Care of Patients with Urinary Diversions
Comprehensive Nursing Notes for Evidence-Based Practice
Learning Objectives
Upon completion of this module, nursing students will be able to:
- Identify the three main types of urinary diversions and their indications
- Demonstrate comprehensive preoperative and postoperative nursing care
- Recognize and manage complications associated with urinary diversions
- Implement evidence-based patient education strategies
- Apply critical thinking skills in assessment and intervention planning
- Collaborate effectively with the interdisciplinary healthcare team
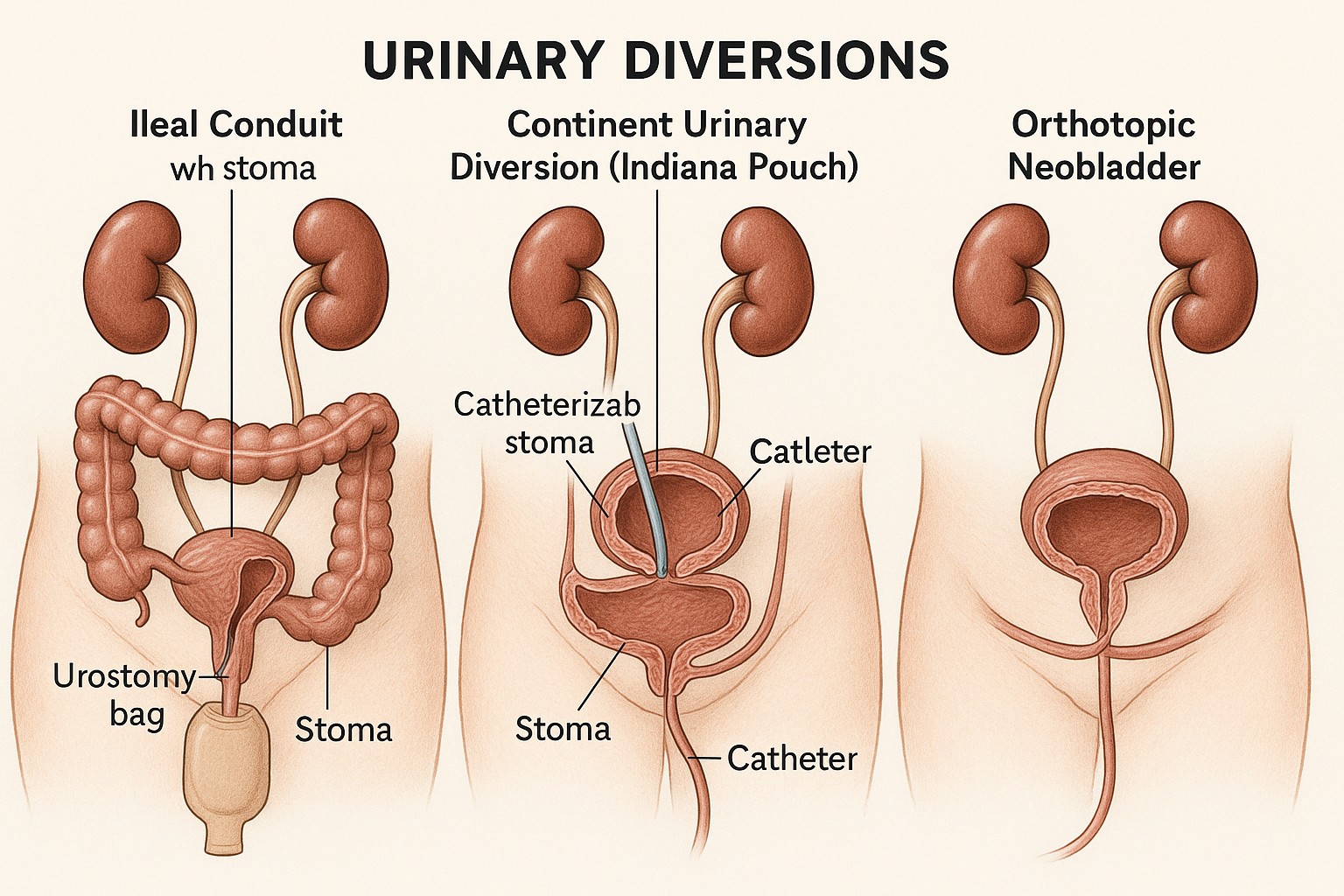
Figure 1: Three Main Types of Urinary Diversions – Ileal Conduit, Continent Diversion, and Orthotopic Neobladder
Introduction
Urinary diversions are surgical procedures that create alternative pathways for urine elimination when the normal urinary tract is compromised. These complex procedures require specialized nursing care to ensure optimal patient outcomes and quality of life. As a nursing professional, understanding the intricacies of urinary diversion care is essential for providing comprehensive, evidence-based patient care.
