Pediatric Communicable Diseases: Chickenpox
Comprehensive Nursing Guide for Student Nurses
Introduction to Chickenpox
Chickenpox (varicella) is a highly contagious viral infection primarily affecting children. It’s characterized by an itchy, blister-like rash that appears first on the face, chest, and back before spreading throughout the body. As a nursing student, understanding chickenpox is essential for providing effective care to pediatric patients and educating families about this common childhood illness.
Key Facts About Chickenpox
- Caused by the varicella-zoster virus (VZV), a member of the herpesvirus family
- Primarily affects children aged 1-10 years
- Highly contagious with a 90% transmission rate among susceptible household contacts
- Spreads through respiratory droplets and direct contact with lesions
- Incubation period: 10-21 days (average: 14 days)
- Contagious period: 1-2 days before rash appears until all lesions have crusted
- Natural infection typically confers lifelong immunity
Pathophysiology of Chickenpox
Chickenpox is caused by the varicella-zoster virus (VZV), which enters the body through the respiratory tract or conjunctiva. The virus initially replicates in regional lymph nodes before causing primary viremia (virus in bloodstream), allowing it to spread to the liver, spleen, and other organs.
Secondary viremia occurs 4-6 days later, leading to the characteristic skin lesions. The virus infects skin cells, causing them to degenerate and form fluid-filled vesicles. After recovery, VZV remains dormant in the dorsal root ganglia and can reactivate later in life as herpes zoster (shingles).
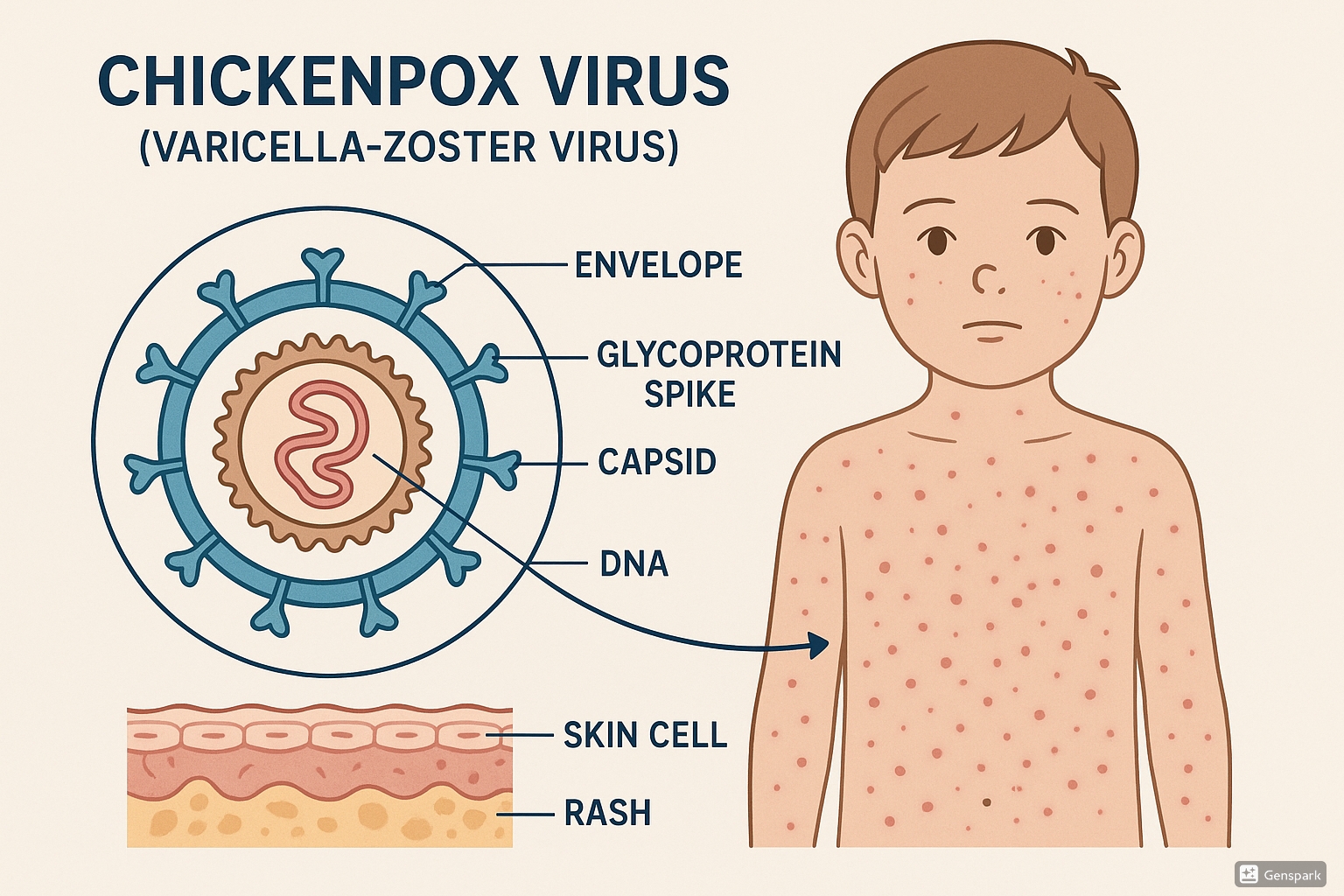
Figure 1: Varicella-zoster virus structure and skin infection process
Disease Progression Mnemonic: “VIRUS”
- V – Viral entry through respiratory tract
- I – Initial replication in lymph nodes
- R – Replication in liver and spleen (primary viremia)
- U – Ultimate spread to skin (secondary viremia)
- S – Skin lesions development (macule → papule → vesicle → pustule → crust)
Clinical Manifestations
Chickenpox typically progresses through distinct phases, with symptoms varying in severity. Understanding the characteristic presentations helps nurses accurately identify the disease and stage of progression.
Prodromal Phase (1-2 days before rash)
- Low-grade fever (38-39°C or 100.4-102.2°F)
- Malaise and fatigue
- Anorexia (loss of appetite)
- Mild headache
- General discomfort
Exanthem Phase (Skin Manifestations)
Classic “dew drop on rose petal” appearance – clear vesicles on erythematous base
Characteristic progression of lesions:
- Macules (flat, red spots)
- Papules (raised, solid bumps)
- Vesicles (clear, fluid-filled blisters)
- Pustules (cloudy, infected-looking blisters)
- Crusts (dried scabs)
