Epidemiology in Community Health Nursing
Concepts, Distribution, and Disease Transmission
Table of Contents
Introduction to Epidemiology
In community health nursing, epidemiology serves as the cornerstone of public health practice and preventive healthcare. As a scientific discipline, epidemiology provides nurses with essential tools to understand disease patterns, identify risk factors, and implement effective interventions at the population level.
The word “epidemiology” derives from Greek roots: “epi” (upon), “demos” (people), and “logos” (study), literally meaning “the study of what is upon the people.” This etymology reflects the discipline’s focus on health events affecting human populations rather than individuals.
Why Epidemiology Matters in Nursing: Epidemiological principles guide community health nurses in making evidence-based decisions, allocating resources efficiently, designing targeted interventions, and evaluating the effectiveness of health programs. Understanding epidemiology empowers nurses to serve as advocates for population health and contributes to addressing health disparities in communities.
Definition and Concept of Epidemiology
Epidemiology is the study of the distribution and determinants of health-related states or events in specified populations and the application of this study to control health problems.
Several key components define the core of epidemiology:
- Population focus: Examines groups rather than individuals
- Distribution: Analyzes how disease cases are distributed across populations by time, place, and person
- Determinants: Identifies factors that influence health (causal and risk factors)
- Health-related states: Studies diseases and other health conditions, behaviors, and physiological states
- Application: Uses findings to improve public health through prevention and control measures
Distinct Perspective: The epidemiological approach differs from clinical medicine by focusing on populations rather than individual patients. While clinicians treat disease in individual patients, epidemiologists study the factors that make populations susceptible to disease and develop strategies to prevent it.
MNEMONIC: “EPIDEMIC”
Examine health events in
Populations to determine
Incidence and prevalence while
Discovering patterns and
Exploring causes to
Mitigate risks and
Implement interventions for
Controlling disease spread
Distribution and Frequency of Disease
A central aspect of epidemiological practice is describing and analyzing the distribution of health and disease within populations. This involves understanding:
Measures of Disease Frequency
| Measure | Definition | Formula | Application |
|---|---|---|---|
| Incidence Rate | Frequency of new cases in a population during a specified time period | New cases / Population at risk × Time period | Useful for studying acute diseases and evaluating effectiveness of preventive measures |
| Prevalence Rate | Proportion of a population with a specific condition at a given point in time | Existing cases / Total population × 100 | Useful for planning health services and resource allocation |
| Attack Rate | Proportion of exposed population that develops disease | Number affected / Number exposed × 100 | Commonly used in outbreak investigations |
| Mortality Rate | Frequency of deaths in a defined population | Number of deaths / Total population × 1,000 or 100,000 | Assesses the lethality of a disease or overall population health |
Descriptive Epidemiology: Person, Place, Time
Person
- Age and sex
- Race and ethnicity
- Socioeconomic status
- Occupation
- Marital status
- Behaviors (diet, exercise)
Place
- Geographic location
- Urban vs. rural
- Climate conditions
- Environmental factors
- Population density
- Country, region, neighborhood
Time
- Seasonal patterns
- Secular trends (long-term)
- Epidemic patterns
- Cyclical fluctuations
- Day of week effects
- Time of day variations
Example of Distribution Analysis in Community Nursing
A community health nurse investigating a tuberculosis outbreak would analyze:
- Person: Age groups affected, immune status, housing conditions
- Place: Geographic clustering of cases, environmental risk factors
- Time: When cases occurred, temporal relationship between cases
This analysis helps identify at-risk populations and target interventions effectively.
Aims & Uses of Epidemiology
Epidemiology serves multiple crucial functions in public health and community nursing practice. Understanding these aims helps nurses apply epidemiological principles effectively in their work.
Primary Aims of Epidemiology
1. Identify Disease Etiology and Risk Factors
Discover causal mechanisms and identify modifiable risk factors that can be targeted through interventions.
2. Determine Health Status of Populations
Assess population health through surveillance and screening to establish baseline measurements and identify trends.
