Investigations for Mentally Ill Patients
A Comprehensive Guide to Blood Chemistry, EEG, CT & MRI
Introduction
The assessment and management of mentally ill patients often requires a comprehensive approach that includes various diagnostic investigations. These investigations help clinicians to rule out organic causes of psychiatric symptoms, monitor medication effects and side effects, and understand the neurobiological basis of mental disorders.
The brain and body do not exist in isolation – mental health affects physical health and vice versa. Having a complete picture of both neurological and systemic function is essential for providing optimal care for patients with psychiatric disorders.
Why Investigations Matter in Psychiatry
Despite the historical separation between psychiatry and other medical specialties, modern psychiatric practice recognizes that:
- Many physical conditions can manifest with psychiatric symptoms
- Psychiatric medications can affect multiple body systems requiring monitoring
- Mental disorders have neurobiological correlates that can be observed through brain imaging
- Comorbid medical conditions are common in psychiatric populations
This guide focuses on four key investigative modalities:
Blood Chemistry Tests
Laboratory tests that analyze various components in blood to assess general health, identify medical conditions that may mimic psychiatric disorders, and monitor medication effects.
Electroencephalography (EEG)
A non-invasive method that records electrical activity of the brain to detect abnormalities in brain function, which can be relevant in various psychiatric conditions.
Computed Tomography (CT)
An imaging technique that uses X-rays to produce detailed images of the brain, helping to rule out structural abnormalities that might contribute to psychiatric symptoms.
Magnetic Resonance Imaging (MRI)
An advanced imaging modality that provides detailed structural and functional information about the brain without using radiation.
Blood Chemistry Tests
Blood tests are essential components of the psychiatric evaluation, helping clinicians to rule out medical causes of psychiatric symptoms, establish baseline health parameters before starting medications, and monitor for medication effects and side effects.
Basic Blood Tests in Psychiatric Assessment
| Test Category | Specific Tests | Clinical Relevance |
|---|---|---|
| Complete Blood Count (CBC) | Hemoglobin, WBC, RBC, platelets, hematocrit | Anemia (can cause fatigue, depression), infection, inflammation |
| Basic Metabolic Panel | Sodium, potassium, chloride, BUN, creatinine, glucose | Electrolyte imbalances, kidney function, diabetes (can all affect mental status) |
| Comprehensive Metabolic Panel | Basic panel plus liver enzymes (AST, ALT, ALP) | Adds liver function assessment (important for medication metabolism) |
| Thyroid Function Tests | TSH, Free T4, Free T3 | Hypothyroidism (depression, cognitive slowing), hyperthyroidism (anxiety, insomnia) |
| Lipid Panel | Total cholesterol, LDL, HDL, triglycerides | Monitoring for metabolic effects of second-generation antipsychotics |
| Hemoglobin A1c | Glycated hemoglobin | Screening for diabetes/prediabetes, especially with atypical antipsychotics |
B – Blood count (CBC)
A – A1c (Hemoglobin A1c)
S – Sodium & other electrolytes
I – Iron studies (if anemia suspected)
C – Creatinine (kidney function)
M – Metabolic panels
E – Enzymes (liver)
D – Drug levels (when applicable)
Specialized Blood Tests
Medication Monitoring
- Lithium levels: Therapeutic range 0.6-1.2 mEq/L; requires regular monitoring due to narrow therapeutic window
- Valproic acid levels: For mood stabilization; therapeutic range 50-100 µg/mL
- Carbamazepine levels: For mood stabilization; therapeutic range 4-12 µg/mL
- Clozapine levels: Can guide dosing of this atypical antipsychotic, especially in partial responders
Substance Use Screening
- Urine drug screen: Detects common substances of abuse
- Blood alcohol level: Quantifies alcohol consumption
- Liver function tests: May indicate alcohol-related liver damage
