Treatment Modalities for Special Populations
Mental Health Nursing Guide
Introduction
Mental health care for special populations requires tailored approaches to address unique needs, barriers, and circumstances. These notes provide evidence-based treatment modalities and nursing interventions specifically designed for vulnerable groups including geriatric patients, pediatric patients, LGBTQ+ individuals, culturally diverse populations, and persons with disabilities.
Key Principles of Mental Health Care for Special Populations
- Individualized assessment and treatment planning
- Culturally responsive and inclusive approaches
- Trauma-informed care
- Evidence-based interventions with population-specific adaptations
- Continuous evaluation and adjustment of treatment plans
According to the World Health Organization, barriers to mental health care are often amplified for special populations, resulting in disparities in treatment access, quality, and outcomes. As nurses, understanding these unique considerations is essential for providing equitable, effective, and compassionate care.
General Overview of Treatment Modalities
Mental Health Treatment Modalities Framework

Figure 1: Range of mental health interventions across the care continuum.
Core Treatment Approaches
Pharmacotherapy
Medication management approaches tailored to specific population needs, considering factors like metabolism, comorbidities, and drug interactions.
Psychotherapy
Includes cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), interpersonal therapy (IPT), and other evidence-based approaches adapted for specific populations.
Psychosocial Interventions
Family therapy, group therapy, social skills training, and community support programs designed to address social determinants of mental health.
Integrative Approaches
Complementary therapies including mindfulness, art therapy, music therapy, and other holistic interventions that can enhance conventional treatments.
The “CARES” Framework for Special Population Approaches
- Cultural Competence – Adapt interventions to cultural contexts
- Accessibility – Ensure treatments are accessible and appropriate
- Relationship-based – Focus on therapeutic alliance
- Evidence-informed – Use validated approaches with adaptations
- Strength-focused – Build on resilience and existing supports
Evidence-Based Practice Consideration
Research indicates that treatment outcomes improve when interventions are tailored to address the specific needs, values, and preferences of special populations. Standard protocols often require adaptations while maintaining fidelity to core therapeutic mechanisms.
Geriatric Population
Unique Considerations
- Age-related pharmacokinetic and pharmacodynamic changes
- Higher risk of polypharmacy and drug interactions
- Comorbid medical conditions that complicate treatment
- Cognitive impairment affecting treatment engagement
- Social isolation and loss as contributing factors
- Increased risk of suicide, particularly in older men
Special Caution: “Start Low, Go Slow”
Geriatric patients generally require lower initial doses of psychotropic medications with gradual titration to minimize adverse effects. Close monitoring is essential due to increased sensitivity to side effects.
Common Mental Health Conditions
- Depression: Often presents atypically with more somatic complaints than mood symptoms
- Anxiety disorders: Frequently comorbid with physical health conditions
- Neurocognitive disorders: Including dementia and associated behavioral symptoms
- Substance use disorders: Particularly alcohol use and prescription medication misuse
- Sleep disorders: Common and often undertreated
Evidence-Based Treatment Approaches
Pharmacotherapy
- SSRIs (e.g., sertraline, escitalopram) preferred for depression and anxiety
- Avoid anticholinergic medications (TCAs, certain antipsychotics)
- Cautious use of benzodiazepines due to fall risk
- Mood stabilizers with renal/hepatic dose adjustments
Psychotherapy
- Problem-solving therapy
- Age-adapted cognitive behavioral therapy
- Reminiscence and life review therapy
- Interpersonal therapy focused on role transitions
- Supportive psychotherapy
Psychosocial Interventions
- Social activation and engagement programs
- Caregiver support and education
- Group-based interventions
- Behavioral management for dementia
- Environmental modifications
The “ELDERS” Mnemonic for Geriatric Mental Health Assessment
- Environment – Assess living situation and support systems
- Losses – Recent bereavements or significant changes
- Drugs – Complete medication review including OTC
- Emotional state – Screen for depression and anxiety
- Recent illness – Medical conditions affecting mental health
- Sensory changes – Vision/hearing affecting communication
Nursing Interventions
Assessment Strategies
- Use validated geriatric-specific screening tools (e.g., Geriatric Depression Scale)
- Conduct comprehensive medication reviews
- Assess for physical health comorbidities
- Evaluate cognitive status using tools like MMSE or MoCA
- Screen for elder abuse and neglect
Implementation Strategies
- Implement fall prevention protocols with psychotropic use
- Provide memory aids for medication adherence
- Establish consistent daily routines
- Encourage physical activity appropriate to ability
- Facilitate social connection and family involvement
- Use clear, simple communication strategies
Pediatric Population
Developmental Considerations
- Developmental stage affects symptom presentation and treatment approaches
- Rapidly changing physiology impacts medication metabolism
- School environment as a critical context for intervention
- Family system plays central role in treatment
- Increased vulnerability to adverse childhood experiences (ACEs)
- Limited ability to articulate emotions and experiences verbally
Special Consideration: FDA Black Box Warnings
Antidepressants carry black box warnings for increased suicidality risk in children and adolescents. Close monitoring is essential during the initial treatment period and with any dose changes.
