Cardiac Disease in Pregnancy
Comprehensive Nursing Notes
An essential guide for nursing assessment, care planning, and management
Table of Contents
Introduction to Cardiac Disease in Pregnancy
Cardiac disease in pregnancy presents unique challenges for healthcare providers due to the significant physiological changes that occur during pregnancy. It is estimated that 1-4% of all pregnancies are complicated by cardiac disease, with mortality rates as high as 7% in high-risk cases. Cardiovascular disease (CVD) has emerged as the leading cause of pregnancy-related maternal death in the United States.
Key facts about cardiac disease in pregnancy:
- Leading cause of indirect maternal mortality in developed countries
- Occurs in approximately 1-4% of all pregnancies
- Up to two-thirds of CVD-related maternal deaths are preventable with proper counseling and targeted interventions
- Risk is increasing due to rising rates of hypertension, diabetes mellitus, obesity, and advanced maternal age
- Early recognition and multidisciplinary care can significantly improve outcomes
Understanding the intersection of cardiovascular health and pregnancy is essential for nurses to provide optimal care for this vulnerable patient population. This comprehensive guide will focus on the pathophysiology, assessment, nursing management, and patient education aspects of cardiac disease in pregnancy.
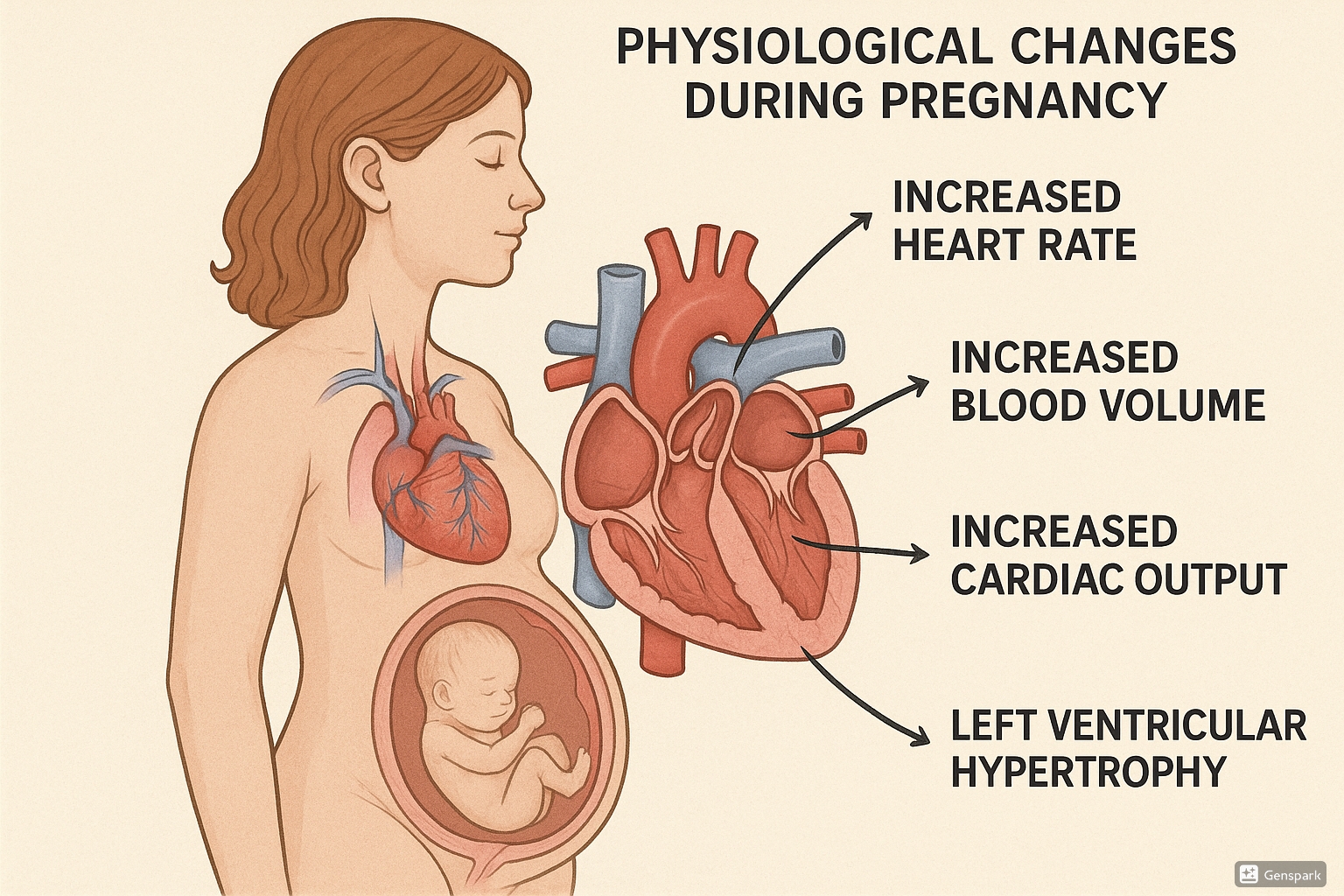
Cardiovascular Physiology in Pregnancy
Pregnancy induces significant hemodynamic changes that begin as early as 5 weeks gestation and peak during the second trimester. These adaptations are necessary to meet the increased metabolic demands of both mother and fetus but can unmask or exacerbate underlying cardiac conditions.
The major cardiovascular adaptations during pregnancy include:
- Increased cardiac output (30-50% above baseline)
- Expanded blood volume (40-50% increase)
- Elevated heart rate (15-20 beats per minute increase)
- Decreased systemic vascular resistance (up to 30% reduction)
- Slight decrease in blood pressure during first and second trimesters
Memory Aid: “PRIME” Changes
Remember the primary cardiovascular changes in pregnancy with “PRIME”:
- Plasma volume increases (40-50%)
