Mental Status Examination
Comprehensive Nursing Assessment Guide
Introduction to Mental Status Examination
The Mental Status Examination (MSE) is a structured assessment of a patient’s psychological functioning at a specific point in time. As a core component of psychiatric and psychological assessment, it helps nursing professionals evaluate cognitive abilities, emotional states, thought patterns, and behavioral presentations of patients.
Clinical Pearl
The MSE is like a “psychiatric vital sign” – it provides a baseline and allows for tracking changes in mental status over time, making it an essential tool for ongoing patient care.
Unlike a physical examination that might use tools like a stethoscope or blood pressure cuff, the MSE primarily relies on your observational skills, interview techniques, and clinical judgment. It’s both a science and an art – combining structured assessment with intuitive observations.
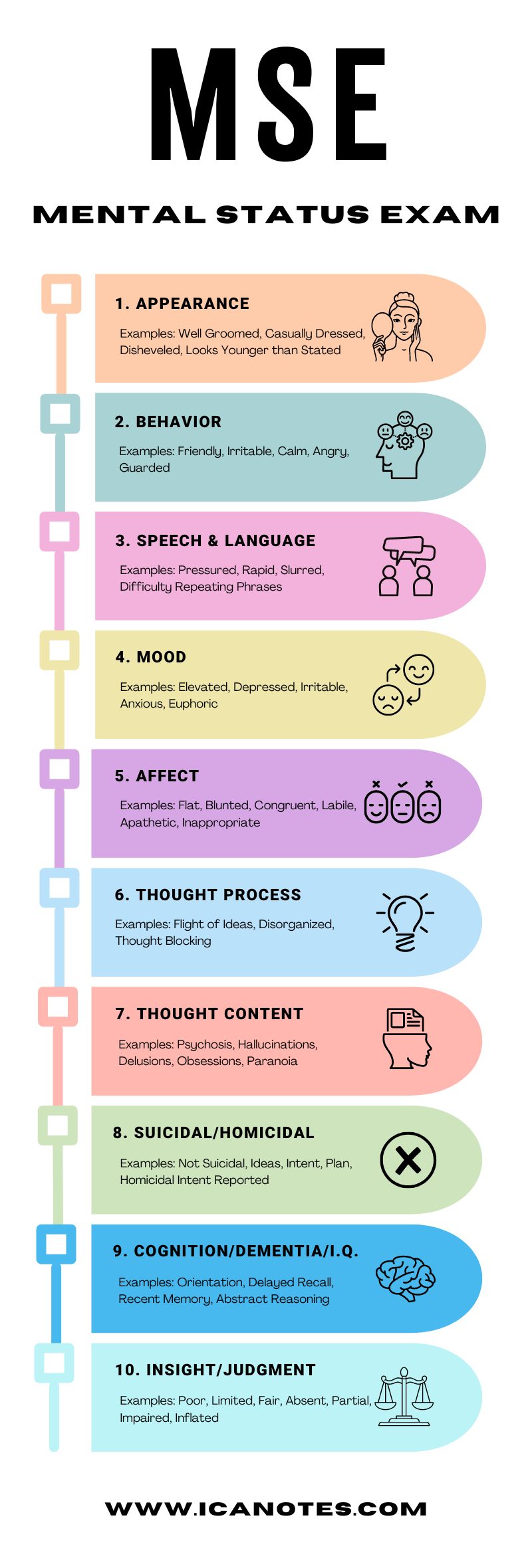
Figure 1: Components of Mental Status Examination
The MSE complements other aspects of patient evaluation, including:
- Patient history
- Physical examination
- Diagnostic testing
- Collateral information from family/caregivers
When conducted properly, the MSE helps distinguish between various psychiatric and neurological conditions, guides treatment decisions, and establishes a baseline for monitoring a patient’s progress.
