GI Bleeding Disorders
Comprehensive Nursing Education Notes
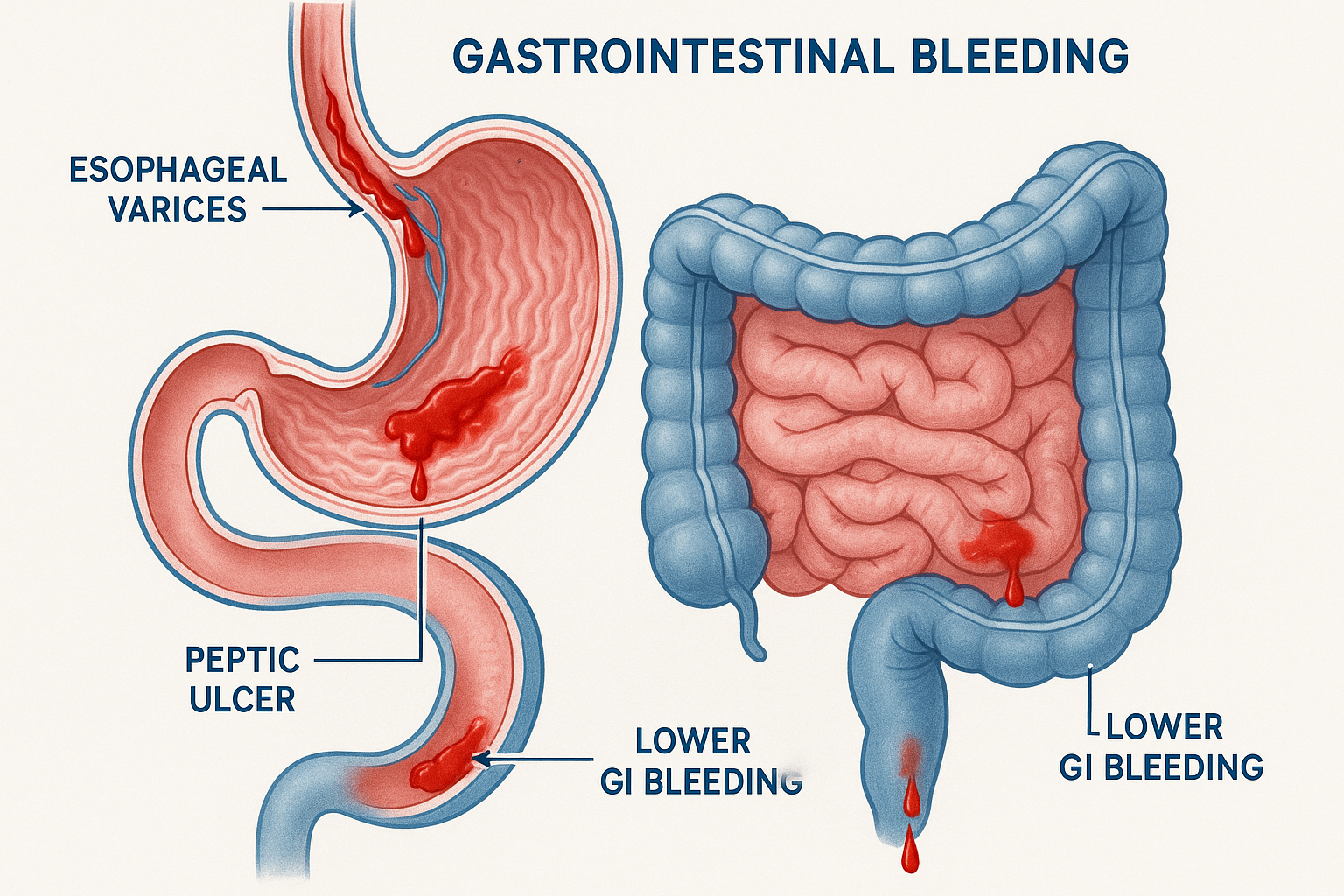
Figure 1: Anatomical overview of common GI bleeding sites
Table of Contents
1. Overview & Definition
Gastrointestinal (GI) bleeding represents a critical medical emergency characterized by bleeding from any portion of the digestive tract, extending from the mouth to the anus. This condition affects approximately 300,000 hospital admissions annually in the United States, with mortality rates ranging from 2-10% depending on the underlying cause and patient comorbidities.