3. Complete the Natural History of Disease
Study how diseases progress from onset to resolution, identifying opportunities for intervention at different stages.
4. Evaluate Preventive and Therapeutic Measures
Assess the effectiveness of health interventions, treatments, and programs through controlled studies.
Practical Applications in Community Health Nursing
| Application | Description | Nursing Implications |
|---|---|---|
| Community Diagnosis | Identifying health problems and needs within communities | Guides resource allocation and program planning based on population needs |
| Disease Surveillance | Ongoing systematic collection and analysis of health data | Allows early detection of outbreaks and monitoring of health trends |
| Program Planning | Designing evidence-based health interventions | Ensures interventions target actual community needs and risk factors |
| Program Evaluation | Assessing impact and effectiveness of health initiatives | Provides data to modify programs for improved outcomes |
| Policy Development | Informing health policies with evidence | Helps nurses advocate for evidence-based policy changes |
Epidemiology in Action: During the COVID-19 pandemic, community health nurses used epidemiological principles to conduct contact tracing, implement targeted testing strategies, identify high-risk populations, and evaluate the effectiveness of public health measures. This demonstrates how epidemiology serves as a foundation for evidence-based nursing practice in community settings.
Epidemiological Models of Causation of Disease
Various conceptual models have been developed to explain disease causation and guide epidemiological investigations. These models help community health nurses understand the complex interplay of factors that contribute to disease development.
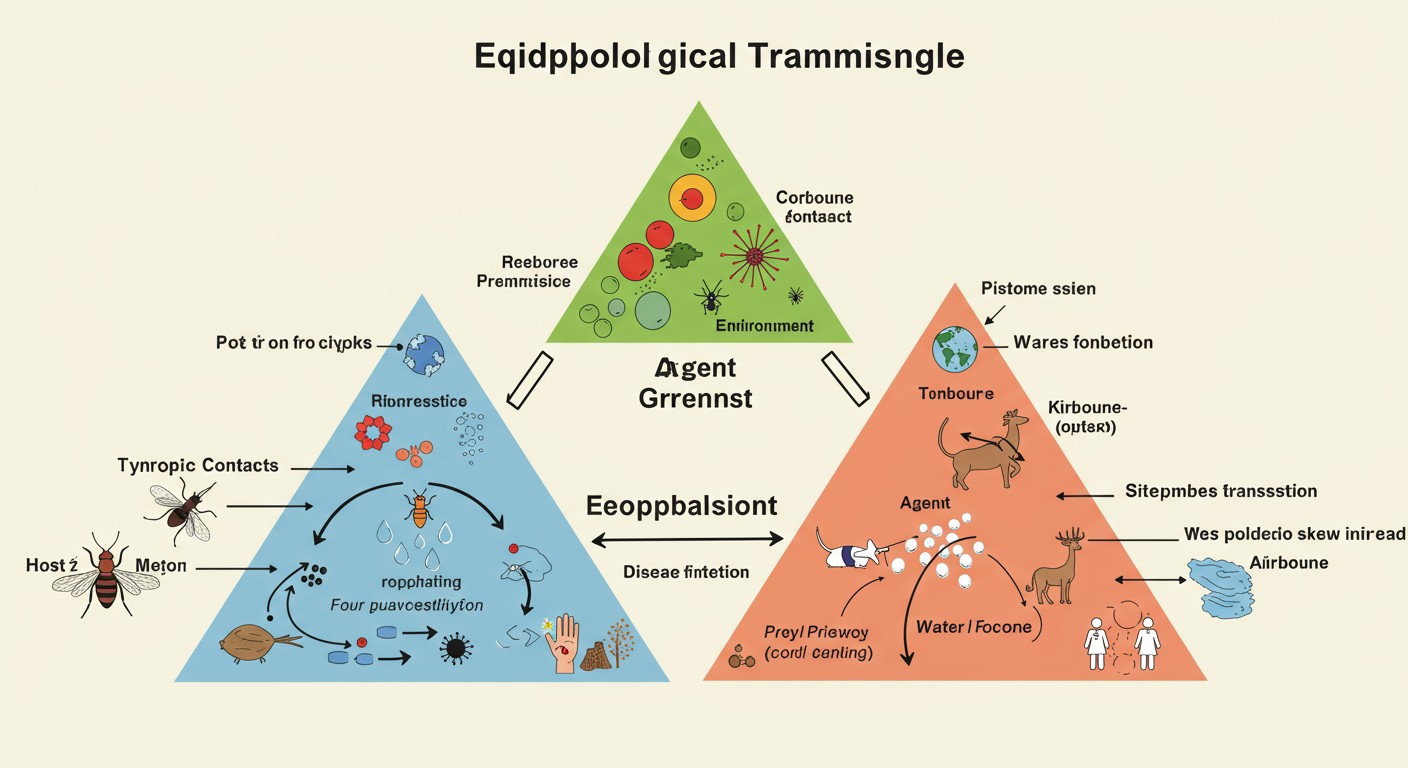
The Epidemiological Triangle illustrating the relationship between host, agent, and environment in disease causation.
