Master Oral, Sublingual, & Buccal Medication Administration
Unlock Flawless Administration Techniques for Nurses
Evidence-Based • Interactive • Student-Focused
Introduction to Medication Administration Mastery
Medication administration represents one of the most critical responsibilities in nursing practice, directly impacting patient outcomes and safety. Understanding the nuances of oral, sublingual, and buccal routes ensures optimal therapeutic effects while minimizing adverse reactions. This comprehensive guide empowers nursing students with evidence-based techniques, safety protocols, and practical mnemonics to master medication administration across these essential routes.
Oral Route
Most common medication administration method with systematic absorption
Sublingual Route
Rapid absorption under the tongue for emergency medications
Buccal Route
Absorption through cheek tissues for sustained release
Effective medication administration requires comprehensive understanding of anatomical structures, pharmacokinetics, patient assessment, and safety protocols. Each route offers unique advantages and considerations that directly influence therapeutic outcomes. Professional nurses must develop expertise in selecting appropriate administration techniques based on medication properties, patient conditions, and clinical objectives.
Oral Cavity Anatomy for Medication Administration
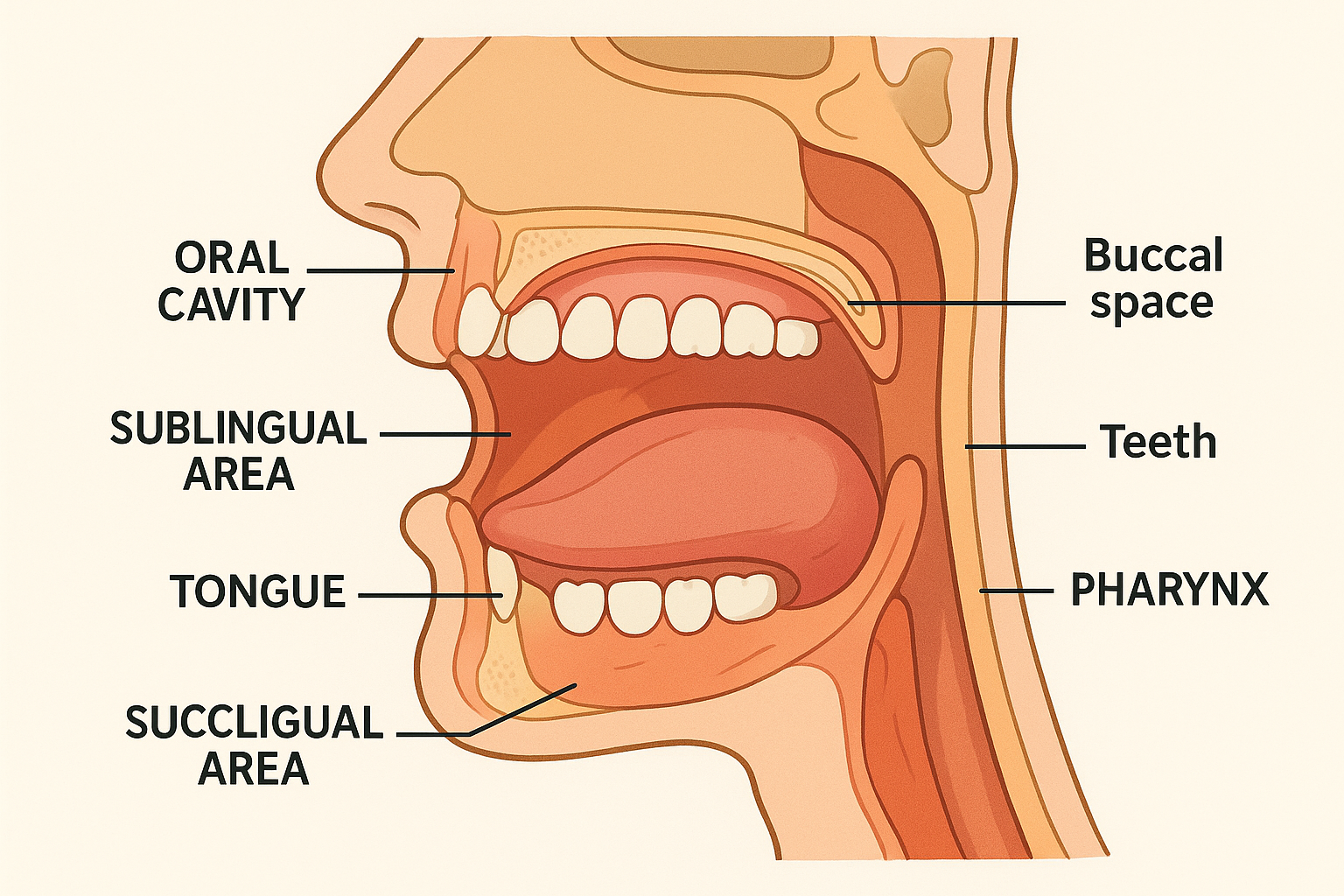
Cross-sectional view of oral cavity anatomy highlighting key areas for medication administration
Key Anatomical Landmarks
-
Oral Cavity: Primary space for conventional tablet and liquid administration
-
Sublingual Area: Highly vascularized region beneath the tongue
-
Buccal Pouch: Space between cheek and gum for sustained absorption
-
Salivary Glands: Major, minor, and parotid glands affecting dissolution
Memory Aid: “ORAL”
Clinical Significance
Understanding oral anatomy is fundamental for safe medication administration. The rich blood supply in sublingual and buccal areas enables rapid systemic absorption, bypassing first-pass hepatic metabolism. This anatomical knowledge guides route selection, timing considerations, and patient positioning during administration procedures.
Oral Medication Administration Mastery
Overview and Advantages
Oral administration represents the most frequently used medication route in clinical practice, accounting for approximately 80% of all medication administration events. This route offers convenience, patient compliance, and cost-effectiveness while maintaining therapeutic efficacy for most medications.
Step-by-Step Technique
Tablets & Capsules
- • Ensure adequate fluid intake (150-200ml)
