Constipation Management
A Community Health Nursing Approach
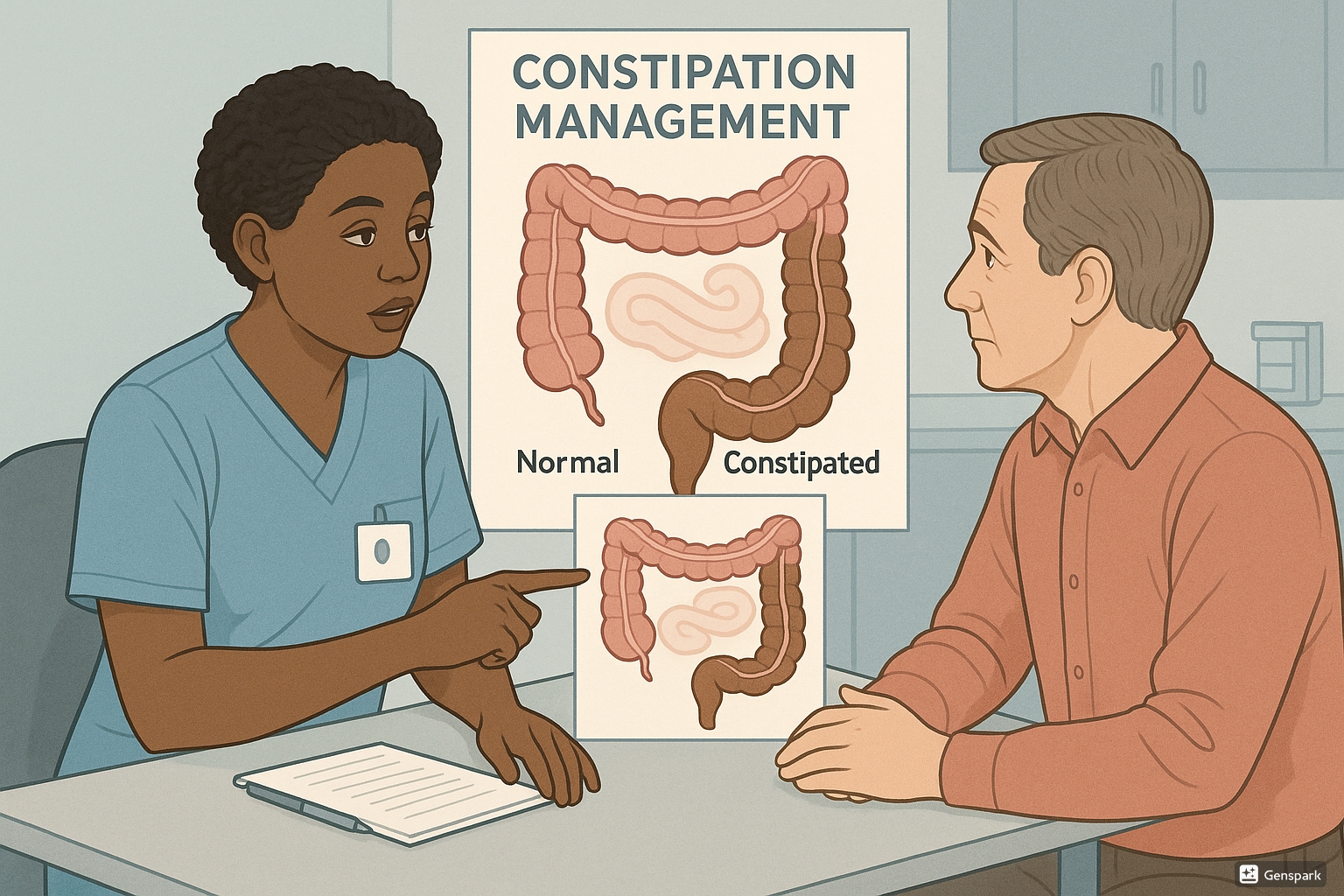
Table of Contents
Introduction to Constipation
Constipation is a common gastrointestinal condition that significantly impacts patients’ quality of life. As community health nurses, understanding constipation management is essential for providing comprehensive care to individuals across all age groups and settings. This prevalent digestive issue affects approximately 16% of adults worldwide and about 33% of adults over 60 years old, making it one of the most common digestive complaints encountered in community health practice.
