Levels of Prevention & Health Problems of India
Comprehensive Nursing Notes
Table of Contents
Introduction to Levels of Prevention
Prevention is a cornerstone of public health nursing practice that aims to promote health, preserve health, and restore health when it is impaired. Understanding the different levels of prevention is crucial for nurses to implement effective interventions across the healthcare continuum.
Definition
Levels of prevention are a framework categorizing healthcare interventions based on the stage at which they are implemented in the natural history of disease. This concept, originally developed by Leavell and Clark in 1965, outlines how healthcare providers can intervene at different stages to prevent disease onset, progression, or complications.
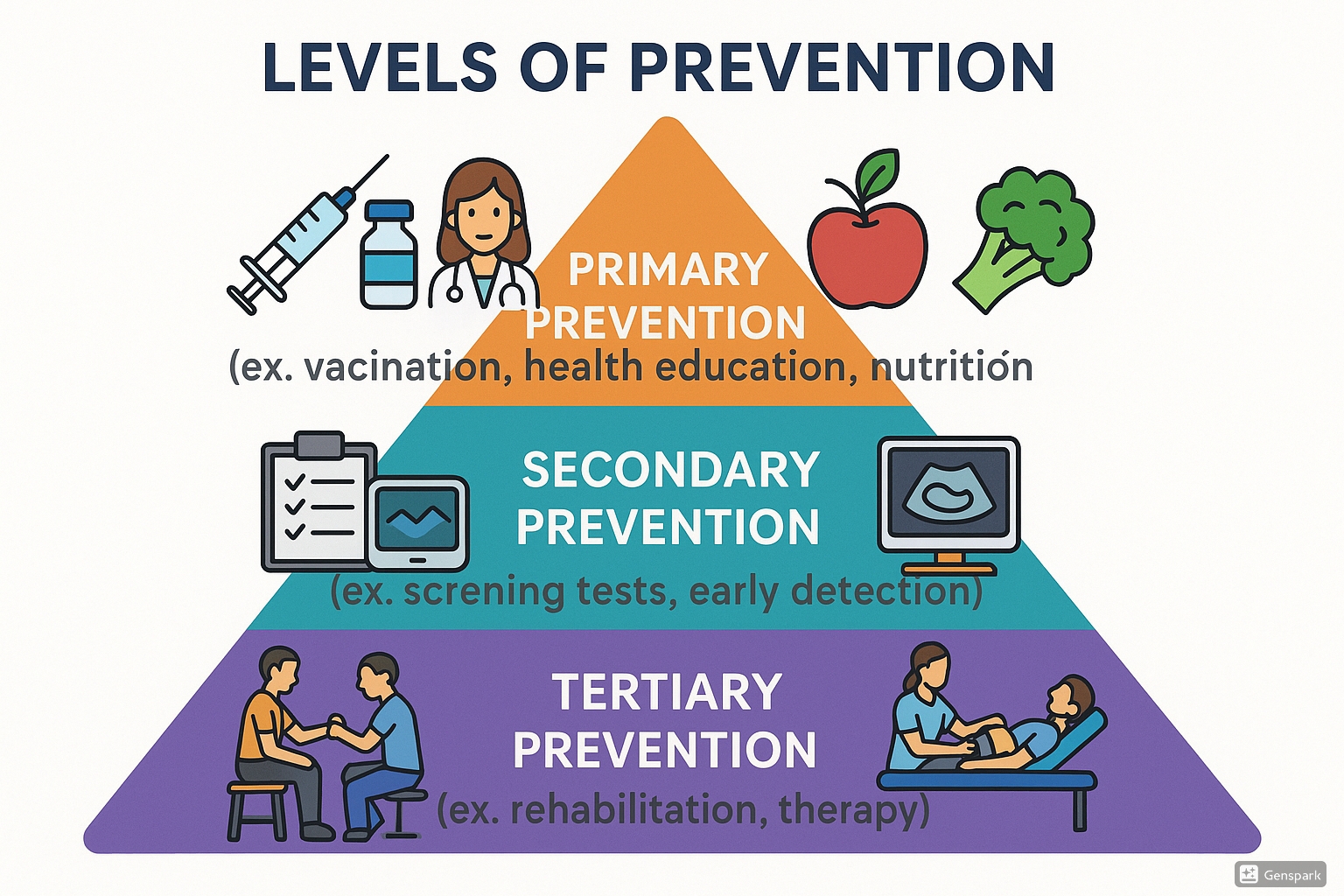
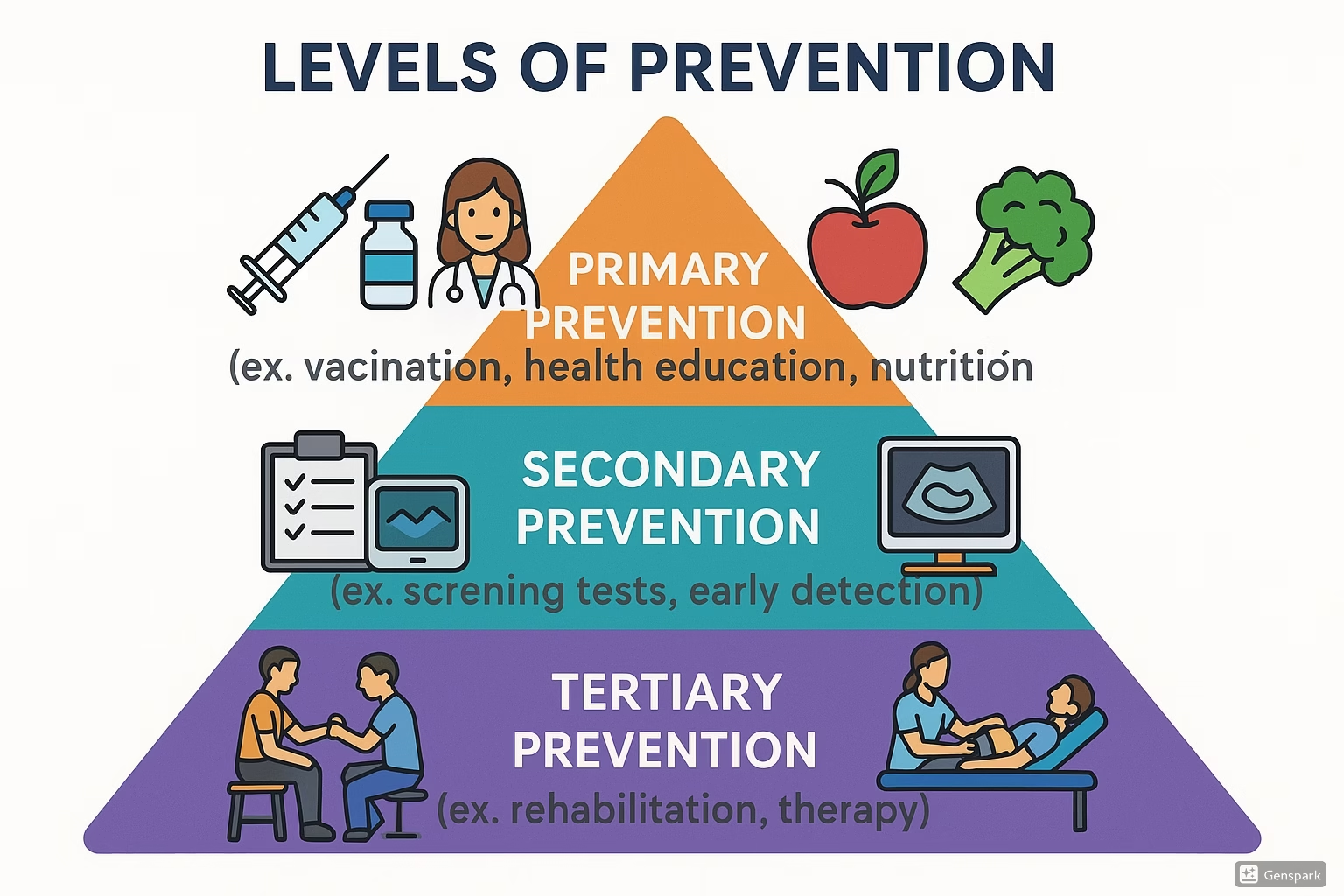
Figure 1: The Three Levels of Prevention in Healthcare
Classification of Prevention Levels
Prevention in healthcare is traditionally classified into three distinct levels:
- Primary Prevention: Aims to prevent disease before it occurs by reducing exposure to risk factors or increasing resistance.
- Secondary Prevention: Focuses on early detection and intervention to reduce the impact of a disease that has already begun.
- Tertiary Prevention: Targets the management of established disease to minimize disability and complications.
Some modern classifications also include:
- Primordial Prevention: Addressing the most fundamental societal and environmental conditions that contribute to disease.
- Quaternary Prevention: Protecting individuals from unnecessary medical interventions and their potential harm.
Key Principles of Prevention:
- Prevention is more effective and cost-efficient than treatment
- Different levels of prevention can be implemented simultaneously
- Prevention strategies must be culturally appropriate and context-specific
- Nurses play vital roles across all prevention levels
- Prevention approaches should be evidence-based and regularly evaluated
Level 1Primary Prevention
Definition
Primary prevention includes measures that prevent the onset of disease by removing its causes or increasing resistance to disease. It is implemented before the disease process begins and aims to prevent the occurrence of disease or injury altogether.
