Japanese Encephalitis: Comprehensive Nursing Notes
A Community Health Nursing Perspective
- 1. Introduction to Japanese Encephalitis
- 2. Epidemiology
- 3. Transmission and Vector Biology
- 4. Clinical Manifestations
- 5. Prevention & Control Measures
- 6. Screening Methods
- 7. Diagnostic Approaches
- 8. Primary Management
- 9. Referral Guidelines
- 10. Follow-up Care
- 11. Nursing Care Plans
- 12. Community-Level Interventions
- 13. Global Best Practices
Introduction to Japanese Encephalitis
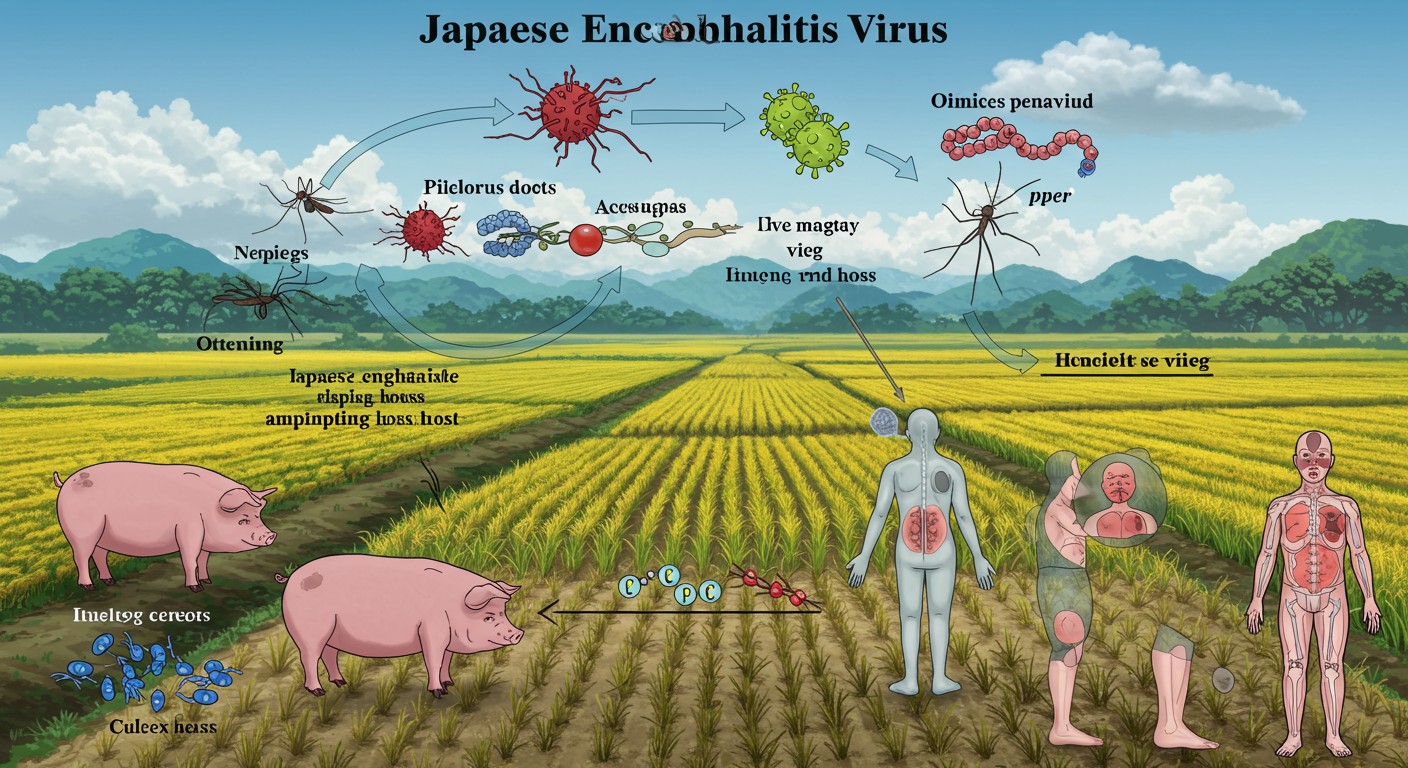
Figure 1: Japanese Encephalitis transmission cycle showing the virus, vectors, hosts, and environmental factors
Japanese Encephalitis (JE) is a serious vector-borne viral disease that affects the central nervous system. It is caused by the Japanese Encephalitis virus (JEV), which belongs to the Flaviviridae family. JE remains a significant public health concern across many parts of Asia and the Western Pacific, with approximately 68,000 clinical cases occurring annually. Although mortality rates vary between 20-30%, up to 50% of survivors experience significant neurological sequelae.
Key Facts About Japanese Encephalitis:
- Caused by a flavivirus (Japanese Encephalitis virus)
- Transmitted primarily by Culex mosquitoes, especially Culex tritaeniorhynchus
- Pigs and wading birds serve as amplifying hosts
- Leading cause of viral encephalitis in Asia
- Vaccination is the most effective preventive measure
From a community health nursing perspective, understanding Japanese Encephalitis is crucial for implementing effective prevention strategies, early case detection, and appropriate management protocols. This comprehensive guide explores the epidemiological aspects, prevention measures, screening approaches, diagnostic methods, and management strategies essential for community health nurses working in endemic areas.