- Rate of heartbeat increases (15-20 bpm)
- Increased cardiac output (30-50%)
- Minimal blood pressure changes (slight decrease then return to baseline)
- Evident decrease in systemic vascular resistance (30%)
Structural Cardiac Changes
The heart undergoes several structural adaptations during pregnancy:
- Left ventricular mass increases by up to 50% by the third trimester
- Eccentric hypertrophy with increased septal thickness
- Enlargement of all four cardiac chambers
- Mild physiologic valvular regurgitation may occur due to annular dilation
These structural changes typically reverse within 6-8 months postpartum but can pose challenges for women with pre-existing cardiac conditions.
Classification of Cardiac Disease in Pregnancy
The World Health Organization (WHO) has established a modified classification of maternal cardiovascular risk that serves as a valuable tool for risk stratification and management planning in pregnant women with cardiac conditions.
| WHO Classification | Risk Level | Clinical Examples | Recommendations |
|---|---|---|---|
| Class I | No detectable increased risk of maternal mortality; slight increase in morbidity |
|
Routine prenatal care; cardiology evaluation once during pregnancy |
| Class II | Small increased risk of maternal mortality; moderate increase in morbidity |
|
Cardiology evaluation each trimester; close monitoring during labor and delivery |
| Class II-III | Intermediate increased risk (depends on individual) |
|
Expert cardiology consultation; monthly or bimonthly cardiac evaluations |
| Class III | Significantly increased risk of maternal mortality or severe morbidity |
|
Expert counseling; frequent (monthly) cardiac and obstetric monitoring throughout pregnancy |
| Class IV | Extremely high risk of maternal mortality or severe morbidity |
|
Pregnancy contraindicated; if pregnancy occurs, termination should be discussed; if continued, intensive specialist monitoring required |
Clinical Pearl
The WHO classification system has proven to be more accurate than NYHA functional classification in predicting cardiac events during pregnancy. WHO Class III and IV patients should be managed by specialized cardio-obstetrics teams at centers with experience in high-risk pregnancies.
