Comprehensive Nursing Notes: Hernias
Complete Guide for Nursing Students
Introduction to Hernias
A hernia represents one of the most common surgical conditions encountered in clinical practice, affecting millions of individuals worldwide. As nursing professionals, understanding the complex pathophysiology, diverse presentations, and comprehensive care requirements for patients with hernias is essential for providing optimal outcomes and preventing complications.
Key Learning Objectives
- Understand the pathophysiology of hernia formation
- Identify different types of hernias and their characteristics
- Recognize clinical signs and symptoms
- Implement evidence-based nursing interventions
- Develop comprehensive patient education strategies
The term “hernia” originates from the Latin word meaning “rupture” or “tear,” which accurately describes the fundamental mechanism underlying this condition. A hernia occurs when an organ or tissue protrudes through a weakened area in the muscle or connective tissue that normally contains it. This anatomical disruption can occur at various locations throughout the body, with each type presenting unique challenges for nursing assessment and management.
Anatomy & Pathophysiology
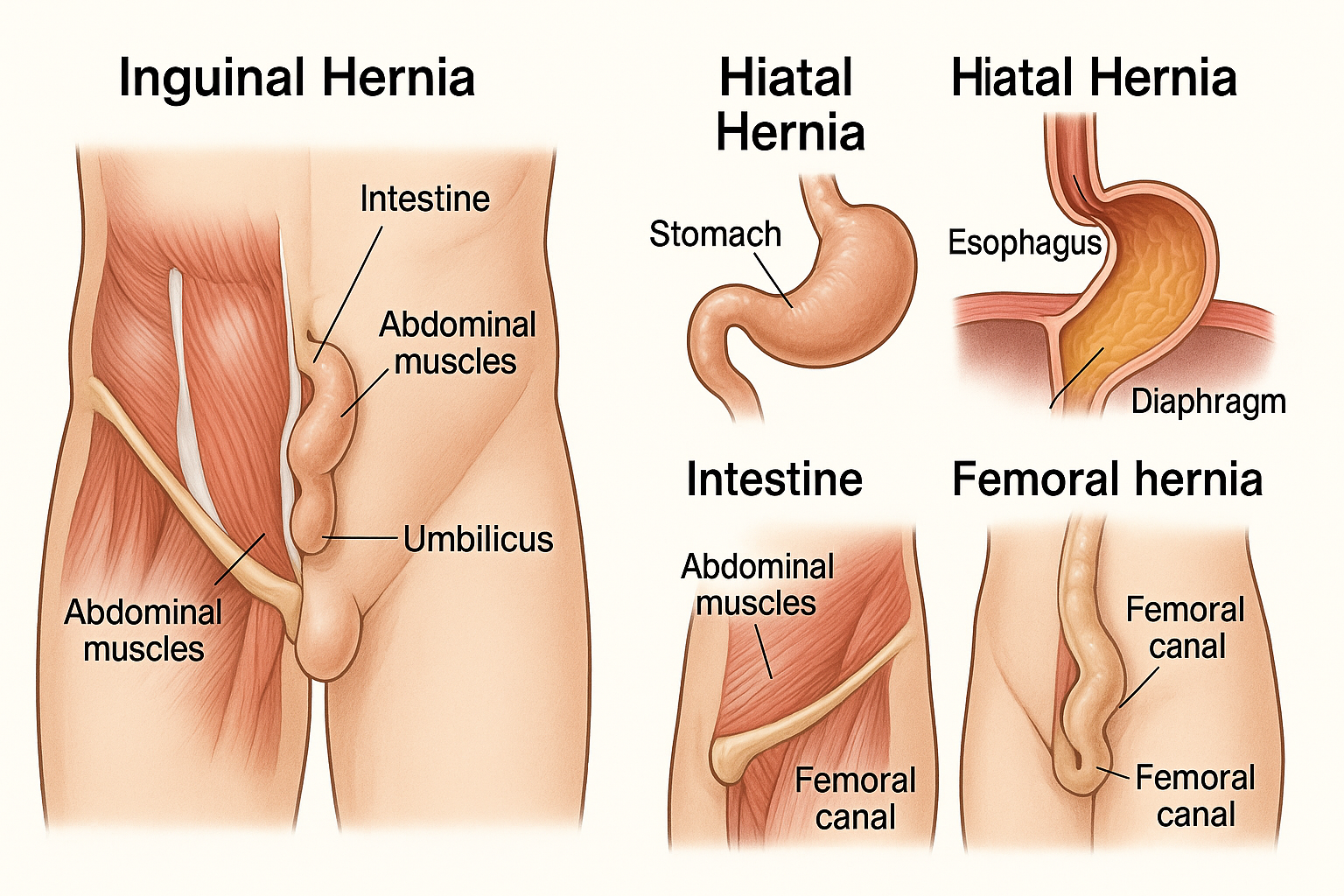
Anatomical illustration showing different types of hernias
Normal Anatomy
- Fascial layers: Provide structural support
- Muscle fibers: Maintain tissue integrity
- Connective tissue: Binds structures together
- Natural openings: Allow passage of vessels and nerves
Pathophysiology Mnemonic
WEAK SPOT
- Wall defect develops
- Elevated pressure
- Anatomy compromised
- Keeps expanding
- Sac formation
- Protrusion occurs
- Organ displacement
- Tissue weakness
Mechanisms of Hernia Formation
The development of a hernia involves a complex interplay of factors that compromise the structural integrity of the abdominal wall or other anatomical barriers. Understanding these mechanisms is crucial for nursing professionals to identify risk factors and implement preventive strategies.
Primary Contributing Factors
Increased Intra-abdominal Pressure:
- • Chronic coughing
- • Heavy lifting
- • Straining during bowel movements
- • Pregnancy