Epidemiology of Japanese Encephalitis
Global Distribution
Japanese Encephalitis is endemic in 24 countries across the WHO South-East Asia and Western Pacific regions, placing over 3 billion people at risk. The geographical distribution of JE encompasses:
- Most countries in Southeast Asia
- Eastern and Southern regions of Asia
- Parts of Western Pacific Islands
- Northern Australia
- Parts of Papua New Guinea
Seasonal Patterns
The epidemiology of Japanese Encephalitis demonstrates distinct seasonal patterns that vary by region:
| Region | Transmission Pattern | Peak Seasons |
|---|---|---|
| Temperate Regions (Northern China, Korea, Japan) | Epidemic transmission | Summer and early autumn (June-September) |
| Tropical Regions (Southern Thailand, Indonesia, Malaysia) | Endemic transmission | Year-round with increased cases during rainy season |
| Subtropical Regions (Northern India, Nepal, Southern China) | Mixed pattern | Primarily during and after monsoon season |
Risk Factors
Several demographic, environmental, and occupational factors influence Japanese Encephalitis transmission:
Demographic Factors
- Children (1-15 years) most vulnerable
- Unvaccinated individuals
- Non-immune travelers to endemic areas
Environmental Factors
- Proximity to rice paddies
- Standing water bodies
- Pig farming areas
- Poor drainage systems
Occupational Factors
- Rice field workers
- Pig farmers
- Agricultural laborers
- Military personnel in endemic areas
Impact and Burden
Japanese Encephalitis imposes a significant public health burden:
- Approximately 68,000 clinical cases annually worldwide
- Case fatality rate: 20-30% among symptomatic cases
- 30-50% of survivors develop permanent neurological sequelae
- Disproportionately affects rural and poor communities
- Economic impact through healthcare costs, lost productivity, and long-term disability care
- J – Juvenile population most affected
- A – Asian countries predominately endemic
- P – Pigs as amplifying hosts
- A – Agricultural settings (rice fields) as risk zones
- N – Neurological sequelae common in survivors
Transmission and Vector Biology
Understanding the transmission cycle of Japanese Encephalitis is essential for implementing effective prevention and control strategies. The virus maintains a complex enzootic cycle involving mosquito vectors and vertebrate amplifying hosts.
Vector Biology
The primary vectors for Japanese Encephalitis virus transmission are:
- Primary Vector: Culex tritaeniorhynchus
- Secondary Vectors: Culex vishnui, Culex gelidus, Culex fuscocephalus
These mosquitoes share several characteristics that facilitate JE transmission:
- Breed predominantly in rice fields and other water bodies
- Feed at dusk and during night hours
- Prefer to feed on animals but readily bite humans
- Rest outdoors in vegetation
- Flight range of 1-3 km
Transmission Cycle
The JE virus persists in nature through a cycle involving mosquitoes and vertebrate hosts:
- Primary Cycle (Enzootic Cycle): Involves mosquitoes and amplifying hosts (pigs and wading birds)
- Secondary/Spillover Cycle: Transmission to humans and horses (dead-end hosts)
Important Note: Humans and horses are considered “dead-end hosts” because they typically do not develop sufficient viremia to infect feeding mosquitoes, thus not contributing to the ongoing transmission cycle.
Amplifying Hosts
Certain vertebrates play crucial roles in the JE transmission cycle:
| Host Type | Examples | Role in Transmission |
|---|---|---|
| Primary Amplifying Hosts | Domestic pigs, wild boars | Develop high and prolonged viremia; key for virus amplification |
| Secondary Amplifying Hosts | Wading birds (herons, egrets) | Maintain virus during dry seasons; aid in geographic spread |
| Dead-end Hosts | Humans, horses | Develop infection but insufficient viremia to continue transmission |
Environmental Factors
Several environmental conditions influence Japanese Encephalitis transmission:
Water-related Factors
- Irrigated rice fields
- Stagnant water bodies
- Poor drainage systems
- Monsoon patterns
Climatic Factors
- Temperature (optimal: 22-34°C)
- Humidity (>70% favors transmission)
- Rainfall patterns
- Seasonal variations
Agricultural Practices
- Rice cultivation techniques
- Pig farming proximity to human habitation
- Farming seasons
- Irrigation methods
The complex interaction between vector ecology, host biology, and environmental factors creates ideal conditions for Japanese Encephalitis transmission in endemic regions, particularly in rural agricultural areas across Asia.
Clinical Manifestations
Japanese Encephalitis presents with a wide spectrum of clinical manifestations, ranging from asymptomatic infection to severe encephalitis. Understanding the clinical presentation is crucial for early recognition and timely intervention by community health nurses.
Key Point: Most JE infections (approximately 99%) are asymptomatic or result in mild febrile illness. Only about 1:250 to 1:500 infections progress to encephalitis.
