First Aid Management of Stings
Comprehensive Evidence-Based Nursing Guide
Based on 2024 AHA/Red Cross Guidelines & Best Practice Evidence
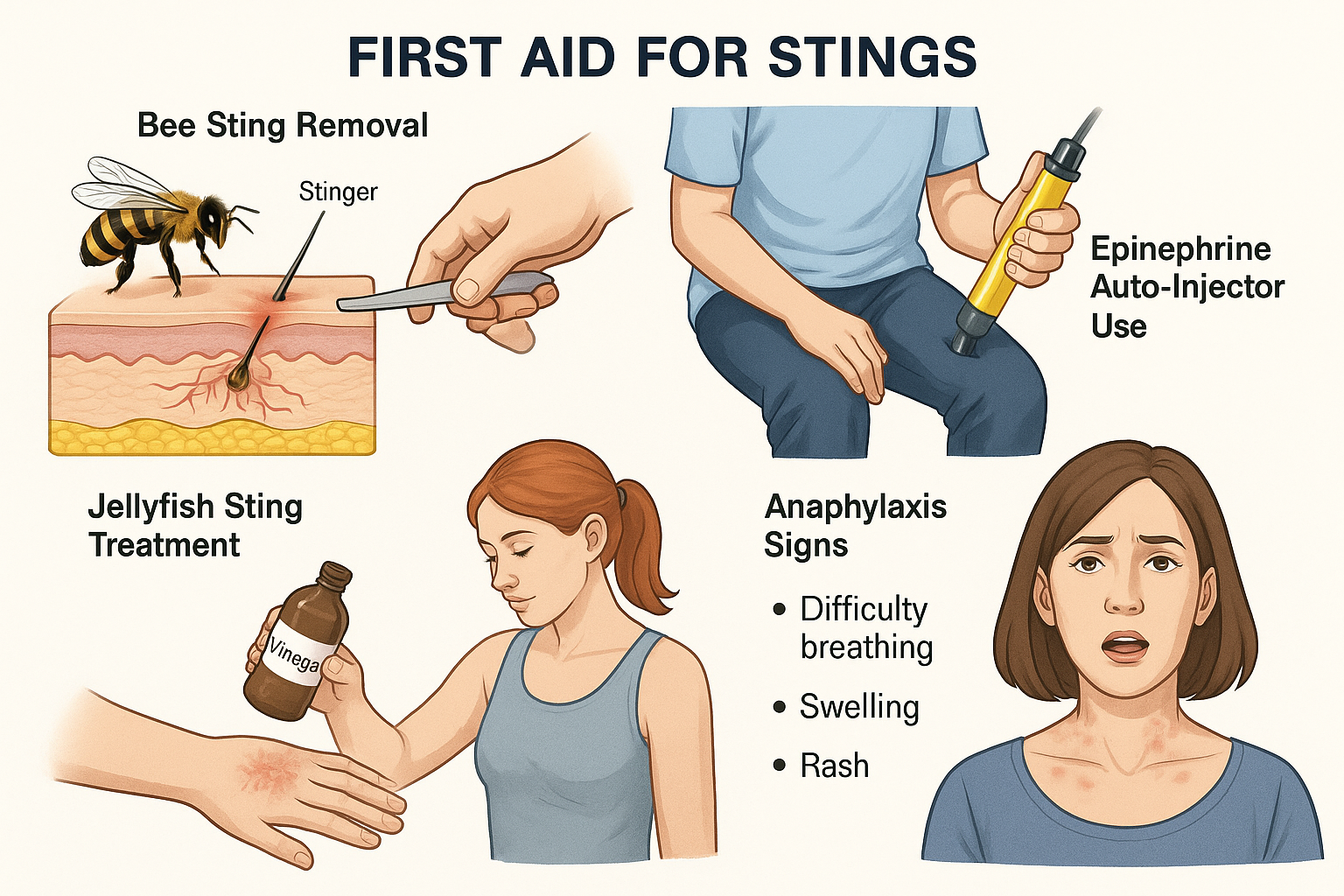
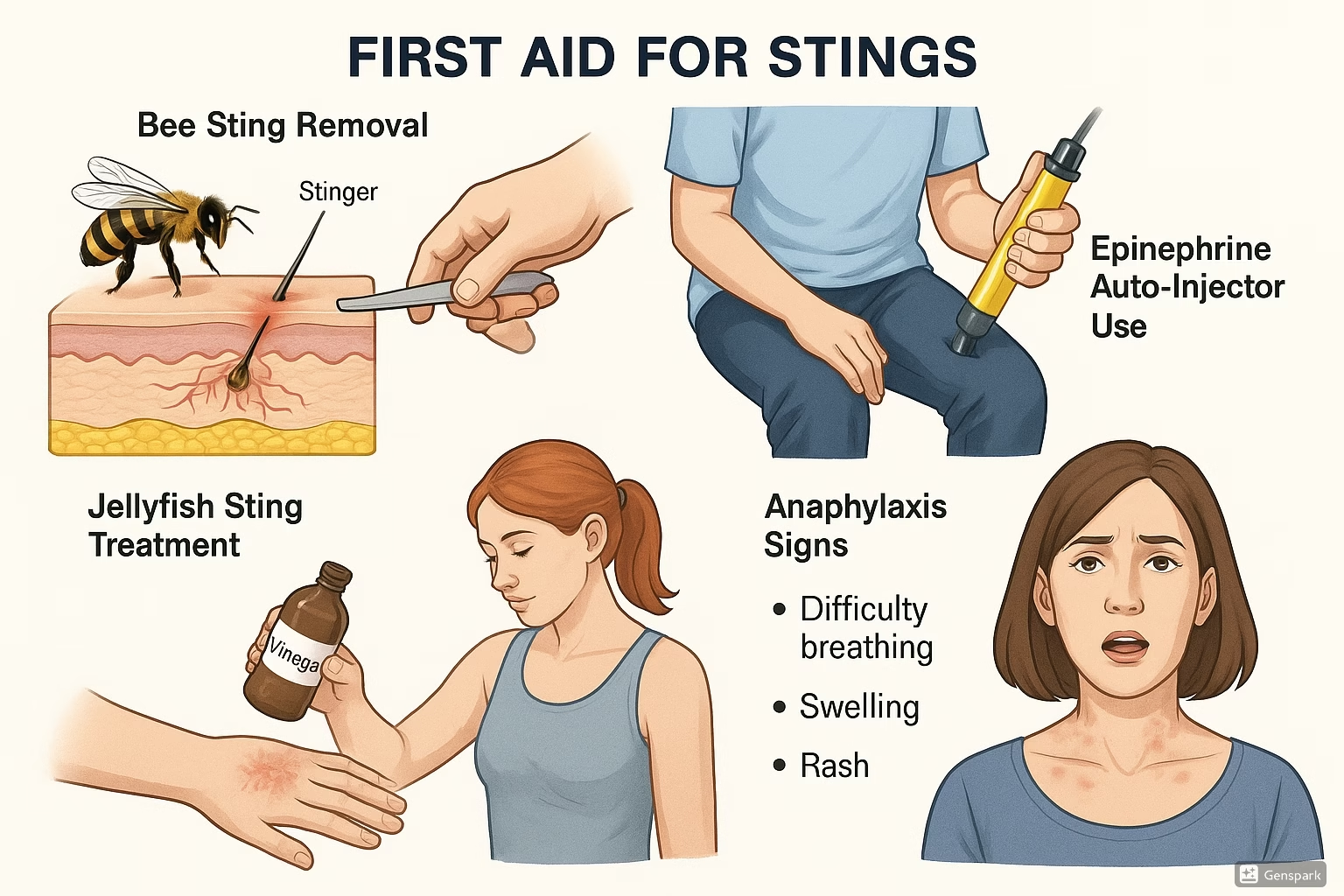
Figure 1: Comprehensive overview of first aid management techniques for various types of stings
Table of Contents
Introduction & Learning Objectives
Sting injuries represent a significant clinical challenge in emergency and community healthcare settings. As a nurse, your immediate response to sting-related emergencies can be life-saving, particularly when anaphylaxis develops. This comprehensive guide provides evidence-based protocols for managing all types of stings, from common insect encounters to dangerous marine envenomations.