Clinical Pearl
GI bleeding accounts for over 300,000 hospitalizations yearly, making it one of the most common gastroenterology emergencies. Early recognition and intervention are crucial for optimal patient outcomes.
Key Statistics
- 300,000+ annual hospitalizations
- 2-10% mortality rate
- Higher incidence in elderly patients
- $2.5 billion annual healthcare cost
Nursing Priorities
- Hemodynamic stabilization
- Source identification
- Blood loss monitoring
- Complication prevention
2. Pathophysiology
Understanding the Bleeding Process
GI bleeding occurs when the integrity of the mucosal, submucosal, or vascular structures within the digestive tract is compromised, leading to blood loss into the GI lumen.
Mucosal Injury
Erosion or ulceration of protective mucosal barriers leading to exposed blood vessels
Vascular Rupture
Direct injury to blood vessels from increased pressure, trauma, or vessel wall weakness
Hemostatic Failure
Inadequate clotting mechanisms or anticoagulant effects preventing natural bleeding cessation
Memory Aid: “BLEEDING” Pathophysiology
- Blood vessel injury
- Loss of mucosal integrity
- Erosion of protective barriers
- Elevated gastric acid
- Deficient clotting factors
- Increased portal pressure
- NSAID-induced damage
- Gastric varices rupture
Physiological Response to Blood Loss
↑HR, ↑Contractility
Vasoconstriction
↑ADH, ↑Aldosterone
↑Catecholamines
Platelet aggregation
Clotting cascade
3. Classification & Types
GI bleeding is primarily classified based on anatomical location relative to the ligament of Treitz, which serves as the dividing line between upper and lower GI tract bleeding.
Upper GI Bleeding (UGIB)
Bleeding proximal to the ligament of Treitz
Common Causes:
- Peptic Ulcer Disease (45%) – H. pylori, NSAIDs
- Esophageal Varices (15%) – Portal hypertension
- Mallory-Weiss Tear (5%) – Forceful vomiting
- Boerhaave Syndrome – Full-thickness rupture
- Erosive Esophagitis – GERD, medications
Clinical Presentations:
Vomiting blood
Digested blood
Black, tarry stools
If massive bleeding
Lower GI Bleeding (LGIB)
Bleeding distal to the ligament of Treitz
Common Causes:
- Diverticulosis (40%) – Most common in elderly
- Angiodysplasia (20%) – Vascular malformations
- Colorectal Cancer (10%) – Malignant lesions
- Inflammatory Bowel Disease – UC, Crohn’s
- Hemorrhoids – Internal/external
Clinical Presentations:
Bright red blood
Right-sided bleeding
Chronic, hidden
If right-sided, slow
Memory Aid: “UPPER” vs “LOWER” Causes
- Mallory-Weiss tear
- Oesophageal varices
- Vascular lesions
- Erosions & ulcers
- Diverticulosis
- IBD (Inflammatory Bowel Disease)
- Tumors/Cancer
- Colonic angiodysplasia
- Hemorrhoids
4. Clinical Assessment
Comprehensive nursing assessment is crucial for early detection, risk stratification, and appropriate intervention planning. The assessment must be systematic, thorough, and frequently repeated.
Critical Assessment Priority
Always assess hemodynamic stability FIRST – airway, breathing, circulation. A patient can exsanguinate rapidly with massive GI bleeding.
Primary Assessment (ABCDE Approach)
A – Airway
- • Patent airway
- • Risk of aspiration
- • Hematemesis present?
B – Breathing
- • Respiratory rate
- • Oxygen saturation
- • Signs of distress
C – Circulation
- • Heart rate/rhythm
- • Blood pressure
- • Capillary refill
D – Disability
- • Neurological status
- • Glasgow Coma Scale
- • Confusion/altered LOC
E – Exposure
- • Temperature
- • Skin assessment
- • Other injuries
Hemodynamic Assessment
Class I (Mild)
- • Blood loss: <15%
- • HR: <100 bpm
- • BP: Normal
- • No orthostatic changes
- • Normal mental status
Class II (Moderate)
- • Blood loss: 15-30%
- • HR: 100-120 bpm
- • BP: Orthostatic changes
- • Mild anxiety
- • Delayed capillary refill
Class III-IV (Severe)
- • Blood loss: >30%
- • HR: >120 bpm
- • BP: Hypotensive
- • Altered mental status
- • Oliguria
Focused History
Key Questions to Ask:
- • When did bleeding start?
