Cardiovascular Diseases: Community Health Nursing Perspectives
Comprehensive Notes for Nursing Students
Table of Contents
- Introduction to Cardiovascular Diseases
- Epidemiology of Cardiovascular Diseases
- Risk Factors
- Prevention and Control Measures
- Screening and Diagnosis
- Primary Management in Community Settings
- Referral Criteria and Process
- Follow-up Care
- Considerations for Vulnerable Populations
- Health Education and Promotion
- Global Best Practices
- References
Introduction to Cardiovascular Diseases
Cardiovascular diseases (CVDs) are a group of disorders affecting the heart and blood vessels, representing the leading cause of mortality worldwide. As community health nurses, understanding the complexities of these diseases is essential for effective prevention, early detection, and management at the community level.
Cardiovascular disease encompasses a variety of conditions including:
Coronary Heart Disease
Disease of the blood vessels supplying the heart muscle, often caused by atherosclerosis (plaque buildup in arteries).
Cerebrovascular Disease
Disease of the blood vessels supplying the brain, which can lead to strokes and transient ischemic attacks.
Peripheral Arterial Disease
Disease of blood vessels supplying the arms and legs, causing reduced blood flow and symptoms like pain and fatigue.
Rheumatic Heart Disease
Damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria.
Congenital Heart Disease
Birth defects that affect the normal development and functioning of the heart due to malformations present from birth.
Deep Vein Thrombosis & Pulmonary Embolism
Blood clots in the leg veins that can dislodge and move to the heart and lungs, causing potentially fatal complications.
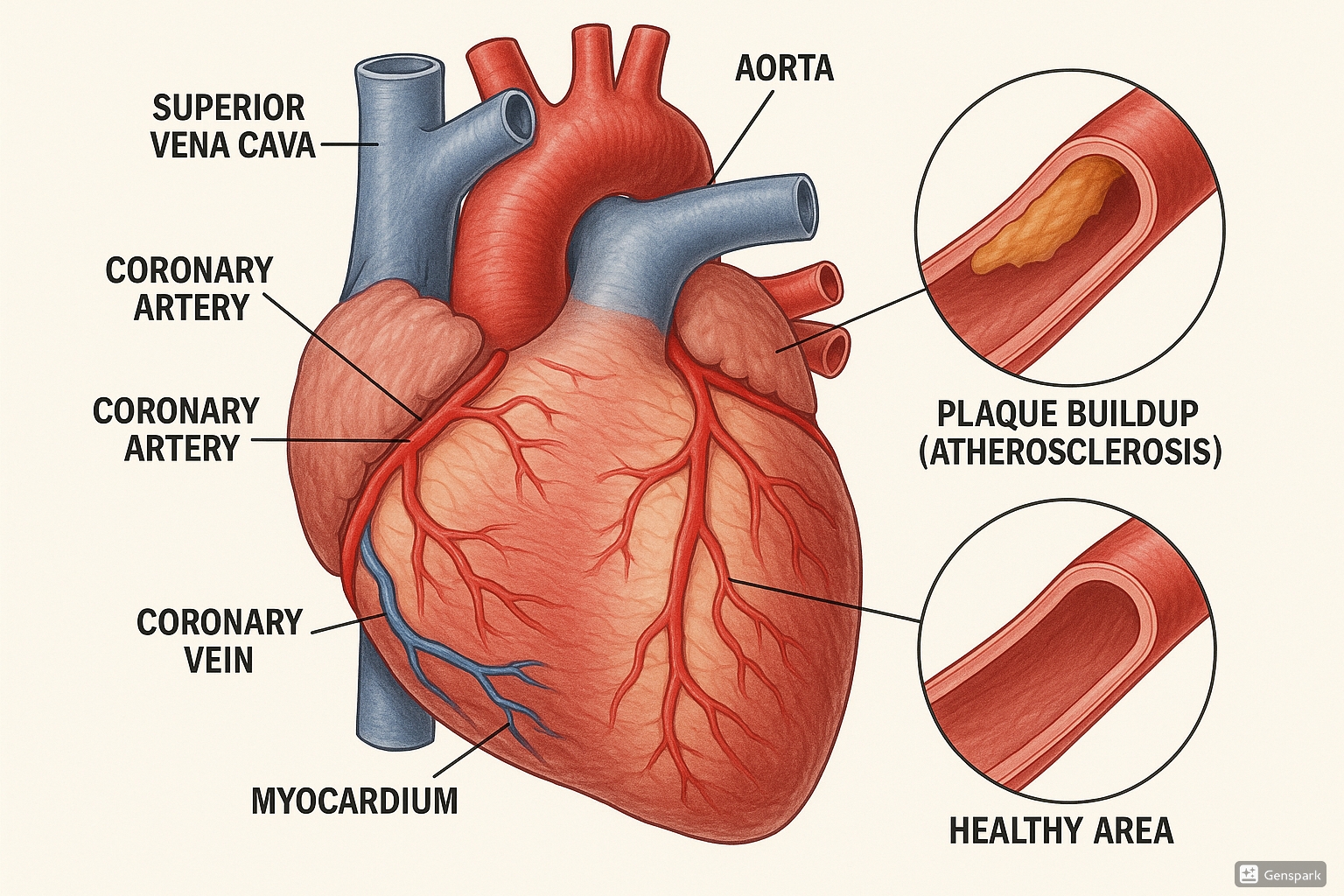
Figure 1: Anatomical illustration of heart showing atherosclerosis and coronary arteries
From a community health nursing perspective, cardiovascular disease prevention and control are critical responsibilities that require a comprehensive understanding of the epidemiology, risk factors, and evidence-based interventions at both individual and population levels.