Goals of Primary Prevention
- Prevent disease or injury before it occurs
- Reduce or eliminate causative risk factors
- Promote health and well-being
- Build resistance through improved health status
- Create environments conducive to optimal health
Types of Primary Prevention Interventions
| Type | Examples | Nursing Role |
|---|---|---|
| Health Education | Nutritional counseling, hygiene education, sex education | Develop and implement educational programs, counsel patients |
| Specific Protection | Immunization, use of specific nutrients, chemoprophylaxis | Administer vaccines, educate about preventive medications |
| Environmental Measures | Safe water supply, air pollution control, waste disposal | Advocate for healthy environments, educate about environmental hazards |
| Lifestyle Modifications | Physical activity promotion, smoking cessation, stress management | Provide counseling, facilitate behavior change programs |
| Chemoprophylaxis | Iron supplements for pregnant women, antimalarial drugs | Prescribe/administer prophylactic medications, monitor for effectiveness |
Primary Prevention Strategies in India
In the Indian context, primary prevention takes on special significance due to the country’s diverse population, socioeconomic disparities, and disease burden. Key primary prevention strategies include:
Universal Immunization Program (UIP)
Provides free vaccines against preventable diseases like tuberculosis, polio, diphtheria, tetanus, pertussis, measles, hepatitis B, and more recently, rotavirus and pneumococcal diseases.
National Nutrition Mission (POSHAN Abhiyaan)
Aims to reduce malnutrition through improved monitoring, convergence, targeting of essential nutrition interventions, and community mobilization.
National Tobacco Control Programme
Works to reduce tobacco consumption through public awareness, smoke-free laws, and cessation services to prevent associated diseases like cancer and cardiovascular conditions.
Swachh Bharat Mission
Focuses on improving sanitation infrastructure and practices to prevent water and sanitation-related diseases that contribute significantly to India’s disease burden.
Key Nursing Activities in Primary Prevention:
- Conducting health education sessions in communities
- Administering vaccines in immunization clinics
- Screening for risk factors (pre-disease)
- Implementing maternal and child health programs
- Promoting lifestyle modifications for chronic disease prevention
- Participating in school health programs
- Conducting home visits for health promotion
Primary Prevention Case Example
Scenario: A community health nurse in rural Rajasthan is working to prevent iron-deficiency anemia among adolescent girls.
Primary Prevention Interventions:
- Conducting nutritional education sessions in schools about iron-rich foods
- Distributing weekly iron and folic acid supplements (WIFS) to adolescent girls
- Training Anganwadi workers to counsel families on diverse diets
- Organizing cooking demonstrations using locally available iron-rich foods
- Educating about inhibitors and enhancers of iron absorption in diet
Outcome: Reduced incidence of new anemia cases in the community, improved hemoglobin levels, and enhanced knowledge about nutrition.
Level 2Secondary Prevention
Definition
Secondary prevention involves early detection and prompt treatment of disease to prevent its progression. These interventions are implemented after the disease process has begun but before it causes significant symptoms or disability, with the goal of halting or slowing its progress.
Goals of Secondary Prevention
- Early detection of disease through screening
- Prompt intervention to prevent disease progression
- Reduction of disease severity and complications
- Limiting disability and preventing premature death
- Shortening the course of illness
Types of Secondary Prevention Interventions
| Type | Examples | Nursing Role |
|---|---|---|
| Screening Programs | Mammography, Pap smears, blood pressure monitoring, diabetes screening | Conduct screenings, educate patients about screening importance |
| Case Finding | Contact tracing for TB or STIs, high-risk population screening | Identify at-risk individuals, facilitate screening, follow-up |
| Early Diagnosis | Diagnostic tests, clinical examinations, symptom assessment | Assist with diagnostic procedures, analyze test results |
| Prompt Treatment | Early antibiotic therapy, early management of chronic diseases | Administer treatments, monitor effectiveness, adjust care plans |
| Limiting Disability | Early stroke management, acute cardiac care | Implement evidence-based protocols, monitor for complications |
Secondary Prevention Programs in India
India has implemented several secondary prevention initiatives to address its significant disease burden. Some key programs include:
National Program for Prevention and Control of Cancer, Diabetes, CVD and Stroke (NPCDCS)
Provides opportunistic screening for common NCDs at various healthcare facilities, enabling early detection and management.
Revised National Tuberculosis Control Program (RNTCP)
Implements active case finding for TB through sputum microscopy and newer diagnostic technologies like GeneXpert, ensuring early treatment initiation.
National AIDS Control Program (NACP)
Conducts HIV screening through Integrated Counseling and Testing Centers (ICTCs), targeting early diagnosis and antiretroviral therapy initiation.
