Epidemiology of Vector-Borne and Vaccine-Preventable Diseases: A Community Health Nursing Perspective
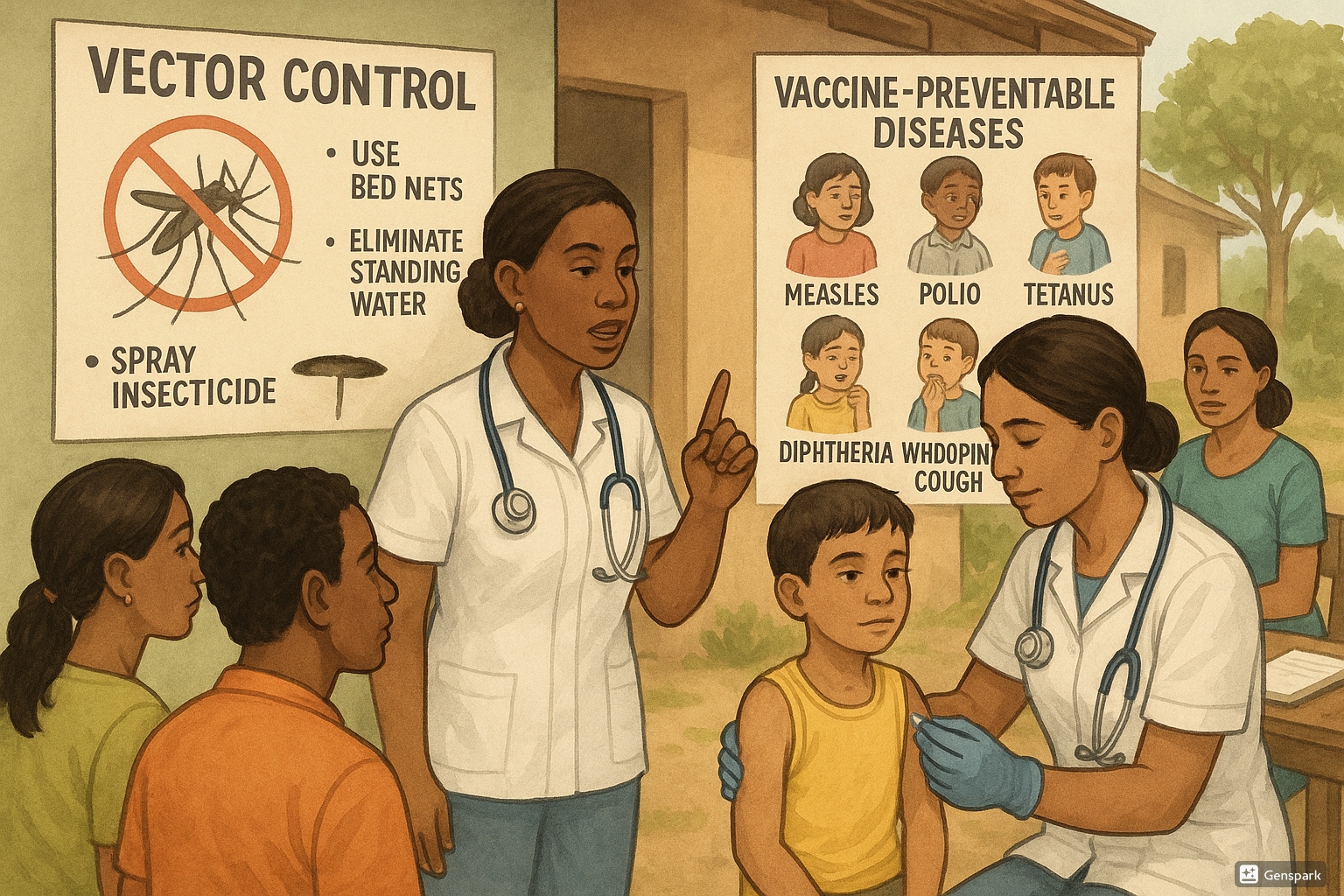
Community health nurses conducting vaccination and disease prevention activities
- 1. Introduction to Disease Prevention in Community Health Nursing
- 2. Vector-Borne Diseases: Overview and Epidemiology
- 2.1 Vector Control and Prevention Strategies
- 2.2 Screening and Diagnosis of Vector-Borne Diseases
- 2.3 Primary Management and Referral
- 3. Vaccine-Preventable Diseases: Overview
- 3.1 Diphtheria
- 3.2 Whooping Cough (Pertussis)
- 3.3 Tetanus
- 3.4 Poliomyelitis
- 3.5 Measles
- 4. Community Health Nursing Strategies for Disease Prevention
- 5. Vaccination Programs and Schedules
- 6. Disease Surveillance and Reporting
- 7. Health Education and Community Empowerment
- 8. Global Best Practices in Disease Prevention
- 9. Conclusion
1. Introduction to Disease Prevention in Community Health Nursing
Community Health Nursing plays a pivotal role in disease prevention across populations. The primary focus of disease prevention in community settings involves surveillance, early detection, prompt intervention, and health promotion activities. Nurses serve as frontline healthcare providers who implement various preventive measures to reduce the burden of communicable diseases.