Distribution pattern: Begins on face, scalp, and trunk, then spreads to extremities (centripetal distribution)
Key feature: Lesions present in different stages simultaneously (“crops” of lesions)
Systemic Symptoms
- Fever (typically higher in older children and adults)
- Intense pruritus (itching) of lesions
- Irritability
- Lymphadenopathy (swollen lymph nodes)
- Possible headache and abdominal pain
Mnemonic: “CHICKENPOX”
- Centripetal rash distribution (trunk to extremities)
- Highly contagious through respiratory droplets and direct contact
- Itching (pruritus) – severe and persistent
- Crops of lesions in different stages simultaneously
- Known to affect mucosal surfaces (mouth, conjunctiva)
- Eruptions evolve from macules to vesicles to crusts
- Notable fever before or with rash onset
- Prodrome of mild illness 1-2 days before rash
- Occasionally causes complications in high-risk groups
- X-treme care needed to prevent secondary infections
Diagnosis and Assessment
Diagnosis of chickenpox is typically based on clinical presentation, but several assessment methods and diagnostic tests can confirm the infection, especially in unclear cases.
Clinical Assessment
| Assessment Component | Key Findings in Chickenpox |
|---|---|
| History Taking |
|
| Physical Examination |
|
| Vital Signs |
|
| Skin Assessment |
|
Laboratory Confirmation
While diagnosis is primarily clinical, laboratory tests can confirm uncertain cases:
- Tzanck smear: Microscopic examination of cellular material from vesicles showing multinucleated giant cells (not specific to VZV)
- Direct fluorescent antibody (DFA) testing: Rapid test detecting viral antigens in skin lesion specimens
- Polymerase chain reaction (PCR): Most sensitive test for detecting VZV DNA in vesicular fluid or scabs
- Viral culture: Isolation of virus from vesicular fluid (takes 3-5 days)
- Serologic testing: Detection of VZV-specific antibodies (IgM and IgG) – useful for retrospective diagnosis
Nursing Alert: Differential Diagnosis
Chickenpox must be differentiated from other conditions presenting with vesicular rashes:
- Herpes simplex infection: Localized clusters of vesicles rather than widespread distribution
- Impetigo: Honey-colored crusts, limited distribution, often around nose and mouth
- Hand, foot, and mouth disease: Vesicles primarily on hands, feet, and mouth; caused by coxsackievirus
- Drug eruptions: Rash pattern different, often lacks vesicle formation in multiple stages
- Insect bites: Localized reactions, not in crops or different developmental stages
Complications of Chickenpox
While most cases of chickenpox resolve without significant issues, complications can occur, especially in high-risk populations. Nurses should be vigilant in monitoring for these potential complications.