Common Mental Health Conditions
- Anxiety disorders: Most common pediatric mental health condition
- ADHD: Requires multimodal treatment approaches
- Depression: Often presents with irritability rather than sadness
- Autism spectrum disorders: Focus on comorbid conditions and behavioral supports
- Trauma-related disorders: Including PTSD and adjustment disorders
Evidence-Based Treatment Approaches
Pharmacotherapy
- Stimulants (first-line for ADHD)
- SSRIs (with close monitoring for depression/anxiety)
- Age-appropriate dosing and formulations
- Regular monitoring of growth, weight, and vital signs
- Consideration of long-term developmental impacts
Psychotherapy
- Cognitive-behavioral therapy (age-adapted)
- Play therapy for younger children
- Parent-child interaction therapy
- Family therapy approaches
- Trauma-focused CBT
School-Based Interventions
- IEP and 504 accommodations
- Classroom behavioral interventions
- Social skills groups
- School-based counseling
- Teacher consultation and education
Pediatric Mental Health Treatment Decision Pathway

Figure 2: Multimodal treatment approach for pediatric mental health conditions.
The “CHILD” Approach to Pediatric Mental Health Nursing
- Communication – Age-appropriate engagement strategies
- Holistic – Assessment includes family, school, and social contexts
- Individualized – Developmentally appropriate interventions
- Life skills – Building coping strategies and emotional regulation
- Developmental – Considering stage-specific needs and capabilities
Nursing Interventions
Assessment Strategies
- Use age-appropriate assessment tools
- Gather information from multiple sources (child, parents, teachers)
- Screen for adverse childhood experiences (ACEs)
- Assess developmental status and functioning
- Evaluate family dynamics and parenting approaches
Implementation Strategies
- Establish therapeutic relationship using play and age-appropriate activities
- Provide parent education and family support
- Collaborate with school personnel
- Teach coping skills and emotional regulation techniques
- Monitor medication effects and side effects closely
- Create safety plans for crisis situations
LGBTQ+ Population
Unique Considerations
- Higher prevalence of mental health conditions due to minority stress
- Experiences of discrimination, stigma, and rejection
- Internalized stigma affecting self-concept and treatment engagement
- Historical trauma within healthcare settings
- Gender-affirming care considerations for transgender individuals
- Intersectionality with other identity factors
Important Note: Language and Terminology
Using appropriate, affirming language is a critical component of care. Nurses should ask about and use preferred names, pronouns, and terminology, recognizing that language evolves and varies among individuals.
Mental Health Disparities
- Elevated rates of:
- Depression and anxiety disorders
- Suicidal ideation and attempts
- Substance use disorders
- PTSD and trauma-related conditions
- Body dysmorphia and eating disorders
- Contributing factors:
- Minority stress and microaggressions
- Family rejection and social isolation
- Discrimination in healthcare settings
- Gender dysphoria (for transgender individuals)
Evidence-Based Treatment Approaches
Affirming Psychotherapy
- LGB-affirmative cognitive behavioral therapy
- Gender-affirming approaches for transgender individuals
- Minority stress-focused interventions
- Identity development and integration work
- Family acceptance interventions
Pharmacotherapy Considerations
- Medication interactions with hormone therapy
- Mental health support during gender transition
- Standard psychopharmacology with awareness of identity-specific stressors
- Sensitivity to medication side effects affecting body image
Community-Based Support
- LGBTQ+-specific support groups
- Peer navigation programs
- Community center resources
- Online support communities
- Family acceptance programs
The “AFFIRM” Framework for LGBTQ+ Mental Health Nursing
- Acknowledge identity and use affirming language
- Foster safety in the therapeutic environment
- Facilitate access to LGBTQ+-knowledgeable providers
- Intersectionality awareness in assessment and planning
- Recognize minority stress impacts on mental health
- Mobilize community resources and support systems
Nursing Interventions
Creating Affirming Environments
- Display visual cues of LGBTQ+ inclusion (e.g., pride symbols, inclusive materials)
- Use inclusive language on forms and in verbal communication
- Address patients by their preferred name and pronouns
- Ensure privacy and confidentiality, particularly for youth
- Develop non-discriminatory policies and procedures
Clinical Care Approaches
- Conduct comprehensive, identity-affirming assessments
- Screen for experiences of discrimination and rejection
- Assess for internalized stigma and its mental health impacts
- Connect patients with LGBTQ+-affirming resources
- Provide education about minority stress and resilience
- Support family acceptance and understanding
Evidence-Based Practice Highlight
Research demonstrates that affirming approaches that validate LGBTQ+ identities lead to better mental health outcomes. Family acceptance interventions, particularly for LGBTQ+ youth, are associated with significantly lower rates of depression, suicidal ideation, and substance use.
