Comprehensive Foot Care for Nursing Students
Osmosis-Style Medical Notes
Introduction
Foot care is a critical component of nursing practice that requires comprehensive knowledge of anatomy, assessment techniques, and preventive strategies. The feet bear the entire body weight and are susceptible to various complications, particularly in vulnerable populations such as diabetic patients, elderly individuals, and those with peripheral vascular disease.
This comprehensive guide provides essential knowledge for nursing students to develop competency in foot assessment, wound care, prevention strategies, and patient education. Understanding proper foot care can prevent serious complications including infections, ulcerations, and potential amputations.
Structural Components
Bones (26 total)
- Hindfoot: Talus, Calcaneus
- Midfoot: Navicular, Cuboid, 3 Cuneiforms
- Forefoot: 5 Metatarsals, 14 Phalanges
Soft Tissues
- Muscles: 13 extrinsic, 21 intrinsic
- Ligaments: 112 supporting structures
- Tendons: Connect muscles to bones
- Fascia: Plantar and deep compartments
Memory Aid: “FOOT BONES”
For remembering foot bone groups:
- Forefoot – metatarsals and phalanges
- Outside bones – lateral structures
- Organized in arches – longitudinal and transverse
- Talus and calcaneus – hindfoot
- Bridge bones – midfoot navigation
- Operative structures – joints and ligaments
- Navicular, cuboid, cuneiforms – midfoot
- Essential arches – support body weight
- Support system – muscles and tendons
Vascular and Neurological Supply
Arterial Supply
- Posterior tibial artery: Medial plantar, lateral plantar
- Anterior tibial artery: Dorsalis pedis
- Peroneal artery: Lateral foot supply
- Plantar arch: Deep and superficial
Nerve Supply
- Tibial nerve: Plantar sensation
- Deep peroneal nerve: Dorsal foot
- Superficial peroneal nerve: Lateral dorsum
- Sural nerve: Lateral foot sensation
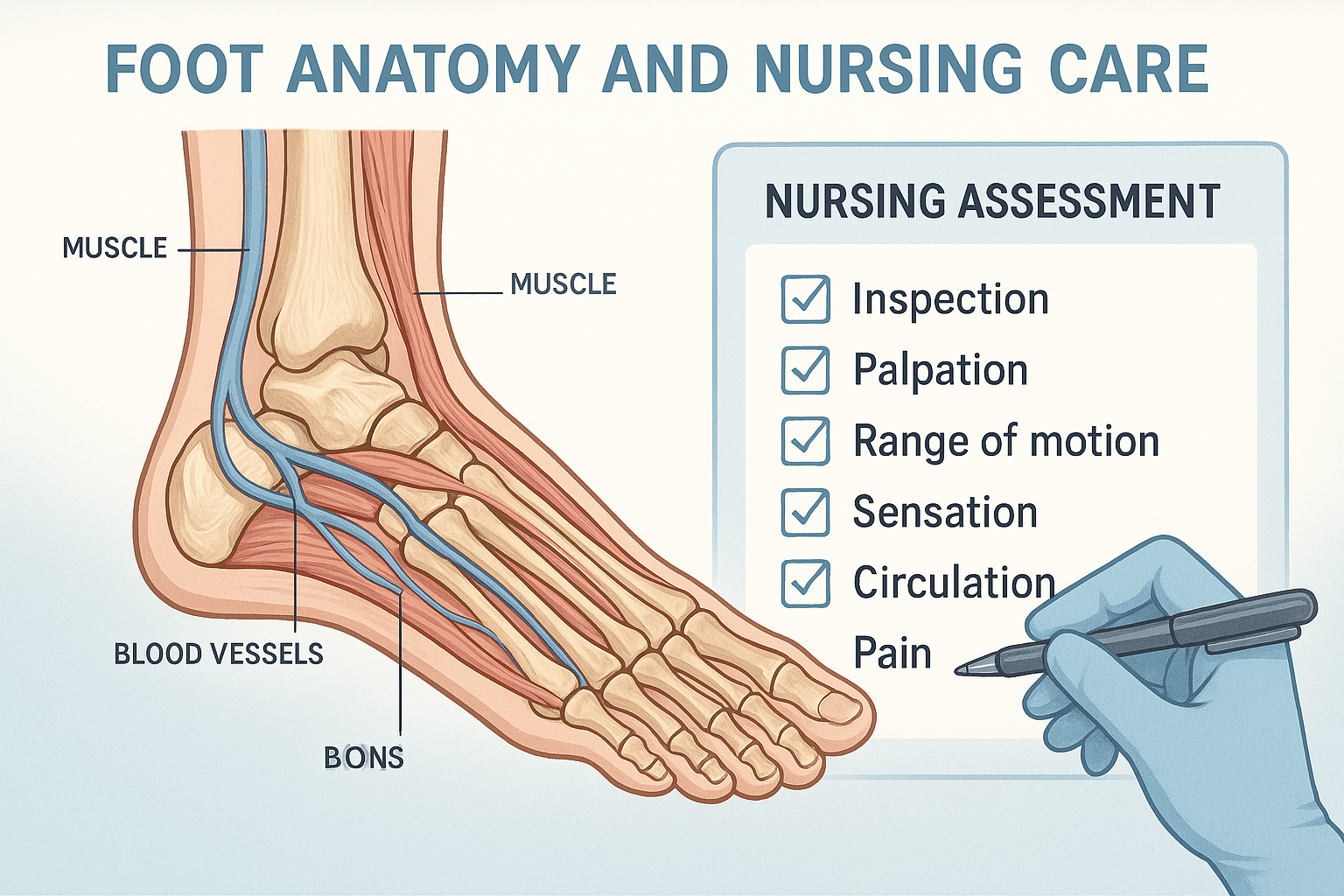
Systematic Assessment Approach
Follow the structured “INSPECT” method for thorough foot evaluation:
“INSPECT” Assessment Mnemonic
- Inspection – Visual examination of skin, nails, deformities
- Neurological – Sensation, reflexes, motor function
- Structure – Alignment, arches, deformities
- Palpation – Pulses, temperature, edema
- Evaluation – Range of motion, strength
- Circulation – Capillary refill, color changes
- Temperature – Bilateral comparison, warmth
Foot Assessment Flowchart
Position patient comfortably, ensure good lighting, wash hands
