Burns & Scalds: First Aid Management
Comprehensive Nursing Guide for Emergency Care
Table of Contents
Introduction & Overview
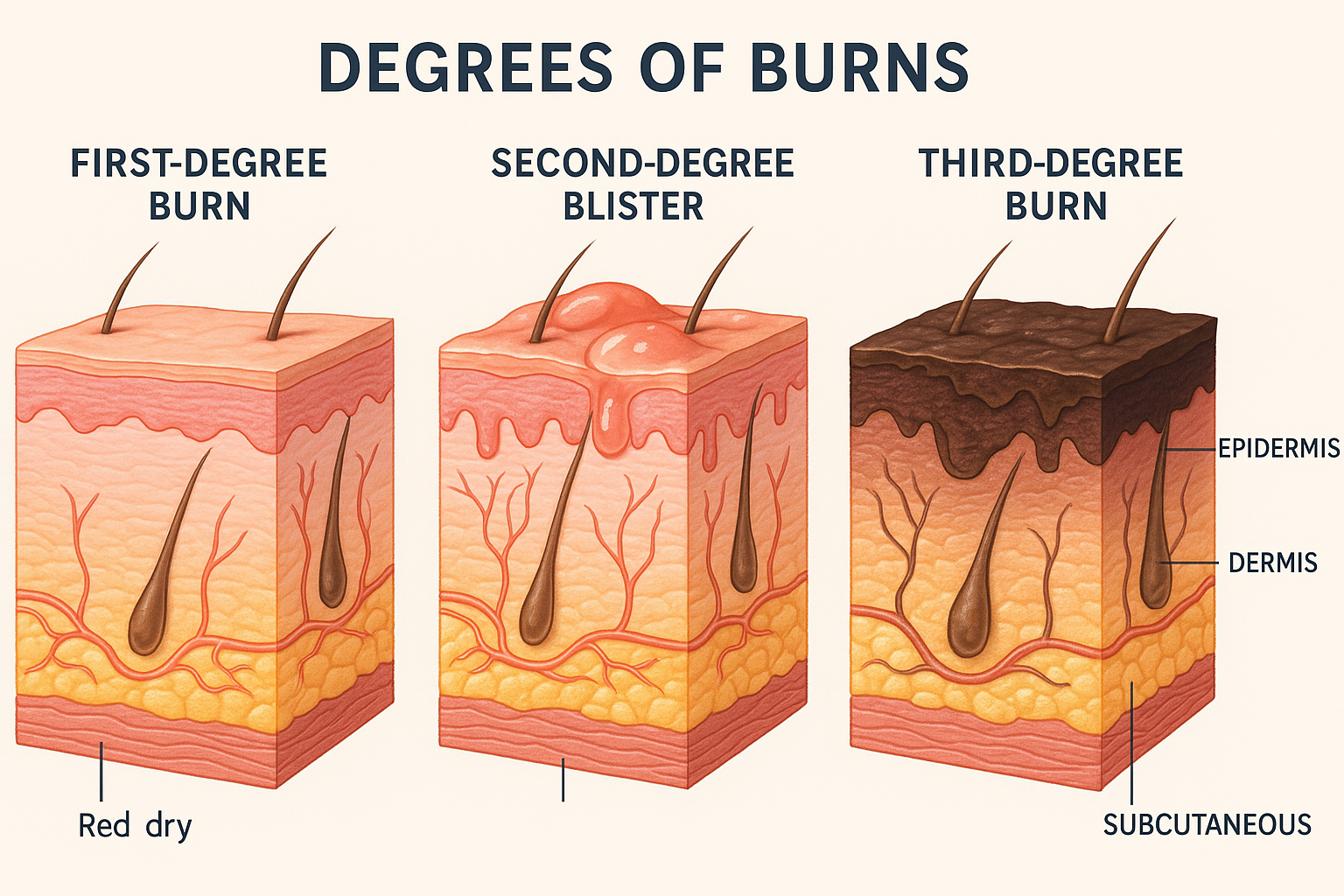
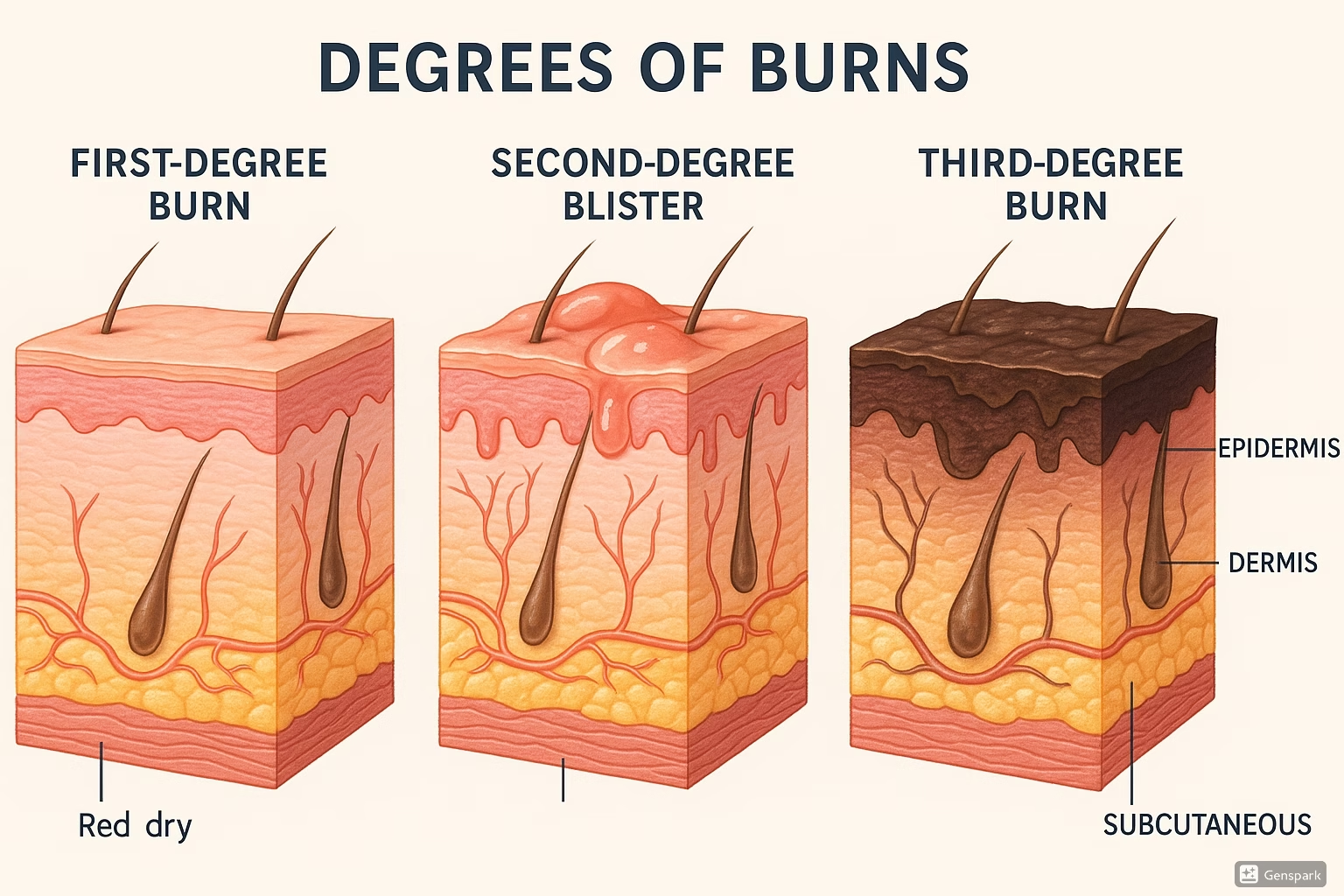
Figure 1: Cross-sectional anatomy showing different degrees of burn injuries
Burns and scalds represent one of the most common emergency presentations in healthcare settings, affecting millions of individuals worldwide annually. As a nursing professional, understanding the comprehensive management of thermal injuries is crucial for optimal patient outcomes and prevention of long-term complications.
Clinical Pearl
The first hour after a burn injury is critical – appropriate first aid can reduce burn depth, minimize pain, and prevent infection. Remember: “Cool, Clean, Cover, Comfort, and Convey to hospital.”