Culturally Diverse Populations
Considerations for Culturally Responsive Care
- Cultural variations in symptom expression and help-seeking
- Different conceptualizations of mental health and illness
- Language barriers affecting assessment and treatment
- Cultural stigma around mental health treatment
- Historical trauma and mistrust of healthcare systems
- Role of cultural healing practices and traditional approaches
Cultural Humility vs. Cultural Competence
Cultural humility emphasizes ongoing self-reflection and openness to learning about others’ cultures, rather than achieving “competence.” This approach recognizes that cultures are dynamic and that individuals vary within cultural groups.
Impact of Culture on Mental Health
- Symptom presentation: Culture influences how mental health symptoms are expressed and interpreted
- Help-seeking behaviors: Cultural values affect when and from whom help is sought
- Treatment preferences: Beliefs about healing influence treatment acceptability
- Family involvement: Cultural norms around family roles in healthcare decisions
- Communication styles: Cultural differences in directness, eye contact, and disclosure
Framework for Culturally Responsive Mental Health Care

Figure 3: Cultural considerations in assessment and treatment planning.
Evidence-Based Culturally Adapted Approaches
Assessment Approaches
- Cultural formulation interview (DSM-5)
- Culturally validated screening tools
- Exploration of explanatory models of illness
- Assessment of acculturation and cultural identity
- Evaluation of cultural strengths and resources
Adapted Psychotherapy
- Culturally adapted CBT
- Community-based interventions
- Integration of cultural values and beliefs
- Culturally specific metaphors and examples
- Cultural brokering and mediation
Integrative Approaches
- Collaboration with traditional healers
- Incorporation of cultural healing practices
- Family-centered approaches
- Community-based participatory methods
- Faith-based interventions where appropriate
The “LEARN” Model for Cross-Cultural Communication
- Listen with empathy and understanding
- Explain your perceptions and clinical reasoning
- Acknowledge and discuss differences and similarities
- Recommend treatment with cultural considerations in mind
- Negotiate a treatment plan that incorporates cultural values
Nursing Interventions
Cultural Assessment and Planning
- Use cultural formulation in assessment
- Explore cultural explanatory models of illness
- Assess for culture-bound syndromes
- Identify cultural strengths and protective factors
- Incorporate cultural beliefs into care planning
Implementation Strategies
- Work with trained interpreters when needed
- Adapt patient education to cultural context
- Involve family members according to cultural norms
- Collaborate with community cultural resources
- Adapt therapeutic communication to cultural styles
- Demonstrate respect for cultural health practices
Evidence-Based Practice Highlight
Studies show that culturally adapted mental health interventions demonstrate significantly better outcomes than standard treatments alone. Cultural adaptations that maintain core therapeutic elements while incorporating cultural values, beliefs, and practices show the greatest efficacy.
Individuals with Disabilities
Unique Considerations
- Higher prevalence of mental health conditions
- Diagnostic overshadowing (attributing mental health symptoms to disability)
- Communication barriers affecting assessment and treatment
- Accessibility issues in mental health services
- Complex interactions between disability and psychiatric symptoms
- Medication interactions and side effects requiring special monitoring
Ableism in Mental Health Care
Ableism, or discrimination against people with disabilities, can manifest in mental health care through inaccessible services, assumptions about quality of life, invalidation of emotional experiences, and lack of accommodations. Recognizing and addressing ableism is essential for equitable care.
Common Mental Health Challenges
- For intellectual/developmental disabilities:
- Higher rates of anxiety, depression, and behavioral disorders
- Challenging behaviors that may indicate underlying mental health conditions
- Difficulty identifying and expressing emotional states
- For physical disabilities:
- Adjustment disorders related to disability onset or progression
- Depression associated with chronic pain and functional limitations
- PTSD related to traumatic injury experiences
Evidence-Based Treatment Approaches
Adapted Psychotherapy
- Modified CBT for intellectual disabilities
- Skills-based interventions
- Behavioral approaches for communication challenges
- Trauma-informed care for individuals with disabilities
- Simplified materials and concrete examples
Pharmacotherapy Considerations
- Lower starting doses with gradual titration
- Careful monitoring for atypical responses
- Consideration of drug interactions with medications for physical conditions
- Non-verbal assessment of medication effects and side effects
- Caution with medications affecting mobility or cognition
Psychosocial Interventions
- Positive behavioral support approaches
- Caregiver training and support
- Adapted group therapy interventions
- Environmental modifications
- Assistive technology for communication
- Peer support programs
The “ACCESS” Framework for Disability-Inclusive Mental Health Care
- Adaptations to assessment and interventions
- Communication support and accommodations
- Collaboration with disability specialists
- Environmental accessibility and modifications
- Support for caregivers and support networks
- Strengths-focused approach emphasizing capabilities
Nursing Interventions
Assessment Strategies
- Use adapted assessment tools validated for specific disabilities
- Employ multiple modes of communication (verbal, visual, written)
- Allow additional time for assessment completion
- Gather collateral information from caregivers
- Distinguish between disability-related behaviors and mental health symptoms
- Assess for sensory processing issues
Implementation Strategies
- Provide accessible education materials
- Use clear, concrete language and visual supports
- Implement environmental accommodations
- Develop consistent routines and structured approaches
- Collaborate with specialist disability services
- Involve caregivers in treatment planning and implementation
- Advocate for accessibility in mental health services
Evidence-Based Practice Highlight
Research demonstrates that adapted psychotherapeutic approaches, such as modified CBT for individuals with intellectual disabilities, can be highly effective when appropriate accommodations are made. These adaptations include simplified language, visual aids, shorter sessions, and concrete examples while maintaining fidelity to core therapeutic principles.