Disease prevention strategies are categorized into three levels:
- Primary Prevention: Measures taken to prevent the onset of disease (e.g., vaccination, vector control)
- Secondary Prevention: Early detection through screening programs and prompt treatment
- Tertiary Prevention: Rehabilitation to reduce complications and improve quality of life
Disease prevention measures implemented by community health nurses significantly reduce morbidity and mortality rates. Through systematic approaches to preventable conditions, nurses contribute substantially to public health outcomes and community welfare.
2. Vector-Borne Diseases: Overview and Epidemiology
Vector-borne diseases are illnesses caused by pathogens transmitted through living organisms such as mosquitoes, ticks, flies, and fleas. The epidemiology of these diseases is influenced by various factors including climate change, urbanization, population movement, and socioeconomic conditions.
| Vector | Common Diseases | Geographic Distribution | Key Epidemiological Factors |
|---|---|---|---|
| Mosquitoes | Malaria, Dengue, Zika, Chikungunya, Yellow fever | Tropical and subtropical regions | Rainfall patterns, temperature, urbanization |
| Ticks | Lyme disease, Rocky Mountain spotted fever, Tick-borne encephalitis | Temperate forests, grasslands | Outdoor activities, wildlife habitats |
| Fleas | Plague, Murine typhus | Worldwide distribution | Rodent populations, poor sanitation |
| Flies | Leishmaniasis, Sleeping sickness, Onchocerciasis | Africa, Latin America, Middle East, South Asia | Rural settings, poverty, proximity to water bodies |
The global burden of vector-borne diseases is substantial, accounting for over 17% of all infectious diseases and causing more than 700,000 deaths annually. Climate change is expanding the geographic range of many vectors, leading to the emergence of diseases in previously unaffected regions.
- Vulnerable populations (children, pregnant women, elderly)
- Environmental factors (temperature, rainfall, altitude)
- Climate change impacts
- Transmission cycles (human-vector-human or animal-vector-human)
- Outbreak potential
- Resistance development (vector resistance to insecticides)
- Socioeconomic determinants
2.1 Vector Control and Prevention Strategies
Effective disease prevention in vector-borne diseases requires comprehensive vector control strategies. Community health nurses play a crucial role in implementing these strategies at the community level:
Environmental Management
- Elimination of breeding sites (stagnant water, garbage)
- Modification of living structures (screens on windows, bed nets)
- Land reclamation and drainage projects
- Community cleanup campaigns
Chemical Control
- Indoor residual spraying (IRS)
- Insecticide-treated nets (ITNs)
- Larviciding of breeding sites
- Space spraying during outbreaks
Biological Control
- Introduction of larvivorous fish
- Use of bacterial agents (Bacillus thuringiensis)
- Genetic modification of vectors
Personal Protection
- Use of repellents
- Wearing appropriate clothing
- Avoiding outdoor activities during peak vector activity
Nursing Intervention for Disease Prevention: Community health nurses should conduct regular health education sessions on personal protection measures and environmental management. Creating visual demonstrations of proper bed net use and repellent application significantly improves community adherence to preventive practices.