This guide provides community health nurses with evidence-based approaches to constipation management, including screening, diagnosis, standing orders, primary care interventions, and appropriate referral criteria. By implementing these constipation management strategies, community health nurses can significantly improve patient outcomes and quality of life.
Definition and Prevalence
Clinical Definition of Constipation
Constipation is defined as infrequent bowel movements (typically fewer than three per week) accompanied by difficult passage of stools that are often hard, dry, small in size, and difficult to eliminate. Constipation management requires a comprehensive assessment of both subjective symptoms and objective findings.
Rome IV Diagnostic Criteria
The Rome IV criteria define functional constipation as the presence of at least two of the following symptoms for at least 3 months, with symptom onset at least 6 months prior to diagnosis:
- Straining during at least 25% of defecations
- Lumpy or hard stools in at least 25% of defecations
- Sensation of incomplete evacuation in at least 25% of defecations
- Sensation of anorectal obstruction/blockage in at least 25% of defecations
- Manual maneuvers to facilitate at least 25% of defecations
- Fewer than three spontaneous bowel movements per week
Prevalence and Impact
Constipation affects people of all ages but is particularly common in:
- Older adults (33% of adults over age 60)
- Women (2-3 times more common than in men)
- Pregnant women (approximately 40% experience constipation)
- Children (prevalence of 1-30% depending on criteria used)
- Individuals with limited mobility or neurological conditions
Effective constipation management is critical as chronic constipation significantly impacts quality of life, causing physical discomfort, anxiety, and social limitations. It also creates substantial healthcare costs due to medical visits, medications, and potential complications.
Screening and Assessment
Community health nurses play a pivotal role in screening for constipation. A systematic approach to constipation management screening helps identify at-risk individuals and those requiring intervention.
Screening Tools
| Screening Tool | Description | Application in Community Setting |
|---|---|---|
| Bristol Stool Form Scale | Visual chart categorizing stool into 7 types based on form and consistency | Quick visual assessment; Types 1-2 indicate constipation |
| Constipation Assessment Scale (CAS) | 8-item questionnaire measuring presence and severity of constipation | Comprehensive assessment for routine clinic visits |
| Patient Assessment of Constipation Symptoms (PAC-SYM) | 12-item self-report measuring severity of constipation symptoms | Useful for monitoring symptom changes over time |
| Bowel Function Diary | Daily record of bowel movements, consistency, associated symptoms | Patient self-monitoring; valuable for home care settings |
Key Assessment Components
History Taking
- Bowel movement frequency and consistency
- Duration of constipation symptoms
- Dietary habits, especially fiber and fluid intake
- Physical activity levels
- Current medications (many are constipating)
- Straining and painful defecation
- Previous constipation management approaches
Physical Assessment
- Abdominal examination (distention, tenderness)
- Bowel sounds assessment
- Rectal examination (if appropriate)
- Assessment of mobility and functional status
- Hydration status evaluation
- Signs of complications (e.g., hemorrhoids)
CONSTIPATED Mnemonic for Assessment
Use this mnemonic during constipation management assessment:
- C – Consistency and character of stool
- O – Onset and duration of symptoms
- N – Number of bowel movements per week
- S – Straining and difficulty passing stool
- T – Treatment history and attempts at relief
- I – Intestinal habits and diet patterns
- P – Pain or discomfort with defecation
- A – Associated symptoms (bloating, cramping)
- T – Toilet facilities and accessibility
- E – Exercise and mobility status
- D – Drugs and medications (current and past)
Diagnosis/Identification
Proper diagnosis is essential for effective constipation management. Community health nurses should be able to identify the type of constipation and potential underlying causes to guide treatment decisions.