Trauma-Informed Care Approaches
Core Principles
- Recognition of the widespread impact of trauma
- Understanding signs and symptoms of trauma
- Integration of trauma knowledge into policies and procedures
- Active prevention of re-traumatization
- Emphasis on safety, trustworthiness, choice, collaboration, and empowerment
- Recognition of cultural, historical, and gender issues in trauma
Trauma Prevalence in Special Populations
Special populations often experience disproportionately high rates of trauma. For example, studies show 70-90% of individuals with serious mental illness report trauma histories, while LGBTQ+ individuals, people with disabilities, and racial/ethnic minorities face higher rates of violence, abuse, and traumatic discrimination.
Trauma-Informed Care Framework
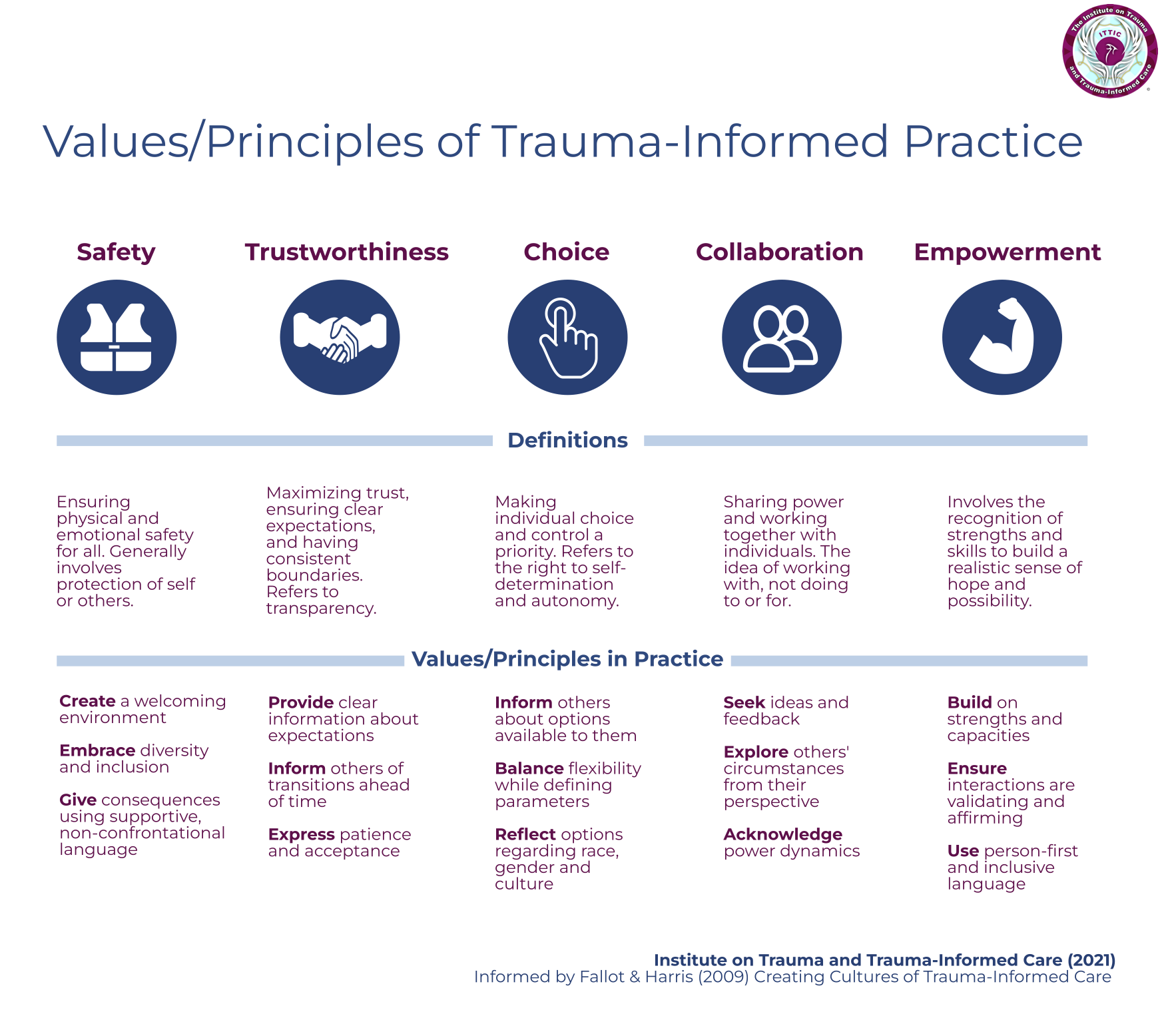
Figure 4: Six principles of trauma-informed care approach.