2.2 Screening and Diagnosis of Vector-Borne Diseases
Early detection through appropriate screening is essential for effective disease prevention and management. Community health nurses should be familiar with screening approaches for different vector-borne diseases:
| Disease | Screening Method | Diagnostic Tests | Key Clinical Features |
|---|---|---|---|
| Malaria | Fever surveillance, travel history | Rapid diagnostic tests, blood smear microscopy | Cyclical fever, chills, sweats, headache |
| Dengue | Febrile illness surveillance | NS1 antigen test, IgM/IgG antibody detection | High fever, severe headache, pain behind eyes, joint/muscle pain |
| Lyme Disease | History of tick exposure | ELISA, Western blot | Erythema migrans rash, fever, fatigue, joint pain |
| Japanese Encephalitis | Neurological symptoms in endemic areas | CSF analysis, IgM antibody detection | Fever, headache, vomiting, altered consciousness |
- Fever pattern (continuous, cyclical, biphasic)
- Exposure history (travel, outdoor activities)
- Visible rash or lesion characteristics
- Endemic area residence or visit
- Related symptoms (headache, myalgia, arthralgia)
- Persistence beyond typical viral illness duration
- Laboratory abnormalities (thrombocytopenia, leukopenia)
- Unusual manifestations (bleeding, neurological symptoms)
- Seasonal correlation
2.3 Primary Management and Referral
Community health nurses provide critical primary management for vector-borne diseases and determine appropriate referral pathways. Disease prevention efforts include prompt treatment to reduce transmission and complications:
Primary Management
- Initial assessment and triage
- Symptomatic treatment (antipyretics, pain management)
- Hydration support
- Monitoring for warning signs
- Initial dose of appropriate antimicrobials when indicated
Indications for Referral
- Severe manifestations (high-grade fever not responding to antipyretics)
- Warning signs (bleeding, respiratory distress, altered consciousness)
- Special populations (pregnant women, children under 5, elderly)
- Complex diagnostic needs
- Treatment requiring hospitalization
Follow-up Care
- Adherence monitoring for medication regimens
- Assessment of treatment response
- Surveillance for complications
- Reinforcement of preventive measures
- Contact tracing and family screening where applicable
Critical Point for Disease Prevention: Delayed recognition and management of vector-borne diseases significantly increases mortality rates. Community health nurses should maintain a high index of suspicion during peak transmission seasons and prioritize rapid testing and treatment initiation.
3. Vaccine-Preventable Diseases: Overview
Vaccine-preventable diseases (VPDs) have been significantly controlled through effective immunization programs, representing one of public health’s greatest achievements in disease prevention. Despite this success, these diseases continue to cause outbreaks in under-vaccinated populations.
According to the World Health Organization (WHO), immunization prevents 2-3 million deaths annually. However, an additional 1.5 million deaths could be avoided if global vaccination coverage improves. Community health nurses are essential to achieving optimal coverage through their role in vaccination programs.
3.1 Diphtheria
Epidemiology
Diphtheria is an acute bacterial disease caused by toxin-producing strains of Corynebacterium diphtheriae. Once a major cause of illness and death among children, its incidence has dramatically decreased due to widespread vaccination.