- • Check for enteric coating before crushing
- • Monitor for choking in elderly patients
- • Consider alternative forms for swallowing difficulties
Liquid Medications
- • Use appropriate measuring devices
- • Shake suspensions thoroughly
- • Administer slowly to prevent aspiration
- • Check for drug interactions with food
Special Formulations
- • Effervescent tablets require dissolution
- • Sublingual tablets should not be swallowed
- • Extended-release forms must remain intact
- • Chewable forms require complete mastication
Critical Safety Considerations
Contraindications:
- • Unconscious or sedated patients
- • Severe dysphagia or swallowing disorders
- • Nausea and vomiting
- • Gastric obstruction or surgery
Monitoring Parameters:
- • Onset of therapeutic effects
- • Gastrointestinal adverse reactions
- • Drug-food interactions
- • Patient compliance and adherence
Sublingual Medication Administration Excellence
Memory Technique: “UNDER”
Pharmacokinetics
Common Medications
- • Nitroglycerin for angina
- • Sublingual immunotherapy
- • Lorazepam for anxiety
- • Ondansetron for nausea
- • Buprenorphine for pain
- • Emergency hormone preparations
Key Advantages
- • Bypasses first-pass metabolism
- • Rapid therapeutic onset
- • Useful during emergencies
- • Patient can self-administer
- • Non-invasive delivery method
- • Effective in nauseous patients
Detailed Administration Procedure
Pre-Administration:
- Verify patient identification using two identifiers
- Explain procedure and expected effects to patient
- Assess oral cavity for lesions or inflammation
- Position patient comfortably in upright position
- Ensure patient has not eaten or drunk recently
During Administration:
- Use clean technique when handling medication
- Instruct patient to lift tongue
- Place tablet under tongue on either side
- Advise patient to keep mouth closed
- Monitor for complete dissolution (5-10 minutes)
Critical Teaching Points
Patient Instructions:
- • Do not chew, swallow, or move tablet
- • Avoid talking during dissolution
- • Do not eat or drink for 15 minutes
- • Report any unusual taste or irritation
Nurse Monitoring:
- • Watch for signs of therapeutic response
- • Monitor vital signs as appropriate
- • Document time of administration
- • Assess for any adverse reactions
Buccal Medication Administration Proficiency
Understanding Buccal Administration
Buccal administration involves placing medications between the gum and cheek, allowing absorption through the buccal mucosa. This route provides sustained drug delivery with excellent bioavailability while avoiding gastrointestinal degradation and hepatic first-pass metabolism.