MSE Mnemonics: Tools for Remembering
ASEPTIC Mnemonic
Use this mnemonic to remember the main components of the Mental Status Examination:
The patient’s physical appearance, dress, grooming, and behavioral presentation
Rate, volume, articulation, and coherence of speech
Mood (subjective) and affect (objective observation)
Presence of hallucinations, illusions, or perceptual disturbances
Thought process (form) and thought content
Understanding of one’s condition and ability to make sound decisions
Attention, concentration, memory, orientation, and abstract thinking
ABC STAMP LICK Mnemonic
An alternative, more detailed mnemonic that covers the comprehensive components:
Components of Mental Status Examination
Appearance and behavior assessment provides valuable clues about a patient’s overall psychological state. This component begins the moment you first see the patient.
What to Observe:
- Physical appearance: Hygiene, grooming, dress, apparent age vs. stated age
- Body language: Posture, facial expressions, eye contact
- Motor activity: Psychomotor agitation or retardation, tremors, tics
- Behavior: Cooperative, guarded, hostile, withdrawn, dramatic
- Level of consciousness: Alert, drowsy, lethargic, stuporous, comatose
| Clinical Observation | Potential Indication |
|---|---|
| Poor hygiene/self-care | Depression, schizophrenia, dementia |
| Psychomotor retardation | Depression, sedative effects, neurological disorders |
| Psychomotor agitation | Anxiety, mania, stimulant use, akathisia |
| Bizarre or inappropriate dress | Schizophrenia, mania, dementia |
| Disheveled but expensive clothing | Recent decline in functioning (e.g., sudden onset conditions) |
Documentation Tip
Document observations objectively without interpretation. For example, instead of writing “patient looks depressed,” document “patient has poor eye contact, stooped posture, and minimal facial expression.”
Speech assessment provides insights into thought processes and potential neurological issues. Listen carefully not just to what is said, but how it is said.
What to Observe:
- Rate: Fast, slow, normal, pressured
- Volume: Loud, soft, whispered, normal
- Quantity: Verbose, limited, poverty of speech, mutism
- Fluency: Articulate, slurred, stammering, cluttering
- Prosody: Melodic quality, inflection, monotone
| Speech Pattern | Description | Potential Association |
|---|---|---|
| Pressured speech | Rapid, increased volume, difficult to interrupt | Mania, anxiety, stimulant use |
| Poverty of speech | Brief, empty replies with minimal elaboration | Depression, schizophrenia (negative symptoms) |
| Dysarthria | Slurred speech, impaired articulation | Neurological disorders, intoxication |
| Monotonous speech | Lack of inflection or emotional expression | Depression, Parkinson’s disease |
| Mutism | Complete absence of speech | Catatonia, severe depression, selective mutism |
Clinical Alert
Sudden speech changes may indicate neurological emergencies like stroke. If accompanied by facial droop or weakness, initiate emergency protocols immediately.
Mood and affect assessment helps understand a patient’s emotional state. Though related, they represent different aspects of emotional presentation.
Key Distinction
Mood
The patient’s subjective emotional state as reported by them. Document using patient’s own words.
Example: “I feel hopeless and empty.”
Affect
The objective observation of the patient’s emotional expression as observed by the clinician.
Example: “Patient displayed a flat affect with minimal facial expression.”