Types of Constipation
| Type | Description | Clinical Features | Nursing Implications |
|---|---|---|---|
| Primary/Functional Constipation | No underlying medical cause; related to lifestyle factors | Meets Rome IV criteria; normal physiological function | Focus on lifestyle modifications and education |
| Secondary Constipation | Due to medications, medical conditions, or structural issues | Symptoms associated with specific cause; may have other symptoms | Address underlying cause; referral may be needed |
| Slow Transit Constipation | Delayed movement of stool through the colon | Infrequent urge to defecate; abdominal bloating | May require specialized testing; pharmacological interventions |
| Outlet Dysfunction | Difficulty with expulsion of stool from rectum | Feeling of rectal blockage; excessive straining | Pelvic floor assessment; possible biofeedback referral |
Common Causes of Constipation
Lifestyle Factors
- Low-fiber diet
- Inadequate fluid intake
- Physical inactivity
- Ignoring urge to defecate
- Stress and anxiety
- Changes in routine or travel
Medications
- Opioid analgesics
- Anticholinergics
- Calcium channel blockers
- Iron supplements
- Antacids containing aluminum or calcium
- Anticonvulsants
- Antidepressants
Medical Conditions
- Irritable bowel syndrome
- Hypothyroidism
- Diabetes mellitus
- Parkinson’s disease
- Multiple sclerosis
- Spinal cord injuries
- Depression
- Cognitive impairment
Structural Causes
- Colorectal cancer
- Anal fissures
- Rectocele
- Strictures
- Pelvic floor dysfunction
- Hirschsprung’s disease
Red Flags Requiring Immediate Referral
These warning signs may indicate serious underlying conditions requiring prompt medical attention:
- New onset constipation in older adults
- Unexplained weight loss
- Rectal bleeding
- Family history of colorectal cancer or inflammatory bowel disease
- Severe, persistent abdominal pain
- Iron deficiency anemia
- Alternating constipation and diarrhea
- Failure to respond to constipation management interventions
Standing Orders
Definition of Standing Orders
Standing orders are written protocols that authorize nurses and other healthcare providers to deliver specific health services without a physician’s direct examination when certain predetermined conditions are met. For constipation management, standing orders provide community health nurses with a standardized approach to assessment, intervention, and referral.
Uses of Standing Orders in Constipation Management
- Standardize evidence-based care across community health settings
- Expedite assessment and treatment without requiring physician consultation for routine cases
- Clarify criteria for escalation and referral to higher levels of care
- Empower community health nurses to implement appropriate interventions
- Improve efficiency and timeliness of constipation management
- Ensure consistent documentation and follow-up protocols
Sample Standing Order Protocol for Constipation Management
| Component | Protocol |
|---|---|
| Assessment |
|
| Diagnostic Testing |
|
| Interventions |
|
| Documentation |
|
| Referral Criteria |
|
| Follow-up |
|
Implementation Tips for Standing Orders
- Ensure all community health nurses are trained in the standing order protocol
- Review and update standing orders regularly based on emerging evidence
- Maintain clear documentation of standing order implementation
- Establish quality improvement mechanisms to monitor outcomes
- Develop a system for regular communication with supervising physicians
Primary Care Interventions
Community health nurses play a critical role in implementing primary care interventions for constipation management. These interventions include non-pharmacological approaches, pharmacological management, and patient education.