Epidemiology of Cardiovascular Diseases
Key Epidemiological Statistics:
- CVDs are the leading cause of death globally
- An estimated 17.9 million people died from CVDs in 2019, representing 32% of all global deaths
- Of these deaths, 85% were due to heart attack and stroke
- Over three-quarters of CVD deaths take place in low- and middle-income countries
- 38% of premature deaths (under age 70) from noncommunicable diseases are caused by CVDs
Global Distribution
The burden of cardiovascular disease is not evenly distributed worldwide. Several factors influence this distribution, including socioeconomic status, healthcare accessibility, and the prevalence of risk factors in different regions.
| Region | Key Characteristics | Contributing Factors |
|---|---|---|
| High-income countries | Decreasing mortality but high prevalence | Better treatment options, aging population, high rates of obesity |
| Middle-income countries | Rapidly increasing burden | Urbanization, changing lifestyles, increasing prevalence of risk factors |
| Low-income countries | Increasing burden with highest mortality rates | Limited healthcare resources, poor access to preventive care, increasing risk factors |
| Sub-Saharan Africa | Growing burden alongside infectious diseases | Epidemiological transition, urbanization, increasing prevalence of hypertension |
| South Asia | High burden at younger ages | Genetic factors, increasing diabetes prevalence, diet changes |
Socioeconomic Impact
The relationship between cardiovascular disease and socioeconomic status is well-established and has significant implications for community health nursing practice:
- The burden of CVD is highest among individuals in lower socioeconomic status groups
- Strong relationship exists between cardiovascular health and education level, occupation, and income
- Where improvements in CVD outcomes have occurred, there is often an inequity in benefits with lesser impact on those of lower socioeconomic status
- At the household level, CVDs contribute to poverty due to catastrophic health spending and high out-of-pocket expenditure
- At the macro-economic level, CVDs place a heavy burden on the economies of low- and middle-income countries
Epidemiological Transition
Many countries are experiencing an epidemiological transition in cardiovascular disease patterns:
- Shift from infectious to noncommunicable diseases as primary causes of death
- Increasing prevalence of lifestyle-related risk factors due to urbanization
- Growing cardiovascular disease burden in younger populations
- Double burden of disease in many low- and middle-income countries (both infectious and noncommunicable diseases)
Understanding these epidemiological patterns is crucial for community health nurses to develop targeted interventions and allocate resources effectively. The high prevalence and serious consequences of cardiovascular disease highlight the importance of prevention strategies, early detection, and management at the community level.
Risk Factors
Community health nurses must have a comprehensive understanding of cardiovascular disease risk factors to effectively identify high-risk individuals and implement appropriate interventions. Risk factors can be categorized as modifiable and non-modifiable:
Modifiable Risk Factors
- Hypertension: Damages arterial walls and accelerates atherosclerosis
- Tobacco use: Damages blood vessels, reduces oxygen in blood, increases clotting risk
- Unhealthy diet: High in saturated fats, trans fats, salt, and low in fruits and vegetables
- Physical inactivity: Contributes to obesity, hypertension, and diabetes
- Harmful use of alcohol: Raises blood pressure and contributes to obesity
- Obesity: Increases strain on the heart and risk of other conditions
- Diabetes: Damages blood vessels and accelerates atherosclerosis
- High cholesterol: Contributes to atherosclerotic plaque formation
- Stress: Contributes to hypertension and unhealthy coping behaviors
- Air pollution: Damages respiratory and cardiovascular systems
Non-Modifiable Risk Factors
- Age: Risk increases with advancing age
- Gender: Men have higher risk at younger ages; risk in women increases after menopause
- Family history: Genetic predisposition to cardiovascular disease
- Ethnicity: Some ethnic groups have higher CVD risk
- Genetic factors: Inherited conditions affecting lipid metabolism, etc.
Social Determinants of Health
- Education level
- Income
- Housing conditions
- Access to healthcare
- Food security
Risk Factor Clustering
Risk factors often occur together and have synergistic effects. For example, the combination of smoking, hypertension, and high cholesterol creates a much higher risk than any single factor alone. Community health nurses should assess for multiple risk factors and understand their cumulative impact.