Stages of Disease Progression
Incubation Period
Typically 5-15 days after infected mosquito bite
Prodromal Phase (2-3 days)
Non-specific febrile illness resembling flu-like symptoms
- Fever (usually high grade)
- Headache
- Malaise
- Nausea and vomiting
Acute Encephalitic Phase (3-7 days)
Rapid neurological deterioration with signs of CNS involvement
- Altered consciousness
- Seizures
- Focal neurological deficits
- Neck stiffness and meningeal signs
Late/Recovery Phase (weeks to months)
Gradual improvement or development of sequelae
- Progressive recovery in non-severe cases
- Persistent neurological deficits in 30-50% of survivors
Signs and Symptoms
Japanese Encephalitis manifests with diverse clinical features, particularly affecting the central nervous system:
| System Affected | Clinical Manifestations | Significance |
|---|---|---|
| Neurological |
|
Direct indicators of encephalitis; common in severe disease |
| Behavioral/Psychological |
|
Often early signs of encephalitis; may be subtle |
| Systemic |
|
Present in prodromal phase; non-specific |
| Meningeal |
|
Suggests meningoencephalitis; variable presence |
- E – Elevated temperature (high fever)
- N – Neurological deficits (focal or diffuse)
- C – Consciousness alteration (confusion to coma)
- E – Extrapyramidal symptoms (tremor, rigidity)
- P – Parkinsonian features (mask-like facies)
- H – Headache (severe, persistent)
- A – Altered behavior and personality
- L – Lethargy progressing to stupor
- I – Increased intracranial pressure signs
- T – Tremors and movement disorders
- I – Insomnia or somnolence
- S – Seizures (focal or generalized)
Special Considerations in Children
Children with Japanese Encephalitis often present differently than adults:
- More likely to present with seizures as an initial symptom
- Higher probability of developing status epilepticus
- May exhibit non-specific symptoms like abdominal pain, vomiting, and diarrhea
- Cognitive and developmental sequelae more pronounced
- Higher case-fatality rates compared to adults
Sequelae and Long-term Outcomes
Among survivors of Japanese Encephalitis, neurological and psychiatric sequelae are common:
Motor Sequelae
- Paralysis
- Paresis
- Dystonia
- Movement disorders
Cognitive Sequelae
- Memory impairment
- Intellectual disability
- Learning difficulties
- Language deficits
Behavioral/Psychiatric
- Personality changes
- Emotional lability
- Psychosis
- Depression
Prevention & Control Measures
Prevention and control of Japanese Encephalitis require a comprehensive approach encompassing personal protection, environmental management, vaccination, and community-level interventions. Community health nurses play a pivotal role in implementing these strategies.
Primary Prevention
Primary prevention aims to prevent Japanese Encephalitis infection before it occurs:
Vaccination
Vaccination is the most effective preventive measure against Japanese Encephalitis:
| Vaccine Type | Schedule | Target Population | Efficacy |
|---|---|---|---|
| Inactivated Vero Cell-derived Vaccine (IXIARO®/JESPECT®) | 2 doses (0, 28 days) | Children ≥2 months and adults | ≥95% after 2 doses |
| Live Attenuated SA14-14-2 Vaccine | 1-2 doses | Children in endemic areas | 88-96% after single dose |
| Inactivated Mouse Brain-derived Vaccine (JE-VAX®) | 3 doses (0, 7, 30 days) | Limited production, being phased out | 80-90% after 3 doses |
| ChimeriVax-JE (IMOJEV®) | Single dose | Children ≥9 months and adults | ≥95% after single dose |
Nursing Considerations for JE Vaccination:
- Maintain cold chain integrity for vaccine efficacy
- Screen for contraindications (severe allergic reactions to previous dose)
- Monitor for post-vaccination reactions
- Ensure complete documentation in immunization records
- Provide vaccination certificates for travelers to endemic areas
Personal Protective Measures
These measures aim to prevent mosquito bites and should be recommended by community health nurses:
Indoor Protection
- Use of window and door screens
- Bed nets (preferably insecticide-treated)
- Air conditioning when available
- Indoor residual spraying
- Use of mosquito coils or vaporizers
Outdoor Protection
- Wearing long-sleeved shirts and pants
- Application of insect repellents (DEET, picaridin)
- Avoiding outdoor activities during peak mosquito feeding times (dusk and dawn)
- Treating clothing with permethrin
Environmental Management
These interventions target vector breeding sites and amplifying hosts:
- Water Management: Intermittent irrigation of rice fields can reduce mosquito breeding
- Vector Control: Biological control using larvivorous fish or bacterial agents
- Host Management: Separation of pig farms from human habitation
- Integrated Vector Management: Combining multiple approaches for maximum effectiveness
Secondary Prevention
Secondary prevention focuses on early detection and prompt intervention:
- Syndromic Surveillance: Active monitoring for encephalitis clusters in endemic areas
- Case Detection: Early recognition of symptoms by trained health workers
- Laboratory Surveillance: Testing of sentinel cases during transmission season
- Rapid Response: Investigation of outbreaks and implementation of control measures
Tertiary Prevention
Tertiary prevention aims to reduce complications and improve quality of life for affected individuals:
- Rehabilitation Services: Physical, occupational, and speech therapy
- Neurological Support: Management of seizures and movement disorders
- Cognitive Rehabilitation: Support for learning difficulties and cognitive deficits
- Psychosocial Support: Counseling for patients and families
- Community Reintegration: Vocational training and social inclusion programs
- V – Vaccination as primary prevention
- E – Environmental management
- C – Chemical repellents for personal protection
- T – Treated bed nets and screens
- O – Outreach and education in communities
- R – Respiratory and contact precautions (not required for JE)
- S – Surveillance and early detection
Screening Methods
Effective screening is essential for early detection of Japanese Encephalitis cases in endemic areas. Community health nurses should be familiar with various screening approaches to identify potential cases for further evaluation.
Clinical Screening
Clinical screening involves the identification of individuals with symptoms suggestive of Japanese Encephalitis:
Acute Encephalitis Syndrome (AES) Screening
WHO case definition of AES used for initial screening:
A person of any age, at any time of year with:
- Acute onset of fever
- AND change in mental status (including symptoms such as confusion, disorientation, coma, or inability to talk)
- AND/OR new onset of seizures (excluding simple febrile seizures)
Other early clinical findings may include an increase in irritability, somnolence or abnormal behavior greater than that seen with usual febrile illness.