Key Characteristics:
- • Rich blood supply enables rapid absorption
- • Sustained release over 2-6 hours
- • Ideal for hormone and pain management
- • Patient-controlled administration possible
Anatomical Placement
Pro Tip: The upper buccal area typically provides better retention and comfort for most patients.
Memory Device: “CHEEK”
Common Medications
- • Testosterone replacement therapy
- • Fentanyl for breakthrough pain
- • Prochlorperazine for nausea
- • Nicotine replacement products
- • Hormone replacement preparations
- • Local anesthetic agents
Timing Considerations
- • Complete dissolution: 30-60 minutes
- • Onset of action: 15-30 minutes
- • Peak effect: 1-3 hours
- • Duration: 4-6 hours typically
- • Avoid food/drink for 30 minutes
- • Rotate administration sites
Special Precautions
- • Assess for oral lesions or infections
- • Monitor for local irritation
- • Ensure proper tablet placement
- • Watch for excessive salivation
- • Document exact placement location
- • Teach patient proper technique
Step-by-Step Administration Protocol
Preparation Phase:
- Patient Assessment: Verify identity and assess oral cavity for integrity, lesions, or inflammation
- Equipment Preparation: Gather medication, gloves, and teaching materials as needed
- Education: Explain procedure, expected duration, and importance of keeping medication in place
Administration Phase:
- Positioning: Position patient comfortably with good access to buccal area
- Placement: Using clean technique, place medication between gum and cheek
- Monitoring: Ensure proper placement and provide ongoing patient support during dissolution
Universal Safety Guidelines for Medication Administration
The Five Rights of Medication Administration
Right Patient
Two patient identifiers
Right Drug
Triple check medication
Right Dose
Calculate accurately
Right Route
Verify administration path
Right Time
Follow scheduling guidelines
Pre-Administration Checklist
Post-Administration Monitoring
Absolute Contraindications
All Routes:
- • Known drug allergies
- • Expired medications
- • Incorrect patient identity
- • Unclear or illegible orders
Oral Route:
- • Unconscious patients
- • Severe dysphagia
- • Active vomiting
- • Nothing by mouth orders
Sublingual/Buccal:
- • Oral lesions or infections
- • Severe dry mouth
- • Inability to cooperate
- • Excessive salivation
Safety Mnemonic: “SAFE MEDS”
S – Stop
Stop and think before each administration
A – Assess
Assess patient condition and readiness
F – Five Rights
Follow the five rights consistently
E – Educate
Educate patient about medication
M – Monitor
Monitor for therapeutic and adverse effects
E – Evaluate
Evaluate patient response to medication
D – Document
Document administration and outcomes
S – Support
Support patient throughout process
Evidence-Based Best Practices for Medication Administration
Research-Supported Techniques
Barcode Medication Administration (BCMA)
Studies show 58% reduction in medication errors when implementing electronic verification systems during administration processes.
Double-Check Procedures
Independent double-checking reduces calculation errors by 95% for high-risk medications and complex dosing calculations.
Patient Engagement
Active patient involvement in medication reconciliation decreases adverse drug events by 67% in healthcare settings.