National Programme for Control of Blindness and Visual Impairment
Conducts screening for cataracts, glaucoma, and other eye conditions to identify and treat problems before vision loss occurs.
Key Nursing Activities in Secondary Prevention:
- Conducting screening camps in communities
- Performing health assessments to detect early disease
- Educating patients about the importance of screening
- Referring patients for diagnostic tests
- Administering and monitoring early treatments
- Teaching patients about self-monitoring techniques
- Following up with patients after diagnosis
Secondary Prevention Case Example
Scenario: A staff nurse at a primary health center in Tamil Nadu is working with the NPCDCS program to address cardiovascular disease.
Secondary Prevention Interventions:
- Conducting blood pressure screening for adults over 30 visiting the health center
- Performing random blood glucose tests for early diabetes detection
- Identifying individuals with hypertension and initiating prompt treatment
- Teaching newly diagnosed hypertensive patients about medication adherence
- Organizing follow-up visits to monitor treatment effectiveness
Outcome: Early detection of hypertension and diabetes, reduced complications, and improved management of identified cases.
Level 3Tertiary Prevention
Definition
Tertiary prevention focuses on managing established disease and preventing further complications, disability, or deterioration. It aims to improve quality of life for patients with chronic or complex conditions through rehabilitation, proper disease management, and disability limitation.
Goals of Tertiary Prevention
- Prevent complications of established disease
- Slow disease progression and prevent recurrence
- Rehabilitate to maximum functional capacity
- Improve quality of life despite disease
- Reduce disability and dependency
Types of Tertiary Prevention Interventions
| Type | Examples | Nursing Role |
|---|---|---|
| Rehabilitation | Physical therapy after stroke, cardiac rehabilitation, occupational therapy | Coordinate rehabilitation services, provide supportive care |
| Disease Management | Medication regimens for chronic diseases, wound care for diabetic foot ulcers | Administer treatments, educate on self-management, monitor efficacy |
| Support Services | Support groups, palliative care, counseling | Facilitate support groups, provide counseling, coordinate services |
| Adaptive Technology | Prosthetics, home modifications, assistive devices | Assess need for adaptive technology, train in proper use |
| Long-term Care | Nursing home care, home health services | Provide skilled nursing care, coordinate interdisciplinary teams |
Tertiary Prevention Programs in India
Tertiary prevention in India focuses on managing the growing burden of chronic diseases and disabilities. Key initiatives include:
National Mental Health Programme
Provides rehabilitation services and continuity of care for patients with severe mental illnesses, focusing on community integration and reducing disability.
National Programme for Health Care of the Elderly (NPHCE)
Offers specialized geriatric care, rehabilitation services, and management of age-related chronic conditions to improve quality of life.
District Disability Rehabilitation Centers (DDRCs)
Provides comprehensive rehabilitation services including physiotherapy, occupational therapy, speech therapy, and assistive devices for persons with disabilities.
National Programme for Prevention and Control of Cancer, Diabetes, CVD and Stroke (NPCDCS)
In addition to screening, includes tertiary components for management of complications and rehabilitation after events like stroke.
Key Nursing Activities in Tertiary Prevention:
- Providing skilled nursing care for complex conditions
- Training patients and families in self-management techniques
- Coordinating rehabilitation services
- Managing chronic disease complications
- Providing palliative care for advanced diseases
- Conducting home visits for disabled patients
- Facilitating support groups for chronic conditions
Tertiary Prevention Case Example
Scenario: A rehabilitation nurse at a district hospital in Maharashtra is caring for a 58-year-old patient who recently had a stroke with resulting left-sided hemiparesis.
Tertiary Prevention Interventions:
- Implementing a comprehensive rehabilitation program including physical therapy
- Training the patient in activities of daily living with modified techniques
- Educating the family about home modifications to prevent falls
- Managing anti-hypertensive and anti-platelet medications to prevent recurrence
- Conducting regular assessments to monitor functional improvement
- Connecting the patient with stroke support group resources
Outcome: Improved functional ability, prevention of complications like contractures, reduced risk of recurrence, and enhanced quality of life despite disability.
Health Problems Profile of India
India faces a complex health challenge characterized by the triple burden of disease: communicable diseases, non-communicable diseases (NCDs), and emerging health threats. Understanding this health profile is essential for nurses to implement appropriate prevention strategies.
Current Health Indicators (2024-2025)
Communicable Diseases
Despite progress, communicable diseases continue to contribute significantly to India’s disease burden:
Tuberculosis
India accounts for about 27% of the global TB burden. In 2024, TB remains a major public health challenge with approximately 2.8 million cases annually and efforts to achieve TB elimination by 2025 ongoing.