Affect Descriptors:
- Range: Full, restricted, blunted, flat
- Appropriateness: Congruent or incongruent with content
- Stability: Stable, labile (rapidly shifting)
- Quality: Euthymic, dysphoric, euphoric, irritable, anxious
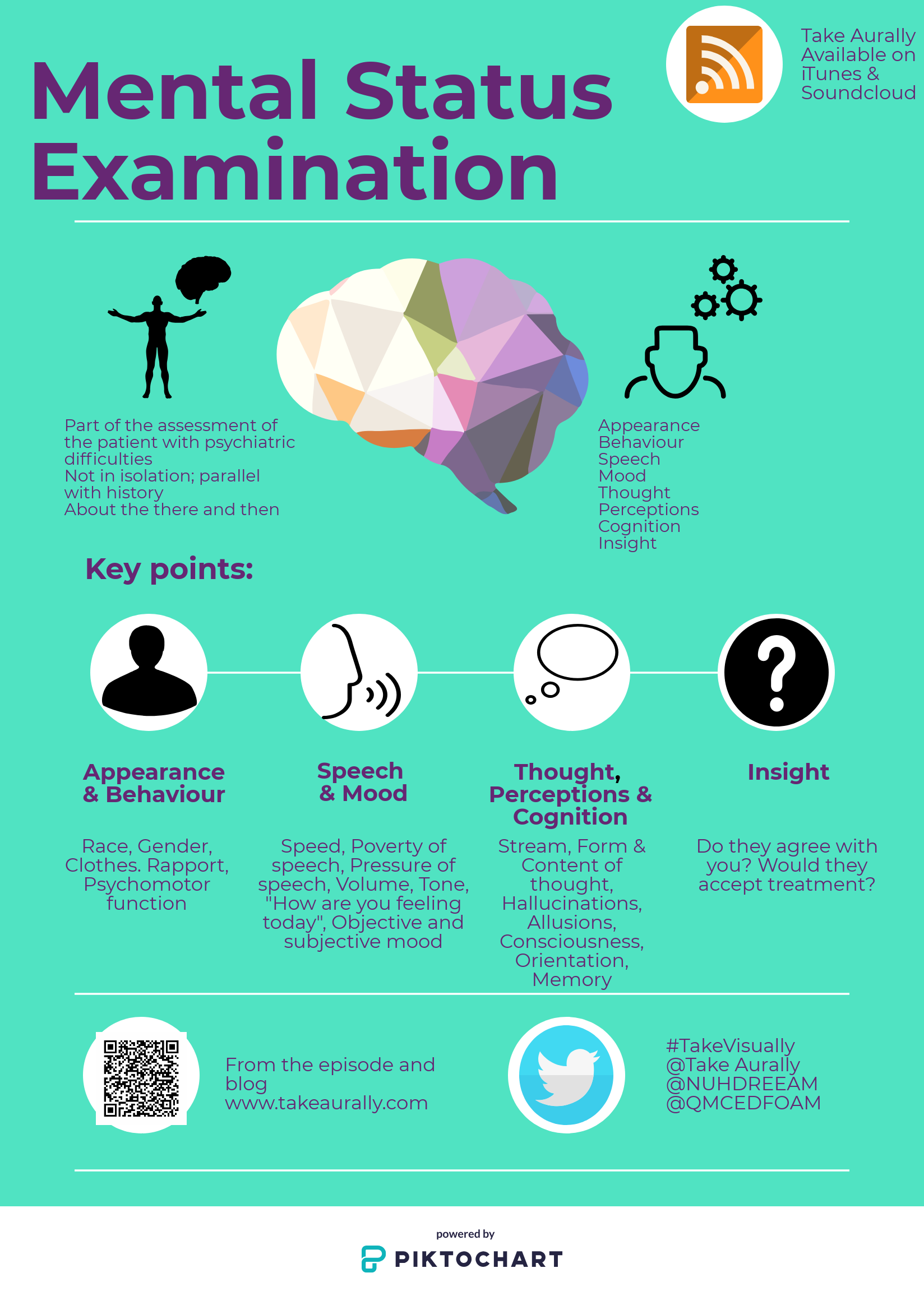
Figure 2: Mood and Affect Assessment Spectrum
Assessment Technique
Ask open-ended questions about mood such as “How have you been feeling lately?” rather than leading questions like “Have you been feeling sad?” The latter may bias the patient’s response.
Thought assessment evaluates how a patient organizes their thoughts (process) and what they are thinking about (content). This component helps identify thought disorders and potential safety concerns.