Examine skin color, lesions, deformities, nail condition
Check pulses, temperature, edema, pain response
Assess sensation, reflexes, motor function
Evaluate range of motion, strength, gait
Record findings, identify risk factors, plan interventions
Detailed Assessment Components
| Assessment Area | Normal Findings | Abnormal Findings |
|---|---|---|
| Skin Color | Pink, uniform tone | Cyanosis, pallor, rubor, mottling |
| Skin Temperature | Warm, bilateral equality | Cold, hot, asymmetrical |
| Skin Integrity | Intact, no lesions | Ulcers, fissures, calluses, corns |
| Nail Condition | Pink, smooth, proper length | Fungal infection, ingrown, thickened |
| Pulses | Palpable dorsalis pedis, posterior tibial | Weak, absent, irregular |
| Sensation | Intact to light touch, vibration | Diminished, absent, hyperesthesia |
Clinical Pearl: Neurological Assessment Tools
- Monofilament testing: Use 10g monofilament to test protective sensation
- Vibration testing: 128 Hz tuning fork on bony prominences
- Pinprick testing: Sharp/dull discrimination
- Position sense: Test joint position awareness
- Ankle reflexes: Achilles tendon reflex assessment
Pathophysiology of Diabetic Foot Complications
Diabetes mellitus leads to foot complications through multiple pathways that create a cascade of problems. Understanding these mechanisms is crucial for prevention and early intervention.
Neuropathy
- Sensory loss
- Motor dysfunction
- Autonomic neuropathy
- Foot deformities
Vascular Disease
- Peripheral arterial disease
- Microvascular dysfunction
- Impaired wound healing
- Tissue hypoxia
Immunocompromise
- Reduced immune response
- Increased infection risk
- Delayed healing
- Hyperglycemia effects
“DIABETIC FOOT” Risk Factors Mnemonic
- Duration of diabetes (>10 years)
- Infection history
- Age (elderly patients)
- Blood glucose control (poor)
- Ethnic background (certain populations)
- Tobacco use
- Ischemia/vascular disease
- Calluses and corns
- Foot deformities
- Obesity
- Orthopedic problems
- Trauma history
Diabetic Foot Assessment Protocol
Low, moderate, high risk classification
Pulse examination, ankle-brachial index
Monofilament, vibration, reflexes
Deformities, pressure points, gait
Integrity, lesions, nail condition
Patient teaching, follow-up planning
Wound Healing Phases
Understanding the normal wound healing process is essential for proper wound care management and recognizing when healing is delayed or impaired.