Emerging Biomarkers
- C-reactive protein (CRP): Marker of inflammation, may predict antidepressant response
- Genetic testing: Pharmacogenomics to guide medication selection based on metabolism
- MindX Blood Tests: RNA sequencing to assess, predict, or manage mood disorders
Additional Tests Based on Presentation
- Vitamin B12 & Folate: Deficiencies associated with depression, psychosis
- Vitamin D: Low levels linked to depression, especially seasonal
- Prolactin: May be elevated by antipsychotic medications
- Cortisol: Abnormal in some patients with major depression
Specialized tests should be ordered based on clinical suspicion and history, not as a routine battery. Consider them when:
- Standard treatments are not effective
- Presentation is atypical or suggests medical etiology
- Monitoring specific medication effects or side effects
- Evaluating potential medication interactions
Interpretation & Clinical Significance
Interpreting blood test results requires context and clinical correlation. Abnormalities may represent:
Medical Causes of Psychiatric Symptoms
- Thyroid disorders: Hypothyroidism mimicking depression; hyperthyroidism resembling anxiety
- Anemia: Fatigue, cognitive symptoms, depression
- Electrolyte imbalances: Confusion, altered mental status, mood changes
- B12 deficiency: Depression, psychosis, cognitive impairment
- Hepatic or renal impairment: Encephalopathy, cognitive changes
Medication Effects and Side Effects
- Metabolic changes: Elevated glucose, lipids with second-generation antipsychotics
- Hematologic effects: Leukopenia with clozapine, agranulocytosis (rare)
- Hepatic effects: Elevated liver enzymes with valproic acid, carbamazepine
- Renal effects: Lithium-induced nephropathy with long-term use
- Endocrine effects: Hypothyroidism with lithium; hyperprolactinemia with some antipsychotics

Figure 1: Blood tests for mental health assessment
T – Thyroid disorders (hypo/hyperthyroidism)
H – Hematologic issues (anemia, B12 deficiency)
I – Infection (systemic, encephalitis)
N – Nutritional deficiencies (B vitamins, folate)
K – Kidney function abnormalities
M – Metabolic disturbances (glucose, electrolytes)
E – Endocrine disorders (adrenal, pituitary)
D – Drugs/toxins (prescription, illicit, alcohol)
Electroencephalography (EEG)
Electroencephalography (EEG) is a non-invasive technique that records the electrical activity of the brain through electrodes placed on the scalp. While primarily used in neurology for diagnosing epilepsy, EEG has important applications in psychiatry for examining brain function in various mental disorders.
Basics & Electrode Placement
EEG measures electrical potentials generated by neurons within the cerebral cortex, with signals primarily originating from pyramidal cells. The standard electrode placement follows the International 10-20 System, which ensures consistent electrode positioning across patients.

Figure 2: International 10-20 System for EEG electrode placement
Key Components of EEG Recording
- Electrodes: Typically 21 recording electrodes plus ground and reference
- Montages: Specific arrangements of electrode pairs for viewing the data
- Filters: Remove unwanted signals and artifacts
- Time base: Usually 30mm/second
- Sensitivity: Typically 7μV/mm
Types of EEG Recording
- Routine EEG: 20-40 minutes, includes resting state, hyperventilation, photic stimulation
- Sleep-deprived EEG: Performed after sleep deprivation to increase sensitivity
- Ambulatory EEG: 24-72 hour monitoring
- Video EEG: Synchronized video and EEG recording
- Quantitative EEG (QEEG): Computerized analysis of EEG data
EEG is indicated in patients with:
- New-onset psychosis to rule out seizure disorders
- Rapid changes in mood or behavior that might suggest organic etiology
- Fluctuating or progressive cognitive impairment
- Suspected delirium or encephalopathy
- Treatment-resistant depression or psychosis
- First-episode catatonia
Brain Wave Patterns
EEG activity is classified by frequency bands, each associated with different states of consciousness and brain activity.
