First Aid Management
Wounds, Hemorrhage & Shock
Comprehensive Nursing Study Notes
Comprehensive first aid management in emergency nursing practice
Table of Contents
Learning Objectives
Identify different types of wounds and their characteristics
Demonstrate proper wound assessment techniques
Apply evidence-based hemorrhage control methods
Recognize signs and symptoms of different shock types
Implement appropriate shock management interventions
Understand the pathophysiology of wound healing
Apply proper sterile techniques in wound care
Document and communicate findings effectively
Wound Management
Pathophysiology of Wound Healing
Wound healing is a complex, dynamic process involving four overlapping phases: hemostasis, inflammation, proliferation, and maturation. Understanding these phases is crucial for effective nursing interventions and optimal patient outcomes. Each phase has specific cellular activities, time frames, and clinical manifestations that guide our assessment and treatment decisions.
1. Hemostasis Phase (0-30 minutes)
- • Vasoconstriction reduces blood loss
- • Platelet aggregation forms initial clot
- • Coagulation cascade activates fibrin formation
- • Temporary wound closure achieved
2. Inflammatory Phase (1-5 days)
- • Vasodilation increases blood flow
- • Neutrophils remove bacteria and debris
- • Macrophages coordinate healing response
- • Classic signs: redness, swelling, heat, pain
3. Proliferation Phase (5-21 days)
- • Fibroblasts produce collagen matrix
- • Angiogenesis creates new blood vessels
- • Granulation tissue fills wound defect
- • Epithelialization resurfaces wound
4. Maturation Phase (21 days-2 years)
- • Collagen remodeling increases strength
- • Scar tissue formation and refinement
- • Wound contracts to minimize size
- • Final tensile strength reaches 80% of original
Types of Wounds
Acute Wounds
Incisional Wounds
Clean cuts with smooth edges, minimal tissue loss. Typically heal by primary intention.
Lacerations
Irregular, torn wounds with possible tissue bridges. May require suturing.
Abrasions
Superficial scraping injuries affecting epidermis and upper dermis.
Puncture Wounds
Deep, narrow wounds with potential for internal organ injury.
Chronic Wounds
Pressure Ulcers
Localized tissue damage from prolonged pressure, shear, or friction forces.
Diabetic Ulcers
Neuropathic or ischemic wounds in diabetic patients with poor healing.
Venous Ulcers
Lower extremity wounds caused by chronic venous insufficiency.
Arterial Ulcers
Ischemic wounds resulting from inadequate arterial blood supply.
Burn Classifications
First Degree (Superficial)
Epidermis only. Red, dry, painful. Heals in 3-7 days without scarring.
Second Degree (Partial Thickness)
Epidermis and dermis. Blistered, moist, very painful. 2-3 weeks healing.
Third Degree (Full Thickness)
All skin layers destroyed. Dry, leathery, painless. Requires grafting.
Fourth Degree
Extends to muscle, bone. Charred appearance. Requires extensive surgery.
