Community Health Nursing: Management of Acute Lower Respiratory Infections
Comprehensive notes for nursing students on assessment, management, and first aid approaches

A community health nurse providing respiratory care and education to a patient at home
Table of Contents
- Introduction to Acute Lower Respiratory Infections
- Standing Orders: Definition and Uses
- Screening and Diagnosis in Community Settings
- Acute Bronchitis: Assessment and Management
- Pneumonia: Assessment and Management
- Bronchial Asthma: Assessment and Management
- Hemoptysis: Assessment and Management
- Acute Chest Pain: Assessment and Management
- First Aid for Respiratory Emergencies
- Primary Care and Referral Guidelines
- Community-Based Interventions
- Global Best Practices
- References
Introduction to Acute Lower Respiratory Infections
Acute lower respiratory infections (ALRIs) are among the most common health problems encountered in community health nursing practice. These infections affect the airways and lungs below the level of the larynx, including the trachea, bronchi, bronchioles, and alveoli. Community health nurses play a vital role in early identification, management, and prevention of these respiratory conditions.
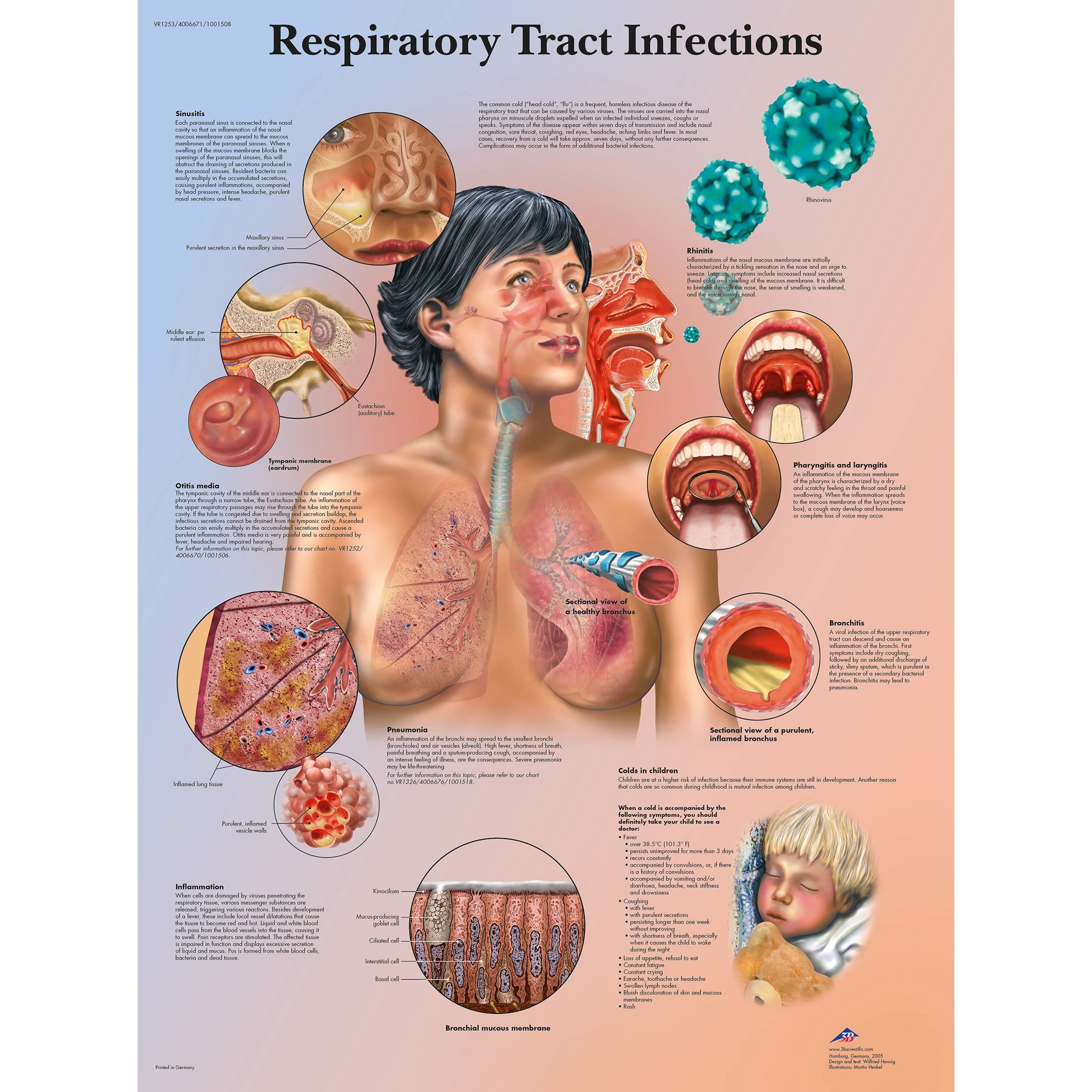
Diagram showing common respiratory tract infection sites
As a community health nurse, understanding the pathophysiology, clinical manifestations, and appropriate management strategies for each respiratory condition is crucial for providing quality care and preventing complications. This comprehensive guide focuses on five key respiratory conditions commonly encountered in community settings:
- Acute Bronchitis – Inflammation of the bronchial tubes
- Pneumonia – Infection of the lung parenchyma
- Bronchial Asthma – Chronic inflammatory airway disorder
- Hemoptysis – Expectoration of blood from the respiratory tract
- Acute Chest Pain – Pain that may be respiratory or cardiac in origin
Standing Orders: Definition and Uses
Definition:
Standing orders are written documents that authorize specific healthcare professionals (e.g., nurses) to carry out designated medical interventions for patient care without requiring a physician’s examination or direct order for each patient and each intervention.