Key Epidemiological Models
1. Epidemiological Triangle
The classic model focusing on three key elements:
- Agent: The causative factor (microorganism, chemical, physical force)
- Host: The human or animal susceptible to the disease
- Environment: External factors that influence exposure or transmission
Disease occurs when an agent capable of causing disease meets a susceptible host in an environment conducive to transmission or exposure.
2. Web of Causation
Recognizes that diseases rarely have a single cause but result from a complex interrelationship of multiple factors.
- Visualizes disease causation as an interconnected web of factors
- Acknowledges direct and indirect causal relationships
- Particularly useful for understanding chronic diseases
3. Wheel Model (Ecological Model)
Places the human host at the center, surrounded by layers of influencing factors:
- Genetics (innermost layer)
- Biology
- Physical environment
- Social environment (outermost layer)
Shows how multiple levels of factors interact to affect health status.
4. Social-Ecological Model
Examines how behavior and health are shaped by multiple levels of influence:
- Individual factors: Knowledge, attitudes, behaviors
- Interpersonal factors: Family, friends, social networks
- Organizational factors: Schools, workplaces, institutions
- Community factors: Relationships among organizations
- Public policy: Laws and policies at local, state, and national levels
Bradford Hill Criteria
Developed by Sir Austin Bradford Hill, these criteria help evaluate whether observed associations are causal:
MNEMONIC: “CAUSATION”
Consistency of the association
Association strength
Universality (specificity)
Sequence of events (temporality)
Analogy to other known causal relationships
Time relationship (dose-response)
Independent of confounding variables
Observations that are replicated
Natural experiments support the relationship
Nursing Application
Community health nurses use these models to:
- Guide comprehensive assessment of health problems in communities
- Identify multiple points for potential intervention
- Develop holistic prevention strategies that address various causal factors
- Explain complex health issues to community members and stakeholders
Concepts of Disease Transmission
Understanding how diseases spread is fundamental to epidemiology and community health nursing practice. Disease transmission concepts provide the framework for developing effective prevention and control strategies.
Basic Terminology in Disease Transmission
| Term | Definition | Nursing Implications |
|---|---|---|
| Infectious Disease | Illness caused by a specific infectious agent capable of being transmitted | Requires specific control measures targeted at agent, transmission, or host |
| Communicable Disease | Infectious disease that can be transmitted from person to person | Focus on breaking chain of transmission and isolation measures |
| Contagious Disease | Communicable disease easily spread through direct contact | Requires strict contact precautions and infection control |
| Vector | Living organism that transmits an infectious agent | Vector control as part of prevention strategy |
| Reservoir | Natural habitat where an infectious agent lives and multiplies | Identification and elimination/control of reservoirs |
| Fomite | Inanimate object that can harbor and transmit infectious agents | Proper disinfection procedures for surfaces and objects |
Patterns of Disease Occurrence
Endemic
Constant presence of a disease within a geographic area or population at an expected level.