This comprehensive guide covers the three main types of urinary diversions: ileal conduits, continent cutaneous diversions, and orthotopic neobladders. Each type presents unique challenges and opportunities for nursing intervention.
Anatomy & Physiology Review
Normal Bladder Function
- Storage Phase: Low-pressure reservoir (0-15 cmH2O)
- Voiding Phase: Coordinated detrusor contraction
- Capacity: 300-500 mL in healthy adults
- Innervation: Parasympathetic (S2-S4) and sympathetic (T10-L2)
Bladder Layers
- Urothelium: Transitional epithelium barrier
- Lamina Propria: Connective tissue, vessels, nerves
- Muscularis Propria: Detrusor muscle layer
- Serosa: Outer protective layer
Memory Aid: Bladder Layers
“Uncle Larry Makes Soup”
- Urothelium
- Lamina Propria
- Muscularis Propria
- Serosa
Types of Urinary Diversions
1. Ileal Conduit (Incontinent Diversion)
Procedure Overview
- • 15-20 cm of ileum isolated as conduit
- • Ureters anastomosed to proximal end
- • Distal end brought to abdominal wall as stoma
- • Continuous urine drainage into collection bag
- • Most common type of urinary diversion
Indications
- • Muscle-invasive bladder cancer
- • Neurogenic bladder dysfunction
- • Radiation cystitis
- • Congenital anomalies
- • Poor candidacy for continent diversion
2. Continent Cutaneous Diversion (Indiana Pouch)
Procedure Overview
- • Uses ascending colon and terminal ileum
- • Creates internal reservoir (400-500 mL)
- • Catheterizable channel to skin
- • Patient empties via intermittent catheterization
- • Provides continence without external appliance
Patient Requirements
- • Manual dexterity for catheterization
- • Motivation for self-care
- • Adequate renal function
- • Understanding of complications
- • Ability to perform 4-6 catheterizations daily
3. Orthotopic Neobladder (Bladder Substitution)
Procedure Overview
- • Uses 55-60 cm of ileum
- • Creates spherical reservoir in pelvis
- • Anastomosed to intact urethra
- • Allows voiding through natural pathway
- • Requires learning new voiding technique
Contraindications
- • Urethral involvement by tumor
- • Severe renal impairment (CrCl <35-40 mL/min)
- • Hepatic insufficiency
- • Cognitive impairment
- • Inability to perform catheterization
| Characteristic | Ileal Conduit | Continent Diversion | Neobladder |
|---|---|---|---|
| Continence | Incontinent | Continent | Continent |
| Voiding Method | Continuous drainage | Intermittent catheterization | Valsalva voiding |
| Appliance Required | Yes | No | No |
| Operative Time | Shortest | Longest | Moderate |
| Metabolic Acidosis Risk | Low (5-15%) | High (26-45%) | Moderate (6-13%) |
Memory Aid: Diversion Selection
“I Can Name” the three types:
- Ileal Conduit – Incontinent, simplest
- Continent Diversion – Catheterizable, complex
- Neobladder – Natural voiding, neurologically intact
Preoperative Nursing Care
Comprehensive Assessment
Physical Assessment
- • Nutritional status (albumin, prealbumin)
- • Renal function (creatinine, BUN, GFR)
- • Hepatic function (if neobladder planned)
- • Cardiac and pulmonary status
- • Cognitive function and manual dexterity
- • Abdominal examination for surgical history
Psychosocial Assessment
- • Coping mechanisms and support systems
- • Body image concerns
- • Educational needs and learning style
- • Cultural and religious considerations
- • Financial concerns about supplies
- • Living situation and self-care ability
Patient Education Priorities
Stoma Site Selection Process
Patient Assessment
Evaluate sitting, standing, and supine positions
Anatomical Considerations
Identify rectus muscle, avoid bony prominences
Lifestyle Factors
Consider clothing, activities, and occupation
Mark and Document
Use indelible marker, photograph if possible
Optimization of Health Status
- • Smoking cessation counseling (minimum 2 weeks prior)
- • Nutritional support if albumin <3.0 g/dL
- • Anemia correction if Hgb <10 g/dL
- • Diabetes management (HbA1c <7%)
- • Cardiac clearance if indicated
Medication Management
- • Anticoagulation protocol per surgical guidelines
- • Bowel preparation if using colon
- • Antibiotic prophylaxis per institution protocol
- • DVT prophylaxis planning
- • Pain management planning
Enterostomal Therapy Consultation