Clinical Significance
- • Over 2 million emergency department visits annually involve sting-related injuries
- • Anaphylaxis occurs in 0.4-0.8% of the population following hymenoptera stings
- • Mortality rate from untreated anaphylaxis can reach 10-20%
- • Early intervention reduces complications by 85%
Learning Objectives
Pathophysiology of Stings & Envenomation
Understanding the Biological Response
Sting injuries involve complex interactions between venom components, immune system responses, and local tissue reactions. Understanding these mechanisms is crucial for effective nursing intervention.
Venom Components
Biogenic Amines
Histamine, serotonin, acetylcholine – cause immediate pain, swelling, and vasodilation
Enzymes
Phospholipase A2, hyaluronidase – enhance venom spread and tissue damage
Peptides & Proteins
Melittin, mastoparan – cause cell membrane disruption and hemolysis
Immune Response Cascade
Memory Aid: “STING” Pathophysiology
Hymenoptera Stings (Bees, Wasps, Hornets)
Most Common Sting Emergencies
Hymenoptera stings account for over 90% of sting-related emergency visits. Proper identification and immediate management are essential for preventing serious complications.
Honeybees
- • Barbed stinger remains in skin
- • Single sting per bee (bee dies)
- • Continued venom injection for 45-60 seconds
- • Less aggressive unless threatened
Wasps
- • Smooth stinger, no barbs
- • Can sting multiple times
- • More aggressive behavior
- • Higher venom concentration
Hornets
- • Largest hymenoptera
- • Most potent venom
- • Can inject larger quantities
- • Highest anaphylaxis risk
First Aid Protocol for Hymenoptera Stings
Scene Safety & Assessment
Ensure scene safety, check for multiple stings, assess patient consciousness and breathing. Look for signs of allergic reaction.
Stinger Removal (Bees Only)
Scrape stinger out with fingernail, credit card, or knife edge. DO NOT use tweezers or pinch – this injects more venom.
Immediate Wound Care
Clean area gently with soap and water. Apply cold compress for 15-20 minutes to reduce swelling and pain.
Monitor for Allergic Reaction
Watch for signs of anaphylaxis: difficulty breathing, swelling of face/throat, rapid pulse, dizziness, widespread rash.
Symptomatic Treatment
Administer oral antihistamine (diphenhydramine 25-50mg) for local reactions. Apply topical calamine or hydrocortisone cream.
RED FLAGS – Call 911 Immediately
- Difficulty breathing or wheezing
- Swelling of face, lips, tongue, or throat
- Rapid pulse or palpitations
- Dizziness or fainting
- Widespread rash or hives
- Nausea, vomiting, or diarrhea
- Multiple stings (>10-15)
- Previous severe allergic reaction
Marine Envenomations
Ocean’s Hidden Dangers
Marine stings present unique challenges due to diverse venom compositions, environmental factors, and limited access to definitive care. Geographic location significantly impacts treatment protocols.
Common Marine Stingers
Jellyfish (Cnidarians)
Box jellyfish, Portuguese man-of-war, sea nettle, moon jelly
Venomous Fish
Stingray, stonefish, lionfish, catfish
Other Marine Life
Blue-ringed octopus, cone snail, sea urchin
High-Risk Species
Box Jellyfish (Chironex fleckeri)
Most venomous marine animal – can cause cardiac arrest within minutes
Blue-ringed Octopus
Neurotoxic venom causing paralysis and respiratory failure
Stonefish
Extremely painful sting, can cause tissue necrosis
Marine Sting First Aid Protocol
Jellyfish Stings
Remove victim from water safely
DO NOT rub area or apply fresh water
Remove tentacles with tweezers (not bare hands)
Rinse with vinegar for 30 seconds (deactivates nematocysts)
Apply hot water (113°F/45°C) for 20 minutes
Venomous Fish Stings
Control bleeding with direct pressure
Remove visible spine fragments (if easy to access)
Irrigate wound with saline or clean seawater
Immerse in hot water (113°F/45°C) for 30-90 minutes
Transport to emergency care for tetanus prophylaxis
Memory Aid: “MARINE” Treatment Protocol
Arthropod Bites & Stings
Beyond the Obvious
Arthropod envenomations include spiders, scorpions, and other arachnids. While most are benign, certain species require immediate medical intervention due to neurotoxic or necrotizing venom effects.