Types of Cardiac Disease in Pregnancy
1. Cardiomyopathies
Peripartum Cardiomyopathy (PPCM)
A form of heart failure that presents in the last month of pregnancy or within 5 months postpartum in women without pre-existing cardiac disease.
Key Features:
- Incidence: 1 in 1,000 to 4,000 pregnancies
- Risk factors: Advanced maternal age, multiparity, African ancestry, preeclampsia, multiple gestation
- Diagnosis: Ejection fraction < 45%, absence of other causes of heart failure
- Potential etiologies: Autoimmune processes, viral myocarditis, genetic factors, abnormal hormone signaling
Nursing Considerations:
- Monitor for signs of heart failure (dyspnea, orthopnea, edema)
- Strict intake and output monitoring
- Daily weights to track fluid status
- Medication management (focus on heart failure therapies safe in pregnancy/lactation)
- Educate on importance of follow-up as recovery may take 6-12 months
Other Cardiomyopathies
Pre-existing cardiomyopathies can worsen during pregnancy due to increased hemodynamic demands:
- Dilated Cardiomyopathy: Pregnancy generally not recommended if EF < 40%
- Hypertrophic Cardiomyopathy: Generally well-tolerated but requires monitoring for arrhythmias and heart failure
- Arrhythmogenic Right Ventricular Cardiomyopathy: Risk of arrhythmias may increase during pregnancy
2. Valvular Heart Disease
Mitral Stenosis
Most common rheumatic valvular lesion in pregnancy. Increased heart rate reduces diastolic filling time, which can lead to pulmonary congestion.
Management:
- Beta-blockers to control heart rate
- Diuretics for pulmonary congestion
- Activity restriction as needed
- Percutaneous balloon valvuloplasty in severe cases
Aortic Stenosis
Fixed obstruction prevents adequate increase in cardiac output during pregnancy. Symptoms often worsen during pregnancy.
Management:
- Maintain adequate preload
- Avoid hypotension
- Avoid excessive exertion
- Consider balloon valvuloplasty before pregnancy in severe cases
Mitral Regurgitation
Usually well-tolerated during pregnancy due to decreased systemic vascular resistance.
Management:
- Monitor for volume overload
- Diuretics if needed
- Treat heart failure if it develops
Aortic Regurgitation
Generally well-tolerated due to increased heart rate and decreased peripheral resistance.
Management:
- Monitor for heart failure symptoms
- Afterload reduction (carefully chosen medications)
- Diuretics if necessary
Memory Aid: “STOP” for Valvular Lesions
Remember which valvular lesions are poorly tolerated in pregnancy:
- Stenotic lesions are worse than regurgitant ones
- Tight mitral stenosis is most concerning
- Obstructive aortic stenosis is high risk
- Pulmonary hypertension with any valve disease dramatically increases risk
3. Congenital Heart Disease
With advances in cardiac care, more women with congenital heart disease (CHD) are reaching childbearing age. Risk during pregnancy depends on the type of defect and any residual abnormalities after repair.
| Condition | Risk Level | Key Considerations |
|---|---|---|
| Repaired ASD, VSD, PDA without residual issues | Low risk (WHO I) | Generally well-tolerated; routine pregnancy care with cardiology consultation |
| Repaired Tetralogy of Fallot | Moderate risk (WHO II) | Monitor for arrhythmias and right heart failure; more frequent follow-up |
| Fontan circulation | High risk (WHO III) | Risk of thromboembolism, arrhythmias, heart failure; requires specialized care |
| Eisenmenger syndrome | Extremely high risk (WHO IV) | Pregnancy contraindicated; maternal mortality 30-50% |
| Unrepaired cyanotic heart disease | Extremely high risk (WHO IV) | High maternal and fetal risk; pregnancy generally contraindicated |
Clinical Pearl
Women with CHD have an increased risk of having children with CHD (3-5% risk compared to 1% in general population). Fetal echocardiography is recommended at 18-22 weeks gestation for all pregnant women with CHD.