Non-pharmacological Interventions
Dietary Modifications
- Fiber intake: Gradually increase to 25-30g daily
- High-fiber foods: Whole grains, fruits, vegetables, legumes
- Hydration: 1.5-2L of fluid daily (unless contraindicated)
- Probiotic foods: Yogurt, kefir, fermented vegetables
- Limit constipating foods: Processed foods, cheese, white bread
Lifestyle Modifications
- Physical activity: 30 minutes of exercise most days
- Toileting routine: Scheduled time after meals
- Proper positioning: Use footstool for squatting position
- Stress reduction: Relaxation techniques, adequate sleep
- Time allocation: Allow sufficient time for defecation
Pharmacological Management
When non-pharmacological approaches are insufficient, pharmacological interventions may be necessary. Community health nurses should understand the various laxative options for constipation management:
| Laxative Type | Examples | Mechanism | Nursing Considerations |
|---|---|---|---|
| Bulk-Forming | Psyllium (Metamucil), Methylcellulose (Citrucel) | Absorb water to increase stool bulk and stimulate peristalsis |
|
| Osmotic | Polyethylene glycol (Miralax), Magnesium hydroxide (Milk of Magnesia) | Draw water into intestines to soften stool |
|
| Stimulant | Bisacodyl (Dulcolax), Senna (Senokot) | Stimulate intestinal motility; increase water secretion |
|
| Stool Softeners | Docusate sodium (Colace) | Increase water penetration into stool |
|
| Lubricants | Mineral oil | Coat stool and intestinal mucosa to ease passage |
|
| Enemas/Suppositories | Glycerin suppositories, Sodium phosphate enemas | Local stimulation and softening of stool |
|
Patient Education for Constipation Management
Key Educational Points
Community health nurses should provide comprehensive education on:
- Normal bowel function: Variations in normal patterns and consistency
- Warning signs: When to seek medical attention
- Dietary fiber: Sources, gradual increase, and fluid requirements
- Medication effects: Identifying constipating medications
- Exercise benefits: How physical activity promotes bowel function
- Toileting habits: Responding to urges and proper positioning
- Proper use of laxatives: Indications, administration, potential side effects
- Self-monitoring: Using bowel diaries and the Bristol Stool Scale
FIBER Mnemonic for Patient Education
Use this mnemonic to structure patient education for constipation management:
- F – Fluids (adequate daily intake)
- I – Increase fiber gradually
- B – Bowel routine establishment
- E – Exercise regularly
- R – Respond promptly to urges
First Aid Management
First aid management for constipation focuses on providing immediate relief for acute constipation while assessing for complications. Community health nurses should be prepared to offer these interventions as part of comprehensive constipation management.
Immediate Relief Measures
- Assessment: Confirm constipation and rule out complications requiring emergency care
- Hydration: Encourage drinking 2-3 glasses of warm water
- Movement: Gentle walking or light exercise to stimulate peristalsis
- Abdominal massage: Gentle clockwise massage following the colon’s path
- Warm bath: To relax abdominal muscles and reduce discomfort
- Over-the-counter relief: Based on severity and standing orders
Urgent Situations
When to Seek Emergency Care
Advise patients to seek immediate medical attention if constipation is accompanied by:
- Severe, unrelenting abdominal pain
- Vomiting with abdominal distension
- Inability to pass gas
- High fever with constipation
- Rectal bleeding with severe pain
- Signs of impaction with mental status changes
- Significant abdominal distention
First Aid Interventions by Severity
| Severity | Presentation | First Aid Interventions |
|---|---|---|
| Mild |
|
|
| Moderate |
|
|
| Severe |
|
|
| Fecal Impaction |
|
|
First Aid Kit for Constipation Management
Community health nurses should recommend a home first aid kit for constipation that includes:
Basic Supplies
- Bulk-forming laxative
- Stool softener
- Glycerin suppositories
- Measuring cup for fluid intake
- Bristol Stool Chart
Comfort Items
- Heating pad for abdominal comfort
- Toilet footstool
- Soothing tea (e.g., peppermint)
- Comfortable clothing
Documentation Tools
- Bowel movement diary
- Medication log
- Symptom tracker
- Contact information for healthcare provider
Referral Protocols
Community health nurses must know when and how to refer patients for additional care as part of effective constipation management. Timely referrals can prevent complications and ensure appropriate treatment.