Skin and Soft Tissue Complications
- Secondary bacterial infections: Most common complication, typically Staphylococcus aureus or Group A Streptococcus
- Cellulitis: Infection of deeper skin layers
- Impetigo: Superficial skin infection
- Scarring: Permanent marks from deep lesions or infected lesions
Neurological Complications
- Cerebellar ataxia: Most common neurological complication (1 in 4,000 cases)
- Encephalitis: Inflammation of the brain (rare, 1 in 10,000 cases)
- Aseptic meningitis: Inflammation of the meninges
- Guillain-Barré syndrome: Autoimmune disorder causing muscle weakness
Respiratory Complications
- Pneumonia: More common in adults but can occur in children with immune compromise
- Bronchitis: Inflammation of the airways
- Secondary bacterial pneumonia: Following viral pneumonia
Other Complications
- Hemorrhagic varicella: Bleeding into vesicles or beneath the skin
- Thrombocytopenia: Low platelet count
- Hepatitis: Inflammation of the liver
- Reye’s syndrome: Associated with aspirin use during chickenpox (rare)
- Nephritis: Inflammation of the kidneys
High-Risk Groups for Severe Chickenpox
- Newborns and infants whose mothers had chickenpox close to delivery date
- Immunocompromised children (HIV, cancer treatments, organ transplant recipients)
- Children on long-term steroid therapy
- Children with underlying skin conditions (eczema, burns)
- Children with chronic respiratory conditions (asthma, cystic fibrosis)
- Adolescents (typically have more severe disease than younger children)
Nursing Management in Hospital
Most children with chickenpox are managed at home, but hospitalization may be necessary for severe cases, complications, or high-risk patients. Nursing care in the hospital setting focuses on isolation, symptom management, complication prevention, and supportive care.
Isolation Precautions
- Airborne and contact isolation until all lesions have crusted (typically 5-7 days)
- Place patient in negative pressure room if available
- Personal protective equipment (PPE): N95 respirator, gown, gloves, and eye protection
- Hand hygiene before and after patient contact
- Limit visitors to those with documented immunity to chickenpox
- Cohort patients with active chickenpox when possible
Pharmacological Management
| Medication | Indication | Nursing Considerations |
|---|---|---|
| Acyclovir (Zovirax) |
Antiviral therapy for high-risk patients or severe cases Dosage: 20 mg/kg/dose four times daily (maximum 800 mg/dose) for 5-7 days |
|
| Antipyretics |
Fever management Acetaminophen (Paracetamol) preferred |
|
| Antihistamines |
Relief of pruritus (itching) Diphenhydramine (Benadryl) or cetirizine |
|
| Antibiotics |
For secondary bacterial infections only Not used prophylactically |
|
| Varicella-Zoster Immune Globulin (VZIG) |
Post-exposure prophylaxis for high-risk patients |
|
Supportive Nursing Care
Skin Care
- Apply calamine lotion to lesions to reduce itching
- Administer tepid baths with colloidal oatmeal or baking soda
- Keep fingernails short and clean to minimize skin damage from scratching
- Apply clean cotton gloves/mitts to prevent scratching in young children
- Change bed linens and clothing frequently
- Use soft, loose-fitting cotton clothing
Nutrition and Hydration
- Encourage fluid intake to prevent dehydration
- Offer cold, soft foods for children with oral lesions
- Maintain accurate intake and output records
- Monitor hydration status (mucous membranes, skin turgor, urine output)
- Consider IV fluid therapy if oral intake is inadequate
Comfort Measures
- Position for comfort
- Provide diversional activities appropriate for isolation
- Maintain comfortable room temperature
- Implement pain management strategies for headache or general discomfort
- Apply cool compresses to areas with dense lesions
Monitoring and Assessment
- Monitor vital signs every 4 hours or as indicated
- Assess skin lesions daily for progression and signs of infection
- Evaluate neurological status for signs of complications
- Monitor respiratory status, especially in high-risk patients
- Document new lesion crops and healing progression
Mnemonic: “SPOTS” – Hospital Nursing Care for Chickenpox
- Skin care and symptom management
- Protection from secondary infections
- Observation for complications
- Thermal regulation (fever management)
- Strict isolation precautions
Nursing Management at Home
Most children with chickenpox are managed at home. Nursing care involves educating parents and caregivers about appropriate home care measures to relieve symptoms, prevent complications, and limit disease spread.
