Mentorship & Preceptorship in Nursing
Delegation, Power & Politics, Empowerment, Mentoring and Coaching
Table of Contents
Introduction to Mentorship in Nursing
Mentorship represents one of the most powerful developmental relationships in nursing practice. It involves the pairing of an experienced, knowledgeable nurse with a less experienced colleague to facilitate professional growth, career development, and integration into the nursing profession. Effective mentorship programs have become increasingly important in healthcare settings as they help bridge theory-practice gaps, enhance clinical competence, and promote retention of nursing staff.
Key Concept
Mentorship in nursing is a dynamic, collaborative relationship that supports professional development through guidance, knowledge transfer, and personal support from an experienced nurse to a novice or developing nurse.
Benefits of Mentorship in Nursing
For Mentees
- Enhanced clinical confidence and competence
- Reduced workplace anxiety and stress
- Improved critical thinking and decision-making skills
- Greater job satisfaction and engagement
- Accelerated professional development and career growth
- Stronger sense of professional identity
For Mentors
- Refinement of leadership and teaching skills
- Professional satisfaction from contributing to the profession
- Stimulation of reflective practice and self-growth
- Recognition of expertise and accomplishments
- Renewed enthusiasm for nursing practice
- Development of a professional legacy
For Healthcare Organizations
- Reduced turnover rates and associated costs
- Improved quality of patient care and safety
- Enhanced workplace culture and team cohesion
- Increased staff engagement and satisfaction
- Strengthened knowledge transfer and institutional memory
- Development of future nursing leaders
Important Consideration
While mentorship offers numerous benefits, its success depends on organizational support, clear program structure, appropriate mentor-mentee matching, and dedicated time for mentoring activities. Without these elements, mentorship programs may fail to achieve their intended outcomes.
Mentorship vs. Preceptorship
Although the terms mentorship and preceptorship are sometimes used interchangeably in nursing literature, they represent distinct relationships with different purposes, timeframes, and focuses. Understanding these differences is crucial for implementing appropriate developmental relationships in nursing practice.

Figure 1: Coaching model framework showing the relationship between preceptor, mentor, and student nurses.
Comparative Analysis
| Characteristic | Mentorship | Preceptorship |
|---|---|---|
| Definition | A dynamic, collaborative relationship between an experienced nurse and a less experienced nurse focused on professional and personal development. | A formal teaching-learning relationship designed to help a new nurse transition into clinical practice and develop clinical competence. |
| Primary Purpose | Career development, professional growth, leadership development, and personal support. | Clinical orientation, skill acquisition, competency development, and socialization to the unit/organization. |
| Duration | Long-term relationship (months to years). | Short-term relationship (weeks to months) with a defined endpoint. |
| Selection Process | Often voluntary and mutually agreed upon; may develop naturally or through formal programs. | Usually assigned by management; formal requirement for orientation. |
| Focus | Broader focus on professional identity, career trajectory, and leadership development. | Narrower focus on clinical skills, unit-specific practices, and immediate job requirements. |
| Evaluation | Typically non-evaluative; focused on guidance rather than assessment. | Includes formal evaluation of performance and competency attainment. |
| Relationship Dynamic | More personal; often extends beyond workplace boundaries. | More formal; primarily confined to the clinical setting during work hours. |
Mnemonic: “MENTOR vs PRECEPT”
M – Mutually selected relationship
E – Extensive timeframe (long-term)
N – Nurtures professional growth
T – Transcends clinical skills
O – Ongoing support and guidance
R – Relationship-focused
P – Prescribed assignment
R – Restricted timeframe (short-term)
E – Ensures clinical competence
C – Clinical skill development
E – Evaluative in nature
P – Practice-focused
T – Task-oriented
Best Practice
Many healthcare organizations have found that a continuum of support—starting with preceptorship for initial orientation and transitioning to mentorship for ongoing development—provides the most comprehensive approach to nursing professional growth.
Models of Mentorship in Nursing
Various theoretical models guide mentorship approaches in nursing. These frameworks provide structure to mentoring relationships and help ensure their effectiveness. Understanding these models allows nursing leaders to implement appropriate mentorship programs based on organizational context and goals.

Figure 2: Transformational-transcendence mentorship model showing the relationship dynamics between mentor and mentee.
Key Mentorship Models in Nursing
Traditional Dyad Model
Structure: One-to-one relationship between mentor and mentee
Characteristics:
- Intensive individual attention
- Personalized development plans
- Close professional relationship
- High level of commitment from both parties
Best for: New graduates, career transitions, leadership development
Group Mentorship Model
Structure: One mentor works with multiple mentees simultaneously
Characteristics:
- Efficient use of mentor resources
- Peer learning and support
- Diverse perspectives and experiences
- Community of practice development
Best for: Organizations with limited mentors, cohort-based orientations
Peer Mentorship Model
Structure: Nurses at similar career stages mentor each other
Characteristics:
- Reciprocal learning and support
- Reduced power differential
- Shared contemporary experiences
- Enhanced collegiality
Best for: New graduate cohorts, specialized practice areas
Transformational Mentorship Model
Structure: Focus on transforming both mentor and mentee through mutual growth
Characteristics:
- Bidirectional learning
- Personal and professional transformation
- Emphasis on reflective practice
- Development of emotional intelligence
Best for: Experienced nurses, leadership development, practice innovation
Mosaic Mentorship Model
Structure: Mentee works with multiple mentors for different aspects of development
Characteristics:
- Specialized guidance in different areas
- Diverse role modeling
- Broad network development
- Flexible mentoring relationships
Best for: Advanced practice nurses, aspiring nurse leaders, specialty development
Virtual/Distance Mentorship Model
Structure: Technology-facilitated mentoring without geographic constraints
Characteristics:
- Flexible scheduling
- Elimination of geographic barriers
- Technology-enhanced communication
- Written reflection opportunities
Best for: Rural nurses, nurses seeking specialty expertise not locally available
The 5 C’s Model of Mentoring
A widely recognized framework for effective mentorship is the 5 C’s model, which outlines key elements of successful mentoring relationships:
- Context: Understanding the organizational and professional environment
- Clarity: Establishing clear expectations and goals
- Coordination: Managing the mentoring process effectively
- Commitment: Dedication to the mentoring relationship by both parties
- Capability: Building the competence and confidence of the mentee