Community-Based Screening
Community health nurses can implement screening strategies at the community level:
- Active Case Finding: Home visits in high-risk areas during transmission season
- Fever Surveillance: Monitoring of febrile illnesses, especially those with neurological symptoms
- Travel History Assessment: Screening individuals with recent travel to JE-endemic areas
- Risk Factor Assessment: Identifying individuals with occupational or environmental risk factors
Laboratory Screening
Laboratory tests are used for confirmatory screening of suspected cases:
| Screening Test | Sample Required | Turnaround Time | Limitations |
|---|---|---|---|
| JE IgM ELISA (Serum) | Blood sample (5-10 ml) | 24-48 hours | May cross-react with other flaviviruses; best collected 4-7 days after onset |
| JE IgM ELISA (CSF) | Cerebrospinal fluid | 24-48 hours | Requires lumbar puncture; more specific than serum testing |
| RT-PCR | Blood, CSF | 6-24 hours | Only positive in early phase (1-3 days); limited sensitivity |
| Rapid Diagnostic Test | Blood (finger prick) | 15-30 minutes | Lower sensitivity; preliminary screening only |
Sentinel and Enhanced Surveillance
In endemic areas, structured surveillance systems help in early detection of JE cases:
- Sentinel Site Surveillance: Designated health facilities routinely test suspected cases
- Event-Based Surveillance: Investigation of clusters of encephalitis cases
- Integrated Disease Surveillance: JE included in broader infectious disease monitoring
- Seasonal Intensified Surveillance: Enhanced screening during high-risk periods
Screening Algorithm for Japanese Encephalitis
Initial Assessment: Patient presents with fever and neurological symptoms
Clinical Screening: Apply AES case definition
Risk Assessment: Evaluate exposure history and risk factors
Laboratory Testing: Collect appropriate samples for confirmation
Case Classification: Categorize as suspected, probable, or confirmed
Diagnostic Approaches
Accurate diagnosis of Japanese Encephalitis involves a combination of clinical evaluation, laboratory testing, and neuroimaging. Community health nurses should understand the diagnostic process to facilitate appropriate referrals and follow-up.
Clinical Diagnosis
The initial diagnosis is based on clinical presentation and epidemiological factors:
- Clinical Features: Fever, altered consciousness, seizures, focal neurological deficits
- Epidemiological Context: Residence or travel in endemic area during transmission season
- Risk Factors: Lack of vaccination, outdoor activities, proximity to rice fields or pig farms
Diagnostic Challenge: The clinical presentation of Japanese Encephalitis can be similar to other causes of encephalitis including other arboviruses, herpes simplex virus, bacterial meningoencephalitis, cerebral malaria, and toxic encephalopathies.
Laboratory Diagnosis
Laboratory confirmation is essential for definitive diagnosis:
Serological Tests
| Test | Interpretation | Timing |
|---|---|---|
| JE IgM ELISA (CSF) | Most specific diagnostic test; presence indicates recent infection | Positive from day 4-7 after onset, remains detectable for 1-3 months |
| JE IgM ELISA (Serum) | Supportive of diagnosis but less specific than CSF | Positive from day 4-7 after onset, remains detectable for 1-3 months |
| JE IgG ELISA | Indicates past infection or vaccination; four-fold rise in paired sera is significant | Appears after 7-10 days, persists for years |
| Plaque Reduction Neutralization Test (PRNT) | Gold standard for specificity; confirms JE antibodies | Usually performed as a reference test to confirm other results |
Molecular Tests
- RT-PCR: Detection of viral RNA in CSF, blood, or tissue samples
- Utility: Most useful in early stage (first 3-4 days) before antibody response
- Limitation: Low sensitivity due to brief viremia and low viral load in CSF
Virus Isolation
- Method: Isolation of virus from clinical specimens in cell culture or mosquito inoculation
- Utility: Research purposes, strain identification
- Limitation: Time-consuming, requires biosafety level 3 facilities, low sensitivity
Neuroimaging
Neuroimaging provides supportive evidence for diagnosis and helps assess the extent of brain involvement:
MRI Findings
- Thalamic lesions (bilateral)
- Basal ganglia involvement
- Brainstem abnormalities
- Hippocampal lesions
- T2-weighted hyperintensities
CT Scan Findings
- Less sensitive than MRI
- May show low-density areas
- Thalamic hypodensities
- Cerebral edema in severe cases
Additional Diagnostic Evaluations
Supportive diagnostic tests help in assessment and differential diagnosis:
- Cerebrospinal Fluid Analysis:
- Moderately elevated protein (50-200 mg/dL)
- Normal glucose levels
- Mild to moderate pleocytosis (10-100 cells/mm³) with lymphocyte predominance
- Electroencephalography (EEG):
- Generalized slowing of background activity
- Epileptiform discharges in patients with seizures
- Periodic lateralized epileptiform discharges in some cases
- Differential Diagnostic Tests:
- Tests for other viral encephalitides (HSV, enterovirus, West Nile virus)
- Blood cultures for bacterial pathogens
- Malaria smears in co-endemic areas
- Toxicology screening when relevant
- D – Determine clinical presentation (fever with neurological symptoms)
- I – Investigate epidemiological links (endemic area, season)
- A – Analyze CSF (lymphocytic pleocytosis, elevated protein)
- G – Gather serology (JE IgM in CSF/serum)
- N – Neuroimaging (MRI showing thalamic lesions)
- O – Obtain molecular tests (RT-PCR in early phase)
- S – Screen for alternative causes
- E – Evaluate response to supportive treatment
- J – Judge clinical course for compatibility
- E – Exclude similar conditions in differential diagnosis
Primary Management
Management of Japanese Encephalitis is primarily supportive as there is no specific antiviral therapy. Early intervention and comprehensive care are essential to improve outcomes.