Phase 1: Hemostasis (0-30 minutes)
- Vasoconstriction
- Platelet aggregation
- Fibrin clot formation
- Bleeding cessation
Phase 2: Inflammatory (1-4 days)
- Vasodilation
- Neutrophil migration
- Macrophage activation
- Debris removal
Phase 3: Proliferative (4-21 days)
- Granulation tissue formation
- Angiogenesis
- Collagen synthesis
- Epithelialization
Phase 4: Remodeling (21 days-2 years)
- Collagen reorganization
- Scar maturation
- Tensile strength increase
- Functional restoration
“HEAL” Wound Care Principles
- Hydration – Maintain moist wound environment
- Evaluation – Regular assessment and monitoring
- Asepsis – Prevent contamination and infection
- Loading – Appropriate offloading and pressure relief
Comprehensive Wound Assessment
| Assessment Parameter | Components | Documentation |
|---|---|---|
| Location | Anatomical position, bilateral | Specific foot region, digit number |
| Size | Length, width, depth | Centimeters, volume if applicable |
| Wound Bed | Tissue type, color, necrosis | Percentage of each tissue type |
| Exudate | Amount, consistency, color, odor | Scant/moderate/heavy, characteristics |
| Edges | Adherence, epithelialization | Attached/unattached, rolled/flat |
| Periwound | Skin condition, inflammation | Intact/macerated, erythema presence |
Clinical Pearl: Wagner Classification System
- Grade 0: Skin intact, no ulceration
- Grade 1: Superficial ulcer, no infection
- Grade 2: Deep ulcer to tendon, bone, or joint
- Grade 3: Deep ulcer with abscess or osteomyelitis
- Grade 4: Localized gangrene
- Grade 5: Extensive gangrene of foot
Warning Signs of Infection
Use the “INFECT” mnemonic to remember infection signs:
- Increased pain or tenderness
- New or worsening drainage
- Fever or systemic symptoms
- Erythema or red streaking
- Cellulitis or spreading inflammation
- Temperature increase (local warmth)
Infection Management Protocol
Assessment
- Culture and sensitivity testing
- Blood work (WBC, ESR, CRP)
- Imaging if osteomyelitis suspected
- Vascular assessment
Treatment
- Appropriate antibiotic therapy
- Surgical debridement if needed
- Offloading and pressure relief
- Glycemic control optimization
“PREVENT” Foot Care Strategy
- Proper footwear selection and fitting
- Regular inspection and self-examination
- Education about foot care and hygiene
- Vascular assessment and management
- Early intervention for problems
- Nail care and professional podiatry
- Temperature protection and moisture control
Patient Education Components
Daily Inspection
- Use mirror for bottom of feet
- Check between toes
- Look for cuts, blisters, swelling
- Note color changes
Hygiene Practices
- Wash daily with lukewarm water
- Dry thoroughly, especially between toes
- Use unscented moisturizer
- Avoid soaking feet
Footwear Guidelines
- Proper fit and support
- Breathable materials
- Avoid walking barefoot
- Regular shoe inspection
Nursing Care Plans
Risk for Impaired Skin Integrity
Goal: Patient will maintain intact skin integrity
- • Assess feet daily for changes
- • Provide education on proper foot care
- • Ensure appropriate footwear
- • Maintain optimal blood glucose levels
Risk for Infection
Goal: Patient will remain free from infection
- • Use aseptic technique for wound care
- • Monitor for signs of infection
- • Educate about hygiene practices
- • Administer antibiotics as prescribed
Deficient Knowledge
Goal: Patient will demonstrate understanding of foot care
- • Assess current knowledge level
- • Provide written and verbal instructions
- • Demonstrate proper techniques
- • Evaluate understanding through return demonstration
Sterile Wound Care Procedure
- 1. Gather supplies and perform hand hygiene
- 2. Position patient comfortably
- 3. Remove old dressing using clean technique
- 4. Assess wound and surrounding tissue
- 5. Clean wound with sterile saline
- 6. Apply appropriate dressing
- 7. Secure dressing and label with date
- 8. Document findings and interventions
Emergency Situations Requiring Immediate Attention
- Acute limb ischemia: Sudden onset of severe pain, pallor, pulselessness
- Necrotizing fasciitis: Rapidly spreading infection with systemic toxicity
- Diabetic foot emergency: Deep infection with systemic signs
- Arterial embolism: Sudden loss of pulse with cold, pale extremity