Mnemonic: “ABCDES” for Cardiovascular Risk Factor Assessment
- A – Age, Activity level (physical inactivity)
- B – Blood pressure (hypertension)
- C – Cholesterol, Cigarettes (smoking)
- D – Diabetes, Diet (unhealthy eating patterns)
- E – Exercise (inadequate physical activity)
- S – Stress, Socioeconomic status
Risk Assessment Tools
Several validated tools are available for cardiovascular risk assessment in community settings:
| Assessment Tool | Description | Application in Community Settings |
|---|---|---|
| Framingham Risk Score | Estimates 10-year risk of cardiovascular event based on age, gender, blood pressure, cholesterol, smoking status, and diabetes | Used in primary care settings; requires laboratory testing |
| SCORE (Systematic Coronary Risk Evaluation) | Assesses 10-year risk of fatal cardiovascular disease; adapted for different European regions | Used in European settings; variations available for high and low-risk regions |
| Non-laboratory INTERHEART Risk Score | Assesses risk without requiring blood tests; uses age, gender, smoking, diabetes, blood pressure, family history, waist-to-hip ratio, diet, physical activity, and psychosocial factors | Ideal for community screening where laboratory testing is not available |
| WHO/ISH Risk Prediction Charts | Developed for different regions globally; estimates 10-year risk of cardiovascular event | Designed for resource-limited settings; versions available without cholesterol measurement |
Community health nurses play a vital role in risk assessment, identification of high-risk individuals, and targeted interventions to modify risk factors. Understanding both individual and population-level risk factors is essential for effective cardiovascular disease prevention strategies.
Prevention and Control Measures
Prevention of cardiovascular disease is a cornerstone of community health nursing practice. The WHO estimates that nearly 75% of premature CVD deaths are preventable through addressing behavioral and environmental risk factors. Prevention strategies are typically categorized into three levels:
Primary Prevention
Aims to prevent disease onset by addressing risk factors before cardiovascular disease develops.
- Lifestyle modification counseling
- Health education programs
- Population-wide interventions
- Risk factor screening
Secondary Prevention
Focuses on early detection and treatment to prevent disease progression or complications.
- Screening for asymptomatic disease
- Early intervention for high-risk individuals
- Management of identified risk factors
- Regular monitoring
Tertiary Prevention
Aims to reduce the impact of established disease through rehabilitation and preventing complications.
- Cardiac rehabilitation programs
- Self-management support
- Prevention of recurrent events
- Medication adherence support
Evidence-Based Prevention Strategies
| Intervention Area | Specific Strategies | Implementation in Community Settings |
|---|---|---|
| Tobacco Control |
|
|
| Nutrition |
|
|
| Physical Activity |
|
|
| Blood Pressure Control |
|
|
| Cholesterol Management |
|
|
| Diabetes Prevention/Management |
|
|
Behavior Change Approaches
Effective cardiovascular disease prevention requires behavior change at individual and community levels. Community health nurses should be skilled in evidence-based behavior change techniques:
Key Behavior Change Techniques for Cardiovascular Disease Prevention
- Motivational Interviewing: Client-centered counseling approach to elicit behavior change by helping clients explore and resolve ambivalence
- Goal Setting: Collaborative establishment of specific, measurable, achievable, relevant, and time-bound (SMART) goals
- Action Planning: Detailed planning of what the person will do including when, where, and how they will perform the behavior
- Problem Solving: Analysis of factors influencing the behavior and generation of strategies to overcome barriers
- Self-monitoring: Person is asked to keep a record of specified behavior(s) as a method for changing behavior
- Social Support: Advising on, arranging, or providing social support or non-contingent praise or reward for performance of the behavior
Community-Based Interventions
Research shows that community-based interventions can successfully improve population knowledge on cardiovascular disease and risk factors and influence physical activity and dietary practices. Effective approaches include:
Community Mobilization
Engaging community members and organizations to take collective action for cardiovascular health improvement
Example: Community coalitions working to improve food environments or increase physical activity opportunities
Health Education Campaigns
Public education initiatives to increase awareness about cardiovascular disease risk factors and prevention
Example: Mass media campaigns about stroke warning signs or heart-healthy eating
Environmental Interventions
Changes to physical and social environments to support heart-healthy behaviors
Example: Creating walking trails, improving access to fresh produce, implementing smoke-free policies
Policy Advocacy
Efforts to change organizational or public policies to support cardiovascular health
Example: Advocating for reduced sodium in processed foods or improved physical education in schools
Role of Community Health Nurses in Prevention
Community health nurses play a crucial role in cardiovascular disease prevention and control through:
- Identifying high-risk individuals through screening programs
- Providing health education about cardiovascular risk factors and prevention strategies
- Implementing evidence-based interventions for risk factor modification
- Coordinating care across different settings and providers
- Monitoring and supporting medication adherence
- Advocating for policy changes to create heart-healthy environments
- Facilitating self-management support for individuals with existing CVD
- Developing and implementing community-based prevention programs
Integration of Prevention Approaches
Most effective cardiovascular disease prevention strategies integrate multiple approaches:
- Combining individual and population-level interventions
- Addressing multiple risk factors simultaneously
- Integration of prevention into routine primary healthcare
- Collaborative partnerships between healthcare, community organizations, schools, workplaces, and policymakers
- Adaptation of interventions to address social determinants of health and health equity
Screening and Diagnosis
Early detection through appropriate screening is essential for effective cardiovascular disease management. Community health nurses play a vital role in implementing screening programs and facilitating diagnosis in community settings.