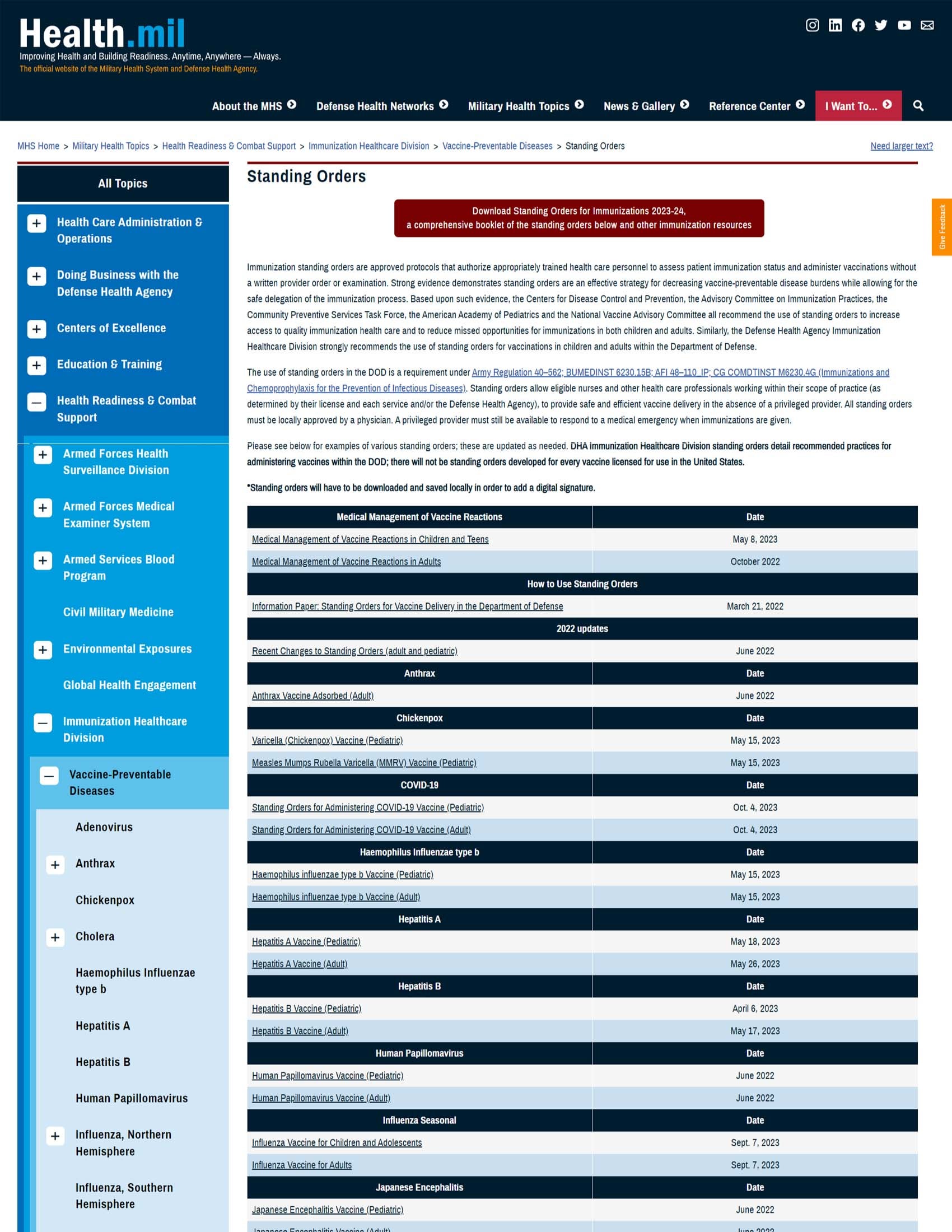
Key Uses of Standing Orders in Respiratory Care:
Assessment
- Authorize respiratory assessments including vital sign monitoring
- Allow for pulse oximetry measurements to evaluate oxygen saturation
- Permit peak flow measurements for asthma monitoring
- Enable respiratory rate and pattern assessment
Interventions
- Initiate oxygen therapy within specified parameters
- Administer prescribed respiratory medications
- Implement infection control measures
- Provide patient education on respiratory care
Screening and Prevention
- Conduct respiratory screenings and risk assessments
- Administer vaccines according to guidelines
- Perform tuberculosis screening
- Identify candidates for pulmonary rehabilitation
Documentation and Referral
- Document respiratory assessments and interventions
- Make appropriate referrals based on assessment findings
- Initiate emergency protocols when indicated
- Coordinate care with interdisciplinary team members
Purpose: To standardize respiratory assessment for patients presenting with respiratory symptoms in community settings.
Qualifying Patients: Adults and children presenting with cough, shortness of breath, wheezing, chest pain, or respiratory distress.
Authorized Personnel: Registered Nurses, Licensed Practical Nurses under RN supervision.
Procedures:
- Assess and document vital signs, including respiratory rate, heart rate, blood pressure, temperature, and oxygen saturation.
- Evaluate work of breathing, use of accessory muscles, and presence of retractions.
- Auscultate breath sounds in all lung fields and document findings.
- Assess for cough characteristics, sputum production, and presence of hemoptysis.
- For patients with asthma or COPD, measure peak expiratory flow rate as appropriate.
- Document findings and notify physician/advanced practice provider for:
- Respiratory rate >24 or <10 breaths/minute
- Oxygen saturation <92% on room air
- Presence of hemoptysis
- Significant respiratory distress
- Peak flow <50% of personal best for asthma patients
Screening and Diagnosis in Community Settings
Effective screening and early diagnosis of respiratory conditions are essential components of community health nursing practice. Implementing appropriate screening tools and diagnostic approaches helps identify at-risk individuals and facilitates timely intervention.
- Symptom-Based Screening: Questionnaires focusing on respiratory symptoms like cough, sputum production, dyspnea, and wheezing
- Risk Factor Assessment: Evaluation of smoking history, occupational exposures, family history, and environmental factors
- Spirometry: Objective measurement of lung function to detect airflow limitations
- Peak Flow Monitoring: Serial measurements to assess airflow variability in asthma
- Oxygen Saturation: Pulse oximetry to detect hypoxemia
- Clinical Assessment: Comprehensive history taking and physical examination
- Sputum Examination: Microscopy, culture, and sensitivity testing
- Chest X-ray: For suspected pneumonia or other lung pathologies
- Laboratory Tests: Complete blood count, C-reactive protein, procalcitonin
- Specialized Testing: Referral for specialized pulmonary function tests, bronchoscopy, or CT scans when indicated
B – Breathing pattern and rate
R – Respiratory effort and use of accessory muscles
E – Expectoration (sputum characteristics)
A – Auscultation findings (breath sounds)
T – Talking ability (ability to complete sentences)
H – Hypoxemia signs (cyanosis, oxygen saturation)
Community-Based Screening Guidelines
| Condition | Target Population | Screening Method | Frequency |
|---|---|---|---|
| Asthma | Individuals with recurrent respiratory symptoms, family history of asthma | Symptom questionnaire, peak flow monitoring, spirometry | As needed based on symptoms |
| COPD | Adults >40 years with smoking history, occupational exposures, or respiratory symptoms | Symptom questionnaire, spirometry | Annually for high-risk individuals |
| Pneumonia | High-risk individuals: elderly, immunocompromised, chronic disease | Clinical assessment, oxygen saturation monitoring | During respiratory illness episodes |
| Tuberculosis | High-risk groups: close contacts, immunocompromised, homeless | Tuberculin skin test, IGRA blood test | As per TB control guidelines |
Acute Bronchitis: Assessment and Management
Overview
Acute bronchitis is an inflammation of the bronchial tubes, typically presenting with a persistent cough. It is most commonly caused by viral infections (90-95% of cases) and is usually self-limiting, resolving within 1-3 weeks. Community health nurses play a key role in differentiating between viral bronchitis and bacterial infections requiring antibiotics.