Vector-borne Diseases
Malaria, dengue, chikungunya, and Japanese encephalitis remain endemic in many states. Climate change and urbanization have altered vector distribution patterns, creating new challenges for control efforts.
Diarrheal Diseases
Contribute to about 10% of deaths in children under five years. Despite improvements in sanitation through initiatives like Swachh Bharat, diarrheal diseases continue to cause significant morbidity.
Respiratory Infections
Acute respiratory infections remain a leading cause of mortality in children under five. Air pollution in urban areas exacerbates respiratory conditions, particularly during winter months.
Non-communicable Diseases
NCDs now account for approximately 60% of all deaths in India, creating a massive public health challenge:
Cardiovascular Diseases
Leading cause of mortality in India, accounting for approximately 28.1% of all deaths. Hypertension prevalence is around 25-30% in urban adults and 12-17% in rural adults as of 2024.
Diabetes
Estimated to affect 77 million individuals (2024 data), with many cases undiagnosed. Prevalence has been rising rapidly, particularly in urban areas where it ranges from 10-15% of adults.
Cancer
India reports approximately 1.39 million new cancer cases annually. Oral, breast, cervical, and lung cancers are among the most common types, with tobacco use being a significant risk factor.
Chronic Respiratory Diseases
Chronic obstructive pulmonary disease (COPD) and asthma affect millions, accounting for about 11% of total deaths. Air pollution is a major contributing factor, especially in urban areas.
Maternal and Child Health
Significant improvements have been made, but challenges remain:
Maternal Mortality
Maternal Mortality Ratio (MMR) has declined to 97 per 100,000 live births as of 2024, but significant state-level disparities persist. Leading causes include hemorrhage, hypertensive disorders, and sepsis.
Infant and Child Mortality
Infant Mortality Rate (IMR) is approximately 28 per 1,000 live births (2024), with neonatal mortality accounting for about two-thirds of infant deaths. Prematurity, birth asphyxia, and infections are major causes.
Malnutrition
Despite the National Nutrition Mission, about 35% of children under five are stunted, 17% are wasted, and 33% are underweight. Iron-deficiency anemia affects over 50% of women and children.
Immunization
Full immunization coverage has improved to approximately 76% nationwide, but pockets of low coverage persist in specific states and among marginalized populations.
Emerging Health Concerns
Several emerging health issues require focused prevention efforts:
Mental Health
Approximately 14% of India’s population suffers from mental health conditions. Depression, anxiety disorders, and substance abuse are prevalent, yet services remain limited with significant treatment gaps.
Road Traffic Injuries
India accounts for about 11% of global road traffic deaths, with over 150,000 fatalities annually. Young adults aged 15-49 years are disproportionately affected.
Antimicrobial Resistance
Emerging as a critical health security threat due to inappropriate antibiotic use. Studies indicate high resistance rates for common pathogens, complicating treatment of infections.
Air Pollution
A major environmental health risk, contributing to respiratory diseases, cardiovascular conditions, and cancer. In 2024, 9 of the 10 most polluted cities globally were in India.
Regional Health Disparities
Significant variations exist in health indicators across states and between rural and urban areas:
- Southern states like Kerala, Tamil Nadu, and Karnataka generally have better health indicators than northern and central states.
- Urban areas have better access to healthcare facilities but face challenges related to lifestyle diseases and pollution.
- Rural areas continue to struggle with access to quality healthcare, with shortages of skilled healthcare providers.
- Tribal and remote populations face disproportionate health burdens and limited healthcare access.