4. Ischemic Heart Disease
Though relatively uncommon in young women, the risk of myocardial infarction during pregnancy is 3-4 times higher than in non-pregnant women of the same age. The incidence is increasing due to advanced maternal age and increased prevalence of cardiovascular risk factors.
Spontaneous Coronary Artery Dissection (SCAD)
A leading cause of pregnancy-associated myocardial infarction, SCAD typically affects the left anterior descending artery during the peripartum period.
Risk Factors for Ischemic Heart Disease
- Hypertension (chronic or pregnancy-induced)
- Diabetes mellitus
- Advanced maternal age
- Obesity
- Smoking
- Dyslipidemia
- Family history of premature coronary artery disease
Management Considerations
- Coronary angiography with abdominal shielding if necessary
- PCI preferred over thrombolysis
- Bare metal stents preferred over drug-eluting stents due to shorter duration of dual antiplatelet therapy
- Aspirin generally considered safe in pregnancy
5. Arrhythmias
Arrhythmias may first appear or worsen during pregnancy due to hemodynamic changes, hormonal effects, and increased sympathetic tone.
Common Arrhythmias
- Sinus tachycardia (physiologic)
- Premature atrial contractions
- Premature ventricular contractions
- Supraventricular tachycardia
- Atrial fibrillation/flutter
- Ventricular tachycardia (less common)
Management Options
Preferences for antiarrhythmic medications in pregnancy:
- First-line: Beta-blockers (except atenolol), digoxin
- Second-line: Adenosine, verapamil, flecainide
- Use with caution: Sotalol, propafenone
- Avoid if possible: Amiodarone (risk of fetal hypothyroidism)
Nursing Assessment
Comprehensive nursing assessment is crucial for early identification of cardiac complications during pregnancy. It is important to distinguish between normal physiological changes of pregnancy and pathological signs of cardiac disease.
Focused History
- Pre-existing cardiac conditions: Previous diagnoses, surgeries, interventions
- Symptom assessment:
- Fatigue
- Dyspnea (at rest or with exertion)
- Orthopnea
- Paroxysmal nocturnal dyspnea
- Chest pain or discomfort
- Palpitations
- Syncope or near-syncope
- Peripheral edema
- Risk factors: Hypertension, diabetes, smoking, family history
- Previous pregnancies: Complications, cardiac events
- Current medications: Including over-the-counter drugs and supplements
Physical Examination
- Vital signs: Heart rate, blood pressure, respiratory rate, oxygen saturation
- Cardiovascular assessment:
- Heart sounds (murmurs, gallops, rubs)
- Jugular venous distension
- Displaced apical impulse
- Respiratory assessment:
- Work of breathing
- Lung sounds (crackles, wheezes)
- Signs of fluid overload:
- Peripheral edema
- Ascites
- Hepatomegaly
- Sacral edema
- Signs of decreased cardiac output:
- Cool extremities
- Decreased urine output
- Altered mental status
Memory Aid: “CARDIAC” Assessment
Key components for nursing assessment of cardiac disease in pregnancy:
- Cardiac history (pre-existing conditions, previous events)
- Activity tolerance (NYHA functional classification)
- Respiratory status (dyspnea, orthopnea, lung sounds)
- Dependent edema (peripheral, sacral)
- Intake and output (fluid status)
- Auscultation findings (murmurs, gallops, rubs)
- Chest pain characteristics (location, radiation, precipitating factors)
Warning Signs
Be alert for these red flags that may indicate cardiac decompensation:
- Progressive dyspnea or orthopnea
- Chest pain unrelieved by rest
- Significant arrhythmias
- Syncope or pre-syncope
- New onset or worsening peripheral edema
- Hemoptysis
- Severe palpitations with hemodynamic compromise
Diagnostic Evaluations
Various diagnostic tools are used to evaluate cardiac function during pregnancy. Nurses should be familiar with these tests and their indications.