Example: Malaria in certain tropical regions
Nursing Focus: Ongoing prevention, surveillance, and management
Epidemic
Occurrence of disease cases in excess of normal expectancy in a community or region.
Example: Seasonal influenza outbreaks
Nursing Focus: Outbreak investigation, containment, and emergency response
Pandemic
Epidemic occurring worldwide or over a very wide area, crossing international boundaries.
Example: COVID-19
Nursing Focus: Global coordination, mass vaccination, and public education
Sporadic
Irregular occurrence of disease cases with no clear connection between them.
Example: Isolated cases of meningitis
Nursing Focus: Case investigation and preventing progression to outbreaks
Stages in Disease Development
Understanding the natural progression of disease helps identify intervention points:
- Exposure: Contact with causative agent
- Incubation period: Time between exposure and symptom onset
- Prodromal period: Early, non-specific symptoms appear
- Illness period: Full clinical manifestations of disease
- Convalescence: Recovery phase
Critical Concept: Communicability period (when a person can transmit the disease) may not align with symptom appearance, making some diseases challenging to control.
Modes of Transmission
Disease transmission occurs through various pathways, which can be broadly categorized as direct or indirect. Understanding these modes is essential for implementing appropriate preventive measures in community health nursing.
Direct Transmission
Occurs when there is immediate transfer of infectious agents from a reservoir to a susceptible host without an intermediate object or entity.
Direct Contact
Physical contact between infected source and susceptible host.
- Person-to-person touching
- Skin-to-skin contact
- Contact with body fluids
Examples: MRSA, scabies, herpes simplex
Droplet Transmission
Transmission through relatively large respiratory droplets (>5μm) that don’t remain suspended in air.
- Typically travels short distances (<1 meter)
- Generated by coughing, sneezing, talking
- Requires close proximity to infected person
Examples: Influenza, pertussis, meningitis
Vertical Transmission
Passage of disease from mother to child during pregnancy, birth, or breastfeeding.
- Transplacental (during pregnancy)
- Perinatal (during birth)
- Postnatal (through breast milk)
Examples: HIV, hepatitis B, syphilis
Indirect Transmission
Involves the spread of infectious agents through intermediary vehicles or vectors.
Airborne Transmission
Spread via small respiratory droplets (<5μm) that remain suspended in air for long periods.
- Can travel over extended distances
- May remain infectious in the air for hours
- Requires special air handling and ventilation
Examples: Tuberculosis, measles, chickenpox
Vehicle-borne Transmission
Transmission through contaminated items or substances.
- Fomites: Inanimate objects (doorknobs, toys)
- Food: Contaminated edible items
- Water: Contaminated drinking or recreational water
- Medications: Contaminated pharmaceutical products
Examples: Norovirus, E. coli, hepatitis A
Vector-borne Transmission
Spread by living organisms that carry pathogens from one host to another.
- Mechanical: Vector physically carries pathogen
- Biological: Pathogen develops/multiplies within vector
Examples:
- Mosquitoes: Malaria, Zika, dengue fever
- Ticks: Lyme disease, Rocky Mountain spotted fever
- Fleas: Plague
Nursing Interventions by Transmission Mode
| Transmission Mode | Prevention Strategies | Community Nursing Interventions |
|---|---|---|
| Direct Contact | Handwashing, proper PPE, isolation precautions | Education on hygiene practices, screening programs, contact tracing |
| Droplet | Masks, physical distancing, respiratory etiquette | Promoting vaccination, educating about respiratory hygiene, isolation of symptomatic individuals |
| Airborne | N95 respirators, negative pressure rooms, air filtration | TB screening programs, ensuring adequate ventilation in community facilities |
| Vehicle-borne | Food safety, water treatment, proper disinfection | Community education on food handling, promoting water safety, environmental health initiatives |
| Vector-borne | Insect repellent, bed nets, vector control | Community-wide vector control programs, surveillance for vector-borne diseases |
| Vertical | Maternal screening, prophylactic treatment | Prenatal care programs, prevention of mother-to-child transmission initiatives |
MNEMONIC: “TRANSMIT”
To remember key modes of disease transmission:
Touching (direct contact)
Respiratory droplets
Airborne particles
Nutrition/food sources
Surfaces/fomites
Mother-to-child (vertical)
Insect/arthropod vectors
Tainting of water supplies
Chain of Infection
The chain of infection represents the sequence of events needed for an infection to occur. Understanding this concept helps community health nurses identify critical points for intervention to break the chain and prevent disease transmission.