- • Obesity
Tissue Weakness:
- • Age-related collagen degradation
- • Genetic predisposition
- • Previous surgical incisions
- • Connective tissue disorders
- • Malnutrition
Types of Hernias
Inguinal Hernia
Most common type (75-80%)
- • More common in males
- • Groin area protrusion
- • May extend into scrotum
- • Direct vs. indirect subtypes
Femoral Hernia
Higher risk in females
- • Below inguinal ligament
- • High strangulation risk
- • Often requires urgent surgery
- • Less common than inguinal
Umbilical Hernia
Common in infants and adults
- • Naval area protrusion
- • Often self-resolves in children
- • Associated with pregnancy/obesity
- • May become incarcerated
Incisional Hernia
Post-surgical complication
- • Occurs at surgical sites
- • Wound healing complications
- • Risk factors: infection, obesity
- • May require mesh repair
Hiatal Hernia
Upper GI involvement
- • Stomach protrudes through diaphragm
- • Sliding vs. paraesophageal
- • GERD symptoms common
- • May cause respiratory issues
Epigastric Hernia
Upper abdominal wall
- • Between xiphoid and umbilicus
- • Often contains fat only
- • May be multiple
- • Can cause epigastric pain
Hernia Type Comparison
| Type | Location | Demographics | Strangulation Risk | Treatment Priority |
|---|---|---|---|---|
| Inguinal | Groin/inguinal canal | Males 85%, all ages | Moderate (2-3%) | Elective |
| Femoral | Femoral canal | Females 70%, elderly | High (15-20%) | Urgent |
| Umbilical | Umbilical ring | Infants, obese adults | Low-Moderate | Elective |
| Incisional | Previous surgical site | Post-surgery patients | Variable | Case-dependent |
| Hiatal | Esophageal hiatus | Adults >50, females | High (Type II) | Symptom-based |
Clinical Presentation & Signs
Visual Signs
-
Visible bulge or protrusion: Most obvious sign, may be intermittent or constant
-
Asymmetry: Comparison between affected and unaffected sides
-
Skin changes: Discoloration, thinning, or stretching over hernia site
-
Size variation: Changes with position, coughing, or straining
Palpation Findings
-
Palpable mass: Soft, reducible, or firm and fixed
-
Cough impulse: Positive cough test indicates hernia
-
Reducibility: Can contents be pushed back manually?