Key Statistics & Epidemiology
- Burns account for approximately 180,000 deaths globally each year
- Children under 5 years and adults over 65 years are at highest risk
- Scalds represent 65% of burns in children under 4 years
- 95% of burns occur in low- and middle-income countries
- Most burns are preventable through education and safety measures
Types of Thermal Injuries
Burns
Injuries caused by dry heat sources such as flames, hot objects, electricity, chemicals, or radiation.
Scalds
Injuries caused by moist heat such as hot liquids, steam, or hot gases.
Classification of Burns
By Depth (Degree System)
| Degree | Depth | Appearance | Pain Level | Healing Time | Scarring |
|---|---|---|---|---|---|
| First Degree (Superficial) |
Epidermis only | Red, dry, no blisters Blanches with pressure |
Very painful | 3-7 days | None |
| Second Degree (Partial Thickness) |
Epidermis + partial dermis | Red, moist, blisters present Blanches with pressure |
Extremely painful | 7-21 days | Minimal to moderate |
| Third Degree (Full Thickness) |
Through dermis into subcutaneous | White, brown, or black Leathery texture No blanching |
Painless (nerve damage) | Weeks to months Requires grafting |
Severe scarring |
| Fourth Degree (Deep Full Thickness) |
Into muscle, bone, organs | Charred, dry Visible bone/muscle |
Painless | Requires amputation or extensive surgery |
Severe deformity |
Memory Aid – “RED PAIN HEAL”
Red and painful = First degree
Extremely painful with blisters = Second degree
Dry and painless = Third degree
Partial thickness = Second degree
All layers involved = Third degree
Incredibly deep = Fourth degree
Heals fast (days) = First degree
Extended healing (weeks) = Second degree
Always needs grafting = Third degree
Limb threatening = Fourth degree
By Cause
Thermal Burns
- • Flames
- • Hot liquids/steam
- • Hot surfaces
- • Hot gases
Electrical Burns
- • Low voltage (<1000V)
- • High voltage (>1000V)
- • Lightning
- • Arc injuries
Other Burns
- • Chemical
- • Radiation
- • Cold injury
- • Friction
Pathophysiology of Burn Injuries
Jackson’s Burn Wound Model
Coagulation
Irreversible tissue death
Stasis
Decreased perfusion
Potentially salvageable
Hyperemia
Increased blood flow
Will heal spontaneously
Systemic Response to Burns
Immediate Phase (0-72 hours)
- Massive fluid shift from intravascular to interstitial space
- Increased capillary permeability
- Hypovolemic shock risk
- Inflammatory mediator release
- Hypermetabolic state initiation
Recovery Phase (72+ hours)
- Fluid mobilization and diuresis
- Wound healing processes begin
- Risk of infection increases
- Hypermetabolism peaks
- Scar formation begins
Clinical Pearl – The “48-72 Hour Rule”
The zone of stasis can be converted to either recovery or coagulation within 48-72 hours post-injury. Proper first aid and early intervention can save this tissue, while inadequate care can worsen the injury.
Initial Assessment & Triage
Critical Priority
Always follow ABCDE approach: Airway, Breathing, Circulation, Disability, Exposure. Burns affecting airway or breathing take absolute priority.