Cardiovascular Screening Approaches
| Screening Type | Components | Target Population | Implementation in Community Settings |
|---|---|---|---|
| Basic Risk Factor Screening |
|
All adults, beginning at age 20 |
|
| Blood-Based Screening |
|
Adults aged 40-75; earlier for those with risk factors |
|
| Non-Laboratory Risk Assessment |
|
Adults in resource-limited settings |
|
| Targeted Screening |
|
High-risk individuals identified through initial screening |
|
Key Screening Parameters and Interpretation
Blood Pressure
| Category | Systolic (mmHg) | Diastolic (mmHg) |
|---|---|---|
| Normal | <120 | and <80 |
| Elevated | 120-129 | and <80 |
| Hypertension Stage 1 | 130-139 | or 80-89 |
| Hypertension Stage 2 | ≥140 | or ≥90 |
| Hypertensive Crisis | >180 | and/or >120 |
Blood Lipids
| Parameter | Optimal | Borderline High | High |
|---|---|---|---|
| Total Cholesterol | <200 mg/dL | 200-239 mg/dL | ≥240 mg/dL |
| LDL Cholesterol | <100 mg/dL | 130-159 mg/dL | ≥160 mg/dL |
| HDL Cholesterol | ≥60 mg/dL | 41-59 mg/dL | <40 mg/dL (low) |
| Triglycerides | <150 mg/dL | 150-199 mg/dL | ≥200 mg/dL |
Blood Glucose
| Test | Normal | Prediabetes | Diabetes |
|---|---|---|---|
| Fasting Plasma Glucose | <100 mg/dL | 100-125 mg/dL | ≥126 mg/dL |
| 2-hr Plasma Glucose (OGTT) | <140 mg/dL | 140-199 mg/dL | ≥200 mg/dL |
| HbA1c | <5.7% | 5.7-6.4% | ≥6.5% |
Body Mass Index (BMI)
| Category | BMI (kg/m²) |
|---|---|
| Underweight | <18.5 |
| Normal weight | 18.5-24.9 |
| Overweight | 25.0-29.9 |
| Obesity Class I | 30.0-34.9 |
| Obesity Class II | 35.0-39.9 |
| Obesity Class III | ≥40.0 |
Diagnostic Approaches
When screening identifies individuals at high risk or with suspected cardiovascular disease, further diagnostic testing may be needed:
Common Diagnostic Tests for Cardiovascular Disease
- Electrocardiogram (ECG/EKG): Records electrical activity of the heart to detect abnormal rhythms, evidence of previous heart attacks, or structural abnormalities
- Exercise Stress Test: Monitors heart function during physical activity to detect coronary artery disease or abnormal heart rhythms that may not be apparent at rest
- Echocardiogram: Uses ultrasound to create images of the heart’s structure and function, including chambers, valves, and blood flow
- Cardiac CT Scan: Provides detailed images of the heart and blood vessels to detect coronary artery disease, congenital heart defects, or other abnormalities
- Coronary Angiogram: Invasive procedure using contrast dye and X-rays to visualize blood flow through coronary arteries and identify blockages
- Holter Monitor: Portable ECG device worn for 24-48 hours to detect irregular heart rhythms during daily activities
Screening Implementation in Community Settings
Community health nurses face several considerations when implementing cardiovascular screening programs:
Challenges
- Limited resources and equipment
- Reaching vulnerable populations
- Cultural barriers to screening participation
- Ensuring appropriate follow-up for abnormal findings
- Maintaining accuracy in non-clinical settings
- Integration with existing healthcare systems
Successful Strategies
- Mobile screening units for underserved areas
- Collaboration with community organizations
- Use of non-laboratory risk assessment tools
- Culturally tailored screening approaches
- Clear referral pathways for follow-up care
- Integration with other health screenings
Mnemonic: “SCREEN” for Cardiovascular Screening Implementation
- S – Select appropriate screening tools for your population and setting
- C – Create protocols for abnormal findings and referrals
- R – Reach vulnerable populations through targeted outreach
- E – Educate participants about the meaning of results
- E – Ensure quality control and accuracy of measurements
- N – Network with healthcare providers for follow-up care
Community health nurses must balance the benefits of early detection with considerations of cost-effectiveness, potential for false positives, and ensuring appropriate follow-up care. Targeted screening approaches that focus on high-risk populations are often most effective in community settings with limited resources.
Primary Management in Community Settings
Community health nurses play a vital role in the primary management of cardiovascular disease within community settings. While severe cases and complications often require hospital care, many aspects of cardiovascular disease management can be effectively implemented in primary care and community contexts.