| Diagnostic Test | Purpose | Safety Considerations | Nursing Implications |
|---|---|---|---|
| Electrocardiogram (ECG) | Detect arrhythmias, ischemic changes, chamber enlargement | Safe in all trimesters |
|
| Echocardiography | Assess cardiac structure, function, valvular disease, ejection fraction | Safe in all trimesters |
|
| Cardiac MRI | Detailed assessment of cardiac structure and function when echocardiography is inadequate | Safe in all trimesters; avoid gadolinium contrast if possible |
|
| Exercise testing | Assess functional capacity and hemodynamic response to exercise | Usually safe with monitoring; adjust protocols for pregnancy |
|
| BNP/NT-proBNP | Assess for heart failure; aid in distinguishing between cardiac and pulmonary causes of dyspnea | Blood test; safe in all trimesters |
|
| Cardiac catheterization | Definitive diagnosis of coronary artery disease or complex structural heart disease | Use only when absolutely necessary; abdominal shielding required |
|
Clinical Pearl
Echocardiography is the diagnostic test of choice during pregnancy due to its safety profile and comprehensive assessment capabilities. For peripartum cardiomyopathy diagnosis, echocardiography showing EF <45% and end-diastolic dimension >2.7cm/m² in the absence of other causes of heart failure is diagnostic.
Management Principles
Management of cardiac disease in pregnancy requires a multidisciplinary approach involving obstetricians, cardiologists, anesthesiologists, and specialized cardiac nursing care.
Pharmacologic Management
| Medication Class | Common Examples | Safety in Pregnancy | Nursing Considerations |
|---|---|---|---|
| Beta-blockers | Metoprolol, Labetalol | Generally safe; avoid atenolol |
|
| Calcium channel blockers | Nifedipine, Verapamil | Generally safe |
|
| Diuretics | Furosemide, Hydrochlorothiazide | Use with caution; may reduce placental perfusion |
|
| ACE inhibitors/ARBs | Lisinopril, Losartan | Contraindicated (teratogenic) |
|
| Hydralazine | Hydralazine | Safe; often used for hypertension in pregnancy |
|
| Nitrates | Isosorbide dinitrate | Generally safe |
|
| Anticoagulants | Heparin, LMWH, Warfarin | LMWH and UFH safe; warfarin contraindicated in first trimester |
|
| Antiarrhythmics | Adenosine, Digoxin, Flecainide | Most are relatively safe; avoid amiodarone if possible |
|
Memory Aid: “SAFE MEDS”
Medications generally considered safe in pregnancy:
- Selective beta-blockers (metoprolol)
- Adenine derivatives (adenosine)
- Furosemide (for pulmonary edema)
- Electrolyte supplements
- Methyldopa (for hypertension)
- Enoxaparin and heparin
- Digoxin
- Slow-release calcium channel blockers
Labor and Delivery Considerations
Mode of Delivery
Vaginal delivery is preferred for most women with cardiac disease, exceptions include:
- Severe aortic stenosis
- Marfan syndrome with aortic dilation >40mm
- Acute heart failure
- Mechanical prosthetic valves with anticoagulation
- Severe pulmonary hypertension
Monitoring During Labor
- Continuous ECG monitoring
- Pulse oximetry
- Regular blood pressure measurements
- Consideration of invasive hemodynamic monitoring in severe cases
- Maintain left lateral position when possible
- IV access with consideration for central venous access in high-risk cases
Anesthesia Considerations
Regional Anesthesia
- Preferred for most cardiac patients
- Provides pain relief and reduces cardiac strain
- Slow administration to avoid sudden blood pressure changes
- Careful fluid management
General Anesthesia
- May be necessary for emergencies
- Higher risk of hemodynamic instability
- Requires experienced cardiac anesthesiologist
- May be preferred in certain lesions (e.g., critical aortic stenosis)
Critical Alert
The immediate postpartum period represents a time of significant hemodynamic shifts and increased risk for cardiac decompensation. Close monitoring should continue for at least 24-72 hours after delivery, with high-risk patients requiring longer observation.