-
Temperature changes: Warmth may indicate inflammation
Assessment Mnemonic: HERNIA
- H – History of symptoms
- E – Examine for bulge
- R – Reducibility test
- N – Note size and location
- I – Impulse on coughing
- A – Associated symptoms
Red Flag Symptoms – Immediate Medical Attention Required
Strangulation Signs:
- • Severe, constant pain
- • Inability to reduce hernia
- • Nausea and vomiting
- • Fever and systemic illness
Incarceration Signs:
- • Non-reducible hernia
- • Increasing pain
- • Bowel obstruction symptoms
- • Abdominal distension
Assessment & Diagnosis
History Taking
- • Duration of symptoms
- • Pain characteristics
- • Aggravating factors
- • Previous hernia repairs
- • Family history
- • Occupational factors
Physical Exam
- • Inspection in standing/lying positions
- • Palpation techniques
- • Valsalva maneuver
- • Cough test
- • Percussion and auscultation
- • Bilateral comparison
Diagnostic Tests
- • Ultrasound imaging
- • CT scan (complex cases)
- • MRI (sports hernias)
- • Contrast studies
- • Laboratory tests (if complications)
- • Endoscopy (hiatal hernias)
Nursing Assessment Priority Matrix
| Assessment Area | Priority Level | Key Indicators | Nursing Actions |
|---|---|---|---|
| Pain Assessment | HIGH | Severity, location, character, timing | Pain scale, positioning, analgesics |
| Reducibility | HIGH | Can hernia be pushed back? | Gentle reduction attempts, positioning |
| GI Function | MEDIUM | Bowel sounds, nausea, vomiting | NPO if indicated, IV fluids |
| Mobility | LOW | Activity tolerance, limitations | Activity modification, support |
Nursing Diagnostic Considerations
Primary Nursing Diagnoses:
- • Acute pain related to hernia protrusion
- • Risk for injury related to strangulation
- • Impaired physical mobility
- • Anxiety related to surgical intervention
Secondary Considerations:
- • Risk for infection (post-operative)
- • Deficient knowledge about condition
- • Ineffective coping mechanisms
- • Risk for constipation
Nursing Interventions & Management
Pre-operative Care
-
Pain Management: Position patient for comfort, administer prescribed analgesics, use non-pharmacological methods
-
Patient Education: Explain procedure, risks, benefits, and post-operative expectations
-
Physical Preparation: NPO status, bowel preparation if indicated, surgical site preparation
-
Psychological Support: Address anxiety, provide emotional support, involve family
Post-operative Care
-
Wound Assessment: Monitor for signs of infection, bleeding, or dehiscence
-
Pain Control: Multi-modal pain management, positioning, ice therapy
-
Early Mobilization: Progressive activity as tolerated, prevent complications
-
Discharge Planning: Activity restrictions, follow-up appointments, home care instructions
Post-op Monitoring Mnemonic: REPAIR
- R – Respiratory status
- E – Elimination patterns
- P – Pain assessment
- A – Activity tolerance
- I – Incision assessment
- R – Return of bowel function
Conservative Management (Non-surgical Cases)
Lifestyle Modifications:
- • Weight reduction programs
- • Smoking cessation
- • Constipation prevention
- • Proper lifting techniques
Symptom Management:
- • Supportive garments
- • Activity modification
- • Pain management
- • Regular monitoring
Monitoring Parameters:
- • Size changes
- • Pain patterns
- • Functional limitations
- • Complication signs
Evidence-Based Nursing Interventions