Evidence-Based Trauma-Specific Interventions
For Adults
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Seeking Safety (for trauma and substance use)
- Cognitive Processing Therapy (CPT)
- Prolonged Exposure Therapy (PE)
For Children/Adolescents
- Trauma-Focused CBT (adapted for youth)
- Child-Parent Psychotherapy
- Attachment, Regulation and Competency (ARC)
- Trust-Based Relational Intervention
- Trauma Systems Therapy
Group-Based Approaches
- Skills Training in Affective and Interpersonal Regulation (STAIR)
- Trauma Recovery and Empowerment Model (TREM)
- Trauma-Informed Mindfulness-Based Stress Reduction
- Sanctuary Model (organizational approach)
- TARGET (Trauma Affect Regulation)
The “TRAUMA” Framework for Nursing Assessment
- Triggers – Identify potential triggering situations
- Reactions – Document typical trauma responses and coping mechanisms
- Avoidance – Note avoidance patterns and their impact
- Understanding – Assess patient’s understanding of trauma effects
- Management – Evaluate current symptom management strategies
- Adaptations – Identify needed adaptations to care approach
Nursing Interventions for Trauma-Informed Care
Creating Safety
- Establish predictable routines and clear expectations
- Provide information about procedures before they occur
- Offer choices whenever possible
- Create calm, quiet treatment environments
- Allow patients to have a trusted person present
- Use trauma-sensitive language and approach
- Respect physical boundaries and personal space
Supporting Regulation
- Teach grounding techniques for managing triggers
- Demonstrate and practice deep breathing exercises
- Provide sensory tools for self-regulation
- Create safety plans for managing intense emotions
- Recognize and validate trauma responses
- Help identify early warning signs of dysregulation
- Support development of healthy coping strategies
Preventing Re-traumatization
Mental health procedures can inadvertently trigger trauma responses. Particular attention should be paid to:
- Avoiding restraint and seclusion whenever possible
- Minimizing invasive procedures
- Providing clear explanations before physical contact
- Being sensitive to power dynamics in the therapeutic relationship
- Recognizing cultural factors in trauma experiences and responses
- Ensuring patient privacy and confidentiality
Pharmacological Approaches for Special Populations
General Considerations
- Medication selection based on population-specific risk/benefit profiles
- Consideration of comorbid conditions and drug interactions
- Monitoring for population-specific adverse effects
- Attention to adherence barriers for different populations
- Cultural and religious beliefs affecting medication acceptance
- Genetic variations affecting medication metabolism
Medication Usage Patterns
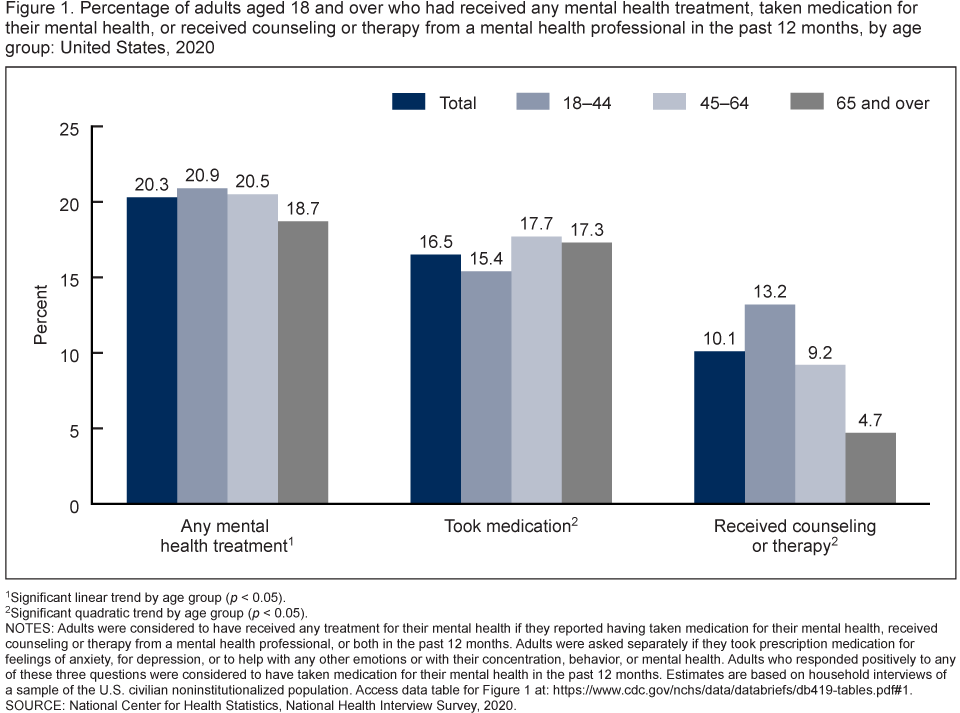
Figure 5: Demographic patterns in psychiatric medication prescription.