- • Stoma site marking and patient education
- • Appliance selection and fitting
- • Demonstration of care techniques
- • Resource identification and contact information
- • Psychological support and counseling
Postoperative Nursing Care
Immediate Postoperative Priorities (0-24 hours)
Monitoring
- • Vital signs and hemodynamic stability
- • Urine output and character (goal >30 mL/hr)
- • Stoma viability and color
- • Drain output and character
- • Pain assessment and management
- • Neurological status
Interventions
- • Maintain catheter patency
- • Monitor for bleeding/hematuria
- • Assess for signs of infection
- • Support respiratory function
- • Prevent thromboembolism
- • Promote early mobilization
Memory Aid: Stoma Assessment “COAST”
- Color – Should be red/pink, not dusky or black
- Output – Urine flow and character
- Appliance – Fit and seal integrity
- Size – Edema reduction over time
- Tissue – Peristomal skin integrity
Ileal Conduit Care
- • Maintain urostomy appliance seal
- • Empty bag when 1/3 full
- • Monitor for mucus in urine (normal)
- • Assess for stomal stenosis
- • Educate about appliance changes
Continent Diversion Care
- • Maintain catheter patency
- • Monitor reservoir capacity
- • Assess for mucus plugging
- • Teach catheterization technique
- • Monitor for pouch-related complications
Neobladder Care
- • Maintain urethral and suprapubic catheters
- • Monitor for urethral-enteric anastomotic leak
- • Assess for excessive mucus production
- • Prepare for Valsalva voiding training
- • Monitor for retention/incomplete emptying
Complications and Management
Early Complications (0-30 days)
Surgical Complications
- • Urine leak: 5-15% incidence
- • Ileus: 20% incidence
- • Wound infection: 10-25% incidence
- • Anastomotic bleeding: 3-8% incidence
- • Stoma ischemia: 1-3% incidence
Medical Complications
- • Pneumonia: 5-15% incidence
- • DVT/PE: 3-8% incidence
- • Dehydration: 10-20% incidence
- • Electrolyte imbalances: 15-30% incidence
- • Sepsis: 2-5% incidence
Late Complications (>30 days)
Metabolic
- • Hyperchloremic acidosis
- • Vitamin B12 deficiency
- • Bone demineralization
- • Chronic kidney disease
- • Electrolyte abnormalities
Structural
- • Ureteral stricture (3-17%)
- • Parastomal hernia (5-65%)
- • Stomal stenosis (2-10%)
- • Reservoir stones (4-42%)
- • Chronic pyelonephritis
Functional
- • Urinary incontinence
- • Incomplete emptying
- • Recurrent UTIs
- • Mucus production
- • Erectile dysfunction
Urine Leak Management Protocol
Identify Leak
Decreased urine output, abdominal pain, fever
Assessment
CT scan, drain output analysis, laboratory studies
Conservative Management
Maintain catheter drainage, monitor closely
Surgical Intervention
If conservative management fails after 7-10 days
Evidence-Based Nursing Interventions
Research-Supported Interventions
Pain Management
- • Multimodal analgesia reduces opioid requirements
- • Regional blocks improve early mobilization
- • Patient-controlled analgesia increases satisfaction
- • Non-pharmacological interventions reduce total pain scores
Infection Prevention
- • Chlorhexidine skin preparation reduces SSI by 40%
- • Antibiotic prophylaxis within 60 minutes of incision
- • Maintenance of normothermia reduces infection risk
- • Early catheter removal decreases CAUTI incidence
Enhanced Recovery After Surgery (ERAS) Protocol
Preoperative
- • Carbohydrate loading 2-3 hours before
- • Minimize fasting duration
- • Smoking cessation counseling
- • Patient education and expectation setting
Intraoperative
- • Goal-directed fluid therapy
- • Maintain normothermia
- • Multimodal analgesia
- • Minimize opioid use
Postoperative
- • Early mobilization (POD 1)
- • Early feeding when tolerated
- • Proactive nausea management
- • Daily assessment for discharge readiness
Patient Education & Discharge Planning
Discharge Readiness Criteria
Physical Criteria
- • Stable vital signs
- • Adequate pain control with oral medications
- • Bowel function returned
- • Adequate oral intake
- • Ambulating independently
- • Urine output >30 mL/hr
Educational Criteria
- • Demonstrates stoma/catheter care
- • Verbalizes signs of complications
- • Understands medication regimen
- • Has follow-up appointments scheduled
- • Home care resources arranged