Primary Survey – ABCDE Approach
Burn Size Assessment
Rule of Nines (Adults)
- Head & neck: 9%
- Each arm: 9%
- Chest: 9%
- Abdomen: 9%
- Upper back: 9%
- Lower back: 9%
- Each leg front: 9%
- Each leg back: 9%
- Genitalia: 1%
Modified Rule (Children)
- Head: 18% (larger proportion)
- Each arm: 9%
- Chest & abdomen: 18%
- Back: 18%
- Each leg: 14% (smaller proportion)
- Genitalia: 1%
Palm Rule: Patient’s palm = 1% TBSA
Memory Aid – “Head to Toe Nines”
Head = 9%
Each arm = 9%
Anterior trunk = 18% (chest 9% + abdomen 9%)
Dorsal trunk = 18% (upper back 9% + lower back 9%)
Thighs and legs = 36% (each leg 18%)
One percent for genitals
Burn Severity Classification
| Severity | Criteria | Treatment Setting | Nursing Priorities |
|---|---|---|---|
| Minor |
• <15% TBSA (adult) • <10% TBSA (child/elderly) • <2% full thickness • No special areas involved |
Outpatient/Home care | Education, wound care, pain management |
| Moderate |
• 15-25% TBSA (adult) • 10-20% TBSA (child/elderly) • 2-10% full thickness • Some special areas |
Hospital admission | Fluid resuscitation, monitoring, wound care |
| Major |
• >25% TBSA (adult) • >20% TBSA (child/elderly) • >10% full thickness • Special areas involved • Inhalation injury |
Burn center/ICU | Intensive monitoring, aggressive resuscitation |
First Aid Management
Golden Rule of Burn First Aid
“Stop, Drop, Cool, Call, Cover” – The immediate actions that can save lives and reduce burn severity.
Immediate Actions – The “5 C’s”
COOL
Apply cool running water for 20 minutes
CLEAN
Gently clean with mild soap if possible
COVER
Apply sterile, non-adherent dressing
COMFORT
Provide pain relief and emotional support
CONVEY
Transport to appropriate healthcare facility
Detailed First Aid Protocol
Step-by-Step First Aid Process
Ensure Safety
Remove patient from source of burn. Turn off electricity, extinguish flames, remove from chemicals.
Stop the Burning Process
Remove smoldering clothing (not adherent). Pour cool water over area immediately.
Cool the Burn
Apply cool (not ice-cold) running water for 20 minutes. Temperature: 8-25°C (46-77°F).
Assess and Call for Help
Evaluate burn severity using TBSA and depth. Call emergency services if indicated.
Cover and Protect
Apply sterile, non-adherent dressing. Use plastic wrap if sterile dressings unavailable.
Monitor and Support
Monitor vital signs, provide emotional support, prepare for transport if necessary.
What NOT to Do
- Never use ice – can cause further tissue damage
- Don’t apply butter, oils, or home remedies
- Don’t break blisters
- Don’t remove adherent clothing
- Don’t use cotton balls or fluffy materials directly on burn
- Don’t delay cooling to find “perfect” temperature water
Special Considerations
Electrical Burns
- • Ensure power source is OFF before approach
- • Look for entry and exit wounds
- • Monitor for cardiac arrhythmias
- • Assess for internal injuries
- • All electrical burns require hospital evaluation
Chemical Burns
- • Remove contaminated clothing immediately
- • Flush with copious amounts of water
- • Continue flushing for 20-60 minutes
- • Identify the chemical if possible
- • Some chemicals may require special antidotes
Advanced Medical Care
Fluid Resuscitation
Parkland Formula
4 mL × weight (kg) × %TBSA = Total fluid in first 24 hours
Give 50% in first 8 hours, 50% in next 16 hours
Fluid Resuscitation Protocol
Hours 0-8
50% of calculated volume
Lactated Ringer’s solution
Monitor urine output
Hours 8-24
Remaining 50% of volume
Adjust based on response
Target urine: 0.5-1 mL/kg/hr
Day 2+
Colloid solutions
Maintenance fluids
Nutritional support
Pain Management
| Pain Type | Characteristics | Management | Nursing Considerations |
|---|---|---|---|
| Background Pain | Continuous, dull aching | Long-acting opioids NSAIDs (if appropriate) |
Regular assessment Prevention of breakthrough |
| Breakthrough Pain | Sudden, severe spikes | Short-acting opioids Immediate release medications |
Rapid intervention Document triggers |
| Procedural Pain | Associated with dressing changes | Pre-medication Topical anesthetics |
Timing of procedures Non-pharmacological methods |
Wound Care Principles
Topical Antimicrobials
- Silver sulfadiazine: Broad spectrum, good penetration
- Mafenide acetate: Deep penetration, eschar coverage
- Silver-impregnated dressings: Sustained release