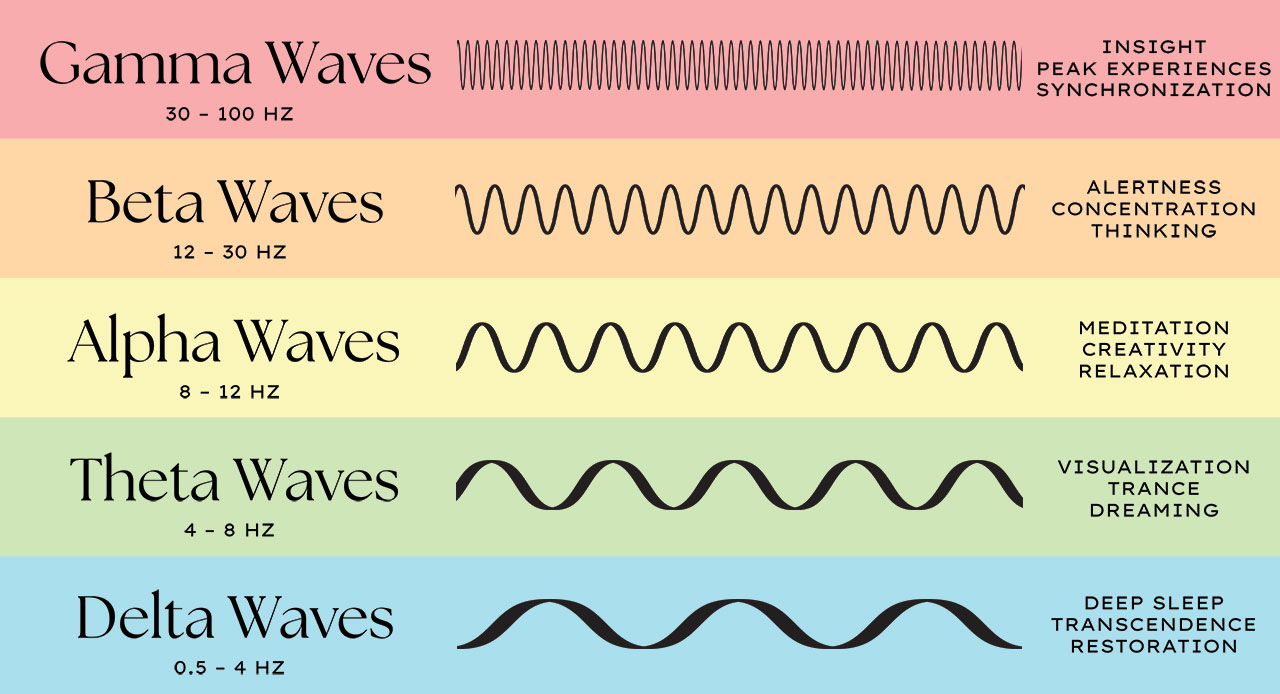
Figure 3: Types of brain waves and their frequency ranges
| Wave Type | Frequency | Normal Occurrence | Psychiatric Significance |
|---|---|---|---|
| Delta (δ) | 0.5 – 4 Hz | Deep sleep, infants, serious brain diseases | Increased in delirium, encephalopathy, and some medications |
| Theta (θ) | 4 – 7 Hz | Drowsiness, childhood, meditation | Excess may indicate encephalopathy, medication effects, or cognitive disorders |
| Alpha (α) | 8 – 12 Hz | Relaxed wakefulness, eyes closed | Asymmetry linked to depression; decreased in anxiety, stress |
| Beta (β) | 13 – 30 Hz | Alert, active concentration | Increased in anxiety disorders, stimulant use; enhanced by benzodiazepines |
| Gamma (γ) | >30 Hz | Higher cognitive processing, perception | Abnormalities in schizophrenia, cognitive disorders |
From fastest to slowest frequency:
B – Beta (13-30 Hz): Busy, active mind
A – Alpha (8-12 Hz): Awakened relaxation
T – Theta (4-7 Hz): Tired, drowsy state
D – Delta (0.5-4 Hz): Deep sleep
EEG Findings in Psychiatric Disorders
Depression
- Alpha asymmetry: increased right vs. left frontal alpha power
- Reduced slow-wave (delta) activity during sleep
- EEG changes may predict antidepressant response
Schizophrenia
- Reduced alpha activity
- Abnormal gamma oscillations during cognitive tasks
- Reduced sleep spindles
- Non-specific slowing in some patients
Bipolar Disorder
- Increased beta activity during manic episodes
- EEG may predict response to lithium vs. valproate
- Some patients show epileptiform activity that may respond to anticonvulsants
Anxiety Disorders
- Increased beta activity, especially frontally
- Decreased alpha activity
- Hypercoherence between frontal regions in some cases
Limitations of EEG in Psychiatry
- No specific diagnostic patterns for most psychiatric disorders
- Findings are often non-specific or inconsistent
- Limited spatial resolution compared to neuroimaging techniques
- Interpretation requires specialized training
- Results must be interpreted in clinical context
Subclinical epileptiform activity may be present in 10-30% of patients with certain psychiatric disorders, particularly those with:
- Treatment-resistant psychosis
- Episodic behavioral disturbances
- Atypical presentation of mood disorders
- History of head injury or other neurological insult
In these cases, a trial of anticonvulsant medication may be beneficial, even without a clinical diagnosis of epilepsy.
Computed Tomography (CT)
Computed Tomography (CT) is an imaging technique that uses X-rays to create cross-sectional images of the brain. In psychiatry, CT scans are primarily used to rule out structural abnormalities that might contribute to or mimic psychiatric symptoms.
Principles & Techniques
CT imaging works by rotating an X-ray source around the patient’s head, with detectors measuring the X-ray attenuation through different tissues. A computer reconstructs these measurements into cross-sectional images.
Key Features of CT Scanning
- Quick scan time: Typically 5-10 minutes
- Good bone imaging: Superior to MRI for bony structures
- Readily available: More accessible than MRI in many settings
- Minimal contraindications: Safe with most implants
- Cost-effective: Less expensive than MRI
Limitations of CT
- Radiation exposure: Uses ionizing radiation
- Limited soft tissue contrast: Less detailed than MRI
- Posterior fossa artifacts: Difficulty visualizing brainstem, cerebellum
- No functional information: Shows structure only
- Limited sensitivity: May miss subtle abnormalities
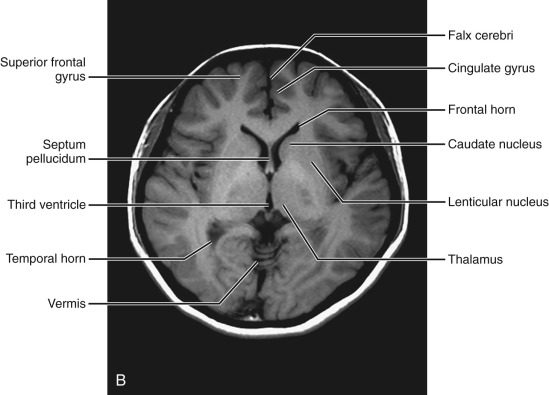
Figure 4: Normal brain CT scan (axial view) with anatomical structures labeled
CT Brain Anatomy – Key Structures
When interpreting a CT brain scan, these key structures should be evaluated:
- Ventricles: Size, symmetry, presence of blood
- Gray-white matter differentiation: Should be clear
- Midline structures: Any shift indicates mass effect
- Basal cisterns: Should be open and visible
- Sulci & gyri: Pattern and symmetry
- Skull: Integrity, thickness, abnormalities
CT Applications in Psychiatry
While CT scans cannot diagnose primary psychiatric disorders, they play an important role in the evaluation of patients with psychiatric symptoms.