Home Care Instructions for Parents/Caregivers
Managing Fever and Discomfort
- Give acetaminophen (paracetamol) as directed for fever and discomfort
- NEVER give aspirin to children with chickenpox – risk of Reye’s syndrome
- Avoid ibuprofen – some research suggests possible increased risk of secondary infections
- Dress child in lightweight clothing and maintain comfortable room temperature
- Sponge with lukewarm water if fever is high (avoid cold water or alcohol)
Relieving Itching
- Apply calamine lotion to itchy areas (avoid eyes and mucous membranes)
- Give oral antihistamines as prescribed (diphenhydramine or non-sedating alternatives)
- Provide cool baths with colloidal oatmeal or baking soda (1 cup per tub)
- Keep fingernails short and clean
- For young children, use cotton gloves or mittens to prevent scratching, especially at night
- Use loose-fitting, soft cotton clothing to minimize skin irritation
Nutrition and Hydration
- Encourage fluids to prevent dehydration – water, juice, popsicles, gelatin
- Offer soft, cold foods if mouth sores are present (yogurt, applesauce, smoothies)
- Avoid salty, acidic, or spicy foods that may irritate mouth lesions
- Monitor urine output – should be light-colored and regular
- Watch for signs of dehydration: dry mouth, decreased urine output, tearless crying
Preventing Transmission
- Keep child at home until all lesions have crusted (usually 5-7 days after rash onset)
- Avoid contact with high-risk individuals (pregnant women, newborns, immunocompromised people)
- Cover mouth and nose when coughing or sneezing
- Do not share towels, washcloths, or other personal items
- Wash hands frequently, especially after touching lesions
- Launder clothing and bedding separately in hot water with detergent
When to Seek Medical Attention
Instruct parents to seek immediate medical care if the child develops any of the following:
- High fever (>39.5°C or 103°F) or fever lasting more than 4 days
- Difficulty breathing or persistent cough
- Severe headache, stiff neck, or sensitivity to bright light
- Unusual drowsiness, confusion, or difficulty waking
- Severe abdominal pain or persistent vomiting
- Signs of skin infection: increased redness, warmth, tenderness, swelling, or pus
- Difficulty walking or unsteady movements
- Rapid spread of rash or unusual bleeding into the skin
- Signs of dehydration: dry mouth, decreased urination, tearless crying
Follow-up Care
- Schedule follow-up appointment if needed, particularly for high-risk children
- Discuss return to school guidelines (all lesions crusted, typically 5-7 days after rash onset)
- Review importance of completing full course of any prescribed medications
- Document chickenpox infection in child’s health record
- Discuss potential for future shingles infection and recognition
- Address any concerns about missed vaccinations (timing of catch-up doses)
Prevention and Control
Prevention of chickenpox focuses on vaccination and measures to prevent transmission. Nurses play a crucial role in educating families and implementing preventive strategies.