Geriatric Pharmacology
- Reduced starting doses (typically 1/3 to 1/2 standard dose)
- Extended titration periods with close monitoring
- Avoid medications with high anticholinergic burden
- Prefer medications with once-daily dosing
- Monitor for drug-drug interactions with existing medications
- Increased risk of extrapyramidal symptoms with antipsychotics
- Increased fall risk with sedating medications
Pediatric Pharmacology
- Weight-based dosing for most medications
- Monitoring for behavioral activation with antidepressants
- Close monitoring during initiation and dose changes
- Consideration of long-term effects on development
- FDA black box warnings for suicidality with antidepressants
- Metabolic monitoring with atypical antipsychotics
- Medication adherence strategies involving caregivers
Disability Considerations
- Alternative medication formulations (liquid, ODT) for swallowing difficulties
- Consideration of cognitive impact of medications
- Monitoring for atypical medication responses
- Attention to communication about side effects
- Adaptation of medication administration techniques
- Interactions with medications for primary disabilities
- Sensory considerations in medication administration
The “SAFER” Mnemonic for Special Population Medication Management
- Start low, go slow with dosing
- Assess for population-specific side effects
- Frequent monitoring and follow-up
- Educate about medication in accessible ways
- Review for drug interactions and contraindications
Nursing Responsibilities in Medication Management
Assessment and Monitoring
- Conduct thorough medication history including OTC and cultural remedies
- Assess for population-specific risk factors
- Monitor for atypical or exaggerated side effects
- Use appropriate scales for non-verbal patients
- Screen for allergies and previous adverse reactions
- Evaluate medication adherence barriers
Patient and Family Education
- Provide accessible medication information (appropriate literacy level, language)
- Use visual aids for medication schedules
- Address cultural concerns about medications
- Demonstrate medication administration techniques
- Teach about red-flag side effects requiring immediate attention
- Include caregivers in education when appropriate
Integrative Mental Health Approaches
Integrative mental health combines conventional treatments with evidence-based complementary approaches. These holistic strategies can be particularly beneficial for special populations who may face barriers to conventional treatments or have cultural preferences for alternative approaches.
Evidence-Based Integrative Approaches
Mind-Body Interventions
- Mindfulness-based stress reduction (MBSR)
- Yoga therapy (adapted for abilities)
- Tai chi and qigong for older adults
- Progressive muscle relaxation
- Biofeedback and neurofeedback
- Breathwork techniques
Creative Arts Therapies
- Art therapy for trauma and emotional expression
- Music therapy for emotional regulation
- Dance/movement therapy for physical expression
- Drama therapy for social skills
- Poetry and narrative therapy
- Play therapy for children
Other Complementary Approaches
- Nutritional psychiatry and dietary interventions
- Exercise as medicine approaches
- Nature-based therapies
- Animal-assisted interventions
- Acupuncture and acupressure
- Light therapy for seasonal affective disorder
Population-Specific Applications
| Special Population | Recommended Approaches | Evidence Level | Special Considerations |
|---|---|---|---|
| Geriatric |
|
Strong | Modified for mobility and cognitive capacity |
| Pediatric |
|
Moderate to Strong | Developmentally appropriate adaptations |
| Cultural Minorities |
|
Moderate | Integration with cultural beliefs and traditions |
| Individuals with Disabilities |
|
Moderate | Modified based on physical and cognitive abilities |
| Trauma Survivors |
|
Strong | Trauma-informed modifications essential |
Integration with Conventional Care
Integrative approaches are most effective when combined with evidence-based conventional treatments in a coordinated care plan. Open communication between all providers is essential to ensure safety and avoid contradictory approaches. Nurses play a critical role in coordinating these aspects of care and advocating for holistic treatment plans.