Indications for CT in Psychiatric Patients
- First episode psychosis: Rule out organic causes
- Late-onset psychiatric symptoms: After age 40
- Atypical presentation: Not fitting standard diagnostic patterns
- Neurological signs: Focal deficits, abnormal reflexes
- History of head trauma: Evaluating structural damage
- Rapid cognitive decline: Rule out space-occupying lesions
- Treatment resistance: When symptoms don’t respond to standard treatment
| CT Finding | Potential Psychiatric Manifestation | Clinical Significance |
|---|---|---|
| Brain tumor | Personality changes, psychosis, depression, anxiety | Location-dependent; frontal tumors often present with psychiatric symptoms |
| Subdural hematoma | Fluctuating consciousness, cognitive impairment, personality changes | May be chronic and subtle, especially in elderly; often history of falls |
| Hydrocephalus | Cognitive slowing, apathy, incontinence, gait disturbance | Normal pressure hydrocephalus can mimic dementia or depression |
| Cerebral atrophy | Cognitive impairment, behavioral changes | May be seen in dementia, chronic schizophrenia, alcoholism |
| Silent infarcts | Late-life depression, cognitive impairment | Vascular depression hypothesis; may predict treatment resistance |
| Calcifications | Varies by location | Basal ganglia calcifications may cause neuropsychiatric symptoms |
H – History of trauma or falls
E – Elderly onset of psychiatric symptoms
A – Atypical presentation of mental illness
D – Deficit, neurological (focal signs)
C – Cognitive changes, rapid or unexplained
T – Treatment resistance to psychiatric medications
CT is preferred over MRI in emergency settings for psychiatric patients when:
- Acute altered mental status needs rapid evaluation
- History of trauma or suspicion of acute bleeding
- Patient is agitated and cannot remain still for MRI
- MRI contraindications are unknown or present
- Immediate availability is required
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) uses strong magnetic fields and radio waves to generate detailed images of the brain. It provides superior soft tissue contrast compared to CT, making it the preferred modality for detailed neuroanatomical evaluation in psychiatric patients when time permits.
Principles & Techniques
MRI works by aligning hydrogen atoms in the body with a strong magnetic field, then disturbing this alignment with radio frequency pulses. As the atoms return to alignment, they emit signals that are detected and processed into images.
Basic MRI Sequences
- T1-weighted: Good for anatomical detail; CSF appears dark
- T2-weighted: Highlights pathology; CSF appears bright
- FLAIR: Fluid-attenuated inversion recovery; suppresses CSF signal
- DWI: Diffusion-weighted imaging; sensitive for acute stroke
- SWI: Susceptibility-weighted imaging; detects blood products, calcifications
Advanced MRI Techniques
- fMRI: Functional MRI; measures blood flow changes during tasks
- DTI: Diffusion tensor imaging; shows white matter tracts
- MRS: Magnetic resonance spectroscopy; measures brain metabolites
- Perfusion MRI: Measures cerebral blood flow
- Volumetric MRI: Quantifies regional brain volumes
:watermark(/images/watermark_5000_10percent.png,0,0,0):watermark(/images/logo_url.png,-10,-10,0):format(jpeg)/images/overview_image/238/o7ofnEgw4nuC4uVDPZ8QA_mri-t2-axial-thalamus-level_english.jpg)
Figure 5: Normal brain MRI (axial view) with key structures labeled
Advantages of MRI over CT
- Superior soft tissue contrast
- No ionizing radiation exposure
- Multiplanar imaging (axial, coronal, sagittal) without repositioning
- Better visualization of posterior fossa structures
- Ability to detect subtle abnormalities
- Advanced functional and metabolic imaging capabilities
Limitations and Contraindications
- Absolute contraindications: Certain implanted devices (pacemakers, cochlear implants), ferromagnetic foreign bodies, claustrophobia (severe)
- Relative contraindications: Pregnancy (first trimester), tattoos with metallic ink, claustrophobia (mild to moderate)
- Practical limitations: Longer scan time, higher cost, reduced availability, requires patient compliance
MRI Applications in Psychiatry
MRI has revolutionized our understanding of the neurobiological basis of psychiatric disorders by revealing structural and functional brain changes associated with various conditions.