- • Character of blood/stool?
- • Associated symptoms?
- • Previous GI bleeding episodes?
- • Current medications?
- • Alcohol use history?
- • Recent trauma or procedures?
Red Flag Symptoms:
- • Massive hematemesis
- • Severe abdominal pain
- • Syncope or near-syncope
- • Severe weakness/fatigue
- • Chest pain/dyspnea
- • Altered mental status
- • Signs of shock
Memory Aid: “SHOCK” Assessment
- Skin – pale, cool, clammy
- Heart rate – tachycardia
- Orthostatic vital signs
- Capillary refill – delayed >2 seconds
- Kidney function – oliguria
5. Diagnostic Testing
Diagnostic evaluation of GI bleeding involves a systematic approach combining laboratory studies, imaging, and endoscopic procedures to identify the source, severity, and underlying cause of bleeding.
Laboratory Studies
Immediate Labs (STAT)
- Complete Blood Count (CBC)
• Hemoglobin/Hematocrit (may be normal initially)
• Platelet count
• White blood cell count - Basic Metabolic Panel (BMP)
• BUN/Creatinine ratio >20:1 suggests UGIB
• Electrolyte imbalances - Coagulation Studies
• PT/INR, aPTT
• Assess bleeding risk
Additional Studies
- Type & Crossmatch
• 2-4 units PRBCs for active bleeding
• Type & screen if stable - Liver Function Tests
• AST, ALT, Bilirubin
• Albumin, Total Protein - Special Studies
• H. pylori testing
• Lactate (tissue perfusion)
Clinical Pearl: BUN/Creatinine Ratio
A BUN/Creatinine ratio >20:1 suggests upper GI bleeding due to protein digestion and absorption of blood in the small intestine. This is a valuable early diagnostic clue!
Endoscopic Procedures
Upper Endoscopy (EGD)
Indications:
- • Hematemesis or coffee-ground emesis
- • Melena
- • Suspected UGIB
- • High-risk patients
Timing:
- • Emergent: <12 hours for high-risk
- • Early: <24 hours for stable patients
Colonoscopy
Indications:
- • Hematochezia
- • Suspected LGIB
- • After negative EGD
- • Chronic bleeding
Preparation:
- • Bowel preparation required
- • May be delayed if unstable
Imaging Studies
CT Angiography
- • Active bleeding >0.3 mL/min
- • Non-invasive
- • Guides intervention
- • Shows extravasation
Tagged RBC Scan
- • Detects bleeding >0.1 mL/min
- • Intermittent bleeding
- • Localizes general area
- • Nuclear medicine study
Angiography
- • Therapeutic intervention
- • Embolization possible
- • Active bleeding >0.5 mL/min
- • Invasive procedure
Memory Aid: “TESTS” for GI Bleeding
- Type & Crossmatch blood
- Endoscopy (EGD/Colonoscopy)
- Stool studies (occult blood)
- Tissue perfusion (lactate)
- Scans (CT, tagged RBC)
6. Nursing Interventions
Nursing interventions for GI bleeding focus on hemodynamic stabilization, monitoring for complications, supporting diagnostic procedures, and providing comprehensive patient care throughout the treatment continuum.
Priority Nursing Actions
Time is critical! Establish IV access, monitor vital signs continuously, and prepare for potential emergent interventions while maintaining calm, professional demeanor.