Nursing Interventions
Effective nursing care can significantly improve outcomes for pregnant women with cardiac disease. Interventions should be tailored to the specific cardiac condition and severity.
Antepartum
- Conduct thorough baseline assessment
- Monitor for signs of cardiac decompensation
- Educate about activity modification based on NYHA class
- Coordinate care between cardiology and obstetrics
- Regular monitoring of weight and vital signs
- Assist with medication adherence and education
- Support stress reduction techniques
- Facilitate dietary counseling for appropriate sodium restriction
- Teach self-monitoring techniques
- Support preparation for labor and delivery
Intrapartum
- Position to optimize venous return (left lateral)
- Continuous maternal and fetal monitoring
- Monitor for signs of fluid overload during IV therapy
- Oxygen administration as needed
- Pain management to reduce cardiac stress
- Limit active pushing in compromised patients
- Careful monitoring during stage transitions
- Prepare for potential cardiac emergencies
- Maintain normothermia
- Early identification of postpartum hemorrhage
Postpartum
- Continue cardiac monitoring for 24-72 hours
- Vigilant assessment during autotransfusion period
- Early ambulation with monitoring
- Thromboprophylaxis as indicated
- Careful fluid management
- Support lactation with consideration of medication safety
- Educate about postpartum red flags
- Facilitate contraception counseling
- Arrange follow-up care
- Screen for postpartum depression
Patient Education
Key Education Topics
Self-Monitoring
- Daily weight measurements
- Recognition of worsening symptoms
- Heart rate monitoring techniques
- When to seek immediate medical attention
- Blood pressure monitoring (if indicated)
Lifestyle Modifications
- Appropriate activity levels and limitations
- Dietary recommendations (sodium restriction if needed)
- Stress reduction techniques
- Sleep positioning (elevate head of bed if orthopneic)
- Energy conservation strategies
Medication Education
- Purpose of each medication
- Administration schedule and technique
- Common side effects
- Signs of adverse reactions
- Importance of adherence
- Medication safety during breastfeeding
Memory Aid: “RED FLAGS”
Teach patients to seek immediate medical attention for these warning signs:
- Rapid breathing that is new or worsening
- Edema that is increasing (shoes, ankles, hands)
- Dizziness, especially with position changes
- Fatigue that is severe or worsening
- Lying flat becomes increasingly difficult
- Anguishing chest pain or pressure
- Gasping for air during minimal activity
- Syncope or near-syncope episodes
Current Best Practices (2024)
The field of cardiac disease in pregnancy continues to evolve with new research and guidelines. Below are three key current best practices based on the latest evidence:
1. Universal Cardiovascular Risk Assessment
The American College of Cardiology and American Heart Association now recommend universal screening for cardiovascular risk factors during pregnancy to identify women at risk for cardiac complications.
Key components include:
- Comprehensive history and risk factor assessment
- Early screening for hypertension and diabetes
- Referral to cardio-obstetrics team for moderate to high-risk patients
- Development of individualized pregnancy management plans
- Extended postpartum follow-up for women with pregnancy-related cardiovascular complications
2. Multidisciplinary Cardio-Obstetrics Teams
The establishment of specialized cardio-obstetrics teams has emerged as a standard of care for managing pregnant women with cardiac disease.
Team composition includes:
- Maternal-fetal medicine specialists
- Cardiologists with expertise in pregnancy
- Specialized cardiac nurses
- Anesthesiologists
- Neonatologists
- Social workers
This approach has been shown to reduce maternal mortality and morbidity in high-risk cardiac patients.