| Psychiatric Disorder | Common MRI Findings | Clinical Significance |
|---|---|---|
| Schizophrenia | Ventricular enlargement, reduced gray matter in prefrontal and temporal regions, thalamic abnormalities | Supports neurodevelopmental hypothesis; findings correlate with symptom severity and cognitive impairment |
| Major Depression | Reduced volume in hippocampus, amygdala, anterior cingulate cortex; white matter hyperintensities in late-life depression | Hippocampal volume may predict treatment response; white matter changes associated with vascular depression |
| Bipolar Disorder | Reduced volume in prefrontal regions, enlarged amygdala, white matter abnormalities | Some findings overlap with schizophrenia; white matter changes suggest connectivity issues |
| PTSD | Reduced hippocampal volume, hyperactive amygdala on fMRI, reduced anterior cingulate activation | Supports stress-related neurotoxicity model; may predict treatment outcomes |
| OCD | Alterations in cortico-striatal-thalamo-cortical circuits; caudate nucleus abnormalities | Suggests circuit-based pathophysiology; may help target interventions |
| Dementia | Hippocampal atrophy (Alzheimer’s), frontal/temporal atrophy (FTD), subcortical infarcts (vascular) | Aids differential diagnosis; can distinguish neurodegenerative from psychiatric causes |
Research Applications of Advanced MRI in Psychiatry
- Functional MRI (fMRI): Maps brain activity during cognitive tasks or at rest; identifies dysfunctional neural circuits
- Diffusion Tensor Imaging (DTI): Evaluates white matter tract integrity; reveals connectivity issues
- MR Spectroscopy: Measures brain metabolites like N-acetylaspartate (neuronal marker), choline (cell membrane turnover), and glutamate (excitatory neurotransmitter)
- Volumetric Analysis: Quantifies regional brain volumes; can track progression over time
Consider MRI over CT when:
- Detailed evaluation of brain structure is needed
- Suspected abnormalities involve areas poorly visualized on CT (posterior fossa, temporal lobes)
- Following up on indeterminate CT findings
- Evaluating neurodegenerative conditions
- Patient can tolerate longer scan time and has no contraindications
- Radiation exposure is a concern (younger patients, need for repeated imaging)
I – Improved soft tissue contrast
M – Multiple planes available
A – Advanced functional assessment (fMRI)
G – Gray matter analysis optimized
E – Excellent posterior fossa visualization
S – Safe (no radiation)
Comparison of Imaging Modalities
Selecting the appropriate imaging modality depends on the clinical context, availability, patient factors, and the specific information needed.
| Feature | CT | MRI | EEG |
|---|---|---|---|
| Primary Function | Structural imaging | Structural & functional imaging | Functional assessment of brain electrical activity |
| Time Required | 5-10 minutes | 30-60 minutes | 20-40 minutes (routine) |
| Cost | Moderate | High | Low to moderate |
| Radiation | Yes (ionizing) | No | No |
| Availability | Widely available | Less widely available | Moderately available |
| Contraindications | Few; pregnancy (relative) | Many; metallic implants, claustrophobia | Very few; skin conditions at electrode sites |
| Best For | Acute evaluation, trauma, hemorrhage, bone abnormalities | Detailed structural analysis, subtle abnormalities, white matter pathology | Seizure activity, encephalopathy, medication effects on brain function |
| Temporal Resolution | Low | Low (standard); moderate (functional) | Excellent (milliseconds) |
| Spatial Resolution | Moderate | High | Low |
Best Uses of CT in Psychiatry
- Emergency evaluation
- Screening for organic causes
- Patients who cannot tolerate MRI
- Acute altered mental status
- Following head trauma
Best Uses of MRI in Psychiatry
- Detailed evaluation after screening CT
- Suspected neurodegenerative disorders
- Subtle abnormalities or lesions
- Research protocols
- Following disease progression
Best Uses of EEG in Psychiatry
- Suspected seizure disorder
- Encephalopathy evaluation
- Unexplained altered consciousness
- Monitoring medication effects
- Evaluating sleep disorders
Clinical Approach to Investigations
A systematic approach to selecting and interpreting investigations is essential for cost-effective and clinically meaningful diagnostic workup of mentally ill patients.