Thought Process
How thoughts are organized and connected:
- Linear: Logical, goal-directed
- Circumstantial: Includes excessive details but eventually returns to point
- Tangential: Digresses without returning to original point
- Flight of ideas: Rapidly shifting between unrelated topics
- Loose associations: Disconnected, illogical thoughts
- Thought blocking: Sudden interruption in thought flow
- Perseveration: Pathological repetition of words or ideas
Thought Content
What the patient is thinking about:
- Delusions: Fixed false beliefs (persecutory, grandiose, etc.)
- Obsessions: Intrusive, unwanted thoughts
- Phobias: Irrational fears
- Suicidal ideation: Thoughts about ending one’s life
- Homicidal ideation: Thoughts about harming others
- Preoccupations: Excessive focus on specific concerns
Safety Assessment
Always assess for suicidal and homicidal ideation when evaluating thought content. Document the presence of plans, intent, means, and protective factors.
| Thought Disturbance | Clinical Example | Associated Conditions |
|---|---|---|
| Persecutory delusion | “The government has implanted a tracking device in my brain.” | Schizophrenia, delusional disorder, psychotic depression |
| Flight of ideas | Rapidly jumping between topics: “I need to clean my house—my house is blue—blue reminds me of the ocean—I went swimming last week—the weather was hot…” | Mania, hypomania |
| Thought blocking | Sudden stopping mid-sentence, unable to continue the thought | Schizophrenia, severe anxiety |
| Obsessions | Intrusive thoughts about contamination despite recognizing they are excessive | OCD, anxiety disorders |
| Loose associations | Disconnected speech with no logical connection between thoughts | Schizophrenia, severe mania |
Perception assessment evaluates how the patient interprets sensory information. Disturbances in perception are important indicators of various psychiatric and neurological conditions.
Key Perceptual Disturbances:
Hallucinations
Sensory perceptions in the absence of external stimuli. Types include:
- Auditory: Hearing voices or sounds (most common in psychiatric disorders)
- Visual: Seeing people, objects, lights, or patterns
- Tactile: Feeling sensations like bugs crawling on skin
- Olfactory: Smelling odors that aren’t present
- Gustatory: Tasting substances that aren’t present
Illusions
Misinterpretations of actual external stimuli (e.g., seeing a coat hanging as a person)
Depersonalization/Derealization
Depersonalization: Feeling detached from oneself, as if observing from outside
Derealization: Feeling that surroundings are unreal or distorted
Assessment Approach
When assessing for hallucinations, use neutral phrasing such as “Sometimes people hear voices or sounds that others cannot hear. Has this ever happened to you?” This non-judgmental approach may increase disclosure.
| Perceptual Disturbance | Common in Psychiatric Disorders | Common in Medical/Neurological |
|---|---|---|
| Auditory hallucinations (complex, voices) | Schizophrenia, psychotic disorders, severe mood disorders | Less common, except in delirium |
| Visual hallucinations | Less common in primary psychiatric disorders (except with severe psychosis) | Delirium, dementia with Lewy bodies, seizures, migraines, Charles Bonnet syndrome |
| Tactile hallucinations | Less common, except in severe psychosis | Substance withdrawal (especially alcohol, “formication”), neuropathy |
| Illusions | Can occur in many conditions, especially with anxiety | Delirium, sensory impairment, normal in low-light conditions |
Cognitive assessment evaluates a patient’s mental functions including orientation, attention, memory, and higher-level thinking. In the MSE, this is typically a screening rather than comprehensive assessment.
Key Cognitive Domains:
Orientation
Person, place, time, and situation.
Assessment: “Can you tell me your full name? Where are we now? What’s today’s date? Why are you here today?”
Attention/Concentration
Ability to focus and maintain concentration.