Key Principle: While community health nurses may not directly manage severe JE cases in hospital settings, understanding management principles is crucial for patient education, referral decisions, and post-discharge follow-up.
Initial Management
Early interventions focus on stabilization and supportive care:
Assessment and Stabilization
- Airway, breathing, circulation (ABC) assessment
- Vital signs monitoring
- Neurological assessment (GCS, pupillary reactions, focal deficits)
- Secure IV access
Diagnostic Workup
- Blood collection for baseline investigations and serology
- Arrangement for lumbar puncture (if no contraindications)
- Neuroimaging as indicated
- Other investigations to rule out differential diagnoses
Immediate Interventions
- Antipyretics for fever management
- Anticonvulsants if seizures present
- Airway protection if consciousness impaired
- Fluid management
Decision for Referral
- Assessment of severity
- Evaluation of local management capabilities
- Arrangement for appropriate level of care
- Communication with referral center
Supportive Management
Comprehensive supportive care is the mainstay of JE management:
| Management Aspect | Interventions | Nursing Considerations |
|---|---|---|
| Respiratory Support |
|
|
| Neurological Management |
|
|
| Fluid and Electrolyte Balance |
|
|
| Fever Management |
|
|
| Nutrition and Hydration |
|
|
Management of Complications
Prompt identification and management of complications is essential:
Raised Intracranial Pressure
- Head elevation (30°)
- Osmotic diuretics (mannitol, hypertonic saline)
- Avoid fluid overload
- Hyperventilation (short-term only)
- Sedation if needed
Status Epilepticus
- IV benzodiazepines (first line)
- IV phenytoin or fosphenytoin
- IV valproate, levetiracetam
- Barbiturate coma for refractory cases
- Continuous EEG monitoring when available
Secondary Infections
- Early recognition of signs
- Appropriate cultures
- Empiric antibiotics based on likely pathogens
- VAP prevention measures
- Aseptic techniques for procedures
Autonomic Disturbances
- Monitoring of vital signs
- Treatment of hypertension or hypotension
- Management of cardiac arrhythmias
- Temperature regulation
- Prevention of autonomic storms
Note: There is no specific antiviral therapy proven effective for Japanese Encephalitis. Ribavirin, interferon alfa, and other antivirals have been studied but show no clear benefit. Management remains supportive.
Early Rehabilitation
Early initiation of rehabilitation improves outcomes and prevents complications:
- Physical Therapy: Passive range of motion exercises, positioning to prevent contractures
- Respiratory Therapy: Chest physiotherapy, incentive spirometry
- Swallowing Assessment: Early evaluation to prevent aspiration
- Cognitive Stimulation: Orientation activities, sensory stimulation
- Psychological Support: Addressing anxiety, emotional needs of patient and family
- S – Seizure control and management
- U – Understand disease progression
- P – Prevent complications (aspiration, pressure ulcers)
- P – Provide respiratory support as needed
- O – Optimize fluid and electrolyte balance
- R – Reduce intracranial pressure when elevated
- T – Temperature regulation
- J – Judge neurological status regularly
- E – Early rehabilitation interventions
Referral Guidelines
Appropriate and timely referral is critical for optimal management of Japanese Encephalitis cases. Community health nurses should be familiar with referral criteria and procedures to ensure continuity of care.
Indications for Referral
Patients with suspected Japanese Encephalitis should be referred to higher levels of care when certain criteria are met:
Emergency Referral Criteria
- Altered level of consciousness (GCS <13)
- Seizures, especially if multiple or prolonged
- Respiratory distress or inadequate airway protection
- Signs of increased intracranial pressure
- Hemodynamic instability
- Rapid neurological deterioration
Urgent Referral Criteria
- Suspected JE with neurological symptoms but stable vital signs
- Fever with meningeal signs requiring diagnostic lumbar puncture
- Need for neuroimaging not available at primary facility
- Persistent vomiting affecting hydration status
- Inability to provide appropriate supportive care locally
Referral Pathways
Well-defined referral pathways ensure efficient transfer of patients to appropriate facilities:
Primary Health Center to District Hospital
For initial assessment, stabilization, and basic laboratory testing
District Hospital to Regional/Tertiary Center
For cases requiring specialized neurological care, ICU management, or advanced diagnostics
Regional Center to Specialized Neuro Center
For complex cases requiring neurosurgical intervention or specialized neurorehabilitation
Pre-Referral Management
Before transfer, community health nurses should ensure that appropriate stabilization measures are completed:
| Aspect | Pre-Referral Interventions |
|---|---|
| Airway Management |
|
| Seizure Management |
|
| Circulation |
|
| Elevated ICP Management |
|
| Documentation |
|
Communication During Referral
Effective communication ensures continuity of care during transitions:
- Direct Communication: Telephone discussion between referring and receiving clinicians
- Structured Handover: Using standardized formats (e.g., SBAR: Situation, Background, Assessment, Recommendation)
- Transfer Documents: Comprehensive referral notes including treatment given, response, and pending results
- Family Communication: Clear explanation to family regarding reason for transfer, destination, and expected process
SBAR Example for JE Referral Communication:
- Situation: “I am referring a 6-year-old male with suspected Japanese Encephalitis presenting with fever for 3 days and new onset seizures.”
- Background: “Patient lives near rice fields in an endemic area. No vaccination history. Developed altered consciousness this morning after two generalized seizures.”
- Assessment: “Currently GCS 10, febrile at 39.2°C, has neck stiffness. Initial assessment suggests acute encephalitis syndrome. Basic labs show leukocytosis.”