3. Revised Management of Hypertension in Pregnancy
Recent studies have shifted the approach to hypertension management during pregnancy, with evidence supporting tighter blood pressure control than previously recommended.
Current recommendations include:
- Earlier treatment initiation at BP ≥140/90 mmHg
- Target BP of 110-140/85 mmHg
- Preference for labetalol, nifedipine, or methyldopa as first-line agents
- Regular home BP monitoring
- Extended postpartum follow-up (12 months)
This approach has been shown to reduce the risk of severe maternal hypertension, preeclampsia, and preterm birth.
Clinical Pearl: The “Rule of 5” in Cardiac Disease Management
Contemporary management of cardiac disease in pregnancy follows the “Rule of 5” principle:
- 5 Cardiac Risk Factors: Focus on hypertension, diabetes, dyslipidemia, obesity, and smoking cessation
- 5 Key Assessments: ECG, echocardiogram, cardiac biomarkers, functional capacity, and fetal well-being
- 5 Critical Periods: Preconception, each trimester, and postpartum require specialized attention
- 5 Essential Team Members: Obstetrician, cardiologist, anesthesiologist, neonatologist, and specialized nurse
- 5 Postpartum Priorities: Cardiac monitoring, medication adjustment, contraception counseling, lactation support, and long-term cardiovascular risk reduction
Key Takeaways
- Cardiac disease in pregnancy requires early identification, risk stratification, and multidisciplinary management
- Understanding normal cardiovascular adaptations to pregnancy is essential for distinguishing physiological from pathological changes
- The WHO classification system provides a framework for risk assessment and management planning
- Nursing care must be comprehensive, addressing monitoring, medication management, education, and emotional support
- The postpartum period represents a high-risk time for cardiac complications and requires vigilant monitoring
- Patient education about warning signs and self-monitoring is critical for early intervention
- Long-term follow-up is essential, especially for women with pregnancy complications that increase future cardiovascular risk
For the Nursing Student
Understanding cardiac disease in pregnancy requires integration of knowledge from cardiovascular nursing, obstetrics, and pharmacology. Focus on:
- Differentiating normal physiological changes from pathological signs
- Developing skilled assessment techniques specific to pregnant cardiac patients
- Understanding medication safety during pregnancy and lactation
- Practicing effective patient education and advocacy
- Working collaboratively within multidisciplinary teams
For the Practicing Nurse
Enhance your practice by:
- Staying current with evolving guidelines and best practices
- Participating in specialized training in high-risk obstetrics and cardiac care
- Developing expertise in fetal monitoring and maternal cardiac assessment
- Contributing to quality improvement initiatives in cardio-obstetrics
- Advocating for appropriate resources and support for this specialized patient population
References and Further Reading
- American Heart Association. (2020). Cardiovascular Considerations in Caring for Pregnant Patients. Circulation, 141(23), e884-e903.
- European Society of Cardiology. (2018). ESC Guidelines for the management of cardiovascular diseases during pregnancy. European Heart Journal, 39(34), 3165-3241.
- Regitz-Zagrosek, V., et al. (2018). 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. European Heart Journal, 39(34), 3165-3241.
- American College of Obstetricians and Gynecologists. (2019). Pregnancy and Heart Disease. ACOG Practice Bulletin No. 212. Obstetrics & Gynecology, 133(5), e320-e356.
- Canobbio, M.M., et al. (2017). Management of Pregnancy in Patients With Complex Congenital Heart Disease: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation, 135(8), e50-e87.
- Parsonage, W.A., et al. (2021). Heart disease and pregnancy: the need for a twenty-first century approach to care. Heart, Lung and Circulation, 30(1), 45-51.
- American College of Cardiology. (2024). Optimizing Cardiovascular Health in Pregnancy: Strategies For Healthcare Providers. Journal of the American College of Cardiology.