Clinical Features
- Persistent cough, initially dry, later productive
- Mild fever (usually <38.5°C)
- Chest discomfort or soreness
- Fatigue and general malaise
- Wheezing or rhonchi on auscultation
- Sputum production (may be clear, white, yellow, or green)
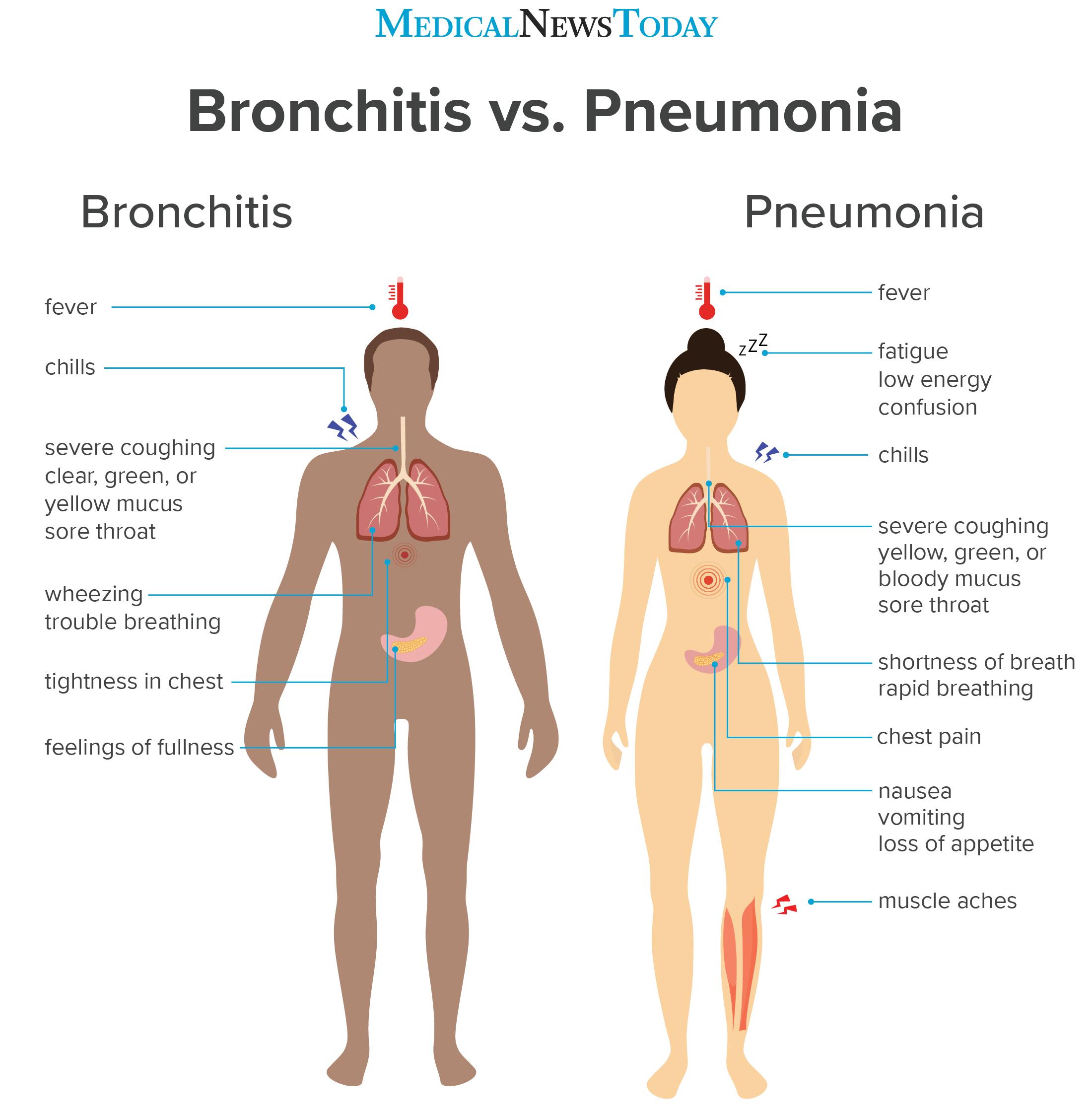
Comparative features of bronchitis and pneumonia
Respiratory Assessment
- Assess respiratory rate, rhythm, and depth
- Evaluate work of breathing and use of accessory muscles
- Auscultate breath sounds, noting presence of wheezes, rhonchi, or crackles
- Assess oxygen saturation via pulse oximetry
Cough Assessment
- Evaluate cough characteristics: dry vs. productive, frequency, timing
- Assess sputum: amount, color, consistency, presence of blood
- Determine triggers and relieving factors
General Assessment
- Monitor vital signs, especially temperature and respiratory rate
- Assess for signs of dehydration
- Evaluate activity tolerance and impact on daily activities
- Screen for risk factors for complications (age >65, immunocompromised state, chronic conditions)
Assessment:
- Perform comprehensive respiratory assessment
- Document vital signs, oxygen saturation, and breath sounds
- Assess hydration status and ability to manage secretions
Interventions:
- Provide education on supportive care measures:
- Adequate rest and hydration
- Humidity and proper positioning
- Avoidance of irritants (smoke, pollution)
- Administer antipyretics for fever as prescribed
- Implement cough management strategies
- Monitor for signs of deterioration or development of pneumonia
Referral Criteria:
- Temperature >38.5°C persisting >3 days
- Respiratory rate >24 breaths/minute
- Heart rate >100 beats/minute
- Oxygen saturation <94% on room air
- Symptoms not improving after 7-10 days
- Development of hemoptysis
C – Clear fluids and hydration
O – Oxygen saturation monitoring
U – Use of humidifier to moisten airways
G – Get adequate rest
H – Hand hygiene and infection control
Patient Education Points
Do’s
- Increase fluid intake to thin secretions
- Use a humidifier to moisturize air and ease breathing
- Rest adequately to support recovery
- Take over-the-counter pain relievers as directed for discomfort
- Use cough suppressants only at night if cough disrupts sleep
Don’ts
- Suppress productive cough during the day
- Expose yourself to smoke or other respiratory irritants
- Overexert yourself during the recovery period
- Expect or demand antibiotics for viral bronchitis
- Return to normal activities before adequately recovered
Pneumonia: Assessment and Management
Pneumonia is an infection that inflames the air sacs in one or both lungs, which may fill with fluid or pus. It can range from mild to life-threatening and is a significant cause of mortality, especially among vulnerable populations. Community health nurses are instrumental in early detection, appropriate referral, and community-based management of pneumonia.