- Recommendation: “Patient requires lumbar puncture, neuroimaging, and possible ICU care. I’ve administered IV diazepam for seizures, started ceftriaxone, and stabilized for transfer. Ambulance estimated arrival at your facility in 40 minutes.”
Post-Referral Follow-up
Community health nurses should maintain involvement after referral:
- Establish communication channels with referral facility
- Obtain updates on patient status and treatment plan
- Prepare for eventual return of patient to community
- Identify rehabilitation and support needs for discharge planning
- Conduct disease surveillance activities in the patient’s community
Follow-up Care
Comprehensive follow-up care is essential for Japanese Encephalitis survivors, as many experience long-term neurological sequelae. Community health nurses play a crucial role in coordinating follow-up services and supporting recovery.
Post-Discharge Follow-up Schedule
A structured follow-up schedule helps ensure appropriate monitoring and early intervention for complications:
| Timeframe | Assessment Focus | Interventions |
|---|---|---|
| 1-2 Weeks Post-Discharge |
|
|
| 1 Month |
|
|
| 3 Months |
|
|
| 6 Months and 1 Year |
|
|
| Annual (Long-term) |
|
|
Management of Sequelae
Japanese Encephalitis survivors often experience various neurological sequelae requiring targeted interventions:
Motor Dysfunction
- Physical therapy for weakness, spasticity
- Occupational therapy for fine motor skills
- Assistive devices (braces, walkers, wheelchairs)
- Botulinum toxin for severe spasticity
- Home exercises program
Cognitive Impairment
- Cognitive rehabilitation
- Special education services
- Memory aids and strategies
- Structured daily routines
- Adaptive learning approaches
Seizure Disorders
- Anticonvulsant medication management
- Seizure diary maintenance
- Seizure first aid education for family
- Regular EEG monitoring
- Safety precautions
Behavioral Issues
- Behavioral therapy
- Family counseling
- Structured environment
- Psychiatric consultation when needed
- Support groups
Community Reintegration
Supporting survivors’ return to community life requires multifaceted approaches:
- Educational Reintegration:
- Individual education plans
- Classroom accommodations
- Teacher education about JE sequelae
- Gradual return to school schedule
- Social Reintegration:
- Peer education to reduce stigma
- Social skills training
- Community awareness programs
- Inclusion in community activities
- Vocational Rehabilitation (for adults):
- Vocational assessment
- Job coaching
- Workplace accommodations
- Supported employment options
Family Support and Education
Families of JE survivors need comprehensive support to manage long-term care needs:
Family Education Components
- Understanding JE and Its Sequelae: Clear information about the disease, expected recovery course, and potential long-term effects
- Home Care Skills: Practical training in caregiving techniques, positioning, feeding, medication administration
- Warning Signs: Recognition of complications requiring medical attention (seizures, infections, deterioration)
- Rehabilitation Techniques: Basic exercises and activities to continue rehabilitation at home
- Psychological Support: Coping strategies, stress management, and accessing mental health resources
Caregiver Support Strategies:
- Respite care arrangements
- Connection to support groups
- Regular assessment of caregiver burden
- Home health aide services when available
- Financial support resources
Documentation and Monitoring
Comprehensive documentation supports continuity of care and outcome tracking:
- Follow-up Record: Standardized documentation of all follow-up assessments and interventions
- Rehabilitation Progress Notes: Regular updates on functional improvements and ongoing challenges
- Medication Log: Detailed record of medications, dosages, adjustments, and side effects
- Functional Assessment Scales: Regular use of standardized tools to monitor progress
- Growth and Development Charts: For pediatric survivors to track developmental milestones
- R – Regular assessment schedule
- E – Evaluate for complications and sequelae
- C – Coordinate multidisciplinary services
- O – Optimize functional abilities through rehabilitation
- V – Vocational/educational reintegration planning
- E – Educate family and caregivers
- R – Resource connection and community support
Nursing Care Plans
Community health nurses should develop comprehensive care plans for individuals affected by Japanese Encephalitis. These plans address both acute and chronic care needs with specific nursing interventions.