- Bacitracin: Superficial burns, facial burns
Dressing Types
- Hydrocolloid: Superficial burns, low exudate
- Hydrogel: Cooling effect, pain relief
- Foam dressings: Moderate to heavy exudate
- Alginate: Heavy exudate, hemostatic properties
Memory Aid – “MOIST Wound Healing”
Maintain moist environment
Optimal temperature (body temperature)
Infection prevention
Support circulation
Tissue viability protection
Nursing Care Plans & Implementation
Priority Nursing Diagnoses
1. Impaired Skin Integrity related to thermal injury
Goals:
- Prevent infection
- Promote healing
- Minimize scarring
Interventions:
- Sterile dressing changes
- Monitor for infection signs
- Apply prescribed topicals
Evaluation:
- Wound healing progression
- Absence of infection
- Patient comfort level
2. Acute Pain related to tissue damage
Goals:
- Pain level <4/10
- Comfort during procedures
- Adequate rest/sleep
Interventions:
- Pre-medication before procedures
- Non-pharmacological methods
- Environmental modifications
Evaluation:
- Pain scale ratings
- Sleep quality
- Activity tolerance
3. Risk for Deficient Fluid Volume related to capillary leak
Goals:
- Maintain adequate perfusion
- Urine output >0.5 mL/kg/hr
- Stable vital signs
Interventions:
- Monitor I&O strictly
- Daily weights
- Assess for edema
Evaluation:
- Hemodynamic stability
- Electrolyte balance
- Tissue perfusion
Daily Nursing Assessment Checklist
Visual Assessment
- Wound appearance and size
- Signs of infection (redness, warmth, purulent drainage)
- Dressing integrity and saturation
- Surrounding skin condition
- Overall patient appearance
Physiological Assessment
- Vital signs and hemodynamic status
- Pain level and characteristics
- Urine output and fluid balance
- Respiratory status (if inhalation injury)
- Neurological status and anxiety level
Medication Administration Guidelines
| Medication Category | Examples | Nursing Considerations | Monitoring Parameters |
|---|---|---|---|
| Opioid Analgesics | Morphine, Fentanyl, Oxycodone | Assess pain before/after Monitor respiratory status Prevent constipation |
Respiratory rate Sedation level Bowel function |
| Topical Antimicrobials | Silver sulfadiazine Mafenide acetate |
Sterile application Monitor for allergic reactions Document wound response |
Wound healing Signs of sensitivity Culture results |
| Tetanus Prophylaxis | Tetanus toxoid TIG if indicated |
Verify immunization history Document administration Monitor injection site |
Local reactions Systemic symptoms Wound healing |
Clinical Pearl – Dressing Change Technique
ASEPTIC Technique:
Assemble supplies and pre-medicate patient
Sterile gloves and instruments
Evaluate wound during removal
Photo-document if protocol requires
Topical agents applied as prescribed
Instruct patient on signs of infection
Comfort measures and follow-up
Patient Education Priorities
Immediate Education
- Proper wound care techniques
- Signs and symptoms of infection
- Pain management strategies
- Activity restrictions and modifications
- When to seek emergency care
Discharge Planning
- Home wound care supplies
- Follow-up appointment scheduling
- Scar prevention and management
- Nutritional support for healing
- Psychological support resources
Complications & Management
Early Complications (0-72 hours)
Hypovolemic Shock
Pathophysiology: Massive fluid shift from intravascular to interstitial space
Signs: Hypotension, tachycardia, decreased urine output, altered mental status
Management: Aggressive fluid resuscitation, hemodynamic monitoring, vasopressors if needed
Inhalation Injury
Pathophysiology: Thermal or chemical damage to respiratory tract
Signs: Hoarseness, stridor, carbonaceous sputum, singed facial hair
Management: High-flow oxygen, early intubation, bronchoscopy, mechanical ventilation
RED FLAGS – Immediate Intervention Required
- Airway compromise: Stridor, hoarseness, difficulty swallowing
- Circumferential burns: Risk of compartment syndrome
- Electrical burns: Risk of cardiac arrhythmias, internal injuries
- Chemical burns: Ongoing tissue damage, systemic toxicity
- Signs of shock: Hypotension, oliguria, altered mental status
Late Complications (>72 hours)
| Complication | Timeline | Risk Factors | Prevention/Management |
|---|---|---|---|
| Infection/Sepsis | 3-7 days | Large TBSA, immunocompromise, poor wound care | Sterile technique, antimicrobials, early recognition |