Types of Pneumonia
| Type | Characteristics | Common Pathogens | Community Nursing Considerations |
|---|---|---|---|
| Community-Acquired Pneumonia (CAP) | Occurs outside healthcare settings; most common type | Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae | Focus on prevention through vaccination, early identification |
| Healthcare-Associated Pneumonia | Develops in individuals with frequent healthcare contact | Multi-drug resistant organisms, Gram-negative bacteria | Strict infection control, monitoring high-risk individuals |
| Aspiration Pneumonia | Results from inhalation of food, liquid, or vomit into lungs | Anaerobic bacteria, mixed oral flora | Swallowing assessment, positioning education for caregivers |
| Viral Pneumonia | Caused by respiratory viruses | Influenza, RSV, COVID-19 | Vaccination promotion, respiratory hygiene education |
Common Symptoms
- Fever, often high (>38.5°C)
- Productive cough with purulent sputum
- Shortness of breath or dyspnea
- Pleuritic chest pain
- Fatigue and malaise
- Decreased appetite
Physical Assessment Findings
- Increased respiratory rate (tachypnea)
- Decreased breath sounds over affected area
- Crackles (rales) on auscultation
- Bronchial breath sounds
- Tactile fremitus
- Dullness on percussion
Severity Assessment Tools
CURB-65 Score for Pneumonia Severity
1 point for each of the following:
- Confusion (new onset)
- Urea >7 mmol/L (BUN >19 mg/dL)
- Respiratory rate ≥30 breaths/minute
- Blood pressure (systolic <90 mmHg or diastolic ≤60 mmHg)
- Age ≥65 years
Interpretation:
- Score 0-1: Low risk, consider home treatment
- Score 2: Moderate risk, consider short hospital stay or supervised outpatient treatment
- Score ≥3: High risk, hospitalization recommended, consider ICU if score 4-5
Initial Assessment:
- Complete vital signs including respiratory rate, oxygen saturation, blood pressure, heart rate, and temperature
- Perform comprehensive respiratory assessment
- Calculate CURB-65 score to determine severity
- Assess risk factors for complications
Diagnostic Measures:
- Obtain sputum sample for culture and sensitivity when indicated
- Arrange for chest X-ray as ordered
- Coordinate blood work including CBC, BMP, and inflammatory markers
Interventions:
- Administer prescribed antibiotics according to guidelines
- Provide supplemental oxygen for SpO2 <92% as ordered
- Implement antipyretic measures for temperature >38.3°C
- Ensure adequate hydration
- Facilitate chest physiotherapy as appropriate
Monitoring and Follow-up:
- Schedule follow-up assessment within 24-48 hours for home-managed cases
- Monitor for clinical improvement (decreased fever, improved respiratory status)
- Assess medication adherence and effectiveness
- Evaluate nutritional status and fluid intake
Referral Criteria:
- CURB-65 score ≥2
- Oxygen saturation <90% on room air
- Inability to maintain oral intake
- Significant comorbidities compromising recovery
- Lack of appropriate home support
- Failure to improve after 48-72 hours of appropriate antibiotics
P – Position (semi-Fowler’s to facilitate breathing)
N – Nutrition and hydration support
E – Education on medication adherence
U – Utilize oxygen therapy if prescribed
M – Monitor vital signs and symptoms
O – Observe for deterioration signs
N – Note response to antibiotics
I – Infection control practices
A – Activity as tolerated
Prevention Strategies in Community Settings
Vaccination
- Pneumococcal vaccines:
- PCV13 (Prevnar 13)
- PPSV23 (Pneumovax)
- Annual influenza vaccination
- COVID-19 vaccination as recommended
- Targeted vaccination campaigns for high-risk groups
Education and Lifestyle
- Respiratory hygiene education
- Smoking cessation programs
- Proper hand hygiene techniques
- Nutritional counseling for immune support
- Management of chronic conditions (diabetes, heart disease)
Bronchial Asthma: Assessment and Management
Bronchial asthma is a chronic inflammatory disorder of the airways characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and cough. Community health nurses play vital roles in asthma education, monitoring, and management to prevent exacerbations and promote optimal control.
- Chronic airway inflammation
- Bronchial hyperresponsiveness
- Reversible airflow obstruction
- Airway remodeling over time
- Mucus hypersecretion
- Allergens (dust mites, pollen, pet dander)
- Respiratory infections
- Exercise and cold air
- Air pollutants and irritants
- Certain medications (NSAIDs, beta-blockers)
- Stress and strong emotions
- Wheezing (usually expiratory)
- Cough (often worse at night)
- Chest tightness
- Shortness of breath
- Increased work of breathing
- Variable symptoms over time
Asthma Classification and Assessment
| Severity Classification | Symptom Frequency | Nighttime Symptoms | Lung Function | Activity Limitation |
|---|---|---|---|---|
| Intermittent | ≤2 days/week | ≤2 nights/month | FEV1 >80% predicted, normal between exacerbations | None |
| Mild Persistent | >2 days/week but not daily | 3-4 nights/month | FEV1 ≥80% predicted | Minor limitation |
| Moderate Persistent | Daily | >1 night/week | FEV1 60-80% predicted | Some limitation |
| Severe Persistent | Throughout the day | Often 7 nights/week | FEV1 <60% predicted | Extremely limited |
Symptom Assessment
- Frequency and severity of symptoms
- Pattern and triggers of exacerbations
- Nighttime awakenings due to asthma
- Impact on daily activities and quality of life
- Response to current medications
Objective Assessment
- Peak expiratory flow rate (PEFR) monitoring
- Auscultation for wheezing, decreased breath sounds
- Signs of respiratory distress:
- Use of accessory muscles
- Nasal flaring
- Tripod positioning
- Inability to speak in complete sentences
- Oxygen saturation monitoring
Assessment:
- Perform asthma control assessment using validated tools (e.g., Asthma Control Test)
- Measure peak expiratory flow rate and compare to personal best
- Assess inhaler technique at each visit
- Evaluate medication adherence and barriers
Management:
- Administer prescribed medications according to asthma action plan
- Adjust medication dosages within prescribed parameters based on symptoms and PEFR readings
- Provide spacer devices for metered-dose inhalers as needed
- Initiate nebulizer treatments for acute symptoms as per protocol
Education:
- Review and update written asthma action plan
- Provide education on proper inhaler technique
- Teach early recognition of worsening symptoms
- Educate on environmental trigger identification and avoidance
Referral Criteria:
- PEFR <50% of personal best despite initial treatment
- Oxygen saturation <92% on room air
- Severe respiratory distress (inability to speak in sentences, use of accessory muscles)
- Poor response to initial bronchodilator therapy
- History of previous severe exacerbations requiring hospitalization
- Persistent poor asthma control despite appropriate therapy
Asthma Action Plan Components
Green Zone (Doing Well)
- No cough, wheeze, chest tightness, or shortness of breath
- Can perform usual activities
- PEFR 80-100% of personal best
- Action: Continue maintenance medications
Yellow Zone (Caution)
- Some symptoms (cough, wheeze, chest tightness)
- Waking at night due to asthma
- PEFR 50-80% of personal best
- Action: Add quick-relief medications, increase controller medication as directed
Red Zone (Medical Alert)
- Severe shortness of breath, difficulty speaking
- Quick-relief medications not helping
- PEFR <50% of personal best
- Action: Take prescribed emergency medications and seek immediate medical attention
A – Action plan development and review
S – Symptom monitoring and documentation
T – Trigger identification and avoidance
H – Healthcare coordination and follow-up
M – Medication technique and adherence
A – Activity and exercise guidance
- Help the person sit upright in a comfortable position
- Assist with their prescribed quick-relief inhaler (typically albuterol)
- Standard dosing: 2-4 puffs every 20 minutes for up to three treatments
- Use a spacer device if available
- Encourage slow, controlled breathing
- Remove potential triggers from the environment if possible
- Monitor response to treatment
- Call emergency services (911) if:
- No improvement after initial treatment
- Severe respiratory distress persists
- Difficulty speaking in complete sentences
- Lips or fingernails turning blue (cyanosis)
- Decreased level of consciousness
- Continue monitoring until emergency services arrive
Hemoptysis: Assessment and Management
Hemoptysis is the expectoration of blood originating from the respiratory tract below the level of the larynx. It ranges from blood-streaked sputum to massive hemorrhage and requires careful assessment and management by community health nurses to identify underlying causes and prevent complications.