Spiders
Black Widow
Neurotoxic – muscle cramps, hypertension
Brown Recluse
Cytotoxic – tissue necrosis, systemic illness
Most Others
Local reaction only – supportive care
Scorpions
- • Most cause local pain only
- • Bark scorpion – neurotoxic
- • Children at higher risk
- • Antivenom available for severe cases
Other Insects
- • Fire ants – multiple stings
- • Mosquitoes – disease vectors
- • Ticks – Lyme disease risk
- • Bedbugs – delayed reactions
Arthropod Bite Assessment & Management
Assessment Priorities
Identify the arthropod if possible
Take photo, collect specimen safely
Document bite characteristics
Size, appearance, pattern, location
Monitor systemic symptoms
Neurological, cardiovascular, respiratory
Treatment Approach
Local wound care
Clean, cold compress, elevate if possible
Pain management
Oral analgesics, topical anesthetics
Monitor for complications
Secondary infection, necrosis, systemic toxicity
Anaphylaxis Recognition & Management
Life-Threatening Emergency
Anaphylaxis is a severe, potentially fatal allergic reaction requiring immediate recognition and treatment. Epinephrine is the first-line treatment and should be administered without delay when anaphylaxis is suspected.
Recognition Signs
Respiratory
- • Shortness of breath, wheezing
- • Stridor, voice changes
- • Throat tightness or swelling
Cardiovascular
- • Tachycardia, hypotension
- • Dizziness, syncope
- • Chest pain, palpitations
Dermatologic
- • Generalized urticaria
- • Facial/lip/tongue swelling
- • Flushing, pruritus
Gastrointestinal
- • Nausea, vomiting
- • Diarrhea, cramping
- • Metallic taste
Epinephrine Administration
Dosing Guidelines
Adults: 0.3-0.5 mg IM (EpiPen/auto-injector)
Children: 0.15 mg IM (EpiPen Jr.)
Infants: 0.01 mg/kg IM (max 0.15 mg)
Auto-injector Technique
Anaphylaxis Management Protocol
1 Immediate Actions
- • Call 911 immediately
- • Administer epinephrine
- • Position patient supine
- • Establish IV access
2 Secondary Treatment
- • H1 antihistamine (diphenhydramine)
- • H2 blocker (ranitidine)
- • Corticosteroids (methylprednisolone)
- • Bronchodilators if wheezing
3 Ongoing Care
- • Monitor vital signs closely
- • Prepare for biphasic reaction
- • Consider ICU admission
- • Discharge planning & education
Memory Aid: “FAST-ED” Anaphylaxis Assessment
Nursing Assessment & Documentation
Comprehensive Patient Assessment
Thorough assessment and accurate documentation are essential for optimal patient outcomes and legal protection. Use systematic approaches to ensure nothing is missed.
Primary Assessment
A – Airway
- • Patency, stridor, voice changes
- • Visible swelling of lips, tongue, throat
- • Ability to swallow, drooling
B – Breathing
- • Respiratory rate, effort, pattern
- • Wheezing, crackles, diminished sounds
- • Oxygen saturation, cyanosis
C – Circulation
- • Blood pressure, pulse quality/rate
- • Capillary refill, skin color
- • Level of consciousness
Focused Assessment
Sting Site Examination
• Location, size, appearance
• Presence of stinger or foreign body
• Local swelling, erythema, warmth
• Pain level (0-10 scale)
Systemic Assessment
• Skin changes (rash, hives)
• Neurological status
• Gastrointestinal symptoms
• Previous allergic reactions
History Taking
• Time of sting occurrence
• Type of insect/marine life
• Number of stings
• Current medications
Documentation Requirements
Essential Elements
Date, time, and circumstances
Exact timing helps track symptom progression
Objective assessment findings
Vital signs, physical exam, pain scores
Interventions performed
Medications given, procedures done
Patient response to treatment
Improvement, deterioration, or no change
Legal Considerations
Contemporaneous notes
Document in real-time when possible
Objective language
Avoid subjective interpretations
Complete accuracy
Never alter records; use addendums
Signature and credentials
Include your name, title, and license number
Nursing Interventions & Care Plans
Evidence-Based Nursing Care
Nursing interventions for sting injuries focus on symptom management, complication prevention, and patient education. Care plans must be individualized based on patient assessment and response to treatment.