Nursing Role in Integrative Mental Health
Assessment
- Screen for current use of complementary approaches
- Assess cultural beliefs about healing and wellness
- Evaluate openness to different modalities
- Identify barriers to conventional treatments
- Assess for contraindications to specific approaches
Implementation
- Provide evidence-based information about options
- Teach simple mindfulness and relaxation techniques
- Incorporate sensory approaches into nursing care
- Connect patients with qualified practitioners
- Monitor for interactions with conventional treatments
- Document responses to integrative approaches
Case Studies
Case Study: Geriatric Patient with Depression
Patient: Maria, 78-year-old widow with history of hypertension, osteoarthritis, and recent bereavement (husband died 8 months ago)
Presentation: Complaints of fatigue, sleep disturbance, poor appetite, and loss of interest in activities. Appears withdrawn during assessment. Reports feeling “useless” and has stopped attending her senior center.
Nursing Assessment
- Geriatric Depression Scale score: 11/15 (indicating moderate depression)
- Mini-Mental State Examination: 28/30 (cognitive function intact)
- Current medications: Lisinopril, acetaminophen, calcium/vitamin D
- Social history: Lives alone, daughter visits weekly, limited other social contacts
- Functional status: Independent in ADLs but increasingly isolating herself
Intervention Plan
- Pharmacotherapy: Started on escitalopram 5mg daily (lower than standard adult dose), with plan to reassess in 2 weeks before considering dose increase
- Psychotherapy: Referred for Problem-Solving Therapy focused on adaptation to widowhood
- Psychosocial: Connected with senior center transportation service and bereavement support group
- Integrative approaches: Daily walking program and music therapy
Nursing Interventions:
- Weekly phone follow-up to monitor medication side effects and response
- Medication education with written schedule and pill organizer
- Sleep hygiene education
- Safety assessment of home environment
- Coordination with daughter for family support
Outcome
After 8 weeks, Maria reported improved mood, increased energy, and resumed attendance at senior center twice weekly. Medication well-tolerated with no significant side effects. GDS score improved to 5/15. Continue current plan with monthly follow-up.
Case Study: Pediatric Patient with Anxiety
Patient: Jason, 9-year-old male with history of academic difficulties and recent school transition
Presentation: Parents report increasing school refusal, complaints of stomachaches on school mornings, excessive worry about tests, and sleep difficulties. Teacher notes he appears anxious in class and struggles with group activities.
Nursing Assessment
- Screen for Child Anxiety Related Disorders (SCARED): Score 34 (above clinical cutoff)
- Academic testing: Reading difficulties identified (possible contributing factor)
- Family assessment: Parents report marital stress and inconsistent discipline approaches
- Medical history: Recent evaluation revealed no organic cause for somatic complaints
- Strengths: Creative, enjoys art, close relationship with younger sister
Intervention Plan
- Psychotherapy: Cognitive-behavioral therapy with age-appropriate adaptations (drawing, games) to address anxiety
- School interventions: Collaborated with school to develop 504 plan with accommodations for reading difficulties and test anxiety
- Family work: Parent management training to develop consistent approaches
- Integrative approaches: Progressive muscle relaxation and guided imagery techniques
Nursing Interventions:
- Taught “worry thermometer” to help Jason identify anxiety levels
- Developed personalized coping skills toolkit with visual cues
- Coordinated care between therapist, school, and pediatrician
- Educated family about anxiety in developmentally appropriate terms
- Established bedtime routine to address sleep difficulties
Outcome
After 12 weeks, Jason’s school attendance improved to 90%. SCARED score decreased to 21. Parents report decreased somatic complaints and improved sleep. School accommodations have reduced academic anxiety. Continue with monthly therapy sessions and quarterly school coordination.
Case Study: Transgender Young Adult with Depression and Anxiety
Patient: Alex, 22-year-old transgender man (he/him), college student, recently began hormone therapy
Presentation: Presents with symptoms of depression, social anxiety, and difficulty navigating college environment. Reports family rejection after coming out. Experiencing dysphoria and anxiety about passing.
Nursing Assessment
- PHQ-9 score: 18 (moderately severe depression)
- GAD-7 score: 15 (severe anxiety)
- Social support assessment: Limited family support, small circle of affirming friends
- Safety assessment: Passive suicidal ideation without plan or intent
- Current medications: Testosterone (3 months), no psychiatric medications
- Strengths: Academically motivated, connected to LGBTQ+ student group
Intervention Plan
- Pharmacotherapy: Sertraline 50mg daily (selected for low interaction potential with hormone therapy)
- Psychotherapy: Gender-affirming cognitive-behavioral therapy focused on identity integration and coping with minority stress
- Social support: Connected with campus LGBTQ+ center and transgender support group
- Academic support: Referral to college disability services for accommodations during transition period
Nursing Interventions:
- Consistent use of affirmed name and pronouns in all interactions
- Education about medication effects and potential interactions with hormone therapy
- Safety planning with identified supports
- Coordination with gender-affirming care provider
- Resource connection for transgender-friendly services
Outcome
After 16 weeks, Alex reported significant improvement in mood and anxiety. PHQ-9 score decreased to 8, GAD-7 to 7. Successfully engaged with campus support services and transgender peer group. Medication well-tolerated with hormone therapy. Continuing with therapy to address family rejection issues.