Assessment: Digit span, counting backward from 100 by 7s, spelling “WORLD” backward
Memory
- Immediate: Repeating information right away
- Recent: Recalling recent events or information
- Remote: Recalling past events or learned information
Assessment: 3-word recall after 5 minutes, recent news events, past personal history
Higher Cognition
- Abstract thinking: Understanding beyond concrete meanings
- Judgment: Decision-making abilities
- Calculation: Numerical operations
Assessment: Interpreting proverbs, similarities/differences, simple calculations
Screening Tools
When cognitive impairment is suspected, consider using standardized screening tools:
- Mini-Mental State Examination (MMSE) – 30-point questionnaire
- Montreal Cognitive Assessment (MoCA) – More sensitive for mild impairment
- Mini-Cog – Brief 3-minute assessment
- Clock Drawing Test – Simple screening for visuospatial and executive function
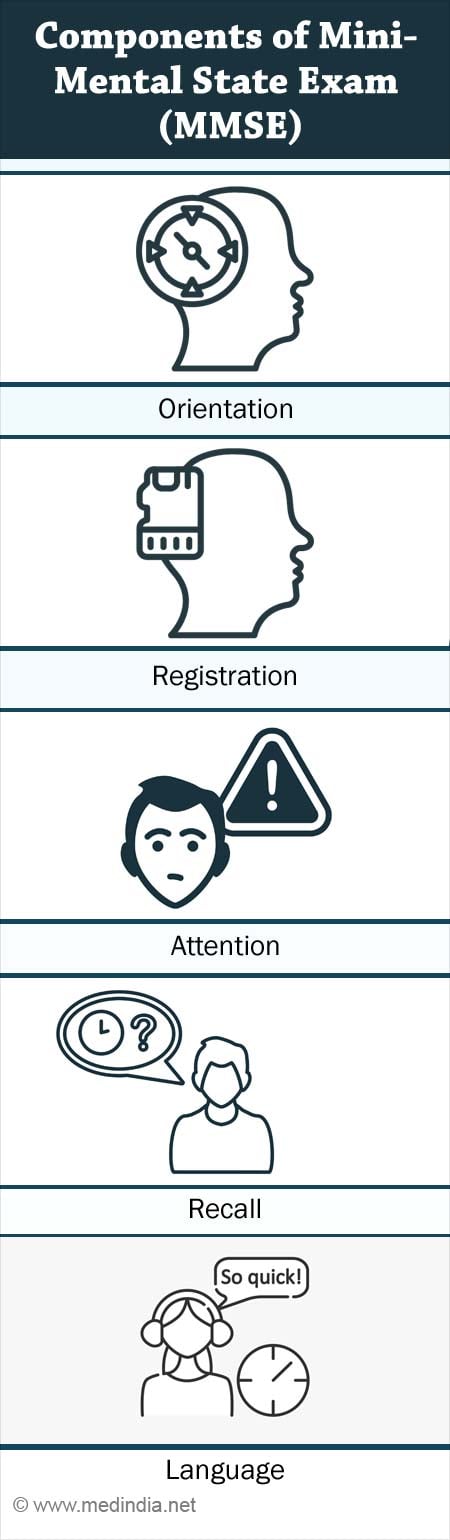
Figure 3: Components of Mini-Mental State Examination (MMSE)
Cultural Considerations
Cognitive assessments can be influenced by educational level, language proficiency, and cultural background. Adjust your interpretation accordingly and use culturally appropriate assessment tools when available.
Insight and judgment assessment evaluates a patient’s understanding of their condition and their decision-making capacity. These components have important implications for treatment planning and risk management.
Insight
The patient’s awareness and understanding of their illness or situation.
Levels of Insight:
- Complete/Good: Full awareness of illness and need for treatment
- Partial/Fair: Some recognition of problems but minimizes severity
- Poor/Limited: Minimal awareness of illness
- Absent: No awareness of illness (anosognosia)
Judgment
The patient’s ability to make rational decisions and understand consequences.