Nurse-Led Interventions
Research demonstrates the effectiveness of nurse-led interventions for cardiovascular disease management in community settings:
Evidence-Based Nurse-Led Approaches
- Nurse-Led Clinics: Dedicated cardiovascular risk management clinics run by specialized nurses have shown improvements in blood pressure control, medication adherence, and lifestyle modification
- Case Management: Proactive, coordinated care for high-risk patients including regular monitoring, education, and care coordination
- Home Visits: Particularly effective for vulnerable populations with mobility limitations or those recently discharged from hospital
- Telehealth Monitoring: Remote monitoring of blood pressure, weight, and symptoms with nurse follow-up for abnormal findings
- Group Education Programs: Structured educational interventions for patients with similar cardiovascular conditions
Risk Factor Management
| Risk Factor | Management Approaches | Nursing Interventions |
|---|---|---|
| Hypertension |
|
|
| Dyslipidemia |
|
|
| Diabetes |
|
|
| Tobacco Use |
|
|
| Obesity |
|
|
Medication Management
Community health nurses support cardiovascular medication management through:
Key Cardiovascular Medications
- Antihypertensives
- Statins and other lipid-lowering agents
- Antiplatelet medications (e.g., aspirin)
- Anticoagulants
- Beta-blockers
- ACE inhibitors/ARBs
- Diuretics
- Antiarrhythmic medications
Nursing Interventions for Medication Management
- Education about medication purpose, dosage, and schedule
- Side effect monitoring and management
- Strategies to improve adherence (pill boxes, reminder systems)
- Monitoring for drug interactions
- Facilitating communication with prescribers
- Medication reconciliation
- Support for medication affordability issues
Self-Management Support
Empowering patients with cardiovascular disease to actively participate in their care is a fundamental component of community-based management. Community health nurses facilitate self-management through:
Self-Management Support Strategies
- Symptom Monitoring: Teaching patients to recognize and respond to warning signs
- Action Plans: Developing personalized plans for managing symptoms and responding to exacerbations
- Goal Setting: Collaboratively establishing meaningful health goals
- Problem-Solving Skills: Building capacity to address barriers to self-care
- Self-Monitoring Tools: Supporting use of blood pressure monitors, weight logs, symptom diaries
- Health Literacy Enhancement: Ensuring patients understand their condition and treatment
- Psychological Support: Addressing anxiety, depression, and stress related to cardiovascular disease
Community-Based Cardiac Rehabilitation
While traditional cardiac rehabilitation often occurs in specialized facilities, community-based models have been developed to improve accessibility:
Components of Community-Based Cardiac Rehabilitation
- Physical Activity: Structured exercise programs adapted to community settings
- Education: Group sessions on cardiovascular health, nutrition, medication management
- Risk Factor Modification: Targeted interventions for smoking cessation, weight management
- Psychosocial Support: Addressing depression, anxiety, and social isolation
- Vocational Counseling: Support for return to work and daily activities
Community health nurses may coordinate these programs or work with allied health professionals to deliver comprehensive rehabilitation services.
Treatment Adherence Support
Nonadherence to treatment plans is a significant challenge in cardiovascular disease management. Community health nurses can implement strategies to improve adherence:
- Simplifying medication regimens where possible
- Addressing barriers (financial, logistical, cultural)
- Using teach-back method to ensure understanding
- Involving family members in management plans
- Implementing reminder systems
- Regular follow-up and reinforcement
- Culturally appropriate education materials
Referral Criteria and Process
Community health nurses must recognize when patients require referral to other healthcare providers or specialized services. Clear referral criteria and efficient processes are essential for timely and appropriate care.
Indications for Referral
| Urgency Level | Clinical Presentations | Referral Destination |
|---|---|---|
| Emergency (Immediate) |
|
Emergency department via emergency medical services |
| Urgent (Within 24-48 hours) |
|
Primary care provider or cardiologist on urgent basis |
| Semi-Urgent (Within 1-2 weeks) |
|
Primary care provider or cardiology referral |
| Routine (Within 1-3 months) |
|
Primary care provider or cardiology referral |
Referral Process
Community health nurses should follow established protocols for cardiovascular disease referrals:
Steps in the Referral Process
- Assessment: Comprehensive assessment including vital signs, symptoms, risk factors, and existing treatments
- Documentation: Clear documentation of findings indicating need for referral
- Communication: Contact with receiving provider/facility with concise summary of concerns
- Patient Education: Explanation to patient regarding reason for referral, expected process, and importance of follow-through
- Coordination: Arrangement of appointment, transportation if needed, and transfer of relevant records
- Follow-up: Verification that patient attended referral appointment and receipt of feedback from specialist
Referral Destinations
Specialist Providers
- Cardiologists: Specialized care for heart conditions
- Vascular Specialists: Management of peripheral arterial disease
- Endocrinologists: Management of diabetes and metabolic disorders
- Nephrologists: Management of hypertension with kidney involvement
- Neurologists: Evaluation of neurological symptoms related to cerebrovascular disease
Specialized Services
- Cardiac Rehabilitation Programs: Structured exercise and education
- Smoking Cessation Programs: Specialized support for tobacco dependence
- Dietitian Services: Nutritional counseling for cardiovascular health
- Heart Failure Clinics: Specialized management for heart failure patients
- Anticoagulation Clinics: Monitoring for patients on anticoagulant therapy
- Mental Health Services: Support for depression, anxiety related to cardiovascular disease
Information Transfer
Effective communication between community health nurses and referral destinations is crucial for continuity of care. Information to be included in referrals:
Mnemonic: “CARDIOV” for Cardiovascular Referral Information
- C – Chief complaint and current symptoms
- A – Assessment findings (vital signs, physical examination)
- R – Risk factors for cardiovascular disease
- D – Diagnostic test results available
- I – Interventions already implemented
- O – Ongoing treatments and medications
- V – Vital background information (allergies, previous cardiovascular events)
Overcoming Referral Barriers
Community health nurses may need to address several barriers to successful referrals:
- Financial barriers: Connecting patients with financial assistance programs, insurance navigation
- Transportation issues: Arranging medical transportation, connecting with community services
- Language barriers: Securing interpreter services, translated materials
- Health literacy: Providing clear, simple explanations of referral purpose and process
- Care coordination gaps: Maintaining communication with all providers involved in care
Follow-up Care
Consistent, structured follow-up care is essential for effective long-term management of cardiovascular disease. Community health nurses play a critical role in ensuring continuity of care and monitoring for changes in patient status.