- Transmission: Respiratory droplets or direct contact with respiratory secretions
- Risk factors: Incomplete immunization, crowded living conditions, poor hygiene
- Global distribution: Higher incidence in areas with low vaccination coverage
- Case fatality rate: 5-10% even with appropriate treatment
Prevention and Control Measures
- Primary prevention through DTaP/Tdap vaccination
- Maintaining high vaccination coverage (>90%) for herd immunity
- Enhanced surveillance in high-risk areas
- Contact tracing and prophylaxis during outbreaks
- Improved living conditions and reduced overcrowding
Screening and Diagnosis
- Clinical presentation: Characteristic gray adherent membrane in throat
- Laboratory confirmation: Throat swab for culture and toxin testing
- Point-of-care screening: Not widely available
Primary Management
- Immediate administration of diphtheria antitoxin (DAT)
- Antimicrobial therapy (erythromycin or penicillin)
- Airway management if respiratory obstruction
- Isolation until negative cultures
Referral Criteria
- Suspected cases require immediate hospital referral
- Complications (myocarditis, polyneuritis)
- Respiratory distress
- Difficulty swallowing
- Infectious and highly contagious
- Pseudo-membrane (gray-white) formation
- Hoarseness and “bull neck” appearance
- Toxin-mediated disease
- High fever
- Erythromycin or penicillin treatment
- Respiratory obstruction risk
- Isolation required
- Antitoxin administration essential
3.2 Whooping Cough (Pertussis)
Epidemiology
Pertussis is a highly contagious respiratory disease caused by Bordetella pertussis. Despite vaccination programs, pertussis remains endemic worldwide with cyclic outbreaks every 3-5 years.
- Transmission: Airborne droplets from coughing or sneezing
- Age distribution: Highest mortality in infants <1 year; increasing incidence in adolescents and adults
- Disease burden: Estimated 24.1 million cases and 160,700 deaths globally per year
- Seasonality: Peak incidence in summer and autumn
Prevention and Control Measures
- Vaccination with DTaP (for children) and Tdap (for adolescents and adults)
- Maternal Tdap vaccination during pregnancy (cocoon strategy)
- Early case identification and treatment
- Prophylaxis for household contacts
- Isolation of confirmed cases
Screening and Diagnosis
- Clinical case definition: Cough lasting ≥2 weeks with paroxysms, inspiratory “whoop,” or post-tussive vomiting
- Laboratory methods: PCR testing of nasopharyngeal specimens, culture
- Serological testing for late diagnosis
Primary Management
- Antimicrobial therapy (azithromycin, clarithromycin, or erythromycin)
- Supportive care for cough management
- Close monitoring for apnea in infants
- Oxygen supplementation if needed
Referral Criteria
- Infants <6 months with suspected pertussis
- Presence of complications (pneumonia, encephalopathy)
- Cyanosis or apneic episodes
- Inability to maintain hydration
Disease Prevention Tip: Community health nurses should emphasize the importance of “cocooning” – vaccinating all close contacts of newborns – as a strategy to protect infants too young to be fully vaccinated against pertussis.
3.3 Tetanus
Epidemiology
Tetanus is a non-communicable disease caused by the toxin of Clostridium tetani, which enters the body through contaminated wounds. It remains a significant public health problem in regions with inadequate vaccination coverage.
- Global burden: Approximately 34,000 neonatal deaths annually
- Risk factors: Inadequate immunization, contaminated wounds, unsafe delivery practices
- Distribution: Higher prevalence in developing countries
- Case fatality rate: 10-80% depending on age, comorbidities, and healthcare access
Prevention and Control Measures
- Universal immunization with tetanus toxoid-containing vaccines
- Maternal tetanus vaccination during pregnancy
- Proper wound management and cleaning
- Tetanus prophylaxis for high-risk injuries
- Promotion of clean delivery practices
| Wound Classification | Clean, Minor Wounds | All Other Wounds | ||
|---|---|---|---|---|
| History of tetanus immunization (doses) | Td/Tdap | TIG | Td/Tdap | TIG |
| Unknown or <3 | Yes | No | Yes | Yes |
| ≥3 | No* | No | No** | No |
*Yes, if ≥10 years since last dose. **Yes, if ≥5 years since last dose. Td: Tetanus and diphtheria toxoids. Tdap: Tetanus, diphtheria, and pertussis vaccine. TIG: Tetanus immune globulin.