| Intervention | Rationale | Expected Outcome | Evidence Level |
|---|---|---|---|
| Early mobilization post-op | Prevents complications, promotes healing | Reduced hospital stay, faster recovery | High |
| Multi-modal pain management | Reduces opioid requirements, better pain control | Improved patient satisfaction, fewer side effects | High |
| Structured patient education | Improves compliance, reduces complications | Better self-care, reduced readmissions | Moderate |
| Surgical site infection prevention | Reduces infection risk, promotes healing | Lower infection rates, faster recovery | High |
Patient Education & Self-Care
Pre-operative Education
- Procedure Explanation: Simple, understandable terms about the surgical process
- Preparation Instructions: NPO guidelines, medication management, pre-operative hygiene
- Expected Outcomes: Recovery timeline, pain expectations, activity restrictions
- Risk Factors: Potential complications, when to seek immediate help
- Support System: Importance of family involvement, transportation arrangements
Post-operative Education
- Wound Care: Proper cleaning techniques, dressing changes, signs of infection
- Activity Guidelines: Progressive increase in activity, lifting restrictions
- Pain Management: Medication schedule, non-pharmacological methods
- Diet Recommendations: High-fiber foods, adequate hydration, gradual resumption
- Follow-up Care: Appointment schedules, monitoring requirements
Patient Education Mnemonic: TEACH
T
Target specific learning needs
E
Explain in simple terms
A
Ask about understanding
C
Clarify misconceptions
H
Help with demonstration
Critical Teaching Points
When to Seek Immediate Medical Attention:
- • Severe, increasing pain at hernia site
- • Signs of wound infection (redness, warmth, discharge)
- • Fever above 101°F (38.3°C)
- • Nausea and vomiting
- • Inability to pass gas or have bowel movement
- • Hernia becomes hard and cannot be pushed back
Prevention Strategies:
- • Maintain healthy body weight
- • Use proper lifting techniques
- • Strengthen core muscles gradually
- • Treat chronic cough promptly
- • Prevent constipation
- • Avoid excessive straining
Activity Progression Guidelines
| Time Period | Allowed Activities | Restrictions | Goals |
|---|---|---|---|
| 0-1 Week | Walking, light ADLs, gentle movement | No lifting >10 lbs, no driving | Pain control, wound healing |
| 1-2 Weeks | Increased walking, return to desk work | No lifting >15 lbs, limited bending | Improved mobility, reduced pain |
| 2-4 Weeks | Light exercise, driving, most work | No lifting >25 lbs, no straining | Return to normal activities |
| 4-6 Weeks | Full activities, exercise progression | Gradual return to heavy lifting | Complete recovery |
Complications & Emergency Management
Strangulation (Medical Emergency)
Definition:
Blood supply to herniated tissue is compromised, leading to ischemia and potential necrosis.
Clinical Signs:
- • Severe, constant pain
- • Hard, tender, non-reducible mass
- • Nausea and vomiting
- • Systemic signs of toxicity
- • Absence of bowel sounds
Nursing Actions:
- • Immediate physician notification
- • NPO status
- • IV access and fluid resuscitation
- • Pain management
- • Prepare for emergency surgery
Incarceration (Urgent)
Definition:
Hernia contents become trapped and cannot be reduced back into the abdominal cavity.