Six Links in the Chain of Infection
1. Infectious Agent (Pathogen)
The microorganism capable of causing disease.
Examples: Bacteria, viruses, fungi, parasites, prions
Intervention Point: Use of antimicrobials, sterilization, disinfection
2. Reservoir
Where the pathogen lives, grows, and multiplies.
Examples: Humans, animals, environment, food, water
Intervention Point: Treatment of infected individuals, eliminating environmental reservoirs
3. Portal of Exit
The path by which the pathogen leaves the reservoir.
Examples: Respiratory tract, gastrointestinal tract, urinary tract, skin, blood
Intervention Point: Containing secretions, proper wound care, masks for respiratory conditions
4. Mode of Transmission
The method by which the pathogen moves from reservoir to host.
Examples: Direct contact, droplet, airborne, vehicle-borne, vector-borne
Intervention Point: Handwashing, isolation precautions, vector control, food/water safety
5. Portal of Entry
The path by which the pathogen enters the new host.
Examples: Mucous membranes, broken skin, respiratory tract, gastrointestinal tract
Intervention Point: Maintaining skin integrity, using protective equipment, covering wounds
6. Susceptible Host
An individual lacking effective resistance to the pathogen.
Factors affecting susceptibility: Age, nutrition, immunization status, underlying conditions, stress
Intervention Point: Immunization, nutrition support, health promotion activities
Breaking the Chain: Nursing Interventions
| Level of Prevention | Chain Link Target | Community Nursing Interventions |
|---|---|---|
| Primary Prevention (Before Disease Occurs) |
Susceptible Host |
|
| Mode of Transmission |
|
|
| Secondary Prevention (Early Detection/Treatment) |
Reservoir |
|
| Portal of Exit |
|
|
| Tertiary Prevention (Reducing Complications) |
Infectious Agent |
|
Community Health Nursing Application
The chain of infection concept helps community health nurses:
- Systematically analyze disease outbreaks in communities
- Develop targeted interventions at multiple points in the chain
- Prioritize resources based on which interventions will be most effective
- Explain disease transmission to community members in understandable terms
- Collaborate with other sectors (environmental health, education) on comprehensive prevention strategies
MNEMONIC: “LINK-UP”
To remember the six links in the chain of infection:
Lethal agent (infectious agent)
Inhabited reservoir
Narrow passage out (portal of exit)
Kinetics of movement (mode of transmission)
Unwelcome entry (portal of entry)
Person at risk (susceptible host)
Global Best Practices in Epidemiology
Around the world, various innovative approaches to epidemiology have emerged to address public health challenges. These best practices offer valuable lessons for community health nursing in different contexts.
1. Participatory Epidemiology (East Africa)
Engages community members as active partners in disease surveillance and response.
Key Components:
- Training community health workers in basic epidemiological methods
- Using local knowledge to identify disease patterns
- Community-led reporting systems using mobile technology
- Integration of traditional and conventional health knowledge
Application: Particularly effective in remote areas with limited health infrastructure. Has been successfully used for early detection of zoonotic diseases and outbreak response.
2. Syndromic Surveillance Systems (United States)
Monitors health data in real-time to detect unusual patterns before laboratory confirmation.
Key Components:
- Automated collection of pre-diagnostic data (ER visits, medication sales)
- Statistical algorithms to detect unusual patterns
- Integration with electronic health records
- Rapid alert systems for public health officials
Application: Provides early warning of emerging health threats, allowing faster public health response. Used extensively during mass gatherings and for bioterrorism preparedness.