Screening and Diagnosis
- Clinical diagnosis based on presentation (no laboratory test confirms tetanus)
- Characteristic manifestations: Trismus (lockjaw), risus sardonicus, muscle rigidity, spasms
- Risk assessment of wounds
Primary Management
- Wound cleaning and debridement
- Tetanus immune globulin (TIG) administration
- Antimicrobial therapy (metronidazole preferred)
- Control of muscle spasms and respiratory support
Referral Criteria
- All suspected cases require immediate hospitalization
- Intensive care management often needed
- Trismus (lockjaw) – early sign
- Entry through contaminated wounds
- Toxin-mediated disease
- Autonomic instability (fluctuating blood pressure, tachycardia)
- Neck stiffness and rigidity
- Unimmunized status – major risk factor
- Spasms triggered by stimuli (noise, light, touch)
3.4 Poliomyelitis
Epidemiology
Poliomyelitis is a highly infectious viral disease caused by poliovirus that primarily affects children under 5 years. Through global eradication efforts, wild poliovirus remains endemic in only two countries: Afghanistan and Pakistan.
- Transmission: Fecal-oral route, primarily through contaminated water
- Global status: 99% reduction in cases since 1988
- Risk factors: Under-immunization, poor sanitation, crowded living conditions
- Clinical manifestations: 72% asymptomatic; <1% develop paralysis
Prevention and Control Measures
- Routine immunization with oral polio vaccine (OPV) and/or inactivated polio vaccine (IPV)
- Supplementary immunization activities (mass vaccination campaigns)
- Active surveillance for acute flaccid paralysis (AFP)
- Environmental monitoring for poliovirus
- Improved sanitation and access to clean water
Screening and Diagnosis
- Active surveillance for acute flaccid paralysis (AFP)
- Laboratory confirmation: Stool specimen collection for virus isolation
- Clinical criteria: Acute onset of flaccid paralysis with decreased or absent tendon reflexes
Primary Management
- No specific antiviral treatment available
- Supportive care (pain management, physical therapy)
- Prevention of complications (contractures, pressure sores)
- Nutritional support
Referral Criteria
- Any case of acute flaccid paralysis requires immediate notification and referral
- Respiratory involvement necessitating ventilatory support
- Bulbar paralysis affecting swallowing
Disease Prevention Success: Polio eradication represents one of the most successful global disease prevention initiatives. Cases have decreased by over 99% since 1988, from an estimated 350,000 cases to 33 reported cases in 2018. Community health nurses play a crucial role in maintaining vaccination coverage and surveillance.
3.5 Measles
Epidemiology
Measles is one of the most contagious viral diseases, caused by the measles virus (genus Morbillivirus). Despite the availability of a safe and effective vaccine, measles remains a leading cause of vaccine-preventable deaths globally.
- Transmission: Airborne spread of respiratory droplets
- Basic reproduction number (R₀): 12-18 (one infected person can infect 12-18 susceptible individuals)
- Global burden: Approximately 140,000 deaths annually, primarily children under 5 years
- Complications: Pneumonia, encephalitis, subacute sclerosing panencephalitis (SSPE)
Prevention and Control Measures
- Two doses of measles-containing vaccine (MCV)
- Maintaining high population immunity (≥95%) for herd protection
- Supplementary immunization activities in high-risk areas
- Case-based surveillance with laboratory confirmation
- Contact tracing and post-exposure prophylaxis
Screening and Diagnosis
- Clinical case definition: Fever and maculopapular rash with cough, coryza, or conjunctivitis
- Laboratory confirmation: Serology for measles-specific IgM antibodies
- Detection of measles RNA by RT-PCR
- Pathognomonic sign: Koplik’s spots (small white spots on buccal mucosa)
Primary Management
- Vitamin A supplementation (two doses 24 hours apart)
- Supportive care (hydration, antipyretics, nutritional support)
- Management of complications
- Isolation to prevent transmission
Referral Criteria
- Severe or complicated measles
- Presence of danger signs (inability to drink, persistent vomiting, convulsions)