Components of Follow-up Care
Essential Elements of Cardiovascular Follow-up
- Regular Monitoring: Scheduled assessments of vital signs, symptoms, and risk factors
- Medication Review: Evaluation of medication effectiveness, side effects, and adherence
- Progress Evaluation: Assessment of progress toward established treatment goals
- Lifestyle Modification Support: Ongoing guidance for diet, exercise, and other lifestyle changes
- Complication Surveillance: Monitoring for signs of disease progression or new complications
- Psychosocial Assessment: Evaluation of mental health, social support, and coping
- Self-Management Support: Reinforcement of self-care skills and knowledge
Follow-up Schedule
The frequency and intensity of follow-up care should be tailored to individual patient needs, but general guidelines include:
| Cardiovascular Condition | Recommended Follow-up Schedule | Assessment Components |
|---|---|---|
| Newly Diagnosed Hypertension |
|
|
| Stable Coronary Artery Disease |
|
|
| Heart Failure |
|
|
| Post-Myocardial Infarction |
|
|
| Atrial Fibrillation |
|
|
Follow-up Methods
Community health nurses can utilize various approaches for effective follow-up care:
In-Person Visits
Traditional face-to-face appointments
- Allows comprehensive physical assessment
- Facilitates building therapeutic relationship
- Enables direct observation of symptoms
- Can be conducted in clinic or home setting
Telehealth
Remote monitoring and virtual visits
- Reduces transportation barriers
- Enables more frequent monitoring
- Can incorporate remote monitoring devices
- Effective for stable patients
Telephone Follow-up
Structured calls to assess status
- Accessible for patients without internet access
- Can be used for symptom checks
- Effective for medication adherence support
- Suitable for interim check-ins
Documentation and Communication
Thorough documentation of follow-up care is essential for continuity and quality improvement:
Essential Elements of Follow-up Documentation
- Current Status: Vital signs, symptoms, functional capacity
- Medication Review: Current medications, adherence, effectiveness, side effects
- Progress Assessment: Changes since previous visit, progress toward goals
- Interventions: Actions taken during follow-up, education provided
- Self-Management: Patient’s self-care abilities, knowledge level
- Plan: Next steps, adjustments to treatment plan, referrals
- Communication: Information shared with other providers
Red Flags During Follow-up
Community health nurses should be vigilant for warning signs that may indicate the need for more urgent assessment:
| Red Flag | Potential Significance | Action Required |
|---|---|---|
| New or worsening chest pain | Possible acute coronary syndrome or unstable angina | Immediate medical evaluation; emergency services if severe |
| Increasing shortness of breath | Possible heart failure exacerbation | Prompt assessment; urgent referral if significant |
| Rapid weight gain (>2-3 pounds in 1-2 days) | Fluid retention, possible heart failure worsening | Early assessment, medication adjustment |
| New or worsening edema | Possible heart failure progression | Evaluation within 24-48 hours |
| Syncope or presyncope | Possible arrhythmia or hemodynamic compromise | Urgent evaluation; emergency services if syncope occurred |
| Significantly elevated blood pressure | Hypertensive urgency or emergency | Prompt assessment; emergency care if >180/120 with symptoms |
| New onset palpitations | Possible arrhythmia | Earlier follow-up; urgent if accompanied by symptoms |
Strategies to Improve Follow-up Adherence
Missed follow-up appointments are common and can lead to worse outcomes. Community health nurses can implement strategies to improve adherence:
- Appointment reminders via phone, text, or mail
- Flexible scheduling options including evening or weekend appointments
- Telehealth options to reduce transportation barriers
- Coordination of multiple appointments on the same day
- Address barriers such as transportation or childcare
- Explain the importance of follow-up to patients and caregivers
- Develop a protocol for reaching out to patients who miss appointments
Considerations for Vulnerable Populations
The burden of cardiovascular disease is not evenly distributed, with vulnerable populations often experiencing higher prevalence, worse outcomes, and barriers to care. Community health nurses must consider the unique needs of these populations in their prevention and management approaches.