Comprehensive Wound Assessment
The WOUNDS Assessment Framework
W – Wound Dimensions
- • Length, width, depth measurements
- • Wound bed percentage assessment
- • Tunneling and undermining evaluation
O – Odor and Exudate
- • Odor: None, mild, moderate, strong, foul
- • Exudate amount: None, scant, moderate, heavy
- • Exudate type: Serous, sanguineous, purulent
U – Undermining
- • Document using clock face method
- • Measure depth of undermining
- • Assess for tunneling presence
N – Necrotic Tissue
- • Black eschar (dry necrosis)
- • Yellow slough (wet necrosis)
- • Percentage of wound bed covered
D – Damage/Tissue Type
- • Red granulation tissue (healthy)
- • Pink epithelial tissue (healing)
- • Pale/dusky tissue (compromised)
S – Surrounding Skin
- • Color, temperature, texture
- • Edema, induration, maceration
- • Signs of infection or inflammation
Pain Assessment
PQRST Method:
- P – Provocation/Palliation factors
- Q – Quality of pain (sharp, burning, aching)
- R – Region/Radiation of pain
- S – Severity (0-10 scale)
- T – Timing (constant, intermittent)
Infection Assessment
Classic Signs:
- • Rubor – Erythema/redness
- • Calor – Increased temperature
- • Dolor – Pain/tenderness
- • Tumor – Swelling/edema
- • Functio laesa – Loss of function
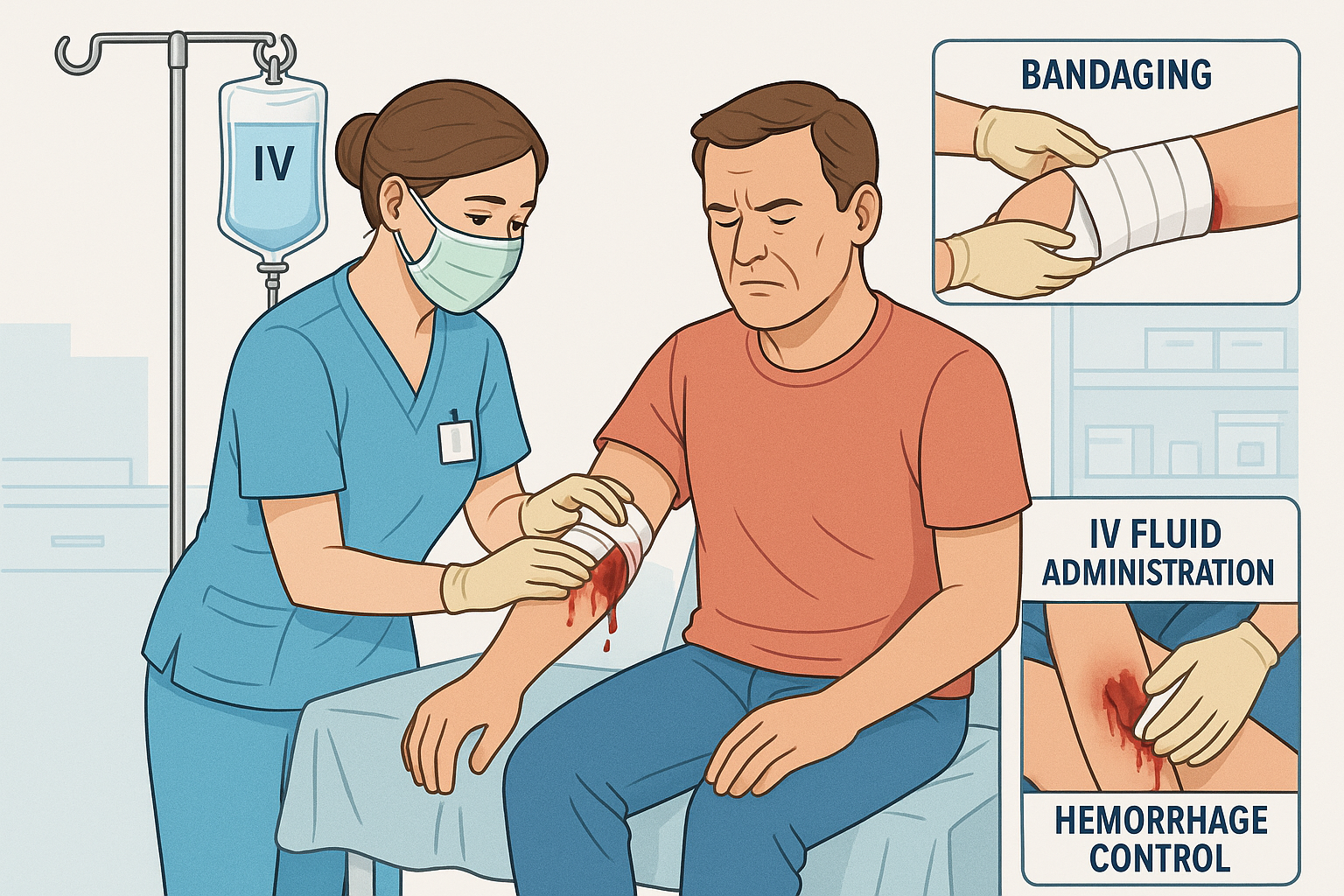
Hemorrhage Control
Classifications of Hemorrhage
Class I
Compensated
- • Blood loss: <15%
- • Volume: <750mL
- • HR: <100 bpm
- • BP: Normal
- • Minimal symptoms
Class II
Mild Shock
- • Blood loss: 15-30%
- • Volume: 750-1500mL
- • HR: 100-120 bpm
- • BP: Slight ↓
- • Anxiety, thirst
Class III
Moderate Shock
- • Blood loss: 30-40%
- • Volume: 1500-2000mL
- • HR: 120-140 bpm
- • BP: ↓ systolic
- • Confusion, oliguria
Class IV
Severe Shock
- • Blood loss: >40%
- • Volume: >2000mL
- • HR: >140 bpm
- • BP: ↓↓ systolic
- • Lethargy, anuria
STOP THE BLEED Protocol
1. Direct Pressure
- • Apply firm, continuous pressure
- • Use sterile gauze or clean cloth
- • Don’t remove blood-soaked materials
- • Add more layers if needed
2. Elevation
- • Raise injured area above heart level
- • Only if no fracture suspected
- • Combine with direct pressure
- • Use gravity to reduce blood flow
3. Pressure Points
- • Brachial artery (upper arm)
- • Femoral artery (groin)
- • Temporal artery (head)
- • Apply between wound and heart
4. Tourniquet (Last Resort)
- • Only for severe limb hemorrhage
- • Place 2-3 inches above wound
- • Document application time
- • Maximum safe time: 2 hours
Shock Management
Pathophysiology of Shock
Shock is a life-threatening condition characterized by inadequate tissue perfusion and cellular oxygen delivery. The body’s compensatory mechanisms initially maintain vital organ function, but progressive deterioration leads to cellular dysfunction, organ failure, and death if untreated. Understanding the pathophysiology is essential for early recognition and appropriate intervention.