Referral Indications
| Referral Type | Indications | Timeframe | Recommended Actions |
|---|---|---|---|
| Urgent Medical Referral |
|
Same day |
|
| Primary Care Provider |
|
Within 1-2 weeks |
|
| Gastroenterologist |
|
Within 2-4 weeks |
|
| Dietitian |
|
Within 4 weeks |
|
| Pelvic Floor Therapist |
|
Within 4 weeks |
|
Referral Documentation
Proper documentation is essential for effective constipation management referrals. Include:
Essential Documentation Elements
- Duration and pattern of constipation
- Complete symptom history
- Bristol Stool Scale findings
- Red flag assessment results
- Physical assessment findings
- Interventions attempted and outcomes
- Current medications and relevant medical history
- Specific reason for referral
Sample Referral Statement
“Referring 68-year-old female with 3-month history of progressively worsening constipation (Bristol Type 1-2). Patient reports straining, incomplete evacuation, and abdominal discomfort. Has implemented dietary changes, increased fluid intake, and tried OTC Miralax without significant improvement. Recent unintentional weight loss of 5kg in 2 months. No rectal bleeding. Requesting gastroenterology evaluation for persistent symptoms and concerning weight loss. Constipation management interventions have been ineffective.”
Post-Referral Follow-Up
Community health nurses should maintain continuity of care after referral:
- Confirm patient attended referral appointment
- Document specialist recommendations
- Adjust community-based constipation management plan based on specialist input
- Provide ongoing monitoring and support
- Ensure communication between all providers involved in care
- Update standing order implementation as appropriate
Prevention Strategies
Prevention is a key component of constipation management in community health nursing. Proactive strategies can reduce the incidence and recurrence of constipation.
Primary Prevention
Strategies to prevent initial occurrence:
- Regular health education on bowel health
- Promotion of balanced diet with adequate fiber
- Hydration awareness campaigns
- Physical activity promotion
- Early identification of at-risk individuals
- Medication review for potential constipating effects
Secondary Prevention
Early detection and management:
- Routine screening in high-risk populations
- Prompt intervention for early symptoms
- Regular assessment of medication side effects
- Bowel monitoring protocols in institutional settings
- Health literacy assessment and education
Tertiary Prevention
Preventing complications and recurrence:
- Comprehensive management plans for chronic cases
- Regular reassessment of chronic constipation
- Monitoring for complications
- Adjustment of interventions based on effectiveness
- Support groups for chronic constipation
Population-Based Prevention Strategies
Prevention in Children
- Age-appropriate fiber intake education for parents
- Toilet training techniques that don’t promote stool withholding
- Regular toileting schedule, especially after meals
- Education on recognizing early signs of constipation
- Promotion of physical activity and play
- Limiting constipating foods (excessive dairy, processed foods)
- School-based education on bathroom access and privacy
Prevention in Adults
- Workplace health promotion focusing on hydration and activity
- Stress management techniques for gut-brain axis health
- Education on dietary fiber sources and gradually increasing intake
- Medication review during routine healthcare visits
- Exercise prescriptions as part of routine healthcare
- Travel constipation prevention strategies
- Addressing cultural barriers to discussing bowel habits
Prevention in Elderly
- Medication regimen review and adjustment
- Mobility preservation strategies
- Modified fiber recommendations based on individual needs
- Dehydration prevention protocols
- Bathroom accessibility assessment
- Regular toileting schedule implementation
- Nutritional assessment and intervention
- Caregiver education on constipation recognition
Prevention in Institutional Settings
- Standardized bowel monitoring protocols
- Staff education on constipation prevention
- Environmental modifications for proper toileting
- Regular medication reviews by clinical pharmacists
- Menu planning for adequate fiber and hydration
- Scheduled physical activity programs
- Quality improvement initiatives targeting constipation rates
- Privacy provisions for toileting
PREVENT Mnemonic for Constipation Prevention
Community health nurses can use this mnemonic for constipation management prevention:
- P – Physical activity daily
- R – Regular toileting schedule
- E – Eat fiber-rich foods
- V – Volume of fluids (adequate hydration)
- E – Education about bowel health
- N – Note medication effects
- T – Timely response to bowel urges
Special Populations
Effective constipation management requires tailored approaches for special populations with unique considerations.