Immediate Interventions
Hemodynamic Stabilization
- IV Access: Two large-bore IVs (18G or larger)
- Fluid Resuscitation: Normal saline or LR as ordered
- Vital Signs: Q15 minutes initially, continuous monitoring
- Oxygen: As needed to maintain SpO2 >95%
- Positioning: Trendelenburg if hypotensive
Monitoring & Assessment
- Neurologic Status: LOC, confusion, agitation
- Orthostatic Vitals: If stable enough
- Urine Output: Foley catheter, goal >0.5 mL/kg/hr
- Skin Assessment: Color, temperature, capillary refill
- Bowel Sounds: Presence and character
Ongoing Nursing Care
Gastrointestinal Care
- • NPO initially
- • NG tube if indicated
- • Monitor gastric output
- • Document stool characteristics
- • Test stools for occult blood
- • Measure abdominal girth
Safety Measures
- • Fall precautions
- • Bed in low position
- • Call light within reach
- • Assist with ambulation
- • Monitor for syncope
- • Side rails up PRN
Psychosocial Support
- • Provide reassurance
- • Explain procedures
- • Family communication
- • Address anxiety
- • Cultural considerations
- • Spiritual support PRN
Blood Product Administration
Transfusion Guidelines
Packed Red Blood Cells (PRBCs)
- • Target Hgb 7-9 g/dL (restrictive strategy)
- • Higher targets for cardiac patients
- • Pre-transfusion vital signs
- • Two-nurse verification
- • Monitor for reactions
Other Products
- • FFP: INR >1.5, active bleeding
- • Platelets: Count <50,000 with bleeding
- • Cryoprecipitate: Fibrinogen <100 mg/dL
- • Factor VIIa: Refractory bleeding
Procedural Support
Endoscopy Preparation
• Consent obtained
• NPO status
• IV access
• Vitals stable
• Monitor vitals
• Assist physician
• Position patient
• Suction PRN
• Recovery position
• Monitor for complications
• Assess gag reflex
• Stable vitals
• No bleeding
• Instructions given
Memory Aid: “STABILIZE” Nursing Actions
- Start large-bore IVs
- Take vital signs frequently
- Assess neurologic status
- Blood products as ordered
- Intake and output monitoring
- Lab values trending
- Immobilize if unstable
- Zero oral intake initially
- Endoscopy preparation
7. Pharmacological Management
Pharmacological interventions play a crucial role in managing GI bleeding by reducing gastric acid production, promoting hemostasis, and treating underlying conditions. Understanding these medications and their nursing implications is essential for safe patient care.
Proton Pump Inhibitors (PPIs)
Common PPIs
- • Omeprazole (Prilosec): 40-80 mg IV/PO daily
- • Pantoprazole (Protonix): 40-80 mg IV daily
- • Esomeprazole (Nexium): 40 mg IV daily
- • Lansoprazole (Prevacid): 30 mg PO daily
Mechanism of Action
Irreversibly binds to H+/K+-ATPase pump, blocking gastric acid secretion for 24-72 hours
Nursing Considerations
- • Administer before meals if PO
- • IV push over 2-5 minutes
- • Monitor for drug interactions
- • Long-term use: B12, Mg monitoring
- • Assess for C. diff risk
- • Monitor bone density with long-term use
Side Effects
- • Headache, diarrhea, nausea
- • Increased infection risk
- • Hypomagnesemia (long-term)
Vasoactive Medications
Octreotide (Sandostatin)
Indication: Esophageal/gastric varices bleeding
Dosing: 50 mcg IV bolus, then 50 mcg/hr infusion
Mechanism: Reduces portal pressure and splanchnic blood flow
Nursing:
- • Monitor blood glucose (can cause hypoglycemia)
- • Assess for bradycardia
- • Give via central line preferred
- • Monitor for gallbladder complications
Vasopressin (Pitressin)
Indication: Variceal bleeding (less commonly used)
Dosing: 0.3-0.4 units/min IV infusion
Mechanism: Causes splanchnic vasoconstriction
Nursing:
- • Monitor for cardiac arrhythmias
- • Assess for chest pain/MI
- • Check electrolytes (hyponatremia)
- • Often given with nitroglycerin
Hemostatic Agents
Vitamin K
- • Dose: 10 mg IV/SQ
- • Use: Warfarin reversal
- • Onset: 6-12 hours
- • Monitor: PT/INR
Prothrombin Complex
- • Dose: Weight-based
- • Use: Rapid reversal
- • Onset: Minutes
- • Risk: Thrombosis
Tranexamic Acid
- • Dose: 1g IV q8h
- • Use: Antifibrinolytic
- • Caution: Seizure risk
- • Monitor: Neuro status
H2 Receptor Antagonists
Common H2 Blockers
- • Ranitidine: Withdrawn from market
- • Famotidine (Pepcid): 20-40 mg IV/PO BID
- • Cimetidine (Tagamet): 300 mg IV q6h
Note: Less effective than PPIs for acute bleeding
Nursing Considerations
- • Dose reduction in renal impairment
- • Monitor for drug interactions (especially cimetidine)
- • Less potent acid suppression than PPIs
- • May be used as step-down therapy
Medications to Avoid or Use Cautiously
High-Risk Medications
Absolutely Avoid:
- • NSAIDs (ibuprofen, naproxen)
- • Aspirin (unless cardioprotective dose needed)
- • Bisphosphonates
- • Iron supplements (can cause GI irritation)
Use with Extreme Caution:
- • Anticoagulants (warfarin, heparin)
- • Antiplatelet agents (clopidogrel)
- • Corticosteroids
- • SSRIs (bleeding risk)
Memory Aid: “ACID STOP” Medication Management
- Avoid NSAIDs and aspirin
- Check anticoagulation status
- IV PPI first-line therapy
- Dose adjust for renal function
- Splanchnic flow reduction (octreotide)
- Tranexamic acid for severe bleeding
- Octreotide for variceal bleeding
- Prothrombotic agents PRN
8. Complications
GI bleeding can lead to numerous serious complications that require prompt recognition and intervention. Understanding these potential complications enables nurses to provide proactive monitoring and early intervention to improve patient outcomes.