Step 1: Basic Screening
Initial evaluation for all new psychiatric patients:
- Complete history and physical examination
- Basic blood chemistry (CBC, electrolytes, glucose)
- Liver and renal function tests
- Thyroid function tests
- Urine toxicology screen when indicated
- Consider vitamin B12, folate
Step 2: Risk Stratification
Based on clinical presentation, determine if additional testing is warranted:
- Age of onset (late onset suggests organic cause)
- Atypical features
- Neurological signs or symptoms
- Treatment resistance
- History of trauma, substance use
- Rapid cognitive decline
Step 3: Targeted Investigations
Select additional tests based on clinical suspicion:
- CT brain (acute presentations, emergency settings)
- MRI brain (detailed evaluation, follow-up)
- EEG (suspected seizures, encephalopathy, fluctuating course)
- Specialized blood tests (medication levels, autoimmune markers)
- Lumbar puncture (when CNS infection/inflammation suspected)
Step 4: Interpretation & Integration
Correlate findings with clinical presentation:
- Consider normal variants vs. pathological findings
- Assess clinical significance of abnormalities
- Determine need for further investigation or specialist referral
- Integrate findings into diagnostic formulation
- Develop treatment plan based on comprehensive assessment
Consider brain imaging when these features are present:
- New-onset headache with psychiatric symptoms
- Late onset (>40 years) of first psychiatric symptoms
- Neurological abnormalities on examination
- Rapid unexplained cognitive decline
- History of significant head trauma
- New-onset seizures
- Symptoms that fluctuate with level of consciousness
- Treatment resistance to appropriate psychiatric interventions
T – Targeted tests based on clinical suspicion
E – Evidence-based selection (not shotgun approach)
S – Stepwise progression from basic to advanced tests
T – Timing considered (emergency vs. elective)
W – Weigh risks and benefits
I – Interpret in clinical context
S – Specialists consulted when needed
E – Economical use of resources
Summary
Key Principles
- Investigations in psychiatry serve to rule out organic causes, monitor treatment effects, and understand neurobiological bases of disorders
- A systematic, evidence-based approach to test selection improves diagnostic yield while minimizing unnecessary tests
- Results must be interpreted in clinical context; no test can diagnose primary psychiatric disorders
- Interdisciplinary collaboration enhances the value of investigations
Blood Chemistry Tests
Screening Monitoring
- Rule out medical causes of psychiatric symptoms
- Establish baseline before medication
- Monitor medication effects and side effects
- Basic tests include CBC, electrolytes, thyroid, liver, renal function
Electroencephalography (EEG)
Functional Dynamic
- Evaluates brain electrical activity
- Indicated for new-onset psychosis, fluctuating symptoms
- Helps identify seizure disorders, encephalopathy
- May predict treatment response in some conditions
Computed Tomography (CT)
Structural Fast
- Quick screening for structural abnormalities
- Ideal for emergency settings
- Good for detecting hemorrhage, large lesions, fractures
- Limited soft tissue contrast and posterior fossa visualization
Magnetic Resonance Imaging (MRI)
Detailed Comprehensive
- Superior soft tissue contrast
- Detailed evaluation of brain structure
- Advanced techniques provide functional information
- Preferred for detailed neuroanatomical assessment
Future Directions
Emerging technologies and approaches show promise for enhancing the role of investigations in psychiatry:
- Blood-based biomarkers: Emerging tests for specific psychiatric disorders
- Advanced neuroimaging: Machine learning approaches to identify patterns associated with specific disorders
- Pharmacogenomics: Genetic testing to predict medication response
- Integrated multimodal assessment: Combining different testing modalities for comprehensive evaluation
- Personalized medicine approaches: Tailoring investigations to individual risk profiles
Remember that no investigation can replace a thorough clinical assessment. Tests are aids to clinical judgment, not substitutes for it.