Key Challenges in India’s Healthcare System:
- Inadequate healthcare infrastructure, particularly in rural areas
- Shortage of trained healthcare professionals, especially specialists
- High out-of-pocket expenditure on healthcare (approximately 63% of total health spending)
- Urban-rural divide in healthcare access and quality
- Implementation gaps in health programs despite comprehensive policies
- Limited health insurance coverage (only about 30% of the population has some form of health insurance)
Nursing Interventions Across Prevention Levels in India
Nurses play a pivotal role in implementing preventive strategies across all three levels within the Indian healthcare context. The following interventions address India’s specific health challenges:
Primary Prevention Nursing Interventions
| Health Problem | Nursing Interventions | Implementation Strategy |
|---|---|---|
| Cardiovascular Disease |
|
Conduct community-based screening camps; organize health education sessions in schools and workplaces; provide dietary counseling using locally available foods |
| Malnutrition |
|
Partner with Anganwadi workers; conduct home visits for pregnant women; demonstrate proper breastfeeding techniques; integrate with ICDS program activities |
| Vaccine-Preventable Diseases |
|
Conduct routine immunization sessions; organize outreach camps for remote areas; address vaccine hesitancy through culturally appropriate education; maintain vaccination records |
| Vector-borne Diseases |
|
Conduct door-to-door education; organize community clean-up drives; demonstrate proper water storage practices; collaborate with local government for source reduction |
| Tobacco-related Diseases |
|
Establish tobacco cessation clinics at health centers; train peer educators; use visual aids showing health impacts; advocate for tobacco-free zones |
Secondary Prevention Nursing Interventions
| Health Problem | Nursing Interventions | Implementation Strategy |
|---|---|---|
| Diabetes |
|
Organize regular screening camps; train ASHAs for glucose monitoring; teach patients foot self-examination; maintain diabetes registries for follow-up |
| Hypertension |
|
Establish hypertension clinics; provide BP monitoring cards; train patients in home BP monitoring; ensure regular follow-up through reminder systems |
| Tuberculosis |
|
Train in proper sputum collection techniques; identify and screen household contacts; ensure treatment adherence through DOTS; monitor for adverse drug reactions |
| Cervical/Breast Cancer |
|
Organize women’s health camps; train in performing VIA/VILI; teach proper breast self-examination techniques; ensure referral systems for positive findings |
| Mental Health Disorders |
|
Incorporate mental health screening in routine care; train in basic counseling techniques; establish referral pathways; reduce stigma through community awareness |
Tertiary Prevention Nursing Interventions
| Health Problem | Nursing Interventions | Implementation Strategy |
|---|---|---|
| Stroke |
|
Train in basic rehabilitation techniques; teach home-based exercises; educate on preventing recurrence; provide assistive device training; establish stroke support groups |
| Diabetic Complications |
|
Establish diabetic foot clinics; train in proper wound dressing techniques; coordinate with ophthalmologists for retinal screening; teach glycemic management during illness |
| COPD |
|
Teach breathing exercises; demonstrate proper inhaler techniques; create action plans for exacerbations; educate on avoiding triggers; promote smoking cessation |
| HIV/AIDS |
|
Establish ART adherence clinics; monitor CD4 counts; screen regularly for TB and other opportunistic infections; provide nutrition supplementation; address psychosocial needs |
| Chronic Kidney Disease |
|
Train patients in peritoneal dialysis techniques; educate on vascular access care; teach fluid restriction management; develop culturally appropriate renal diet plans using local foods |
Cross-cutting Nursing Interventions
Several nursing interventions apply across multiple prevention levels and health conditions:
Health Education and Counseling
Develop culturally appropriate, language-specific health education materials. Use technology (mHealth) for wider reach. Train community health workers to extend education efforts.
Community Mobilization
Engage local leaders and community groups in health initiatives. Form village health committees with active participation of women. Organize health melas (fairs) for awareness and screening.
Capacity Building
Train frontline workers (ASHAs, Anganwadi workers) in prevention activities. Develop skill-building programs for community volunteers. Create peer educator networks for sustained impact.
Record Keeping and Surveillance
Implement effective documentation systems for continuity of care. Contribute to disease surveillance networks. Utilize digital health records where available to track interventions and outcomes.
Integrated Case Studies
The following case studies demonstrate the application of all three prevention levels in addressing specific health challenges in the Indian context:
Case Study 1: Comprehensive Approach to Diabetes Management
Scenario: A community health nurse in an urban slum area of Mumbai is tasked with addressing the growing burden of diabetes in the community.
Primary Prevention Interventions:
- Organizing community awareness sessions about healthy eating using locally available foods
- Conducting physical activity promotion through yoga sessions in community centers
- Implementing school-based education on healthy lifestyle habits
- Training community volunteers as “Diabetes Prevention Champions”
Secondary Prevention Interventions:
- Setting up monthly screening camps for random blood glucose testing
- Establishing a risk assessment protocol to identify high-risk individuals
- Creating a follow-up system for those with prediabetes
- Facilitating early diagnosis by coordinating with the local health center
Tertiary Prevention Interventions:
- Forming a diabetes support group for patients to share experiences and coping strategies
- Conducting home visits to assess medication adherence and proper insulin storage
- Teaching foot care techniques to prevent diabetic foot complications
- Coordinating regular eye screening for early detection of retinopathy
Outcomes: Reduced incidence of new diabetes cases, improved glycemic control among diagnosed patients, decreased complication rates, and enhanced community knowledge about diabetes.
Case Study 2: Maternal and Child Health in Rural India
Scenario: A public health nurse working in a primary health center in rural Rajasthan is implementing a comprehensive maternal and child health program.