Life-Threatening Complications
Hypovolemic shock, exsanguination, and aspiration pneumonia represent the most immediate threats to patient survival and require aggressive intervention.
Immediate Complications
Hypovolemic Shock
Pathophysiology: Rapid blood loss → decreased preload → reduced cardiac output
Signs & Symptoms:
- • Tachycardia >100 bpm
- • Hypotension <90 mmHg systolic
- • Cool, clammy skin
- • Altered mental status
- • Oliguria <0.5 mL/kg/hr
- • Weak, thready pulse
Nursing Interventions:
- • Aggressive fluid resuscitation
- • Blood product administration
- • Continuous hemodynamic monitoring
- • Prepare for ICU transfer
Aspiration Pneumonia
Risk Factors: Hematemesis, altered LOC, supine positioning
Prevention:
- • Position patient on side if vomiting
- • Suction airway PRN
- • Keep HOB elevated when stable
- • Monitor respiratory status closely
Signs of Aspiration:
- • Coughing, choking during vomiting
- • Decreased oxygen saturation
- • Adventitious lung sounds
- • Fever, leukocytosis
Rebleeding
Risk Factors
- • Large ulcer size (>2 cm)
- • Active bleeding at endoscopy
- • Visible vessel or adherent clot
- • Hemodynamic instability
- • Advanced age
- • Comorbidities (cirrhosis, CKD)
- • Continued anticoagulation
Prevention Strategies
- • High-dose PPI therapy
- • Avoid NSAIDs and anticoagulants
- • Endoscopic therapy as indicated
- • Serial monitoring of Hgb/Hct
- • Blood pressure control
- • Treat underlying conditions
Organ System Complications
Cardiac Complications
- • Myocardial Infarction: Demand ischemia from anemia
- • Arrhythmias: Electrolyte imbalances
- • Heart Failure: Volume overload from resuscitation
- • Monitoring: Continuous telemetry, serial ECGs, troponins
Renal Complications
- • Acute Kidney Injury: Hypoperfusion, contrast exposure
- • Prerenal Azotemia: Volume depletion
- • Monitoring: Urine output, BUN/Cr, electrolytes
- • Prevention: Adequate perfusion, avoid nephrotoxins
Neurologic Complications
- • Cerebral Hypoxia: Severe anemia, hypotension
- • Stroke: Hypoperfusion, hypercoagulable state
- • Delirium: ICU stay, medications, illness
- • Assessment: Frequent neuro checks, cognition screening
Long-term Complications
Chronic Iron Deficiency Anemia
- • Fatigue, weakness, dyspnea on exertion
- • Restless leg syndrome, pica
- • Reduced exercise tolerance
- • Treatment: Iron replacement, dietary counseling
Transfusion-Related Complications
- • Iron overload (multiple transfusions)
- • Alloimmunization
- • Transfusion-transmitted infections
- • Transfusion-associated circulatory overload
Psychological Impact
- • Anxiety about recurrent bleeding
- • Depression from chronic illness
- • Fear of medical procedures
- • Impact on quality of life
Economic Burden
- • Recurrent hospitalizations
- • Loss of work productivity
- • Long-term medication costs
- • Follow-up care requirements
Clinical Pearl: Early Recognition
The key to preventing serious complications is early recognition of clinical deterioration. Trends in vital signs, laboratory values, and patient appearance are more important than single abnormal values.