Socioeconomic Disparities
Research consistently shows that cardiovascular disease disproportionately affects individuals with low socioeconomic status (SES):
Impact of Socioeconomic Status on Cardiovascular Health
- Higher Prevalence: Cardiovascular risk factors and disease are more common in low SES groups
- Earlier Onset: CVD tends to develop at younger ages in low SES populations
- Worse Outcomes: Higher mortality and complication rates from cardiovascular events
- Financial Burden: CVD contributes to poverty through catastrophic health spending and lost income
- Limited Benefit from Improvements: When CVD outcomes improve overall, there is often an inequity in benefits with lesser impact on those of lower socioeconomic status
Key Vulnerable Populations
Low Income Individuals
Specific challenges and approaches:
- Limited access to healthy foods
- Financial barriers to medication adherence
- Unstable housing affecting self-care abilities
- Higher exposure to environmental stressors
Interventions: Medication assistance programs, connection to food assistance, community-based care
Racial and Ethnic Minorities
Specific challenges and approaches:
- Higher prevalence of hypertension in Black populations
- Higher diabetes rates in Hispanic and Native American groups
- Cultural barriers to healthcare engagement
- Experiences of discrimination in healthcare
Interventions: Culturally tailored education, diverse healthcare workforce, community health workers
Rural Populations
Specific challenges and approaches:
- Limited access to specialty cardiovascular care
- Transportation barriers to healthcare services
- Fewer resources for lifestyle modification
- Higher rates of risk factors like smoking
Interventions: Telehealth services, mobile health units, community paramedicine
Older Adults
Specific challenges and approaches:
- Multiple comorbidities complicating management
- Polypharmacy and risk of drug interactions
- Cognitive and functional limitations affecting self-care
- Social isolation and limited support systems
Interventions: Medication reconciliation, caregiver education, home-based services
Addressing Barriers to Care
Community health nurses should implement strategies to overcome common barriers to cardiovascular care for vulnerable populations:
| Barrier | Impact on Cardiovascular Care | Nursing Interventions |
|---|---|---|
| Financial Constraints |
|
|
| Low Health Literacy |
|
|
| Transportation Issues |
|
|
| Language Barriers |
|
|
Cultural Considerations
Cultural factors can significantly influence cardiovascular health beliefs, behaviors, and care-seeking patterns:
Culturally Sensitive Cardiovascular Care
- Health Beliefs: Understanding cultural explanations for cardiovascular disease and incorporating these into education
- Dietary Practices: Adapting heart-healthy dietary recommendations to include culturally important foods
- Family Involvement: Recognizing the role of family in decision-making and care processes in different cultures
- Communication Styles: Adjusting communication approaches to align with cultural norms about health discussions
- Traditional Practices: Acknowledging and working with traditional healing practices that may complement conventional care
- Stigma: Addressing potential stigma associated with chronic disease in some cultural contexts
Effective Approaches for Vulnerable Populations
Several approaches have shown promise in addressing cardiovascular health disparities:
- Community Health Workers: Trained community members who share cultural, linguistic, and experiential backgrounds with the population served
- Faith-Based Initiatives: Collaborations with religious organizations to deliver culturally resonant cardiovascular health programs
- Multidisciplinary Teams: Comprehensive care addressing medical, social, and environmental factors
- Community-Based Participatory Research: Engaging community members in developing and implementing interventions
- Policy Advocacy: Working to address structural factors contributing to health disparities
- Mobile Health Technologies: Using accessible technology to overcome geographic and transportation barriers
Health Education and Promotion
Health education and promotion are cornerstone activities for community health nurses working to prevent and manage cardiovascular disease. Effective educational approaches can increase awareness, improve risk factor management, and enhance self-care abilities.
Educational Content Areas
Understanding Cardiovascular Disease
- Basic anatomy and physiology
- Disease processes and progression
- Risk factors and their significance
- Relationship between lifestyle and CVD
Lifestyle Modifications
- Heart-healthy dietary patterns
- Physical activity guidelines
- Smoking cessation strategies
- Stress management techniques
- Alcohol moderation
Self-Monitoring Skills
- Blood pressure measurement
- Heart rate monitoring
- Weight tracking
- Symptom recognition
- Food and activity journaling
Medication Management
- Medication purposes and mechanisms
- Proper administration techniques
- Common side effects
- Adherence strategies
- When to seek help for medication issues
Warning Signs and Emergency Response
- Heart attack and stroke symptoms
- When and how to call emergency services
- Red flags for heart failure exacerbation
- Creating an emergency action plan
Psychosocial Adaptation
- Coping with chronic disease
- Addressing depression and anxiety
- Building social support networks
- Stress management techniques
Educational Approaches
Community health nurses should employ a variety of educational strategies to accommodate different learning styles and needs:
Evidence-Based Educational Methods
- Individual Counseling: One-on-one education tailored to specific needs and learning pace
- Group Education: Classes or workshops providing peer support and shared learning
- Demonstration and Return Demonstration: Showing skills and having patients practice under supervision
- Written Materials: Pamphlets, handouts, and workbooks for reinforcement and reference
- Audiovisual Resources: Videos, apps, and interactive media for visual and auditory learners