| Population | Special Considerations | Nursing Interventions |
|---|---|---|
| Pregnant Women |
|
|
| Children |
|
|
| Older Adults |
|
|
| Bedridden Patients |
|
|
| Neurological Conditions |
|
|
| Palliative Care |
|
|
Cultural Considerations in Constipation Management
Community health nurses should incorporate cultural sensitivity into constipation management:
- Respect cultural beliefs around bowel habits and privacy
- Adapt dietary recommendations to culturally appropriate foods
- Consider cultural attitudes toward medication use
- Acknowledge traditional remedies that may be effective
- Use culturally appropriate language when discussing bowel function
- Address potential language barriers in educational materials
- Consider gender-specific concerns about discussing bowel habits
Global Best Practices in Constipation Management
Different regions have developed effective approaches to constipation management in community settings. These global practices can inform and enhance nursing care.
Nordic Countries
Approach focuses on lifestyle and prevention:
- Integration of physical activity into daily routines
- High-fiber traditional diets promotion
- National dietary guidelines emphasizing whole grains
- Public health campaigns for digestive health
- School-based education on digestive health
- Community health nurses leading preventive programs
Japan
Combines traditional and modern approaches:
- Promotion of traditional high-fiber Japanese diet
- Integration of fermented foods (probiotics)
- Public toilet accessibility and design excellence
- Kampo medicine (traditional herbal medicine) integration
- Abdominal massage techniques (Ampuku)
- Technologically advanced toilet systems supporting assessment
Australia
Emphasizes nurse-led community interventions:
- Advanced practice nursing roles in gastroenterology
- Nurse-led constipation clinics in community settings
- Telehealth services for rural and remote areas
- Standardized protocols across healthcare settings
- Aboriginal health worker involvement for cultural appropriateness
- Integration with aged care assessment teams
United Kingdom
Focuses on systematic community care pathways:
- NICE guidelines for standardized approach
- Specialist constipation nurses in community services
- Bowel care pathways across healthcare settings
- School nurse programs focusing on childhood constipation
- Integration with pharmacist consultation services
- Quality improvement initiatives measuring outcomes
“The integration of traditional wisdom with evidence-based practice creates the most effective approach to constipation management in community settings.”
Lessons for Implementation
Community health nurses can incorporate these global best practices for constipation management:
- Develop culturally appropriate educational materials based on global approaches
- Advocate for specialized constipation management roles within community health
- Implement standardized protocols adapted from successful global models
- Explore integration of traditional approaches with evidence-based practices
- Develop community partnerships to address environmental and social factors
- Advocate for improved public toilet accessibility and design
- Create multidisciplinary approaches involving dietitians, pharmacists, and physicians
- Establish quality metrics to evaluate constipation management outcomes
References
- World Gastroenterology Organisation Global Guidelines. (2018). Constipation: A global perspective.
- National Institute for Health and Care Excellence. (2021). Constipation in children and young people: Diagnosis and management. NICE Guideline NG99.
- American Gastroenterological Association. (2013). American Gastroenterological Association medical position statement on constipation. Gastroenterology, 144(1), 211-217.
- European Society for Paediatric Gastroenterology, Hepatology and Nutrition/North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. (2018). Evaluation and treatment of functional constipation in infants and children.
- Bharucha, A. E., Pemberton, J. H., & Locke, G. R. (2013). American Gastroenterological Association technical review on constipation. Gastroenterology, 144(1), 218-238.
- Camilleri, M., Ford, A. C., Mawe, G. M., et al. (2017). Chronic constipation. Nature Reviews Disease Primers, 3, 17095.
- Joanna Briggs Institute. (2020). Best practice information sheet: Management of constipation in older adults. JBI, 24(2), 1-4.
- World Health Organization. (2018). Integrated care for older people: Guidelines on community-level interventions to manage declines in intrinsic capacity.
- Registered Nurses’ Association of Ontario. (2019). Assessment and management of constipation. Clinical Best Practice Guidelines.
- International Continence Society. (2019). Management of chronic constipation in adults. ICS Educational Module.