- • Emergency contact information provided
Ileal Conduit Teaching
- • Appliance changing technique
- • Skin care and barrier products
- • Emptying schedule (1/3 full)
- • Nighttime drainage system
- • Activity and bathing guidelines
- • Supply ordering and storage
- • Signs of complications
Continent Diversion Teaching
- • Catheterization technique
- • Catheter care and storage
- • Emptying schedule (4-6 times daily)
- • Mucus management
- • Capacity building exercises
- • Backup catheter availability
- • When to seek medical attention
Neobladder Teaching
- • Valsalva voiding technique
- • Timed voiding schedule
- • Intermittent catheterization
- • Kegel exercises
- • Nighttime incontinence management
- • Fluid management strategies
- • Gradual activity progression
Memory Aid: Discharge Teaching “EDUCATE”
- Equipment and supplies needed
- Demonstration of care techniques
- Understanding of complications
- Contact information for emergencies
- Activity restrictions and progression
- Timing of follow-up appointments
- Emergency signs requiring immediate attention
Long-term Care Considerations
Lifelong Surveillance Requirements
Annual Assessments
- • Comprehensive metabolic panel
- • Vitamin B12 levels
- • Bone density screening (DEXA)
- • Imaging of upper urinary tract
- • Cardiovascular risk assessment
Periodic Evaluations
- • Functional capacity assessment
- • Quality of life evaluation
- • Stomal and skin integrity
- • Psychosocial adjustment
- • Nutritional status review
Quality of Life Optimization
Physical Well-being
- • Regular exercise program
- • Adequate hydration
- • Nutritional counseling
- • Skin care routines
- • Sleep hygiene
Emotional Health
- • Counseling services
- • Support group participation
- • Body image therapy
- • Stress management
- • Relationship counseling
Social Integration
- • Return to work planning
- • Travel considerations
- • Activity modifications
- • Intimacy counseling
- • Community resources
Interprofessional Collaboration
Core Team Members
Urologist
Surgical management, complication treatment
Registered Nurse
Direct care, education, coordination
Enterostomal Therapist
Stoma care, appliance fitting, education
Social Worker
Psychosocial support, resource coordination
Supporting Team Members
Pharmacist
Medication management, education
Dietitian
Nutritional assessment, counseling
Physical Therapist
Mobility, strength, endurance
Occupational Therapist
ADL modification, adaptive equipment
SBAR Communication Framework
Situation
Patient identification, current status
Background
Relevant history, diversion type
Assessment
Current findings, concerns
Recommendation
Proposed actions, timeline
Summary & Key Takeaways
Essential Nursing Points
Clinical Excellence
- • Comprehensive assessment drives individualized care
- • Early recognition of complications saves lives
- • Evidence-based interventions improve outcomes
- • Patient education is fundamental to success
- • Interprofessional collaboration enhances care quality
Patient-Centered Care
- • Individual preferences guide decision-making
- • Quality of life is the ultimate goal
- • Continuous support improves adaptation
- • Family involvement enhances outcomes
- • Lifelong surveillance prevents complications
Master Memory Aid: “NURSING EXCELLENCE”
- Normalize expectations
- Understand diversion types
- Recognize complications early
- Support patient education
- Individualize care plans
- Navigate complex needs
- Guide family involvement
- Evaluate outcomes continuously
- X-ray vision for problems
- Collaborate with team
- Ensure quality of life
- Lifelong surveillance
- Lead with compassion
- Empowerment through knowledge
- Never stop learning
- Celebrate patient victories
- Exceed expectations
Additional Resources & References
Professional Organizations
- • Wound, Ostomy and Continence Nurses Society (WOCN)
- • American Urological Association (AUA)
- • International Association for Enterostomal Therapy
- • United Ostomy Associations of America
Educational Resources
- • WOCN Clinical Practice Guidelines
- • AUA/ASCO/ASTRO/SUO Guidelines
- • Cochrane Reviews on Urinary Diversions
- • StatPearls Medical Education Platform
Evidence-Based Nursing Practice
Committed to Excellence in Urological Nursing Care