Case Study: Culturally Responsive Care for Immigrant Patient
Patient: Aisha, 35-year-old Syrian refugee woman, arrived in US 6 months ago with husband and three children
Presentation: Presents with insomnia, hypervigilance, intrusive memories, and cultural bereavement. Reports history of trauma during war and refugee camp experiences. Primary language Arabic, limited English proficiency.
Nursing Assessment
- Harvard Trauma Questionnaire (culturally validated version): Positive for PTSD symptoms
- Cultural formulation interview: Beliefs about mental health rooted in religious and cultural framework
- Religious/spiritual assessment: Practicing Muslim, prayer is important coping mechanism
- Social assessment: Isolated from extended family, limited community connections
- Physical health: Headaches, fatigue, gastrointestinal complaints
Intervention Plan
- Psychotherapy: Culturally adapted trauma-focused CBT with certified interpreter
- Pharmacotherapy: Prazosin for nightmares, herbal tea accepted as complementary approach
- Community resources: Connected with Syrian community center and women’s support group
- Spiritual support: Coordination with local imam who supports mental health treatment
- Family approach: Psychoeducation for husband about trauma responses
Nursing Interventions:
- Provided education about trauma responses using culturally appropriate metaphors
- Ensured female interpreter and provider for all appointments
- Incorporated prayer schedule into treatment appointments
- Used cultural broker to navigate healthcare system
- Developed symptom management techniques compatible with cultural beliefs
Outcome
After 6 months, Aisha reported improved sleep, decreased hypervigilance, and better functioning in daily activities. Successfully integrated into women’s support group. Continuing trauma-focused therapy with attention to cultural bereavement. Family actively supporting treatment process.
Case Study: Patient with Intellectual Disability and Anxiety
Patient: David, 28-year-old male with moderate intellectual disability and autism spectrum disorder
Presentation: Group home staff report increased agitation, self-injurious behavior, sleep disturbance, and refusal to attend day program. Recent environmental change (new roommate) and staff turnover preceded symptoms.
Nursing Assessment
- Glasgow Anxiety Scale for People with Intellectual Disabilities: Elevated score
- Functional behavioral assessment: Behavior increases with environmental changes and sensory overload
- Communication assessment: Uses picture communication system and limited verbal speech
- Medical evaluation: Rule out physical causes of behavior change
- Strengths: Responds well to visual schedules, enjoys music, has established relationship with primary staff
Intervention Plan
- Pharmacotherapy: Low-dose sertraline with gradual titration, monitoring closely for behavioral activation
- Adapted CBT: Modified anxiety management using visual supports and concrete examples
- Environmental modifications: Sensory assessment and adaptations to living space
- Behavioral support plan: Consistent routines and positive behavior support strategies
- Integrative approaches: Music therapy and sensory integration techniques
Nursing Interventions:
- Developed visual anxiety scale and coping cards
- Created social story about medication and transitions
- Trained group home staff in recognition of anxiety triggers
- Implemented sensory diet throughout daily routine
- Established consistent communication method across settings
- Monitored for medication side effects with adapted assessment tools
Outcome
After 12 weeks, staff reported 70% reduction in agitation and self-injurious behavior. Sleep pattern improved. Successfully reintegrated into day program with modified schedule. Continuing with medication and adapted anxiety management strategies. Regular consultation with group home staff maintains consistency.
Summary of Key Principles
Core Approaches Across Populations
- Individualized assessment and person-centered planning
- Adaptation of evidence-based interventions to specific needs
- Collaborative, multi-disciplinary approaches
- Integration of cultural and contextual factors
- Attention to social determinants of mental health
- Trauma-informed care principles as a foundation
- Involving families and support systems appropriately
Nursing Role in Special Population Care
- Comprehensive, holistic assessment
- Care coordination across systems and providers
- Advocacy for accessible and appropriate services
- Patient and family education adapted to needs
- Monitoring treatment response and side effects
- Creating therapeutic environments and relationships
- Ongoing professional development for cultural competence
Integrated Framework for Special Population Mental Health Care

Figure 6: Treatment modalities and their benefits for special populations.
Remember the “DIVERSE” Framework for Special Population Mental Health Nursing
- Developmental and life stage considerations
- Individualized, person-centered approaches
- Validation of lived experiences and identity
- Evidence-based practices with appropriate adaptations
- Respectful, culturally responsive communication
- Strengths-based focus on resilience and recovery
- Engagement of family and community resources
Further Learning Resources
- American Psychiatric Nurses Association: www.apna.org
- Substance Abuse and Mental Health Services Administration: www.samhsa.gov
- National Alliance on Mental Illness: www.nami.org
- National Institute of Mental Health: www.nimh.nih.gov
- Mental Health America: www.mhanational.org