Assessment Approaches:
- Evaluate past decisions and their outcomes
- Assess responses to hypothetical scenarios
- Determine ability to plan appropriately
- Assess safety awareness and risk recognition
| Level | Insight Example | Judgment Example |
|---|---|---|
| Good | “I have bipolar disorder and need to take my medication to prevent manic episodes.” | Recognizes early warning signs and seeks help appropriately |
| Fair | “I’ve been struggling lately, but I don’t think it’s as serious as the doctor says.” | Sometimes makes impulsive decisions but can recognize when they were poor choices |
| Poor | “There’s nothing wrong with me. Everyone else is the problem.” | Makes consistently harmful decisions without recognizing consequences |
| Absent | “I’m not mentally ill. I’m being persecuted because I’m actually a secret government agent.” | Demonstrates dangerous behavior with no recognition of risks |
Clinical Implications
Poor insight and judgment may indicate:
- Need for higher level of care or supervision
- Potential non-adherence to treatment
- Possible need for involuntary treatment (depending on risk and legal criteria)
- Reduced capacity for informed consent
Clinical Applications of MSE in Nursing Practice
The Mental Status Examination is a versatile tool with numerous applications across nursing specialties and healthcare settings.
Psychiatric Nursing
- Establishing baseline mental status
- Monitoring response to psychiatric medications
- Assessing for changes in psychotic symptoms
- Evaluating suicide/violence risk
- Planning appropriate interventions
Medical-Surgical Nursing
- Detecting delirium in hospitalized patients
- Monitoring cognitive effects of medications
- Assessing capacity for medical decision-making
- Evaluating post-operative cognitive changes
- Discharge planning and safety assessment
Neurology Nursing
- Monitoring cognitive changes in neurological conditions
- Assessing impact of seizure activity
- Evaluating stroke symptoms and recovery
- Monitoring traumatic brain injury progression
- Assessing dementia progression
MSE in the Nursing Process
| Nursing Process Step | MSE Application |
|---|---|
| Assessment | Systematic collection of mental status data through observation and interview |
| Diagnosis | Identifying nursing diagnoses based on MSE findings (e.g., disturbed thought processes, impaired social interaction) |
| Planning | Developing care plans tailored to specific mental status findings |
| Implementation | Executing interventions based on MSE findings (e.g., reorientation techniques for confusion) |
| Evaluation | Using serial MSEs to track changes and response to interventions |
Documentation Best Practices
When documenting MSE findings in nursing notes:
- Use objective, descriptive language rather than interpretive statements
- Quote the patient directly when documenting mood or unusual statements
- Document both positive and negative findings
- Note changes from previous assessments
- Avoid stigmatizing language or labels
Common Nursing Interventions Based on MSE Findings
| MSE Finding | Potential Nursing Interventions |
|---|---|
| Disorientation |
|
| Hallucinations |
|
| Suicidal ideation |
|
| Flat affect/depressed mood |
|
| Agitation/aggression |
|
Practical Tips for Conducting the MSE
Do’s
- Establish rapport before beginning formal assessment
- Use open-ended questions when possible
- Consider cultural factors that may influence presentation
- Assess throughout the entire encounter, not just during formal questioning
- Document observations objectively
- Compare findings to patient’s baseline when available
Don’ts
- Make assumptions based on diagnosis or appearance
- Use medical jargon when communicating with patients
- Rush through assessment when dealing with cognitive impairment
- Interpret findings in isolation from other clinical information
- Use leading questions that suggest a desired response
- Ignore contradictions between verbal and non-verbal communication
Special Considerations
Pediatric Patients
- Use age-appropriate language and questions
- Observe play behavior as part of assessment
- Consider developmental stage
- Include parent/caregiver observations
Geriatric Patients
- Allow additional time for processing and responses
- Consider sensory impairments (hearing, vision)
- Assess for delirium vs. dementia
- Be mindful of medication effects on presentation
Cultural Considerations
- Be aware of cultural differences in eye contact, personal space, and expression of emotions
- Consider language barriers and use professional interpreters when needed
- Recognize that cultural beliefs may influence content of thought
- Adapt cognitive testing to cultural context
Emergency Situations
- Focus on safety-critical components first (suicidality, homicidality, psychosis)
- Abbreviate assessment as needed based on acuity
- Reassess frequently as status may change rapidly
- Document timing of observations in rapidly changing situations
Integration Technique
The most effective MSEs are those that feel conversational rather than like a formal interrogation. Practice weaving assessment questions naturally into therapeutic conversation while maintaining systematic observation.