Common Causes
- Infections: Bronchitis, pneumonia, tuberculosis, lung abscess
- Cardiovascular: Pulmonary embolism, mitral stenosis, pulmonary hypertension
- Neoplastic: Lung cancer, bronchial adenoma
- Inflammatory: Bronchiectasis, vasculitis
- Traumatic: Pulmonary contusion, foreign body
- Iatrogenic: Anticoagulation therapy, procedures
Classification
- Mild hemoptysis: <100 mL/24 hours
- Moderate hemoptysis: 100-400 mL/24 hours
- Massive hemoptysis: >400 mL/24 hours (life-threatening)
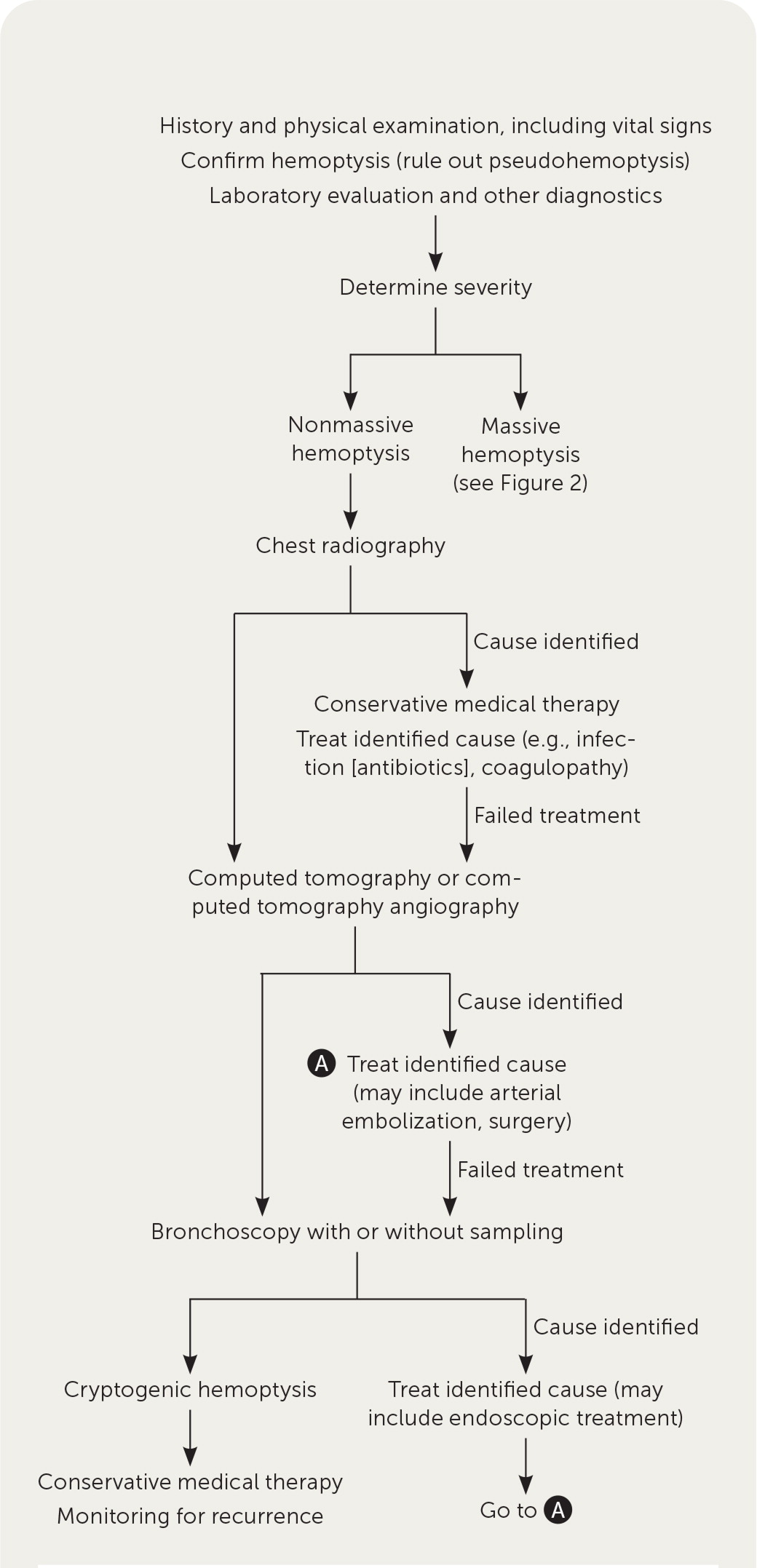
Diagnostic approach to hemoptysis
History Taking
- Quantity and characteristics of expectorated blood
- Duration and frequency of episodes
- Associated symptoms (fever, weight loss, chest pain)
- History of respiratory conditions
- Smoking history and occupational exposures
- Recent infections or trauma
- Medication history (especially anticoagulants)
Physical Assessment
- Vital signs, with focus on respiratory status
- Respiratory examination, including lung auscultation
- Assessment for signs of respiratory distress
- Evaluation of cardiovascular status
- Examination of sputum characteristics
- Observation for signs of hypoxemia
Initial Assessment:
- Measure vital signs, including oxygen saturation
- Assess quantity and characteristics of hemoptysis
- Evaluate respiratory status and work of breathing
- Determine patient’s hemodynamic stability
Initial Management:
- Position patient with bleeding side down (if known) to prevent aspiration into unaffected lung
- Provide supplemental oxygen to maintain SpO2 >92%
- Establish intravenous access if moderate to severe hemoptysis
- Collect sputum specimens for laboratory analysis
- Administer prescribed antitussives for non-productive cough
Immediate Referral Criteria:
- Massive hemoptysis (>100 mL at one time or >400 mL/24 hours)
- Respiratory distress or hypoxemia (SpO2 <90%)
- Hemodynamic instability (tachycardia, hypotension)
- Altered mental status
- Known or suspected malignancy
- Patient on anticoagulation therapy
Non-Urgent Referral Criteria:
- Recurrent hemoptysis, even if mild
- Hemoptysis persisting >1 week
- Risk factors for serious underlying disease (age >40, smoking history)
- Abnormal chest X-ray findings
- Help the person to a comfortable position, preferably sitting upright or lying on the affected side (if known)
- Remain calm and reassure the person
- Encourage the person to cough gently to clear airways
- Provide tissues and a container for bloody sputum
- Monitor vital signs, especially respiratory rate and effort
- Observe and document the amount and characteristics of blood expectorated
- For substantial bleeding:
- Call emergency services (911) immediately
- Maintain open airway
- Provide supplemental oxygen if available
- Monitor for signs of shock (pale, clammy skin, rapid pulse, decreasing consciousness)
- Do not give food or fluids if heavy bleeding is present
- Have the person avoid cough suppression for productive coughs, as clearing blood from airways is important
B – Bleeding amount and characteristics
L – Lung sounds and respiratory assessment
O – Oxygenation status
O – Onset and duration
D – Diagnostic considerations and referral
Patient Education for Hemoptysis
Home Management
- Avoid irritants that trigger coughing (smoke, pollution)
- Maintain adequate hydration
- Avoid strenuous activity during episodes
- Document frequency, amount, and appearance of blood
- Recognize warning signs requiring immediate attention
When to Seek Immediate Help
- Coughing up more than a few teaspoons of blood
- Difficulty breathing or shortness of breath
- Chest pain or discomfort
- Dizziness or lightheadedness
- Rapid heart rate or palpitations
- Blood in sputum with fever >38°C
Acute Chest Pain: Assessment and Management
Acute chest pain is a common presentation in community settings that requires prompt and systematic assessment to differentiate between potentially life-threatening conditions and less serious causes. Community health nurses must be skilled in recognizing patterns of chest pain that suggest specific underlying conditions, particularly respiratory versus cardiac origins.