Priority Diagnoses
Ineffective Airway Clearance
Related to laryngeal edema
Decreased Cardiac Output
Related to vasodilation/shock
Acute Pain
Related to venom effects
Patient Outcomes
• Patent airway maintained
• Vital signs stable
• Pain controlled (≤3/10)
• No signs of infection
• Patient educated on prevention
Key Interventions
• Continuous monitoring
• Medication administration
• Wound care
• Patient education
• Discharge planning
Medication Administration Guidelines
| Medication | Indication | Dose | Nursing Considerations |
|---|---|---|---|
| Epinephrine | Anaphylaxis | 0.3-0.5mg IM | Monitor BP, HR; may repeat q5-15min |
| Diphenhydramine | Allergic reaction | 25-50mg PO/IV | Causes drowsiness; avoid in elderly |
| Methylprednisolone | Severe reaction | 1-2mg/kg IV | Monitor glucose; slow onset |
| Albuterol | Bronchospasm | 2.5mg nebulized | Monitor for tachycardia |
Memory Aid: “NURSE” Intervention Framework
Clinical Implementation & Best Practices
Excellence in Practice
Implementing evidence-based protocols for sting management requires systematic approaches, interdisciplinary collaboration, and continuous quality improvement. Your role as a nurse is pivotal in achieving optimal patient outcomes.
Healthcare Settings
Emergency Department
- • Rapid triage and assessment
- • Immediate access to resuscitation equipment
- • 24/7 physician availability
- • Advanced monitoring capabilities
Urgent Care Centers
- • Limited hours of operation
- • Basic monitoring equipment
- • Stabilize and transfer severe cases
- • Good for minor reactions
Community/School Settings
- • First aid protocols essential
- • EpiPen availability crucial
- • Early recognition training needed
- • Rapid EMS activation
Team-Based Approach
Physician Role
Diagnosis, treatment orders, advanced interventions, disposition decisions
Nursing Role
Assessment, monitoring, medication administration, patient education, coordination
Pharmacy Role
Medication verification, dosing recommendations, drug interaction screening
Patient/Family Role
Accurate history, treatment compliance, follow-up care, prevention strategies
Patient Education Priorities
Prevention Strategies
- • Avoid known allergens
- • Wear protective clothing outdoors
- • Use insect repellents
- • Avoid bright colors and perfumes
- • Stay calm around stinging insects
- • Check for nests around home
EpiPen Instructions
- • Always carry two auto-injectors
- • Check expiration dates monthly
- • Store at room temperature
- • Practice using trainer device
- • Teach family members technique
- • Call 911 after using EpiPen
When to Seek Help
- • Any breathing difficulty
- • Swelling of face/throat
- • Rapid pulse or dizziness
- • Widespread rash or hives
- • Nausea, vomiting, diarrhea
- • Previous severe reactions
Quality Improvement Metrics
Time Metrics
Door-to-epinephrine time, assessment completion time
Outcome Metrics
Patient survival, complication rates, readmissions
Education Metrics
Patient satisfaction, knowledge retention, compliance
Process Metrics
Protocol adherence, documentation completeness
References & Resources
Evidence-Based Practice
This guide is based on current evidence-based guidelines and best practices from leading healthcare organizations. Continue your learning with these authoritative resources.
Primary References
2024 AHA/Red Cross Guidelines
First Aid Guidelines for Envenomation from Tick Bites and Bee, Wasp and Ant Stings
View GuidelinesMayo Clinic Resources
Evidence-based treatment protocols for bee stings and insect bites
Access ResourceBMJ Best Practice
Clinical decision support for insect bites and stings management
Clinical GuidelinesAdditional Resources
Nursing Education Resources
Specialized nursing care plans and educational materials
Nursing ResourcesContinuing Education
Certification Programs
Advanced life support, emergency nursing, allergy/immunology
Professional Organizations
ENA, AACN, AAAI – networking and resources
Conferences & Workshops
Annual meetings, webinars, skills training sessions
Your Expertise Saves Lives
As a nurse, your knowledge and quick thinking in sting emergencies can mean the difference between life and death for your patients.
Stay current with guidelines, practice your skills regularly, and always prioritize patient safety and evidence-based care.