Nursing Diagnosis: Ineffective Cerebral Tissue Perfusion related to inflammatory process of encephalitis
Expected Outcomes:
- Patient will maintain adequate cerebral perfusion as evidenced by stable neurological signs
- Patient will demonstrate improved or stable level of consciousness
- Intracranial pressure will remain within normal limits
Nursing Interventions:
- Monitor neurological status using Glasgow Coma Scale every 2-4 hours and as needed
- Assess for changes in pupillary response, motor function, and vital signs
- Maintain head elevation at 30 degrees to promote venous drainage
- Avoid activities that increase intracranial pressure (Valsalva maneuver, excessive coughing)
- Administer osmotic diuretics as prescribed and monitor response
- Ensure adequate oxygenation and maintain normothermia
- Monitor for signs of increased intracranial pressure (headache, vomiting, altered consciousness)
Nursing Diagnosis: Risk for Injury related to seizure activity
Expected Outcomes:
- Patient will remain free from injury during seizure episodes
- Seizure activity will be promptly recognized and managed
- Caregiver will demonstrate understanding of seizure safety measures
Nursing Interventions:
- Create safe environment by padding bed rails and removing hazardous objects
- Maintain seizure precautions (padded side rails, bed in low position, suction equipment available)
- Administer anticonvulsant medications as prescribed and monitor therapeutic levels
- Document characteristics of seizures including duration, type, precipitating factors, and post-ictal state
- Position patient on side during and after seizures to prevent aspiration
- Educate family members on seizure first aid and safety measures
- Implement seizure action plan for community and home settings
Nursing Diagnosis: Impaired Physical Mobility related to neuromuscular impairment
Expected Outcomes:
- Patient will demonstrate improved mobility within limitations
- Patient will not develop complications of immobility
- Patient/caregiver will demonstrate proper positioning and transfer techniques
Nursing Interventions:
- Perform passive range of motion exercises every 4 hours if patient is immobile
- Collaborate with physical therapist to develop and implement mobility plan
- Implement positioning schedule with position changes every 2 hours
- Apply appropriate assistive devices (braces, splints) as recommended
- Assess skin integrity regularly and implement pressure injury prevention measures
- Teach caregiver proper positioning, transfer techniques, and mobility exercises
- Encourage progressive mobility as tolerated
Nursing Diagnosis: Self-Care Deficit related to neurocognitive impairment
Expected Outcomes:
- Patient will demonstrate increased independence in self-care activities
- Patient/caregiver will utilize adaptive equipment effectively
- Basic hygiene and personal care needs will be consistently met
Nursing Interventions:
- Assess current level of independence using standardized functional assessment tools
- Collaborate with occupational therapist to identify appropriate adaptive equipment
- Establish consistent routines for activities of daily living
- Provide step-by-step instructions using simple language and demonstrations
- Encourage independence in self-care activities while providing necessary assistance
- Train caregivers in techniques to promote patient’s maximum independence
- Monitor progress and adjust care plan as functional status changes
Nursing Diagnosis: Impaired Verbal Communication related to neurological damage
Expected Outcomes:
- Patient will establish a functional communication method
- Patient/caregiver will demonstrate use of alternative communication strategies
- Communication needs will be effectively met
Nursing Interventions:
- Assess type and severity of communication impairment
- Consult with speech-language pathologist for comprehensive evaluation and recommendations
- Implement alternative communication methods as appropriate (picture boards, communication devices)
- Establish consistent communication strategies to be used by all caregivers
- Allow sufficient time for patient to process information and respond
- Use clear, simple language and validate understanding
- Teach family members effective communication techniques
Nursing Diagnosis: Caregiver Role Strain related to long-term care requirements
Expected Outcomes:
- Caregiver will verbalize reduced stress levels
- Caregiver will utilize available support services
- Caregiver will demonstrate self-care practices
Nursing Interventions:
- Assess caregiver burden using standardized tools
- Identify available support systems and resources
- Provide education about respite care options
- Teach stress management techniques
- Connect family with support groups and counseling services
- Establish regular follow-up to monitor caregiver coping
- Assist in developing schedule that includes caregiver self-care time
Community-Level Interventions
Preventing and controlling Japanese Encephalitis requires comprehensive community-level interventions. Community health nurses play vital roles in implementing these strategies to reduce disease burden.
Health Education and Awareness
Raising community awareness about Japanese Encephalitis is essential for prevention:
Key Educational Topics
- Transmission cycle of JE
- Early signs and symptoms
- Personal protection measures
- Importance of vaccination
- Environmental risk factors
Target Audiences
- Parents of young children
- Agricultural workers
- Community leaders and influencers
- School teachers and students
- Local healthcare providers
Educational Approaches
- Community meetings and workshops
- School health programs
- Mass media campaigns
- Visual aids and demonstrations
- Peer education programs
Vector Control at Community Level
Community-based vector control strategies are crucial for reducing transmission:
Environmental Management
- Water Management:
- Intermittent irrigation of rice fields
- Drainage of standing water
- Proper maintenance of irrigation channels
- Vegetation Control:
- Clearing vegetation around homes
- Maintaining clear zones between rice fields and residential areas
- Community clean-up campaigns
- Livestock Management:
- Pig vaccination programs
- Separation of pig farms from residential areas
- Screened pig shelters
Biological Control Methods
- Introduction of larvivorous fish in rice fields and water bodies
- Use of Bacillus thuringiensis israelensis (Bti) as a larvicide
- Community-managed fish farming in irrigation ponds
- Promotion of natural predators of mosquito larvae
Chemical Control Strategies
- Indoor residual spraying in high-risk areas
- Larviciding of breeding sites
- Space spraying during outbreaks
- Insecticide-treated materials (curtains, screens)
Community Participation in Vector Control:
- Formation of village health committees
- Training community volunteers as vector control agents
- Regular community-led monitoring of breeding sites
- Integration with other vector-borne disease control programs
- Recognition and incentive systems for active communities
Vaccination Campaigns
Community-based vaccination strategies maximize coverage in endemic areas:
Planning and Implementing JE Vaccination Campaigns
Preparatory Phase:
- Risk assessment and target population identification
- Vaccine procurement and cold chain preparation
- Training of vaccination teams
- Community sensitization and mobilization
Implementation Strategies:
- Fixed-post vaccination centers
- Outreach sessions in remote areas
- School-based vaccination
- Integration with routine immunization
Coverage Enhancement:
- Defaulter tracking and follow-up
- Community incentives for participation
- Addressing vaccine hesitancy
- Special approaches for hard-to-reach populations
Monitoring and Evaluation:
- Coverage surveys
- Adverse event monitoring
- Documentation and reporting
- Impact assessment
Surveillance and Response Systems
Community-based surveillance enhances early detection and rapid response:
Community-Based Surveillance
- Key Elements:
- Training of community health workers to recognize suspected cases
- Establishment of reporting mechanisms
- Simple case definitions for community use
- Regular supervision and feedback
- Data Collection:
- Standardized reporting forms
- Mobile health (mHealth) applications
- Regular reporting schedules
- Zero reporting during transmission season
- Response Mechanisms:
- Rapid response teams at district level
- Case investigation protocols
- Vector control responses to confirmed cases
- Enhanced surveillance in affected areas
Intersectoral Collaboration
Effective JE prevention requires coordination across multiple sectors:
| Sector | Role in JE Prevention and Control |
|---|---|
| Health Department |
|
| Agriculture Department |
|
| Irrigation and Water Resources |
|
| Education Department |
|
| Local Government |
|
Community Empowerment
Empowering communities for sustainable JE prevention requires:
- Capacity Building: Training community members in prevention and control activities
- Local Leadership: Engaging community leaders as champions for JE prevention
- Community Ownership: Involving communities in planning and implementing interventions
- Resource Mobilization: Supporting communities to identify and utilize local resources
- Knowledge Translation: Converting scientific information into practical community actions
- C – Collaborative partnerships across sectors
- O – Ongoing surveillance and monitoring
- M – Mosquito control strategies
- M – Mass vaccination campaigns
- U – Understanding local context and beliefs
- N – Nurturing community leadership
- I – Information and education campaigns
- T – Training of community health workers
- Y – Yearly evaluation and adaptation of strategies
Global Best Practices
Several countries have implemented successful Japanese Encephalitis prevention and control programs. Understanding these best practices can inform effective approaches in other endemic regions.