Common Causes of Chest Pain
- Cardiac: Myocardial infarction, angina, pericarditis, aortic dissection
- Respiratory: Pneumonia, pleuritis, pneumothorax, pulmonary embolism
- Gastrointestinal: GERD, esophageal spasm, peptic ulcer disease
- Musculoskeletal: Costochondritis, muscle strain
- Psychological: Panic disorder, anxiety
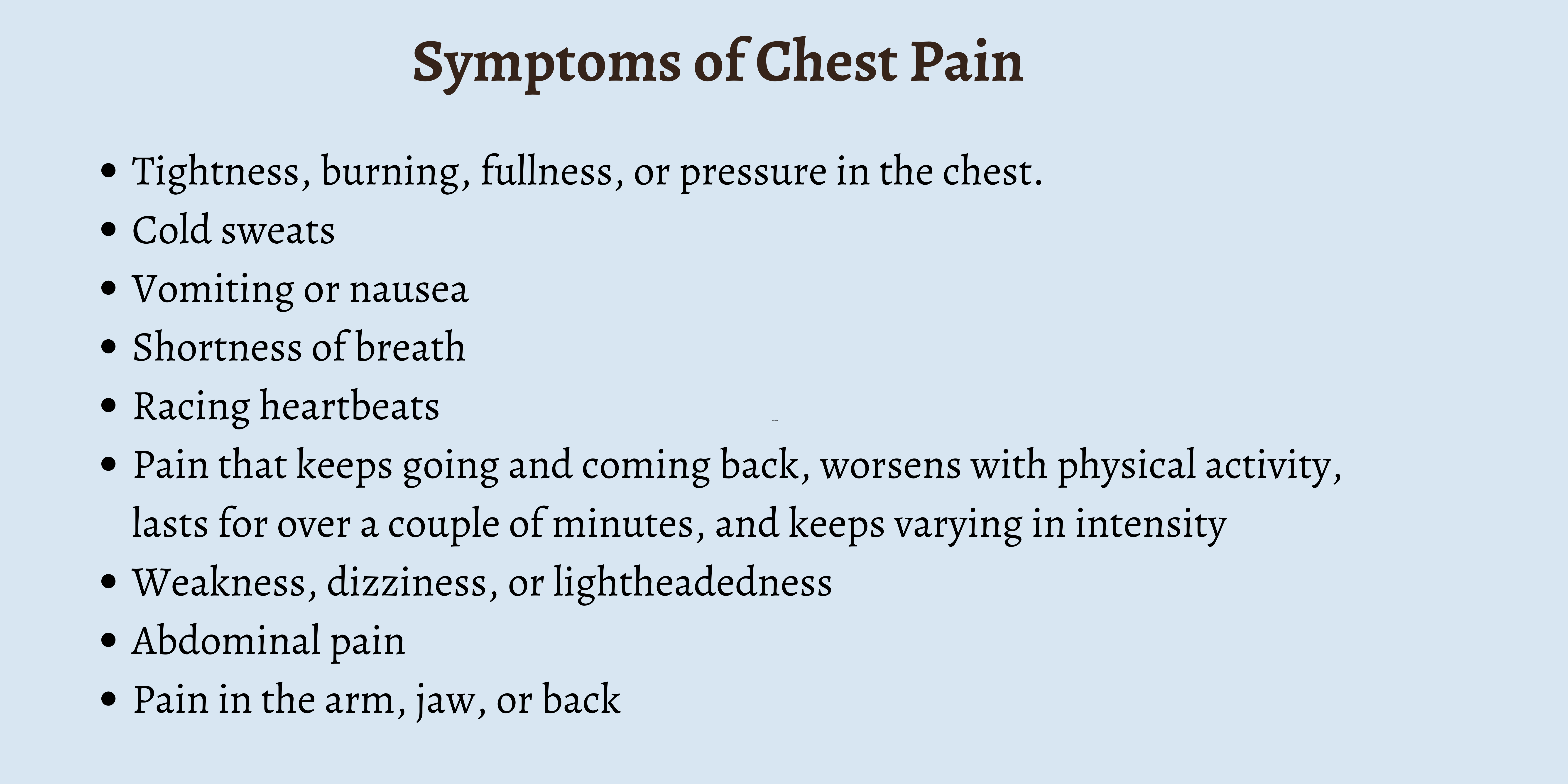
Common symptoms associated with different types of chest pain
Respiratory vs. Cardiac Chest Pain: Differential Features
| Feature | Respiratory Chest Pain | Cardiac Chest Pain |
|---|---|---|
| Quality | Sharp, stabbing, “knife-like” | Pressure, squeezing, “elephant sitting on chest” |
| Location | Localized, can point to specific spot | Diffuse, substernal, may radiate to arm/jaw/back |
| Relation to Breathing | Worse with inspiration (pleuritic) | Usually not affected by respiration |
| Relation to Position | May change with position | Usually not positional |
| Associated Symptoms | Cough, sputum, dyspnea, fever | Nausea, sweating, arm pain, jaw pain |
| Duration | Variable, may be constant | Usually 2-20 minutes, may be longer for MI |
PQRST Pain Assessment
- Provoke/Palliate: What makes it better or worse?
- Quality: What does it feel like?
- Region/Radiation: Where is it and does it spread?
- Severity: Rate pain on scale of 0-10
- Timing: When did it start? Constant or intermittent?
Focused Assessment
- Vital signs including oxygen saturation
- Respiratory assessment: rate, pattern, work of breathing
- Cardiovascular assessment: heart rate, rhythm, peripheral perfusion
- Lung auscultation for abnormal sounds
- Assessment for signs of respiratory distress
- Evaluation of risk factors for serious conditions
Initial Assessment:
- Perform comprehensive chest pain assessment using PQRST method
- Obtain vital signs including temperature, pulse, respiration, blood pressure, and oxygen saturation
- Complete focused cardiopulmonary assessment
- Assess level of distress and severity of symptoms
Immediate Actions for Suspected Cardiac Chest Pain:
- Place patient in position of comfort, typically semi-reclined
- Administer aspirin 325mg (chewed) if no contraindications
- Administer nitroglycerin 0.4mg SL if available and SBP >90mmHg
- Provide supplemental oxygen for SpO2 <94%
- Initiate cardiac monitoring if available
- Arrange immediate emergency transport
Actions for Suspected Respiratory Chest Pain:
- Position for comfort, typically upright or leaning forward
- Administer prescribed respiratory medications as indicated
- Provide supplemental oxygen for SpO2 <92%
- Monitor respiratory rate and effort
- Assess for signs of pneumothorax or severe pathology
Referral Criteria:
- Any chest pain with concerning features (radiation, diaphoresis, nausea, shortness of breath)
- Chest pain in patients with cardiac risk factors
- Pleuritic chest pain with respiratory distress, hypoxemia, or hemoptysis
- Sudden onset of severe, tearing chest pain (possible aortic dissection)
- Chest pain with syncope or near-syncope
- Persistent pain despite initial interventions
- Help the person stop any activity and rest in a comfortable position
- For suspected cardiac pain: Semi-reclined with head and shoulders supported
- For suspected respiratory pain: Upright or leaning forward to ease breathing
- Call emergency services (911) immediately for:
- Chest pain lasting more than a few minutes
- Pain radiating to jaw, neck, arms, or back
- Shortness of breath, sweating, nausea with chest pain
- Known heart condition with new or changed chest pain
- If the person has prescribed nitroglycerin:
- Help them take one dose as prescribed
- Wait 5 minutes; if pain persists, they may take a second dose
- Wait another 5 minutes; if pain still persists, they may take a third dose
- If pain continues after three doses, maintain emergency response
- If the person has prescribed aspirin and heart attack is suspected, help them take one adult aspirin (325 mg) or 4 low-dose aspirin (81 mg each) – chewed for faster absorption
- Loosen any tight clothing
- Monitor and record vital signs if possible
- Keep the person calm and reassured
- If the person becomes unresponsive and is not breathing normally, begin CPR
C – Characteristics of pain (quality, location, radiation)
H – History of cardiac or respiratory conditions
E – Exacerbating and relieving factors
S – Severity and associated symptoms
T – Timing and duration of pain
First Aid for Respiratory Emergencies
Community health nurses must be equipped with essential first aid skills for respiratory emergencies. These skills are not only crucial for direct patient care but also important to teach to patients, families, and community members to enable appropriate initial responses to respiratory distress situations.