Clinical Signs:
- • Non-reducible hernia
- • Increasing discomfort
- • Possible bowel obstruction
- • Abdominal distension
- • Altered bowel patterns
Nursing Actions:
- • Assess for strangulation signs
- • Position for comfort
- • Monitor vital signs
- • Document changes
- • Prepare for possible surgery
Emergency Assessment Mnemonic: DANGER
- D – Discoloration of hernia
- A – Abdominal distension
- N – Non-reducible mass
- G – GI symptoms (N&V)
- E – Extreme pain
- R – Rigid abdomen
Post-operative Complications
| Complication | Incidence | Signs & Symptoms | Prevention/Management |
|---|---|---|---|
| Surgical Site Infection | 2-5% | Redness, warmth, discharge, fever | Sterile technique, antibiotics, wound care |
| Chronic Pain | 5-10% | Persistent pain >3 months | Proper technique, nerve preservation |
| Recurrence | 1-15% | Return of hernia at same site | Proper repair, lifestyle modifications |
| Seroma/Hematoma | 3-7% | Fluid collection, swelling | Drainage, compression, monitoring |
Emergency Protocol Checklist
Immediate Actions (0-5 minutes):
- Assess ABCs (Airway, Breathing, Circulation)
- Obtain vital signs
- Assess pain level (0-10 scale)
- Examine hernia for reducibility
- Notify physician immediately
Follow-up Actions (5-15 minutes):
- Establish IV access
- Make patient NPO
- Position for comfort
- Prepare for OR if indicated
- Document all assessments
Global Best Practices & Innovations
Denmark: Hernia Database
World’s largest hernia registry tracking outcomes since 1998.
- • >400,000 operations recorded
- • Quality improvement initiatives
- • Evidence-based guidelines
- • Reduced recurrence rates to <2%
Netherlands: Day Surgery Model
95% of hernia repairs performed as outpatient procedures.
- • Comprehensive pre-operative screening
- • Standardized protocols
- • Enhanced recovery programs
- • Cost-effective care delivery
Germany: Innovation Centers
Leading development in minimally invasive techniques.
- • TEP and TAPP procedures
- • Robotic-assisted surgery
- • Advanced mesh technologies
- • Reduced post-operative pain
Emerging Technologies & Practices
Surgical Innovations:
- Biological Meshes: Reduced foreign body reaction, better integration
- Self-Gripping Meshes: Tack-free fixation reduces chronic pain
- 3D Printing: Patient-specific mesh designs
- Robotic Surgery: Enhanced precision, reduced invasiveness
Care Innovations:
- Telemedicine: Remote monitoring and follow-up
- Mobile Apps: Patient education and symptom tracking
- ERAS Protocols: Enhanced Recovery After Surgery programs
- Predictive Analytics: Risk stratification and personalized care
Evidence-Based Practice Recommendations
International Guidelines (EHS/AHS):
- • Routine antibiotic prophylaxis not recommended
- • Local anesthesia preferred for inguinal repairs
- • Mesh repair recommended for most adult hernias
- • Early mobilization improves outcomes
Nursing Best Practices:
- • Standardized assessment protocols
- • Multi-modal pain management
- • Structured patient education programs
- • Quality improvement initiatives
Conclusion & Additional Resources
Comprehensive understanding of hernia pathophysiology, assessment, and management is essential for nursing professionals to provide optimal patient care. The complexity of hernia presentations requires a systematic approach to assessment, evidence-based interventions, and thorough patient education to achieve the best possible outcomes.
As healthcare continues to evolve, nursing professionals must stay current with emerging technologies, best practices, and evidence-based guidelines. The integration of global best practices, innovative technologies, and patient-centered care approaches will continue to improve hernia management outcomes and patient satisfaction.
Key Takeaways
- • Early recognition prevents complications
- • Evidence-based interventions improve outcomes
- • Patient education reduces recurrence rates
- • Multidisciplinary approach enhances care quality
- • Continuous learning ensures best practices
Continuing Education
- • Subscribe to surgical nursing journals
- • Attend hernia-focused conferences
- • Participate in quality improvement initiatives
- • Engage in evidence-based practice projects
- • Network with hernia specialty centers
Additional Learning Resources
| Resource Type | Organization | Focus Area | Access Level |
|---|---|---|---|
| Guidelines | European Hernia Society | Clinical practice guidelines | Free |
| Journal | Hernia Journal | Research and case studies | Subscription |
| Database | Danish Hernia Database | Outcome data and trends | Free |
| Education | American Hernia Society | Professional development | Membership |