Memory Aid: “COMPLICATIONS” Monitoring
- Cardiac status (MI risk)
- Oxygen saturation (aspiration)
- Mental status changes
- Pulmonary edema risk
- Liver function (in cirrhosis)
- Infection risk
- Coagulation abnormalities
- Acute kidney injury
- Thromboembolism risk
- Iron deficiency anemia
- Organ hypoperfusion
- Neurologic changes
- Shock development
9. Patient Education
Comprehensive patient education is essential for preventing recurrent GI bleeding, promoting medication adherence, and ensuring patients recognize warning signs that require immediate medical attention. Education should be tailored to the patient’s underlying condition and risk factors.
Education Principle
Use teach-back method to ensure understanding. Ask patients to repeat key information in their own words, and provide written materials in appropriate language and literacy level.
Warning Signs to Report Immediately
🚨 CALL 911 or GO TO ER IMMEDIATELY IF YOU EXPERIENCE: 🚨
Bleeding Signs:
- • Vomiting blood or coffee-ground material
- • Black, tarry, or bloody stools
- • Large amount of bright red blood in stool
- • Sudden increase in bleeding
Serious Symptoms:
- • Dizziness, fainting, or feeling faint
- • Severe weakness or confusion
- • Rapid heartbeat or chest pain
- • Difficulty breathing
Medication Management
PPI Therapy Education
- Timing: Take 30-60 minutes before first meal of the day
- Consistency: Take at the same time daily, even if you feel better
- Duration: Continue for prescribed length (often 8-12 weeks)
- Don’t Stop: Without consulting your healthcare provider
- Swallow Whole: Don’t crush or chew delayed-release capsules
Medications to Avoid
- NSAIDs: Ibuprofen, naproxen, aspirin (unless prescribed)
- Blood Thinners: Only as prescribed by your doctor
- Herbal Supplements: Ginkgo, garlic, ginseng (increase bleeding risk)
- Check First: Ask pharmacist about over-the-counter medications
- Keep List: Carry list of all medications and allergies
Lifestyle Modifications
Dietary Guidelines
- • Eat smaller, more frequent meals
- • Avoid spicy, acidic foods if they cause symptoms
- • Limit caffeine and carbonated beverages
- • Stay well-hydrated
- • Iron-rich foods if anemic
- • Avoid very hot foods/drinks
Alcohol & Smoking
- • Alcohol: Avoid or strictly limit
- • Increases stomach acid production
- • Interferes with healing
- • Smoking: Quit completely
- • Delays ulcer healing
- • Increases bleeding risk
Stress Management
- • Practice relaxation techniques
- • Regular exercise as tolerated
- • Adequate sleep (7-8 hours)
- • Stress reduction activities
- • Consider counseling if needed
- • Support groups available
Follow-up Care
Scheduled Appointments
- • Keep all follow-up appointments
- • Primary care provider within 1-2 weeks
- • Gastroenterologist as scheduled
- • Blood work to monitor hemoglobin
- • Repeat endoscopy if recommended
- • Bring medication list to all appointments
Monitoring at Home
- • Monitor stool color and consistency daily
- • Watch for signs of anemia (fatigue, weakness)
- • Track symptoms in a diary
- • Monitor weight if instructed
- • Check blood pressure if hypertensive
- • Report any concerns promptly
Special Populations
Elderly Patients
- • Higher risk for complications
- • May need assistance with medications
- • Fall risk due to anemia/weakness
- • Ensure caregiver understands instructions
- • Consider medication organization systems
- • Home safety evaluation may be needed
Patients with Cirrhosis
- • Strict alcohol avoidance essential
- • Monitor for signs of liver decompensation
- • Regular screening endoscopy needed
- • Dietary restrictions (sodium, protein)
- • Medication compliance crucial
- • Vaccination updates (hepatitis A/B, pneumonia)
Memory Aid: “EDUCATE” Patient Teaching
- Emergency signs to report
- Drug interactions to avoid
- Understand medication timing
- Compliance with follow-up
- Alcohol and smoking cessation
- Teach-back method verification
- Encourage questions and concerns
10. Summary & Review
GI bleeding disorders represent a critical area of nursing practice requiring comprehensive knowledge, skilled assessment, and rapid intervention. This summary consolidates key concepts for clinical application and examination preparation.