- Compartment syndrome: Severe pain, swelling, loss of function
Essential Documentation Elements
Assessment Documentation
- Complete physical findings
- Wound characteristics and measurements
- Neurological and vascular status
- Patient symptoms and pain level
- Risk factors and complications
Intervention Documentation
- Wound care procedures performed
- Medications administered
- Patient education provided
- Referrals made
- Patient response to interventions
“SBAR” Communication Framework
- Situation – Current patient condition and concerns
- Background – Relevant medical history and context
- Assessment – Current findings and clinical judgment
- Recommendation – Proposed interventions and follow-up
Key Performance Indicators
| Outcome Measure | Target | Monitoring Method |
|---|---|---|
| Ulcer healing rate | >80% within 12 weeks | Weekly wound measurements |
| Infection prevention | <5% infection rate | Culture results tracking |
| Patient satisfaction | >90% satisfied with care | Patient surveys |
| Readmission rate | <15% within 30 days | Electronic health records |
| Amputation prevention | <2% amputation rate | Surgical outcome tracking |
Evidence-Based Practice Highlights
- Offloading: Total contact casting reduces healing time by 50%
- Moist wound healing: Improves healing rates compared to dry dressings
- Debridement: Regular sharp debridement accelerates healing
- Infection control: Topical antimicrobials reduce biofilm formation
- Patient education: Structured programs reduce ulcer recurrence by 60%
Emerging Technologies
Technological Advances
- Artificial intelligence for wound assessment
- Telemedicine for remote monitoring
- 3D printed orthotics and prosthetics
- Smart sensors for pressure monitoring
- Bioengineered tissue substitutes
Novel Therapies
- Stem cell therapy for wound healing
- Growth factor applications
- Hyperbaric oxygen therapy
- Electrical stimulation devices
- Antimicrobial peptides
Key Takeaways for Nursing Practice
- Prevention is paramount: Early identification and intervention prevent complications
- Systematic assessment: Use standardized tools and protocols for consistency
- Patient education: Empower patients with knowledge and skills for self-care
- Multidisciplinary approach: Collaborate with podiatrists, wound specialists, and physicians
- Evidence-based practice: Stay current with research and best practices
- Documentation: Maintain comprehensive records for continuity of care
Conclusion
Foot care represents a critical component of nursing practice that requires comprehensive knowledge, skilled assessment, and evidence-based interventions. The feet, as the foundation of mobility and independence, deserve careful attention and proactive management to prevent complications and maintain quality of life.
Through systematic assessment using the INSPECT method, understanding of wound healing phases, application of the HEAL principles, and implementation of PREVENT strategies, nurses can significantly impact patient outcomes. The integration of evidence-based practice, effective communication using SBAR, and continuous quality improvement ensures the highest standard of care.
As healthcare continues to evolve with technological advances and novel therapies, nurses must remain adaptable and committed to lifelong learning. The principles outlined in these notes provide a solid foundation for developing expertise in foot care and contributing to improved patient outcomes across diverse healthcare settings.
References and Further Reading
1. American Diabetes Association. (2023). Standards of Medical Care in Diabetes—2023. Diabetes Care, 46(Supplement_1), S1-S291.
2. International Working Group on the Diabetic Foot. (2023). IWGDF Guidelines on the Prevention and Management of Diabetic Foot Disease.
3. Wound, Ostomy and Continence Nurses Society. (2023). Guideline for Management of Wounds in Patients with Lower-Extremity Arterial Disease.
4. National Institute for Health and Care Excellence. (2023). Diabetic foot problems: prevention and management. NICE guideline [NG19].
5. Registered Nurses’ Association of Ontario. (2023). Assessment and Management of Foot Ulcers for People with Diabetes.
© 2025 Nursing Education Resources | Comprehensive Foot Care Notes
Developed for nursing students followingeducational principles