| Contractures | Weeks to months | Joint involvement, inadequate therapy | Early mobilization, splinting, physical therapy |
| Hypertrophic Scarring | Months | Deep burns, genetic predisposition, infection | Pressure garments, silicone sheeting, massage |
| PTSD/Depression | Weeks to years | Severe burns, previous trauma, lack of support | Early psychological intervention, support groups |
Memory Aid – “SIRS Criteria for Sepsis”
Systemic inflammatory response syndrome
Increased temperature (>38°C or <36°C)
Respiratory rate >20 or PaCO2 <32
Significant changes in WBC (>12,000 or <4,000)
Plus: Tachycardia >90 bpm
Two or more criteria = SIRS
Monitoring for Complications
Daily Complication Screening Protocol
Infection
- • Temperature trends
- • WBC count
- • Wound appearance
- • Culture results
Circulation
- • Distal pulses
- • Capillary refill
- • Compartment tension
- • Doppler signals
Function
- • Range of motion
- • Sensation
- • Motor function
- • Joint mobility
Psychosocial
- • Mood assessment
- • Sleep patterns
- • Anxiety levels
- • Coping mechanisms
Special Populations
Pediatric Considerations
Anatomical Differences:
- Thinner skin – deeper burns with same exposure
- Higher surface area to body weight ratio
- Greater risk of hypothermia and fluid loss
- Modified Rule of Nines required
Management Modifications:
- More aggressive fluid resuscitation
- Temperature maintenance critical
- Family-centered care approach
- Age-appropriate pain assessment tools
Elderly Considerations
Physiological Changes:
- Delayed wound healing
- Decreased immune response
- Multiple comorbidities
- Medication interactions
Management Modifications:
- Conservative fluid management
- Comprehensive medication review
- Early nutritional intervention
- Fall prevention strategies
Pregnancy and Burns
Maternal-Fetal Considerations
- Increased plasma volume: May require modified fluid calculations
- Fetal monitoring: Continuous monitoring for burns >20% TBSA
- Positioning: Left lateral tilt to prevent supine hypotension
- Medication safety: Consider teratogenic effects of treatments
Burn Center Referral Criteria
American Burn Association Guidelines
Patient Factors
- Age <10 or >50 years
- Pre-existing medical conditions
- Pregnancy
- Immunocompromised state
Burn Characteristics
- Partial thickness >10% TBSA
- Full thickness burns
- Burns involving special areas
- Electrical/chemical burns
- Inhalation injury
Prevention Strategies
Prevention is Always Better Than Treatment
95% of burn injuries are preventable through education, environmental modifications, and safety measures. As nurses, we play a crucial role in community education and prevention.
Home Safety Measures
Scald Prevention
- Set water heater to 120°F (49°C)
- Test bath water temperature
- Supervise children during bathing
- Turn pot handles toward stove center
- Use back burners when possible
Fire Prevention
- Install smoke detectors
- Regular chimney cleaning
- Safe cigarette disposal
- Fire extinguisher accessibility
- Escape plan practice
Electrical Safety
- GFCI outlet installation
- Regular electrical inspections
- Proper extension cord use
- Child-proof outlet covers
- Professional electrical work only
Age-Specific Prevention Education
| Age Group | Primary Risks | Prevention Strategies | Education Focus |
|---|---|---|---|
| Infants (0-1 year) | Bath scalds, hot liquids | Parental supervision, temperature testing | Caregiver education |
| Toddlers (1-4 years) | Scalds, contact burns | Environmental modifications, barriers | Simple safety rules |
| School Age (5-12 years) | Flame burns, experiments | Safety education, supervision | Fire safety, “stop-drop-roll” |
| Adolescents (13-18 years) | Risk-taking behaviors | Peer education, consequences | Personal responsibility |
| Adults (19-64 years) | Workplace, cooking injuries | Safety protocols, equipment | Workplace safety training |
| Elderly (65+ years) | Decreased sensation, mobility | Environmental assessment, aids | Adaptive strategies |
Memory Aid – “SAFE HOME”
Smoke detectors installed and working
Appliance safety and maintenance
Fire extinguishers accessible
Escape plan practiced regularly
Hot water temperature controlled
Outlet covers and electrical safety
Matches and lighters secured
Education for all family members
