations: Honest prognosis discussions
- • Decision support: Involve in care planning when appropriate
Support Services
- • Social work consultation: Family support and resources
- • Chaplain services: Spiritual care and comfort
- • Interpreter services: Language barrier support
- • Waiting area amenities: Comfortable environment
- • Visiting policies: Flexible to support family presence
- • Educational materials: Written information about condition
Documentation & Legal Considerations
Comprehensive documentation is essential for unconscious patients, serving legal, communication, and quality improvement purposes. Understanding documentation requirements protects both patients and healthcare providers.
Essential Documentation Elements
Initial Assessment Documentation
- • Time of discovery/arrival
- • Circumstances of unconsciousness
- • Witness statements
- • Initial Glasgow Coma Scale
- • Vital signs at presentation
- • Physical examination findings
- • Immediate interventions performed
- • Response to interventions
Ongoing Documentation
- • Neurological assessments with time
- • Vital sign trends and patterns
- • Medication administration and effects
- • Nursing interventions and rationale
- • Patient positioning and turning
- • Skin integrity assessments
- • Family communication and presence
- • Physician notifications and orders
Legal and Ethical Considerations
Consent Issues
Implied consent: Emergency treatment for unconscious patients
Life-saving interventions can proceed without explicit consent
Surrogate decision-makers: Next of kin or legal guardians
Involve family in non-emergency decisions when possible
Advanced directives: Living wills and healthcare proxies
Honor patient’s previously expressed wishes
Duty of Care
Standard of care: Act as a reasonable prudent nurse would
Follow evidence-based protocols and guidelines
Scope of practice: Work within nursing competencies
Seek physician orders for medical interventions
Continuous monitoring: Maintain vigilant patient surveillance
Document changes and notify physicians promptly
Documentation Templates and Examples
Initial Assessment Note Template
Date/Time: [Exact time of assessment]
Patient found: [Unconscious in bathroom floor by family member]
Initial GCS: E[1] V[1] M[4] = [6/15]
Vital Signs: BP [140/90], HR [88], RR [12], T [36.8°C], SpO2 [95%]
Blood Glucose: [2.1 mmol/L]
Interventions: [Airway secured, 50ml 50% glucose IV administered]
Response: [GCS improved to 12/15 within 10 minutes]
Physician notified: [Dr. Smith at 14:25 – new orders received]
Neurological Flow Sheet Example
| Time | GCS (E/V/M) | Pupils R/L | Motor | BP | HR | Interventions |
|---|---|---|---|---|---|---|
| 14:00 | 1/1/4 = 6 | 3mm/3mm + | Withdraws | 140/90 | 88 | Glucose 50ml IV |
| 14:15 | 3/4/5 = 12 | 3mm/3mm + | Localizes | 130/80 | 78 | Oriented to person |
Documentation Quality Assurance
Accuracy
- • Document in real-time when possible
- • Use objective, measurable terms
- • Avoid subjective interpretations
- • Correct errors appropriately
Completeness
- • Include all required elements
- • Document absence of findings
- • Note patient responses to care
- • Record family interactions
Compliance
- • Follow organizational policies
- • Meet regulatory requirements
- • Maintain confidentiality
- • Store records securely
Risk Management Considerations
High-Risk Situations
- Delayed recognition: Late identification of unconsciousness
- Medication errors: Wrong dose, route, or drug
- Communication failures: Inadequate handoff information
- Equipment malfunction: Monitoring or life support failure
Protective Strategies
- Follow protocols: Evidence-based care pathways
- Double-check medications: Independent verification
- Structured communication: SBAR format for handoffs
- Equipment checks: Regular maintenance and testing
Prevention & Patient Education
Prevention of unconsciousness episodes and education of patients, families, and communities about recognition and response strategies are essential components of comprehensive nursing care.