- Pneumonia, encephalitis, severe malnutrition
- Children <6 months, pregnant women, immunocompromised individuals
- Maculopapular rash spreading from head to trunk to extremities
- Encephalitis (rare but serious complication)
- Airborne transmission
- Subacute sclerosing panencephalitis (late complication)
- Lymphopenia commonly observed
- Extremely contagious (R₀ 12-18)
- Secondary bacterial infections (pneumonia, otitis media)
4. Community Health Nursing Strategies for Disease Prevention
Community health nurses employ various strategies to prevent and control both vector-borne and vaccine-preventable diseases at the population level:
Community Assessment and Surveillance
- Rapid assessment surveys to identify disease burden
- Active case finding in high-risk populations
- Vector surveillance and mapping
- Vaccine coverage assessment
- Monitoring for unusual disease clusters or outbreaks
Health Promotion and Education
- Culturally appropriate health education campaigns
- School-based health education programs
- Community engagement through local leaders and influencers
- Use of multiple media channels for disease prevention messaging
- Demonstration of preventive practices
Outreach Services
- Mobile immunization clinics
- Home visits for high-risk populations
- Community screening programs
- Vector control demonstrations
- Distribution of preventive tools (bed nets, repellents)
Intersectoral Collaboration
- Partnerships with water and sanitation departments
- Collaboration with education sector for school-based interventions
- Working with agricultural sectors on pesticide use
- Engaging community-based organizations
- Coordination with local government for resource allocation
Effective Disease Prevention Strategy: Community health nurses should develop “community champions” for disease prevention by identifying and training influential community members who can promote vaccination and preventive practices. These champions significantly enhance the acceptance and sustainability of prevention programs.
5. Vaccination Programs and Schedules
Vaccination remains the cornerstone of disease prevention for vaccine-preventable diseases. Community health nurses play a pivotal role in implementing vaccination programs according to national guidelines.
Standard Immunization Schedule
| Age | Vaccines | Target Diseases | Route |
|---|---|---|---|
| Birth | BCG, OPV0, Hep B1 | Tuberculosis, Polio, Hepatitis B | Intradermal, Oral, IM |
| 6 weeks | OPV1, Penta1 (DTwP+HepB+Hib), PCV1, RVV1 | Polio, Diphtheria, Tetanus, Pertussis, Hepatitis B, Hib, Pneumococcal disease, Rotavirus | Oral, IM, IM, Oral |
| 10 weeks | OPV2, Penta2, PCV2, RVV2 | Same as above | Same as above |
| 14 weeks | OPV3, Penta3, PCV3, RVV3, IPV | Same as above plus Injectable Polio | Same as above plus IM |
| 9 months | MR1 | Measles, Rubella | Subcutaneous |
| 16-24 months | MR2, OPV booster, DTP booster | Measles, Rubella, Polio, Diphtheria, Tetanus, Pertussis | Subcutaneous, Oral, IM |
| 5-6 years | DTP booster | Diphtheria, Tetanus, Pertussis | IM |
| 10 & 16 years | Td | Tetanus, diphtheria | IM |
Strategies for Improving Vaccination Coverage
- Reducing missed opportunities for vaccination
- Defaulter tracking and reminder systems
- Addressing vaccine hesitancy through education
- Extended hours and outreach services
- Integration with other maternal and child health services
- School-based vaccination programs
Cold Chain Maintenance
- Temperature monitoring (2-8°C for most vaccines)
- Proper storage equipment (refrigerators, cold boxes, vaccine carriers)
- Regular maintenance of cold chain equipment
- Contingency plans for power failures
- Training of personnel in cold chain management
Critical Disease Prevention Point: Maintaining the cold chain integrity is essential for effective disease prevention through vaccination. Exposing vaccines to temperatures outside recommended ranges can reduce potency and effectiveness, leading to inadequate protection despite apparent compliance with vaccination schedules.
6. Disease Surveillance and Reporting
Effective disease prevention requires robust surveillance systems to detect and respond to cases promptly. Community health nurses are integral to disease surveillance networks.