- Teach-Back Method: Asking patients to explain key concepts in their own words to confirm understanding
- Peer Education: Learning from others with similar health conditions
- Motivational Interviewing: Collaborative conversation to strengthen motivation for change
Health Literacy Considerations
Limited health literacy can significantly impact understanding of cardiovascular disease and adherence to treatment plans. Community health nurses should:
Addressing Low Health Literacy
- Use plain, non-medical language
- Focus on 2-3 key points per session
- Supplement verbal with visual information
- Use concrete examples related to daily life
- Create a shame-free environment for questions
- Check understanding with teach-back method
- Provide materials at appropriate reading level (5th-6th grade)
Enhancing Comprehension and Recall
- Use “chunk and check” approach (small pieces of information followed by verification)
- Create visual aids like pill cards for medications
- Use analogies to explain complex concepts
- Prioritize “need to know” over “nice to know” information
- Provide audio recordings of key instructions
- Involve family members or caregivers
- Schedule follow-up to reinforce information
Community-Based Health Promotion
Beyond individual education, community health nurses should engage in broader health promotion activities:
Community-Level Cardiovascular Health Promotion
- Public Awareness Campaigns: Mass media, social media, and community events to raise awareness about cardiovascular health
- Community Screenings: Blood pressure, cholesterol, and diabetes screening events in accessible locations
- Environmental Interventions: Advocacy for heart-healthy community environments (walking paths, smoke-free spaces)
- School-Based Programs: Education about cardiovascular health for children and adolescents
- Workplace Wellness: Programs targeting cardiovascular health in employment settings
- Community Coalitions: Partnerships with multiple stakeholders to address cardiovascular health
- Policy Advocacy: Working for policies that support cardiovascular health (tobacco control, food labeling)
Mnemonic: “HEARTS” for Cardiovascular Health Education
- H – Holistic approach addressing physical, emotional, and social aspects
- E – Engaging delivery methods that actively involve the learner
- A – Actionable information that can be immediately applied
- R – Relevant content tailored to individual needs and context
- T – Teach-back to confirm understanding
- S – Simplified language appropriate for health literacy level
Evaluating Education Effectiveness
Community health nurses should regularly assess the impact of their educational interventions:
- Knowledge Assessment: Pre/post testing of cardiovascular knowledge
- Behavior Change Monitoring: Tracking adoption of recommended lifestyle changes
- Clinical Outcomes: Measuring changes in risk factors (blood pressure, cholesterol, weight)
- Self-Efficacy Measurement: Assessing confidence in self-management abilities
- Patient Satisfaction: Gathering feedback on educational experiences
- Quality of Life Indicators: Evaluating impact on functional status and wellbeing
Global Best Practices
Cardiovascular disease is a global health challenge, with different regions developing innovative approaches to prevention and management. This section highlights exemplary practices from around the world that community health nurses can learn from and potentially adapt to their contexts.
Integrated Care Models
Finland’s North Karelia Project
This pioneering community-based intervention achieved remarkable reductions in cardiovascular mortality through:
- Comprehensive community engagement
- Policy changes in food production and labeling
- Mass media campaigns
- Integration with primary healthcare
- Cross-sector collaboration
Key lesson: Community-wide approaches combining policy, environmental changes, and individual interventions can dramatically reduce CVD burden.
United Kingdom’s NHS Health Checks
A systematic cardiovascular risk assessment program offering:
- Standardized risk assessment for adults 40-74
- Integration with primary care
- Risk stratification and tailored interventions
- Linkage to lifestyle modification programs
- National data collection and monitoring
Key lesson: Systematic, population-wide screening can identify high-risk individuals for targeted interventions.
Task-Shifting and Workforce Innovation
Brazil’s Family Health Strategy
Community-based primary care model featuring:
- Multidisciplinary teams including community health workers
- Population-based coverage with defined territories
- Proactive home visits for cardiovascular risk assessment
- Integration of prevention with treatment
- Focus on family and community context
Key lesson: Community health workers can effectively extend cardiovascular care to underserved populations.
India’s ASHA Program
Accredited Social Health Activists providing:
- Community-based cardiovascular risk screening
- Health education and lifestyle counseling
- Facilitation of referrals to primary care
- Medication adherence support
- Regular home visits for monitoring
Key lesson: Lay health workers can successfully bridge gaps between communities and formal healthcare systems.
Technology-Enhanced Approaches
Australia’s Integrated Cardiac Telehealth
Comprehensive telehealth model including:
- Remote monitoring for rural and indigenous populations
- Nurse-led video consultations
- Digital cardiac rehabilitation programs
- Electronic health records integration
- Smartphone apps for self-management
Key lesson: Telehealth can effectively overcome geographic barriers to cardiovascular care.
Sweden’s Digital First Strategy
Digital health approaches including:
- Online risk assessment tools
- Virtual nurse consultations
- Automated screening reminders
- Patient access to electronic health records
- Wearable device integration with healthcare systems
Key lesson: Digital tools can empower patients and extend the reach of cardiovascular prevention programs.
Policy and Systems Approaches
Exemplary Policy Interventions
- South Africa’s Salt Reduction Legislation: Mandatory limits on sodium content in processed foods, resulting in population-wide blood pressure reductions