Successful National Programs
Japan’s Elimination Success
Japan has effectively eliminated locally acquired JE through comprehensive interventions:
- Universal Vaccination: National immunization program since 1954
- Agricultural Modernization: Changes in rice cultivation practices reduced vector breeding
- Pig Management: Separation of pig farming from residential areas
- Environmental Modification: Improved irrigation and water management
- Sustained Surveillance: Ongoing monitoring despite low incidence
Key Lesson: Integrated approach combining vaccination, vector control, and agricultural modifications leads to sustainable reduction in JE incidence.
South Korea’s Integrated Approach
South Korea reduced JE incidence by more than 90% through:
- Comprehensive Vaccination: High coverage vaccination campaigns
- Vector Control: Systematic mosquito control in rice-growing regions
- Rice Paddy Management: Implementation of intermittent irrigation
- Surveillance: National surveillance system with mandatory reporting
- Research: Continuous investment in understanding local transmission patterns
Key Lesson: Sustained political commitment and multisectoral coordination are essential for program success.
China’s Control Program
China has significantly reduced JE burden through:
- Massive Vaccination: Inclusion of JE vaccine in Expanded Program on Immunization
- Domestic Vaccine Production: Development of locally produced live attenuated vaccine
- Agricultural Transformation: Changes in pig farming practices and rice cultivation
- Rural Development: Improved housing and infrastructure reducing exposure
- Health System Strengthening: Enhanced diagnostic and case management capabilities
Key Lesson: Local vaccine production and adaptation of strategies to regional contexts enhance program sustainability.
India’s Phased Approach
India has implemented targeted interventions in high-burden areas:
- Risk Mapping: Identification of high-risk districts for prioritized interventions
- Phased Vaccination: Sequential introduction of JE vaccination in endemic areas
- Acute Encephalitis Syndrome Surveillance: Enhanced surveillance in endemic states
- Capacity Building: Training of healthcare workers in case management
- Community Mobilization: Engagement of community-based organizations
Key Lesson: Prioritizing high-burden areas with limited resources can achieve significant impact.
Innovative Approaches
Novel strategies have shown promise in JE prevention and control:
Eco-Bio-Social Approach
- Integration of ecological, biological, and social perspectives
- Community-led ecosystem management
- Sustainable agriculture practices
- Social mobilization for behavior change
Technology Integration
- Mobile health applications for surveillance
- GIS mapping of case distribution
- Remote sensing for vector habitat identification
- Digital platforms for health education
Community-Led Initiatives
- Village health committees for vector control
- Community-based rehabilitation for JE survivors
- Peer education networks
- Local advocacy groups
WHO Recommendations
The World Health Organization provides comprehensive guidance for JE prevention and control:
WHO Core Recommendations:
- Vaccination: Implementation of JE vaccination in all regions where the disease is a public health priority
- Surveillance: Establishment of JE surveillance within encephalitis surveillance systems
- Vector Control: Implementation of integrated vector management appropriate to local ecology
- Capacity Building: Strengthening laboratory and clinical diagnostic capabilities
- Intersectoral Collaboration: Coordination between health, agriculture, and environment sectors
Global Partnerships
International cooperation has accelerated progress in JE control:
- PATH’s Japanese Encephalitis Project: Supporting vaccine introduction and strengthening surveillance
- GAVI Alliance: Funding support for JE vaccine introduction in eligible countries
- WHO Collaborating Centers: Technical support for diagnosis, surveillance, and capacity building
- Bill & Melinda Gates Foundation: Support for research and vaccine development
- Regional Networks: Knowledge sharing and coordination across endemic countries
Research and Future Directions
Ongoing research aims to improve JE prevention, diagnosis, and treatment:
| Research Area | Current Developments | Potential Impact |
|---|---|---|
| Vaccine Development |
|
Improved vaccine coverage, reduced delivery costs, simplified schedules |
| Diagnostics |
|
Earlier detection, improved case management, better surveillance data |
| Treatment |
|
Reduced mortality and neurological sequelae |
| Vector Control |
|
Sustainable reduction in vector populations, reduced transmission |
- G – Governance and political commitment
- L – Local adaptation of strategies
- O – Ongoing surveillance and monitoring
- B – Broad vaccination coverage
- A – Agricultural practice modifications
- L – Linked interventions across sectors