- Position the person appropriately: Generally upright or semi-reclined position to facilitate breathing
- Ensure open airway: Clear visible obstructions, proper positioning
- Assess breathing quality: Rate, depth, work of breathing
- Provide reassurance: Calm, clear communication to reduce anxiety
- Monitor for changes: Ongoing assessment of respiratory status and response to interventions
- Know when to escalate care: Recognition of signs requiring emergency medical services
First Aid for Specific Respiratory Emergencies
- Help the person sit upright, leaning slightly forward with arms supported
- Ensure there is good air circulation (open window if appropriate)
- Loosen tight clothing around neck, chest, and waist
- Help administer any prescribed emergency medications (e.g., rescue inhaler)
- Encourage slow, controlled breathing (in through nose, out through pursed lips)
- Call emergency services if:
- Person is unable to speak in complete sentences
- Lips or fingernails appear blue
- Nostrils flare with each breath
- Person is using accessory muscles to breathe
- No improvement after using prescribed medications
For Conscious Adult or Child (>1 year):
- Determine if airway is completely blocked (unable to speak, cough, or breathe)
- If partial obstruction with good air exchange, encourage coughing
- For complete obstruction, perform abdominal thrusts (Heimlich maneuver):
- Stand behind the person with arms around their waist
- Make a fist with one hand and place it just above the navel
- Grasp fist with other hand and press inward and upward with quick thrusts
- Continue until object is expelled or person becomes unconscious
- If person becomes unconscious, begin CPR
- Check responsiveness by tapping and shouting
- If unresponsive, call for emergency help immediately
- Open the airway using head-tilt, chin-lift method
- Check for breathing (look, listen, feel) for no more than 10 seconds
- If not breathing or only gasping:
- Give two rescue breaths, each lasting one second
- Ensure chest rises with each breath
- If chest doesn’t rise, reposition head and try again
- Begin chest compressions if no pulse
- Continue CPR (30 compressions: 2 breaths) until help arrives
- Help the person find a comfortable position
- Speak calmly and reassuringly
- Encourage slow, controlled breathing:
- Breathe in slowly through nose for 4 counts
- Hold breath for 1-2 counts
- Exhale slowly through pursed lips for 6 counts
- Help them focus on a specific object or your voice
- Suggest rebreathing into cupped hands or paper bag if needed
- Seek medical attention if:
- Symptoms don’t improve within a few minutes
- Person has history of heart or lung problems
- This is their first episode of hyperventilation
R – Recognize signs of respiratory distress
E – Ensure proper positioning
S – Support with prescribed medications
C – Call for help when needed
U – Utilize calming techniques
E – Evaluate response continuously
Community Education on Respiratory First Aid
Essential Topics to Cover
- Recognition of respiratory distress
- Basic airway management
- When and how to use rescue medications
- Proper positioning techniques
- When to call emergency services
- Recovery position for unconscious breathing persons
Target Audiences
- Family members of respiratory patients
- School personnel and daycare workers
- Community groups and organizations
- Workplace first aid responders
- Caregivers of elderly or chronically ill
- Patients with chronic respiratory conditions
Teaching Methods
- Hands-on demonstrations
- Simulation scenarios
- Visual aids and handouts
- Return demonstration by participants
- Video-based learning
- Mobile apps with first aid guidance
Primary Care and Referral Guidelines
Community health nurses serve as critical links between patients and various levels of healthcare services. Understanding when to manage respiratory conditions in primary care settings and when to refer for specialized care is essential for optimal patient outcomes.
The following respiratory conditions can typically be managed in primary care or community settings with appropriate protocols:
Conditions Suitable for Primary Care
- Uncomplicated acute bronchitis
- Mild to moderate asthma with good control
- Stable chronic bronchitis
- Mild community-acquired pneumonia in low-risk patients
- Minor hemoptysis with known cause
- Non-cardiac chest pain with clear cause
Primary Care Interventions
- Clinical assessment and monitoring
- Patient and family education
- Medication management and optimization
- Preventive services (vaccinations)
- Basic pulmonary function testing
- Self-management support
Referral Guidelines by Condition
| Condition | Urgent Referral Criteria | Non-Urgent Referral Criteria | Referral Destination |
|---|---|---|---|
| Acute Bronchitis |
|
|
|
| Pneumonia |
|
|
|
| Bronchial Asthma |
|
|
|
| Hemoptysis |
|
|
|
| Chest Pain |
|
|
|
R – Risk factors evaluation
E – Extent and severity of symptoms
F – Failed initial management
E – Exacerbating conditions present
R – Resources needed beyond primary care
Essential Information for Effective Referrals:
- Patient Demographics: Full name, contact information, date of birth, and insurance details
- Clinical Summary: Concise history of present illness, relevant past medical history, and current medications
- Assessment Findings: Vital signs, physical examination results, laboratory data, and diagnostic studies
- Interventions to Date: Treatments initiated, medications prescribed, and patient response
- Reason for Referral: Clear statement of the clinical question or reason for specialty consultation
- Urgency Level: Indication of whether the referral is urgent, semi-urgent, or routine
- Special Considerations: Language needs, transportation issues, or other social factors
Community-Based Interventions
Community health nurses implement various interventions beyond individual patient care to address respiratory health at the population level. These interventions focus on prevention, early detection, and management of respiratory conditions across the community.
- Vaccination Campaigns:
- Influenza vaccination clinics
- Pneumococcal vaccination programs
- COVID-19 vaccination initiatives
- Smoking Cessation Programs:
- Group counseling sessions
- Individual coaching
- Nicotine replacement therapy access
- Environmental Health:
- Air quality monitoring
- Indoor air quality assessments
- Occupational exposure reduction
- Public Health Campaigns:
- Respiratory infection prevention
- Early warning signs recognition
- Seasonal respiratory health tips
- School Programs:
- Asthma education for students and staff
- Hand hygiene and respiratory etiquette
- Emergency response training
- Community Workshops:
- Respiratory first aid training
- Home environment assessment
- Medication management education
- Support Groups:
- Asthma support networks
- COPD management groups
- Caregiver support circles
- Home Visiting Programs:
- Environmental trigger assessment
- Medication adherence support
- Self-management skills building
- Telehealth Initiatives:
- Remote symptom monitoring
- Virtual coaching sessions
- Digital action plan management
Implementing Community-Based Screening Programs
Program Planning
- Identify target population based on risk factors
- Select appropriate screening tools and parameters
- Establish referral pathways for positive findings
- Develop data collection and follow-up systems
- Secure resources and establish partnerships
Implementation Strategies
- Conduct outreach to target populations
- Train staff in screening protocols
- Provide education during screening events
- Ensure privacy and confidentiality
- Create welcoming and accessible environments
Screening Tools and Approaches
- Symptom Questionnaires: Standardized tools to assess respiratory symptoms
- Spirometry: Basic lung function testing to detect airflow limitations
- Peak Flow Monitoring: To identify variable airflow obstruction
- Pulse Oximetry: To detect decreased oxygen saturation
- Risk Assessment Tools: To identify individuals at high risk for respiratory conditions
Evaluating Community Interventions
| Evaluation Domain | Indicators | Data Collection Methods |
|---|---|---|
| Process Measures |
|
|
| Outcome Measures |
|
|
| Impact Measures |
|
|
Global Best Practices in Community Respiratory Care
Community health nursing approaches to respiratory conditions vary worldwide, with innovative models and best practices emerging from different healthcare systems. Understanding these global perspectives can enrich local practice and provide inspiration for program development.