Quality Improvement Strategies
Interprofessional Collaboration
- • Pharmacist consultation for complex medications
- • Physician communication about patient response
- • Patient and family involvement in care planning
- • Multidisciplinary team rounds for high-risk patients
- • Regular medication reconciliation meetings
Error Prevention Strategies
- • Minimize interruptions during administration
- • Use standardized concentration guidelines
- • Implement fail-safe double-check systems
- • Maintain current drug reference resources
- • Practice mindful administration techniques
Professional Development
- • Annual competency assessments
- • Simulation-based learning opportunities
- • Peer mentoring and observation programs
- • Continuing education on new medications
- • Evidence-based practice integration
Innovation in Medication Administration
Emerging Technologies:
- • Smart pill technology with embedded sensors
- • Automated medication dispensing robots
- • Mobile apps for patient medication tracking
- • Artificial intelligence for drug interaction alerts
Future Directions:
- • Personalized medicine based on genetic profiles
- • Nanotechnology for targeted drug delivery
- • Wearable devices for continuous monitoring
- • Virtual reality training for complex procedures
Global Best Practices in Medication Administration
International Standards and Guidelines
Healthcare systems worldwide have developed sophisticated approaches to medication administration safety. These international best practices demonstrate evidence-based strategies for reducing errors and improving patient outcomes through systematic quality improvement initiatives.
World Health Organization (WHO) Guidelines:
- • High 5s initiative for medication safety
- • Look-alike sound-alike medication protocols
- • Patient safety checklists and verification
- • Global patient safety challenges
Leading Practice Examples
Singapore Model
Comprehensive electronic health records with integrated decision support systems reduce medication errors by 85% through real-time alerts and automated cross-referencing.
Netherlands Approach
National medication safety program emphasizes interprofessional education and standardized administration protocols across all healthcare facilities.
United Kingdom NHS
Australian Model
Canada Healthcare
Global Learning: “WORLD SAFE”
W – WHO Standards
World Health Organization safety guidelines
O – Open Communication
Open reporting and learning culture
R – Research Integration
Research-based practice improvements
L – Leadership Support
Leadership commitment to safety
D – Data Driven
Data-driven quality improvement
S – Standardization
Standardized processes and protocols
A – Advanced Technology
Advanced technology integration
F – Focused Education
Focused competency-based education
International Collaboration Benefits
Cross-border sharing of medication administration best practices has led to significant improvements in patient safety outcomes globally. Countries implementing comprehensive safety programs report 40-60% reductions in preventable medication errors and improved patient satisfaction scores.
Key Success Factors:
- • Executive leadership commitment to safety culture
- • Investment in technology infrastructure and training
- • Multidisciplinary collaboration and communication
- • Continuous monitoring and quality improvement
Measurable Outcomes:
- • 50% reduction in adverse drug events
- • 75% decrease in medication administration errors
- • 90% improvement in patient safety culture scores
- • 65% increase in staff confidence and satisfaction
Mastering Excellence in Medication Administration
Excellence in medication administration represents the cornerstone of safe, effective nursing practice. Through comprehensive understanding of oral, sublingual, and buccal routes, coupled with evidence-based safety protocols and global best practices, nursing professionals can confidently deliver optimal patient care while minimizing risks and maximizing therapeutic outcomes.
“Safe medication administration is not just a skill—it’s a professional commitment to excellence that directly impacts every patient we serve.”
Knowledge Integration
Combine anatomical understanding with pharmacological principles for optimal administration decisions
Safety Excellence
Implement systematic safety checks and error prevention strategies throughout the administration process
Patient-Centered Care
Engage patients as active partners in their medication therapy for improved outcomes and satisfaction
Key Takeaways for Nursing Practice
Clinical Excellence:
- • Master the unique characteristics of each administration route
- • Develop proficiency in patient assessment and route selection
- • Implement evidence-based safety protocols consistently
- • Maintain current knowledge of medications and interactions
Professional Growth:
- • Engage in continuous learning and competency validation
- • Participate in quality improvement and safety initiatives
- • Collaborate effectively with interprofessional team members
- • Advocate for patient safety and optimal therapeutic outcomes
Your Journey to Medication Administration Mastery
Armed with comprehensive knowledge, evidence-based techniques, and unwavering commitment to safety, you are prepared to deliver exceptional medication administration care. Remember that mastery is a continuous journey of learning, practice, and refinement. Each patient interaction offers an opportunity to apply these principles and contribute to optimal healthcare outcomes.