Varicella Vaccination
| Aspect | Details |
|---|---|
| Vaccine Type | Live attenuated virus vaccine |
| Recommended Schedule |
|
| Effectiveness |
|
| Contraindications |
|
| Potential Side Effects |
|
| Catch-up Vaccination |
For children, adolescents, and adults who have not had chickenpox:
|
Post-Exposure Prophylaxis
For Susceptible High-Risk Contacts:
- Varicella-Zoster Immune Globulin (VZIG)
- Recommended for susceptible high-risk individuals exposed to chickenpox
- Must be administered within 96 hours of exposure (ideally within 72 hours)
- Provides passive immunity for approximately 3 weeks
- May prevent or modify disease severity
- Candidate groups for VZIG:
- Immunocompromised children without evidence of immunity
- Newborns whose mothers developed chickenpox 5 days before to 2 days after delivery
- Hospitalized premature infants (≥28 weeks gestation) whose mothers lack evidence of immunity
- Hospitalized premature infants (<28 weeks gestation or ≤1,000g birth weight), regardless of maternal immunity status
For Healthy Susceptible Contacts:
- Varicella vaccine
- May prevent or modify disease if administered within 3-5 days of exposure
- Recommended for susceptible individuals ≥12 months of age without contraindications
Infection Control Measures
In Healthcare Settings
- Implement airborne and contact precautions for confirmed or suspected cases
- Place patients in negative pressure rooms when available
- Healthcare workers should have documented immunity to chickenpox
- Use appropriate PPE: N95 respirator, gown, gloves, and eye protection
- Restrict susceptible staff from caring for patients with chickenpox
- Notify infection control department of all suspected cases
In Community Settings
- Exclude children with chickenpox from school or daycare until all lesions have crusted
- Notify school or daycare when chickenpox is diagnosed
- Identify and inform contacts who may be at high risk
- Postpone visits to households with chickenpox cases by susceptible high-risk individuals
- Promote hand hygiene and respiratory etiquette
- Disinfect frequently touched surfaces
Nursing Role in Prevention
- Education: Provide accurate information about chickenpox and the importance of vaccination
- Advocacy: Promote adherence to recommended immunization schedules
- Assessment: Identify high-risk individuals who may need special protective measures
- Implementation: Administer vaccines according to guidelines and document appropriately
- Surveillance: Monitor for cases and assist in outbreak management
- Documentation: Maintain accurate immunization records and report adverse events
Patient Education
Education is a critical component of nursing care for children with chickenpox. Clear, accurate information helps parents and caregivers provide appropriate home care and recognize when to seek medical attention.
Key Educational Points for Parents and Caregivers
Understanding Chickenpox
- Explain what causes chickenpox and how it spreads
- Describe the typical course of illness (incubation period, prodrome, rash)
- Explain that one infection usually provides lifelong immunity
- Discuss potential for virus to reactivate later as shingles
- Address common misconceptions about chickenpox
Home Care Strategies
- Demonstrate proper application of topical treatments
- Provide written instructions for medication administration
- Teach proper hand hygiene techniques
- Discuss comfort measures (cool baths, loose clothing)
- Explain strategies to prevent scratching
Prevention of Complications
- Emphasize importance of avoiding aspirin
- Teach signs of secondary bacterial infection
- Explain when to contact healthcare provider
- Discuss warning signs of serious complications
- Provide guidance on proper skin care to prevent scarring
Preventing Transmission
- Explain isolation period requirements
- Identify high-risk contacts who should avoid the child
- Discuss school/daycare exclusion policies
- Teach proper handling of contaminated items
- Explain importance of reporting the case to school/daycare
Educational Resources for Families
- Printed materials: Simple, illustrated handouts about chickenpox care
- Digital resources: Recommended websites with accurate information about childhood illnesses
- Follow-up contact: Phone number to call with questions or concerns
- Community resources: Information about local support services if needed
- Medication guides: Clear instructions for administering any prescribed medications
- Return-to-school guidelines: Written documentation of when the child can return to school
Mnemonic: “TEACH” – Education Strategy for Chickenpox
- Treatment options and home care instructions
- Emergency signs requiring medical attention
- Avoid complications with proper management
- Contain the infection through isolation measures
- Hydration and comfort measures to support recovery
Summary
Chickenpox is a common childhood infectious disease caused by the varicella-zoster virus. While typically self-limiting in healthy children, it requires comprehensive nursing care to manage symptoms, prevent complications, and limit transmission.
Key nursing responsibilities include:
- Assessment: Recognizing classic chickenpox presentation and monitoring for complications
- Intervention: Implementing appropriate isolation measures, administering medications, providing skin care, and maintaining comfort
- Education: Teaching families about home care, infection control, and when to seek medical attention
- Prevention: Promoting vaccination and implementing post-exposure prophylaxis when indicated
By understanding the pathophysiology, clinical manifestations, and management principles of chickenpox, nurses can provide high-quality care to affected children and support families through this common childhood illness.