Recovery & Rehabilitation
Phases of Recovery
Acute Phase (0-72 hours)
- • Fluid resuscitation
- • Wound stabilization
- • Pain management
- • Prevention of complications
Sub-acute Phase (3 days – healing)
- • Wound healing support
- • Early mobilization
- • Nutritional optimization
- • Infection prevention
Rehabilitation Phase (weeks-months)
- • Scar management
- • Function restoration
- • Psychological support
- • Community reintegration
Multidisciplinary Team Approach
Core Team Members
- Burn Surgeon: Surgical management, grafting
- Nursing Team: Daily care, education, coordination
- Physical Therapist: Mobility, strength, function
- Occupational Therapist: ADL training, splinting
- Dietitian: Nutritional support, wound healing
- Social Worker: Discharge planning, resources
Specialized Support
- Psychologist: Mental health, coping strategies
- Respiratory Therapist: Pulmonary support
- Chaplain: Spiritual care, family support
- Child Life Specialist: Pediatric emotional support
- Prosthetist: Adaptive devices, prosthetics
- Pharmacist: Medication optimization
Scar Prevention and Management
| Intervention | Mechanism | Application | Expected Outcomes |
|---|---|---|---|
| Pressure Garments | Mechanical pressure reduces collagen formation | 23 hours/day for 12-18 months | Reduced hypertrophy, improved texture |
| Silicone Sheeting | Hydration and pressure effects | 12+ hours daily, replace weekly | Softer, flatter scars |
| Massage Therapy | Breaks up scar tissue, improves circulation | Daily, 15-20 minutes per area | Improved flexibility, reduced contracture |
| Splinting/Positioning | Maintains tissue length, prevents contracture | Night splints, positioning devices | Preserved range of motion |
Rehabilitation Success Factors
“PROGRESS” Framework:
Patient motivation and engagement
Regular therapy participation
Optimal nutrition and hydration
Goal-oriented treatment plans
Range of motion maintenance
Early intervention initiation
Support system involvement
Scar prevention measures
Long-term Follow-up Care
Follow-up Schedule
- Weekly for first month
- Bi-weekly for second month
- Monthly for 6 months
- Quarterly for first year
- Annually thereafter
- PRN for complications
Assessment Areas
- Wound healing progression
- Scar maturation and appearance
- Range of motion and function
- Pain levels and management
- Psychological adjustment
- Quality of life measures
Additional Resources & References
Professional Organizations
- American Burn Association (ABA)
Guidelines, research, education resources - International Association for the Study of Pain (IASP)
Pain management protocols - Wound Healing Society
Evidence-based wound care practices - American Academy of Dermatology
Skin care and scar management
Patient Support Resources
- Phoenix Society for Burn Survivors
Peer support, educational programs - Burn Survivor Resource Center
Recovery information, community support - National Burn Repository
Statistics and outcome data - Local burn support groups
Community-based peer networks
Quick Review – “BURNS CARE” Essentials
Burn depth and size assessment
Understanding pathophysiology
Resuscitation and fluid management
Nursing care planning and implementation
Safety measures and prevention
Complications recognition and management
Assessment using systematic approach
Rehabilitation and recovery support
Education for patients and families
Key Takeaways for Nursing Practice
- First aid is critical: Proper cooling and initial care can significantly impact outcomes
- Assessment drives treatment: Accurate TBSA and depth evaluation guides management decisions
- Prevention is paramount: Education and safety measures prevent most burn injuries
- Holistic care matters: Address physical, psychological, and social needs
- Team approach works: Multidisciplinary collaboration improves outcomes
- Recovery is a journey: Long-term support and follow-up are essential
- Continuous learning: Stay updated with evidence-based practices and guidelines
Final Clinical Pearl
Remember that burn care is not just about treating the wound – it’s about caring for the whole person. Every burn survivor has a story, fears, hopes, and dreams. As nurses, we have the privilege and responsibility to provide not just clinical expertise, but also compassion, hope, and support throughout their healing journey.