MSE Documentation Examples
Proper documentation of MSE findings is essential for continuity of care, communication with the healthcare team, and legal documentation. Below are examples of how to document MSE findings for different clinical scenarios.
Example 1: Patient with Depression
Appearance: 42-year-old female appearing stated age, casually dressed with uncombed hair and wrinkled clothes. Poor eye contact maintained throughout interview. Posture slumped.
Behavior: Minimal spontaneous movement. Responds to questions after noticeable delay. No abnormal movements or psychomotor agitation observed.
Speech: Soft volume, slow rate, limited spontaneous speech with brief responses. No abnormalities in articulation.
Mood: “I just feel empty and tired all the time.”
Affect: Restricted range, congruent with stated mood, predominantly sad.
Thought Process: Linear and goal-directed but with latency in responses.
Thought Content: Preoccupied with feelings of worthlessness and failure. Denies current suicidal ideation but admits to passive thoughts of “not wanting to wake up” in the past week. No homicidal ideation. No delusions elicited.
Perception: Denies hallucinations in all sensory modalities. No illusions noted.
Cognition: Alert and oriented x4. Attention adequate for interview. Memory intact for recent and remote events. Able to perform serial 7s with 1 error.
Insight: Fair – acknowledges depression but minimizes need for treatment.
Judgment: Fair – has continued to meet basic responsibilities despite symptoms.
Example 2: Patient with Acute Psychosis
Appearance: 25-year-old male appearing disheveled with unwashed clothing and body odor. Multiple layers of clothing despite warm room temperature. Poor hygiene with long, untrimmed fingernails and unkempt beard.
Behavior: Hypervigilant, frequently looking around room and at ventilation ducts. Intermittently appears to be listening to something not apparent to interviewer. Difficult to engage and frequently gets up to look out window.
Speech: Variable in volume from whispered to loud. Rate alternates between rapid and halting. Occasional neologisms and word salad noted.
Mood: “They’re after me. Not safe here.”
Affect: Labile, shifting between fearful, suspicious, and briefly inappropriate laughter. Incongruent with context at times.
Thought Process: Disorganized with loose associations and tangentiality. Frequent derailment from topic.
Thought Content: Paranoid delusions about government surveillance through electronic devices. Believes implants were placed in his teeth during dental work. Denies current suicidal or homicidal ideation.
Perception: Reports auditory hallucinations of multiple male voices commenting on his behavior and giving commands. Denies visual hallucinations currently.
Cognition: Alert and oriented to person and place, but disoriented to time (states year is 2015). Attention fluctuates throughout interview. Unable to complete serial 7s.
Insight: Poor – denies mental illness and attributes symptoms to external persecution.
Judgment: Poor – stopped taking medications 2 weeks ago, has been sleeping in car despite having apartment.
Example 3: Patient with Delirium
Appearance: 78-year-old female in hospital gown, appearing older than stated age. Hair uncombed. Hospital ID band and IV present in right arm.
Behavior: Restless in bed, picking at sheets and IV tubing. Fluctuating levels of alertness during 30-minute assessment, with periods of drowsiness alternating with agitation.
Speech: Mumbled at times, difficult to understand. Variable volume. Occasional mid-sentence trailing off.
Mood: Unable to reliably state mood due to fluctuating mental status.
Affect: Fluctuating between flat, confused, and briefly fearful when disoriented.
Thought Process: Disorganized and fragmented. Unable to maintain coherent conversation.
Thought Content: When lucid, expresses concern about being in hospital. During confused periods, makes statements about needing to “go home to feed the children” (patient’s children are adults). No clear delusions elicited.