3. One Health Approach (Global)
Integrates human, animal, and environmental health in epidemiological investigations.
Key Components:
- Collaborative multidisciplinary teams (physicians, veterinarians, environmentalists)
- Shared surveillance systems across sectors
- Joint outbreak investigations
- Coordinated prevention strategies
Application: Essential for addressing zoonotic diseases (like Ebola, COVID-19) and antimicrobial resistance. Recognizes the interconnection between human health and ecosystems.
4. Digital Contact Tracing (Singapore/South Korea)
Uses technology to enhance traditional epidemiological contact tracing methods.
Key Components:
- Smartphone applications for proximity detection
- QR code check-ins at public locations
- Integration with public health case management systems
- Privacy-preserving technologies
Application: Demonstrated effectiveness during COVID-19 pandemic by rapidly identifying exposure risks and reducing community transmission through prompt isolation and quarantine.
5. Community-Based Surveillance (Bangladesh)
Engages community health workers to conduct active surveillance in settings with limited resources.
Key Components:
- Training of community health workers in case definitions
- Regular household visits for active case finding
- Simple reporting mechanisms (often mobile-based)
- Community engagement in response activities
Application: Has been effective for diseases like cholera, tuberculosis, and maternal/child health conditions. Builds sustainable local capacity while improving case detection.
Implications for Community Health Nursing
These global best practices demonstrate several important principles for epidemiological work in community health nursing:
- Community engagement enhances the effectiveness and sustainability of epidemiological activities
- Technology integration can amplify traditional epidemiological methods
- Cross-sector collaboration is essential for addressing complex health threats
- Cultural context must be considered in epidemiological approaches
- Capacity building at the local level ensures sustainable disease surveillance and response
Community health nurses can adapt these approaches to their specific contexts while maintaining core epidemiological principles.
Summary
Epidemiology is a foundational discipline for community health nursing practice, providing the scientific basis for understanding how diseases affect populations and how to implement effective prevention and control measures.
Key Concepts Reviewed
- Definition and Concept: Epidemiology studies the distribution and determinants of health events in populations to inform disease control.
- Distribution and Frequency: Measures like incidence, prevalence, and mortality rates help quantify disease burden, while descriptive epidemiology examines patterns by person, place, and time.
- Aims and Uses: Epidemiology identifies disease causes, assesses population health, studies disease progression, and evaluates interventions.
- Epidemiological Models: Frameworks like the epidemiological triangle and web of causation explain the complex interplay of factors in disease development.
- Disease Transmission Concepts: Understanding endemic, epidemic, and pandemic patterns helps contextualize disease occurrence and guide appropriate responses.
- Modes of Transmission: Diseases spread through direct (contact, droplet, vertical) and indirect (airborne, vehicle-borne, vector-borne) pathways.
- Chain of Infection: The six-link chain (agent, reservoir, portal of exit, transmission, portal of entry, susceptible host) provides a framework for targeted interventions.
Application to Community Health Nursing Practice
Community health nurses apply epidemiological principles to:
- Conduct community health assessments that identify priority health issues
- Design and implement evidence-based prevention programs
- Participate in disease surveillance and outbreak investigations
- Educate communities about disease risks and prevention measures
- Advocate for policies that address social determinants of health
- Evaluate the effectiveness of public health interventions
By integrating epidemiological knowledge with nursing practice, community health nurses play a vital role in protecting and promoting population health.
Key Takeaways for Nursing Students
- Epidemiology provides the scientific foundation for evidence-based community health nursing practice.
- Understanding disease distribution patterns helps target nursing interventions to populations most in need.
- Knowledge of transmission modes is essential for implementing appropriate preventive measures.
- The chain of infection concept offers multiple points for nursing intervention.
- Epidemiological data should inform all levels of prevention: primary, secondary, and tertiary.
- Community participation enhances the effectiveness of epidemiological approaches.
- A global perspective on epidemiological practices enriches local community health nursing efforts.