Types of Surveillance
- Passive surveillance: Routine reporting of cases by health facilities
- Active surveillance: Proactive case finding by health workers
- Sentinel surveillance: Selected sites reporting detailed information
- Syndromic surveillance: Monitoring of symptom patterns
- Vector surveillance: Monitoring vector populations and infection rates
Surveillance Activities for Community Health Nurses
- Case identification using standard case definitions
- Immediate reporting of notifiable diseases
- Maintenance of line-listing during outbreaks
- Collection and transportation of specimens
- Conducting simple surveys and assessments
- Participating in outbreak investigations
Data Analysis and Use
- Monitoring disease trends over time
- Geographic mapping of cases
- Identification of high-risk populations
- Assessment of intervention impact
- Planning resource allocation based on disease burden
- Recognize cases using standard case definitions
- Enter data accurately and completely
- Promptly notify appropriate authorities
- Outbreak detection through pattern recognition
- Respond with appropriate interventions
- Track outcomes and evaluate effectiveness
7. Health Education and Community Empowerment
Health education is essential for disease prevention and control. Community health nurses design and implement educational interventions tailored to community needs.
Key Health Education Messages for Disease Prevention
- Importance of complete vaccination schedules
- Recognition of early disease signs and symptoms
- Vector control methods at household level
- Personal protection measures
- When and where to seek healthcare
- Promoting behavior change for prevention
Educational Approaches
- Individual counseling during clinic visits
- Group education sessions
- Community meetings and demonstrations
- School health programs
- Mass media campaigns
- Use of visual aids and demonstrations
- Peer education programs
Community Empowerment Strategies
- Formation of village health committees
- Training community health volunteers
- Participatory learning and action cycles
- Community-led total sanitation approaches
- Microplanning for disease prevention with community involvement
Effective disease prevention education should use the “KAP” approach – addressing Knowledge gaps, changing Attitudes, and promoting Practices that reduce disease risk. This comprehensive approach ensures that information translates into actual preventive behaviors.
8. Global Best Practices in Disease Prevention
Several global initiatives and approaches have demonstrated significant success in disease prevention and control:
Global Polio Eradication Initiative (GPEI)
The GPEI has reduced polio cases by over 99% since its launch in 1988, using strategies including:
- National Immunization Days reaching millions of children
- Environmental surveillance to detect circulation
- Innovative approaches to reach children in conflict zones
- Transition from OPV to IPV to eliminate vaccine-derived poliovirus
Integrated Vector Management (IVM)
The WHO-recommended IVM approach combines multiple interventions for vector control:
- Integration of chemical and non-chemical methods
- Inter-sectoral collaboration between health, environment, and agriculture sectors
- Community participation in vector control activities
- Evidence-based decision making for context-specific interventions
- Sustainable approach that minimizes environmental impact
Reaching Every District (RED) Approach
The RED approach focuses on improving immunization coverage in low-performing districts through:
- Re-establishing outreach services
- Supportive supervision
- Community engagement
- Monitoring and use of data for action
- Planning and resource management
Thailand’s Village Health Volunteer Program
Thailand’s successful community-based disease prevention model features:
- Network of over 1 million volunteer health workers
- Integration of prevention for multiple diseases
- Regular training and supportive supervision
- Digital health tools for reporting and monitoring
- Recognition and incentive system for volunteers
Rwanda’s Human Papillomavirus (HPV) Vaccination Program
Rwanda achieved over 90% HPV vaccination coverage through:
- School-based vaccination approach
- Strong political commitment
- Community sensitization and education
- Public-private partnerships
- Integration with adolescent health services
9. Conclusion
Disease prevention through comprehensive approaches to vector-borne and vaccine-preventable diseases remains a cornerstone of community health nursing practice. By implementing evidence-based prevention strategies, conducting effective surveillance, delivering quality immunization services, and empowering communities, nurses contribute significantly to reducing the burden of these preventable conditions.
The integration of traditional public health approaches with innovative strategies and technologies offers promising avenues for enhanced disease prevention efforts globally. Community health nurses are uniquely positioned to lead these efforts through their close connection with communities and their holistic approach to health promotion and disease prevention.
As we continue to face challenges such as climate change, urbanization, and vaccine hesitancy, the role of community health nursing in disease prevention becomes increasingly critical. By applying the principles and approaches outlined in these notes, nurses can effectively contribute to local, national, and global efforts to control and eliminate vector-borne and vaccine-preventable diseases.