Key Takeaways
Assessment Priorities
- • Hemodynamic stability assessment first (ABCDE)
- • Location of bleeding determines presentation
- • Upper GI: hematemesis, melena, coffee-ground emesis
- • Lower GI: hematochezia, maroon stools
- • BUN/Creatinine ratio >20:1 suggests upper GI source
- • Orthostatic vitals indicate significant volume loss
Nursing Interventions
- • Two large-bore IVs for fluid resuscitation
- • Frequent vital sign monitoring
- • NPO initially, monitor I&O
- • Blood product administration as ordered
- • Fall precautions due to weakness/anemia
- • Endoscopy preparation and support
Clinical Decision-Making Framework
• Hemodynamic status
• Bleeding severity
• Source location
• IV access
• Fluid resuscitation
• Blood products
• Laboratory studies
• Endoscopy
• Imaging PRN
• Treat underlying cause
• Prevent complications
• Patient education
Common Causes by Location
Upper GI Bleeding (45% of cases)
- 1. Peptic Ulcer Disease (45%) – H. pylori, NSAIDs
- 2. Esophageal Varices (15%) – Portal hypertension
- 3. Mallory-Weiss Tear (5%) – Forceful vomiting
- 4. Erosive Esophagitis – GERD, medications
- 5. Boerhaave Syndrome – Full thickness rupture
Lower GI Bleeding (55% of cases)
- 1. Diverticulosis (40%) – Most common in elderly
- 2. Angiodysplasia (20%) – Vascular malformations
- 3. Colorectal Cancer (10%) – Malignant lesions
- 4. Inflammatory Bowel Disease – UC, Crohn’s
- 5. Hemorrhoids – Internal/external
Medication Pearls
First-Line Therapy
- • PPIs: Pantoprazole 40-80 mg IV daily
- • Most effective acid suppression
- • Promotes ulcer healing
- • Continue 6-8 weeks minimum
Variceal Bleeding
- • Octreotide: 50 mcg bolus + infusion
- • Reduces portal pressure
- • Monitor blood glucose
- • Give with endoscopic therapy
Avoid/Caution
- • NSAIDs: Absolutely contraindicated
- • Anticoagulants: Hold if bleeding
- • Aspirin: Only if cardioprotective
- • Iron: May cause GI irritation
Critical Complications to Monitor
Immediate (Hours)
- • Hypovolemic shock – Most dangerous
- • Aspiration pneumonia – Hematemesis risk
- • Cardiac ischemia – Demand from anemia
- • Rebleeding – 20% within 72 hours
Later (Days-Weeks)
- • Iron deficiency anemia – Chronic bleeding
- • Acute kidney injury – Hypoperfusion
- • Transfusion complications – Multiple units
- • Thromboembolism – Immobilization
Patient Education Essentials
Red Flag Symptoms
- • Vomiting blood or coffee-ground material
- • Black, tarry stools (melena)
- • Bright red blood in stool
- • Dizziness, fainting, weakness
- • Chest pain, shortness of breath
Lifestyle Modifications
- • Take PPIs as prescribed (before meals)
- • Avoid NSAIDs completely
- • No alcohol or smoking
- • Keep follow-up appointments
- • Carry medication list
Master Mnemonic: “GI BLEEDING CARE”
- Get IV access (large bore x2)
- Immediately assess hemodynamics
- Blood products as ordered
- Lab studies (CBC, coags, type & cross)
- Endoscopy preparation
- Educate patient on warning signs
- Document stool characteristics
- Input/output monitoring
- NPO initially
- Give PPIs as prescribed
- Complications monitoring
- Avoid NSAIDs
- Rebleeding surveillance
- Early mobilization when stable
🎯 Nursing Excellence in GI Bleeding Care
Excellence in nursing care for GI bleeding patients combines rapid assessment skills, evidence-based interventions, vigilant monitoring, and compassionate patient education.
Remember: Your prompt recognition and skilled intervention can be life-saving for patients with GI bleeding. Stay vigilant, stay informed, and never hesitate to escalate concerns!