Hypovolemic
Inadequate circulating volume
- • Hemorrhage
- • Dehydration
- • Burns
- • Third spacing
Cardiogenic
Pump failure
- • MI/Heart failure
- • Arrhythmias
- • Valve dysfunction
- • Cardiomyopathy
Distributive
Vasodilation
- • Septic shock
- • Anaphylaxis
- • Neurogenic
- • Drug-induced
Obstructive
Mechanical obstruction
- • Pulmonary embolism
- • Cardiac tamponade
- • Pneumothorax
- • Aortic stenosis
Shock Assessment & Recognition
Early/Compensated
- • Anxiety, restlessness
- • Tachycardia (HR >100)
- • Normal blood pressure
- • Skin pale, cool
- • Decreased urine output
- • Thirst
Progressive/Decompensated
- • Confusion, lethargy
- • Tachycardia (HR >120)
- • Hypotension (SBP <90)
- • Skin mottled, diaphoretic
- • Oliguria (<0.5 mL/kg/hr)
- • Weak, thready pulse
Irreversible/End-stage
- • Unresponsive, comatose
- • Bradycardia or arrhythmias
- • Severe hypotension
- • Skin cold, cyanotic
- • Anuria
- • Organ failure
Shock Management Protocol
Immediate Actions (0-5 minutes)
- • Assess airway, breathing, circulation
- • Administer high-flow oxygen
- • Establish IV access (2 large bore)
- • Obtain vital signs and Glasgow Coma Scale
- • Control external bleeding
Secondary Assessment (5-15 minutes)
- • Complete head-to-toe examination
- • Obtain focused history (SAMPLE)
- • Monitor ECG and pulse oximetry
- • Insert urinary catheter
- • Laboratory studies (CBC, BMP, lactate)
Fluid Resuscitation
- • Crystalloids: 1-2L normal saline or LR
- • Blood products if hemorrhagic shock
- • Vasopressors if distributive shock
- • Monitor response and urine output
- • Avoid fluid overload
Definitive Care
- • Treat underlying cause
- • Surgical intervention if indicated
- • Intensive care monitoring
- • Organ support therapy
- • Prevent complications
Memory Aids & Mnemonics
WOUNDS Assessment
SHOCK Recognition
STOP THE BLEED
PQRST Pain Assessment
Nursing Implementation in Practice
Evidence-Based Nursing Interventions
Assessment Phase
- • Systematic wound evaluation using WOUNDS framework
- • Pain assessment with validated tools (0-10 scale)
- • Neurological status monitoring (GCS, pupils)
- • Vital signs trending and documentation
- • Risk factor identification and history taking
- • Infection surveillance and early detection
Intervention Phase
- • Sterile wound cleaning and irrigation techniques
- • Appropriate dressing selection and application
- • Hemorrhage control using progressive methods
- • IV access establishment and fluid management
- • Pain management using multimodal approaches
- • Patient positioning and comfort measures
Evaluation Phase
- • Wound healing progress monitoring
- • Treatment effectiveness evaluation
- • Complication prevention and early detection
- • Patient response to interventions
- • Care plan modification based on outcomes
- • Discharge planning and patient education
Patient Education Priorities
Wound Care Instructions
- • Proper hand hygiene techniques
- • Dressing change procedures
- • Signs of infection recognition
- • When to seek medical attention
Prevention Strategies
- • Safety measures at home and work
- • Proper nutrition for healing
- • Activity restrictions and modifications
- • Follow-up appointment importance
Safety Considerations
Universal Precautions
- • Personal protective equipment use
- • Proper sharps disposal
- • Hand hygiene protocols
- • Bloodborne pathogen awareness
Environmental Safety
- • Sterile field maintenance
- • Equipment inspection and preparation
- • Emergency equipment accessibility
- • Team communication protocols
Quality Improvement Initiatives
Documentation Excellence
- • Standardized assessment tools
- • Photography for wound tracking
- • Electronic health record optimization
- • Legal compliance requirements
Interdisciplinary Collaboration
- • Wound care specialist consultation
- • Physician communication protocols
- • Physical therapy coordination
- • Nutritionist involvement
Outcome Measurement
- • Healing rate tracking
- • Infection prevention metrics
- • Patient satisfaction scores
- • Cost-effectiveness analysis
Clinical Case Studies
Case Study 1: Traumatic Laceration with Hemorrhage
Patient Presentation
A 28-year-old construction worker presents to the ED with a deep laceration to his right forearm from a circular saw accident. The wound is approximately 8 cm long, 3 cm wide, and 2 cm deep, with active bleeding. Patient is conscious and alert, complaining of severe pain (8/10).