Finland’s Asthma Program
Finland implemented a comprehensive national asthma program focused on early diagnosis and effective management at the primary care level, resulting in significant reductions in hospitalizations and costs.
Key Components:
- Designated asthma coordinators in primary healthcare centers
- Standardized diagnosis and treatment guidelines
- Emphasis on guided self-management
- Continuous education for healthcare professionals
- Regular follow-up and adjustment of treatment plans
Outcomes: 54% reduction in asthma-related hospital days, 69% reduction in emergency visits, and reduced per-patient costs despite increased medication use.
Australia’s Indigenous Respiratory Outreach Care
Australia developed specialized respiratory outreach services for Indigenous communities with culturally appropriate care models and integration of traditional approaches with modern medicine.
Key Components:
- Community-based Indigenous healthcare workers
- Mobile spirometry and diagnostic services
- Culturally adapted education materials
- Integration with traditional healing practices
- Telehealth connections to specialist services
Outcomes: Increased screening rates, improved early diagnosis, better treatment adherence, and reduced disparities in respiratory health outcomes.
United Kingdom’s Community Respiratory Teams
The UK has implemented specialized community respiratory teams that provide home-based assessment, management, and rehabilitation for patients with chronic respiratory conditions.
Key Components:
- Multidisciplinary teams (nurses, physiotherapists, respiratory specialists)
- Hospital admission avoidance programs
- Early supported discharge services
- Home-based pulmonary rehabilitation
- Integrated care pathways with hospital and primary care
Outcomes: 20-30% reduction in hospital readmissions, improved quality of life scores, and cost savings of approximately £1,500 per patient.
Brazil’s Family Health Strategy
Brazil’s comprehensive primary care model integrates respiratory care into family health teams that serve defined geographic areas, with an emphasis on prevention and continuity of care.
Key Components:
- Community health agents conducting home visits
- Standardized respiratory care protocols
- Integration of TB control with primary care
- Group education sessions on respiratory health
- Electronic health records for continuity of care
Outcomes: Increased case detection of TB and other respiratory conditions, higher vaccination rates, and improved management of chronic respiratory diseases.
Innovative Approaches Worth Considering
Digital Health Solutions
- Mobile apps for symptom monitoring
- Electronic action plans with alerts
- Remote consultations for rural communities
- Wearable devices for continuous monitoring
- Air quality monitoring and alert systems
Community Health Worker Models
- Peer educators with lived experience
- Home environmental assessments
- Cultural and linguistic bridging
- Medication adherence support
- Social support coordination
Integrated Care Approaches
- Shared care protocols between primary and specialty care
- One-stop respiratory assessment clinics
- Pharmacy-based monitoring programs
- School-based asthma management
- Workplace respiratory health programs
- Clearly defined roles and responsibilities for all healthcare team members
- Standardized assessment tools and protocols to ensure consistent care
- Strong community engagement and participation in program design
- Cultural competence and adaptation to local contexts
- Robust data collection and evaluation for continuous improvement
- Sustainable funding mechanisms and resource allocation
- Integrated approach addressing social determinants of respiratory health
- Continuous education for healthcare providers and community members
- Clear referral pathways and communication between care levels
- Patient-centered design with emphasis on self-management support
References
- American Academy of Family Physicians. (2022). Hemoptysis: Evaluation and Management. American Family Physician, 105(2), 144-151. https://www.aafp.org/pubs/afp/issues/2022/0200/p144.html
- American Academy of Family Physicians. (2005). Hemoptysis: Diagnosis and Management. American Family Physician, 72(7), 1253-1260. https://www.aafp.org/pubs/afp/issues/2005/1001/p1253.html
- Centers for Disease Control and Prevention. (2024). Best Practices for Patient Care: Respiratory Illnesses. https://www.cdc.gov/respiratory-viruses/hcp/clinical-safety/index.html
- Healthline. (2022). How Asthma Affects Your Respiratory System. https://www.healthline.com/health/asthma/how-does-asthma-affect-the-respiratory-system
- Immunize.org. (2024). Clinical Resources: Standing Orders Templates. https://www.immunize.org/clinical/topic/standing-orders-templates/
- Mayo Clinic. (2024). Chest pain: First aid. https://www.mayoclinic.org/first-aid/first-aid-chest-pain/basics/art-20056705
- Medical News Today. (2019). Lower respiratory tract infection: Symptoms, diagnosis, and treatment. https://www.medicalnewstoday.com/articles/324413
- National Center for Biotechnology Information. (2024). Acute Bronchitis – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448067/
- National Center for Biotechnology Information. (2023). Acute Chest Syndrome – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK441872/
- National Center for Biotechnology Information. (2024). Asthma (Nursing) – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK568760/
- National Center for Biotechnology Information. (2024). Infections of the Respiratory System – Medical Microbiology. https://www.ncbi.nlm.nih.gov/books/NBK8142/
- National Center for Biotechnology Information. (2019). Acute lower respiratory tract infections: Symptoms, findings and management in primary care. https://pmc.ncbi.nlm.nih.gov/articles/PMC7034054/
- National Center for Biotechnology Information. (2015). Diagnosis and management of hemoptysis. https://pmc.ncbi.nlm.nih.gov/articles/PMC4463269/
- Nurseslabs. (2024). 6 Asthma Nursing Care Plans. https://nurseslabs.com/asthma-nursing-care-plans/
- Nurseslabs. (2024). 6 Chest Pain (Angina) Nursing Care Plan & Management. https://nurseslabs.com/angina-pectoris-chest-pain-nursing-care-plans/
- Red Cross. (2024). Respiratory Distress (Trouble Breathing). https://www.redcross.org/take-a-class/resources/learn-first-aid/respiratory-distress-trouble-breathing
- Temple Health. (2024). Lower Respiratory Tract Infections (LRTI). https://www.templehealth.org/services/conditions/lower-respiratory-tract-infections
- Temple Health. (2024). Hemoptysis (Coughing Up Blood). https://www.templehealth.org/services/conditions/hemoptysis-coughing-up-blood
- University of California San Francisco. (2024). Standing Orders. Center for Excellence in Primary Care. https://cepc.ucsf.edu/standing-orders
- World Health Organization. (2024). Chronic respiratory diseases. https://www.who.int/health-topics/chronic-respiratory-diseases