Primary Prevention Interventions:
- Conducting preconception counseling for women of reproductive age
- Organizing iron and folic acid supplementation for adolescent girls
- Promoting institutional deliveries through awareness campaigns
- Implementing childhood immunization drives with community participation
Secondary Prevention Interventions:
- Performing regular antenatal check-ups to identify high-risk pregnancies
- Screening for gestational diabetes and pregnancy-induced hypertension
- Conducting growth monitoring for children under five years
- Implementing early detection of developmental delays through milestone assessment
Tertiary Prevention Interventions:
- Managing high-risk pregnancies through specialized care protocols
- Providing nutritional rehabilitation for malnourished children
- Implementing Kangaroo Mother Care for low birth weight babies
- Coordinating early intervention services for children with developmental delays
Outcomes: Reduced maternal and infant mortality, improved nutritional status of children, increased immunization coverage, and enhanced community awareness about maternal and child health.
Case Study 3: Tuberculosis Control in an Urban Setting
Scenario: A TB control nurse in a large urban hospital in Delhi is implementing a comprehensive TB prevention and control program.
Primary Prevention Interventions:
- Conducting public awareness campaigns about TB transmission and prevention
- Promoting cough hygiene practices in communities and healthcare settings
- Implementing BCG vaccination for newborns
- Advocating for improved housing and reduced overcrowding
Secondary Prevention Interventions:
- Organizing active case finding through symptom screening in high-risk areas
- Setting up sputum collection centers in underserved communities
- Implementing rapid diagnostic testing using GeneXpert
- Conducting contact tracing for all newly diagnosed patients
Tertiary Prevention Interventions:
- Implementing DOTS (Directly Observed Treatment, Short-course) therapy
- Managing drug-resistant TB through specialized treatment protocols
- Providing nutritional support to improve treatment outcomes
- Conducting pulmonary rehabilitation for patients with post-TB sequelae
Outcomes: Increased case detection, improved treatment completion rates, reduced transmission in the community, and decreased development of drug-resistant TB.
Mnemonics & Memory Aids
The following mnemonics and memory aids will help nursing students remember key concepts about levels of prevention:
Mnemonic: “P.S.T” for Prevention Levels
P – Primary Prevention: Prevent disease before it starts
S – Secondary Prevention: Screen and detect early
T – Tertiary Prevention: Treat and rehabilitate
Mnemonic: “P.I.E” for Primary Prevention
P – Protection through immunization and specific measures
I – Information and education about health risks
E – Environmental modifications and healthy lifestyle
Mnemonic: “S.E.D” for Secondary Prevention
S – Screening of high-risk and asymptomatic individuals
E – Early diagnosis before symptoms worsen
D – Disease control through prompt treatment
Mnemonic: “R.I.C.E” for Tertiary Prevention
R – Rehabilitation to maximum potential
I – Impact reduction of disease complications
C – Comprehensive care for chronic conditions
E – Education for self-management and adaptation
Prevention Levels Flowchart
Primary Prevention
Pre-pathogenesis period
Focus: Health Promotion
- Health education
- Immunization
- Nutrition
- Environmental sanitation
Secondary Prevention
Early pathogenesis period
Focus: Early Detection
- Screening
- Case finding
- Early diagnosis
- Prompt treatment
Tertiary Prevention
Late pathogenesis period
Focus: Rehabilitation
- Disability limitation
- Rehabilitation
- Complication management
- Quality of life improvement
Target Populations by Prevention Level
Primary Prevention
Target: Healthy Population
- Pregnant women (for antenatal care)
- Children (for immunization)
- Adolescents (for health education)
- General population (for health promotion)
Secondary Prevention
Target: At-risk or Asymptomatic Population
- High-risk individuals
- Age-specific groups (for cancer screening)
- Contacts of infectious cases
- Population with early or mild symptoms
Tertiary Prevention
Target: Individuals with Disease
- Patients with established diagnosis
- Individuals with disabilities
- People with chronic conditions
- Post-surgical or post-acute event patients
Implementation of Prevention Levels in Nursing Practice
Implementing prevention strategies requires nurses to develop specific competencies and navigate the healthcare system effectively:
Core Nursing Competencies for Prevention
Assessment Skills
- Risk factor identification using standardized tools
- Community health needs assessment
- Cultural competency in assessment
- Screening protocol implementation
Communication Skills
- Health education delivery in local languages
- Motivational interviewing techniques
- Cross-cultural communication
- Health literacy-appropriate messaging
Technical Skills
- Vaccination administration
- Screening procedures implementation
- Basic rehabilitation techniques
- Health monitoring and documentation
Leadership and Advocacy
- Community mobilization
- Interdisciplinary team coordination
- Resource allocation advocacy
- Health policy implementation
Integration with Indian Healthcare System
Nurses implementing prevention strategies must understand how to navigate and utilize India’s healthcare framework:
| Healthcare Level | Prevention Activities | Nursing Role |
|---|---|---|
| Sub-Center | Immunization, maternal care, health education, basic screening | ANMs implement primary prevention and basic secondary prevention; conduct home visits; coordinate with ASHAs |
| Primary Health Center | All primary prevention activities, comprehensive screening, basic treatment | Staff nurses conduct screening clinics; implement national health programs; provide initial treatment; coordinate referrals |
| Community Health Center | Specialized screening, comprehensive diagnosis, secondary prevention interventions | Specialized nursing care; management of NCDs; implementation of treatment protocols; health education |
| District Hospital | All levels of prevention, specialized rehabilitation services | Clinical nurses provide specialized care; rehabilitation nurses implement tertiary prevention; nurse educators train lower-level staff |
| Tertiary Centers | Specialized tertiary prevention, advanced rehabilitation | Specialized nursing care for complex conditions; implementation of advanced rehabilitation protocols; nursing research on prevention effectiveness |
Integration with National Health Programs
Nurses play crucial roles in implementing various national health programs that span across the prevention spectrum:
| Program | Prevention Levels | Nursing Implementation |
|---|---|---|
| National Health Mission | Primary, Secondary, Tertiary | Implementation of RMNCH+A services; coordination of village health and nutrition days; training of frontline workers; supportive supervision |
| National Immunization Program | Primary | Vaccine administration; cold chain management; AEFI monitoring; coverage improvement plans; outreach session organization |
| NPCDCS | Primary, Secondary, Tertiary | NCD screening camps; lifestyle modification counseling; follow-up of diagnosed cases; complication prevention education; rehabilitation guidance |
| National TB Elimination Program | Primary, Secondary, Tertiary | TB preventive education; active case finding; DOTS implementation; adverse reaction management; rehabilitation of post-TB patients |
| National Mental Health Program | Primary, Secondary, Tertiary | Mental health awareness; depression screening; basic counseling; medication adherence support; community reintegration assistance |
Challenges and Solutions
Implementing prevention strategies in the Indian context presents several challenges that nurses must navigate:
Challenge: Resource Constraints
Solutions:
- Task-shifting to optimize available workforce
- Community volunteer engagement
- Integration of services to maximize efficiency
- Telehealth implementation where feasible
Challenge: Cultural Barriers
Solutions:
- Culturally adapted interventions
- Engagement of community leaders and influencers
- Use of local dialects and familiar concepts
- Gender-sensitive approaches
Challenge: Geographic Barriers
Solutions:
- Mobile health units for remote areas
- Village health camps
- Transport arrangements for critical services
- Point-of-care diagnostics
Challenge: Continuity of Care
Solutions:
- Implementation of health cards/records
- Patient tracking systems
- Appointment reminder systems
- Community follow-up mechanisms
Key Points for Successful Implementation:
- Use evidence-based interventions adapted to local contexts
- Establish clear roles and responsibilities for nursing personnel at each level
- Ensure adequate training and continuous skill development
- Develop robust monitoring and evaluation mechanisms
- Foster multi-sectoral collaboration for comprehensive prevention
- Engage communities as partners in prevention activities
- Utilize technology appropriately to enhance reach and effectiveness
References
- World Health Organization (WHO). (2024). WHO Data for India. https://data.who.int/countries/356
- Ministry of Health and Family Welfare, Government of India. (2024). National Health Profile 2023. https://cbhidghs.mohfw.gov.in
- Institute for Work & Health. (2024). Primary, secondary and tertiary prevention. https://www.iwh.on.ca/what-researchers-mean-by/primary-secondary-and-tertiary-prevention
- Kisling, L.A., & Das, J.M. (2023). Prevention Strategies. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537222/
- Ipsos. (2024). Cancer, Obesity, Mental Health, India’s top health concerns – Ipsos Health Service Report 2024. https://www.ipsos.com
- India State-Level Disease Burden Initiative. (2024). Disease burden initiative in India. https://www.healthdata.org
- Montgomery, S.C., et al. (2024). Prevention, Tertiary. In: StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK537222/
- Times of India. (2024). World Health Day 2024: Top 7 most dangerous health concerns in India. https://timesofindia.indiatimes.com
- Mondal, S., & Van Belle, S. (2018). India’s NCD strategy in the SDG era: are there early signs of a paradigm shift? Globalization and Health, 14(1), 39. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5899321/
- Press Information Bureau, Government of India. (2024). India’s Success in Reducing Maternal Mortality. https://www.pib.gov.in/PressReleasePage.aspx?PRID=2113800
- Ministry of Health and Family Welfare, Government of India. (2024). Annual Report 2024-25. https://mohfw.gov.in
- Kasthuri, A. (2018). Challenges to Healthcare in India – The Five A’s. Indian Journal of Community Medicine, 43(3), 141-143. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6166510/