Vital Signs: BP 110/70, HR 110, RR 22, SpO2 98%, Temp 98.6°F
Medical History: No significant medical history, up-to-date on tetanus
Nursing Assessment & Interventions
- • Primary Survey: Airway patent, breathing adequate, circulation stable
- • Wound Assessment: WOUNDS framework application
- • Hemorrhage Control: Direct pressure with sterile gauze
- • IV Access: 18G IV in left antecubital fossa
- • Pain Management: IV morphine 4mg administered
- • Documentation: Detailed wound description and photos
Learning Points
- • Direct pressure effectively controlled bleeding without need for pressure points
- • Early pain management improved patient cooperation during wound cleaning
- • Systematic assessment prevented missed injuries (checked for nerve/tendon damage)
- • Proper documentation supported quality care and legal requirements
Case Study 2: Hypovolemic Shock from GI Bleeding
Patient Presentation
A 65-year-old female with history of peptic ulcer disease presents with hematemesis and melena for 2 days. She appears pale, diaphoretic, and anxious. Reports dizziness when standing and weakness.
Vital Signs: BP 85/50, HR 125, RR 24, SpO2 94%, Temp 97.8°F
Medical History: PUD, HTN, takes NSAIDs regularly
Assessment: Class III hemorrhagic shock
Shock Management Protocol
- • Airway/Breathing: High-flow oxygen at 15L/min
- • Circulation: Two 16G IVs, blood type & crossmatch
- • Fluid Resuscitation: 1L NS bolus, then blood products
- • Monitoring: Continuous cardiac, hourly vitals
- • Labs: CBC, BMP, PT/PTT, lactate, ABG
- • Positioning: Trendelenburg position initially
Critical Nursing Considerations
- • Recognized early signs of hypovolemic shock (tachycardia, hypotension, altered mental status)
- • Prioritized rapid IV access and fluid resuscitation over less critical assessments
- • Monitored response to interventions (improved BP, decreased HR after fluid bolus)
- • Prepared for potential emergency endoscopy and surgical intervention
Case Study 3: Thermal Burn with Distributive Shock
Patient Presentation
A 42-year-old male sustained 25% TBSA second-degree burns to torso and arms in a house fire. Patient is conscious but in severe pain. Burns are red, blistered, and weeping. Some areas appear deeper with white, leathery appearance.
Vital Signs: BP 90/60, HR 130, RR 28, SpO2 96%, Temp 99.2°F
Assessment: Major burn injury with developing shock
Comprehensive Burn Care
- • Airway Assessment: No inhalation injury signs
- • Fluid Resuscitation: Parkland formula calculation
- • Wound Care: Cool, moist dressings to burns
- • Pain Management: IV opioids, avoid IM routes
- • Monitoring: Hourly urine output, vital signs
- • Transfer Prep: Burn center consultation
Specialized Burn Considerations
- • Calculated fluid requirements using Parkland formula (4mL × kg × %TBSA burn)
- • Recognized need for specialized burn center care due to burn size and complexity
- • Avoided ice application which could worsen tissue damage
- • Prepared for potential complications including compartment syndrome
Summary & Key Takeaways
Essential Competencies
- Systematic wound assessment using evidence-based frameworks
- Progressive hemorrhage control techniques from direct pressure to tourniquets
- Early shock recognition and immediate stabilization interventions
- Sterile technique application in emergency wound care
- Comprehensive patient education and discharge planning
Critical Safety Points
- Always prioritize personal safety and universal precautions
- Time-sensitive interventions require immediate action and clear priorities
- Effective communication with team members prevents errors and improves outcomes
- Thorough documentation supports continuity of care and legal protection
- Continuous learning and skill maintenance are essential for competent practice
Remember: Every second counts in emergency situations. Systematic assessment, prompt intervention, and continuous monitoring save lives.
Your knowledge, skills, and quick thinking as a nurse can make the difference between life and death, disability and recovery, despair and hope for patients and their families.