Perception: Visual illusions noted – referred to IV pole as a person at one point. Intermittently reaching for objects not present.
Cognition: Fluctuating level of consciousness. Oriented to person only. Disoriented to place and time. Unable to maintain attention for formal cognitive testing.
Insight: Poor – unaware of current condition and fluctuating mental status.
Judgment: Poor – attempted to remove IV during assessment.
MSE Practice Scenarios
Practice analyzing these clinical scenarios to strengthen your MSE skills. For each case, identify key MSE findings and their potential significance.
Scenario 1
You are assessing a 45-year-old male who was brought to the emergency department by police after being found wandering in traffic. During your assessment, he is pacing, appears disheveled with dirty clothing, and has a strong odor of alcohol. His speech is slurred and he is irritable when questioned. He states, “I just had a couple of drinks, it’s not a big deal.” He acknowledges today’s date but insists he is in New York (you are in Chicago). When you ask why he was in traffic, he states, “I was just crossing the street, mind your own business.” He is able to follow simple commands but has difficulty with concentration tasks.
Key MSE Findings:
- Appearance: Disheveled, poor hygiene
- Behavior: Pacing, irritable
- Speech: Slurred
- Mood/Affect: Irritable
- Thought content: Minimization of drinking behavior
- Cognition: Disoriented to place, difficulty with concentration
- Insight: Poor insight into current situation
Assessment Considerations:
This presentation is consistent with alcohol intoxication, but requires further assessment to rule out other conditions like head injury, metabolic disorders, or psychiatric conditions. The disorientation to place and poor insight raise concerns about his safety and decision-making capacity.
Scenario 2
You are conducting an outpatient assessment of a 19-year-old female college student who was referred by her academic advisor due to declining academic performance. She arrives 20 minutes late for her appointment, dressed neatly but with noticeable dark circles under her eyes. When asked how she’s feeling, she states, “I’m just tired all the time.” She speaks softly and makes minimal eye contact. You notice she becomes tearful when discussing school performance. She denies hallucinations or delusions, but reports difficulty concentrating on her studies and persistent feelings of worthlessness. She mentions “sometimes wondering if everyone would be better off without me” but denies specific suicidal plan or intent. She is fully oriented and her cognitive functions appear intact, though she reports subjective concentration difficulties.
Key MSE Findings:
- Appearance: Appropriately dressed but appears fatigued (dark circles)
- Behavior: Minimal eye contact, tearful at times
- Speech: Soft volume
- Mood: “Tired all the time”
- Affect: Sad, tearful
- Thought content: Feelings of worthlessness, passive suicidal ideation
- Cognition: Oriented, intact, but subjective concentration difficulties
Assessment Considerations:
The presentation is consistent with a depressive disorder. The passive suicidal ideation requires thorough risk assessment and safety planning. Consider screening for anxiety disorders as well, as they commonly co-occur with depression in college students. The impact on academic performance suggests functional impairment warranting intervention.
Summary: Key Points to Remember
- The Mental Status Examination is a structured assessment of psychological functioning that serves as a vital “snapshot” of a patient’s current mental state.
- Use the ASEPTIC mnemonic to remember core components: Appearance/Behavior, Speech, Emotion, Perception, Thought, Insight/Judgment, and Cognition.
- Assessment begins the moment you first see the patient and continues throughout your entire interaction.
- Document objectively, using the patient’s own words when appropriate, and avoid interpretive statements.
- The MSE is applicable across all nursing specialties and can help identify changes in mental status, guide interventions, and evaluate response to treatment.
- Always include safety assessments (suicidal/homicidal ideation) when evaluating thought content.
- Consider cultural, developmental, and situational factors when interpreting MSE findings.
- Serial MSEs provide valuable information about a patient’s progress and response to interventions over time.
Remember: The MSE is both a science and an art – combining systematic assessment with clinical judgment and therapeutic communication skills.