Figure 3: Conceptual model showing the relationship between mentoring, psychological empowerment, and job satisfaction.
Delegation in Nursing Practice
Delegation is a critical skill in nursing practice and an essential component of effective mentorship. It involves transferring responsibility for a nursing task from one individual to another while maintaining accountability for the outcome. As mentors guide developing nurses, teaching proper delegation principles becomes an important aspect of professional development.
Definition
According to the American Nurses Association (ANA), delegation is “the transfer of responsibility for the performance of an activity from one individual to another while retaining accountability for the outcome.”
Principles of Effective Delegation
Core Principles
- The RN must maintain ultimate accountability
- Delegation decisions must be based on patient needs
- Delegation should match task complexity with staff competency
- Clear communication is essential for safe delegation
- Appropriate supervision must accompany delegation
- Evaluation of outcomes must follow the delegated task
Tasks That Cannot Be Delegated
- Nursing assessment and diagnosis
- Development of nursing care plans
- Evaluation of patient progress
- Patient teaching requiring professional judgment
- Activities requiring professional nursing knowledge
- Medication administration (with limited exceptions)
- Interventions requiring independent nursing judgment

Figure 4: NCSBN Delegation Decision-Making Model guiding the delegation process in nursing practice.
Delegation Within the Mentorship Relationship
Delegation is not only a skill to be taught by mentors but also a process that occurs within the mentorship relationship itself. As mentees develop, mentors progressively delegate more complex responsibilities to facilitate growth and autonomy.
| Mentee Development Stage | Appropriate Delegation Level | Mentor Support Level |
|---|---|---|
| Novice | Simple, routine tasks with clear protocols | High level of direction and direct supervision |
| Advanced Beginner | More varied tasks with some decision-making elements | Regular check-ins and readily available guidance |
| Competent | Complex cases with multiple elements requiring coordination | Periodic check-ins, available for consultation |
| Proficient | Full range of responsibilities with minimal restrictions | Minimal supervision, reflective discussions |
| Expert | Complete autonomy with complex cases | Collaborative peer relationship, mutual learning |
Common Delegation Pitfalls
- Inappropriate delegation: Assigning tasks beyond the delegate’s scope of practice or competency level
- Inadequate communication: Failing to clearly articulate expectations, parameters, or outcomes
- Insufficient supervision: Not providing appropriate level of oversight based on task complexity and staff experience
- Abdication vs. delegation: Abandoning responsibility rather than transferring responsibility while maintaining accountability
- Overdelgation: Assigning too many tasks to one individual, potentially compromising patient safety
- Underdelgation: Failing to delegate appropriate tasks, leading to inefficiency and nurse burnout
The Five Rights of Delegation
The American Nurses Association (ANA) has developed the Five Rights of Delegation framework to guide safe delegation decisions. This framework is an essential tool for mentors to teach mentees how to delegate effectively and safely while maintaining professional accountability.

Figure 5: The Five Rights of Delegation framework for safe nursing delegation.
1. Right Task
The activity should be delegable for a specific patient situation and appropriate for delegation.
Key Questions:
- Is the task within the delegate’s legal scope of practice?
- Is the task routine with predictable outcomes?
- Does the task require independent nursing judgment?
- Does organizational policy permit this delegation?
2. Right Circumstances
The setting, available resources, and patient condition must be appropriate for delegation.
Key Questions:
- Is the patient’s condition stable and predictable?
- Are adequate resources available for task completion?
- Is the environment conducive to successful task completion?
- Is there appropriate support for questions or emergent situations?
3. Right Person
The delegate must have the appropriate qualifications, skills, and competence to perform the task safely.
Key Questions:
- Does the delegate have the required training and education?
- Has competency been verified for this specific task?
- Does the delegate have the confidence to perform the task?
- Is the delegate willing to accept the responsibility?
4. Right Direction
Clear, concise communication of expectations, procedures, outcomes, and parameters is essential.
Key Questions:
- Have specific instructions been provided?
- Are expected outcomes clearly communicated?
- Has the delegate been informed when to seek assistance?
- Has the delegate confirmed understanding of instructions?
5. Right Supervision
Appropriate monitoring, evaluation, intervention, and feedback must be provided as needed.
Key Questions:
- What level of supervision is required for this task?
- How will the outcome be evaluated?
- How and when will feedback be provided?
- What follow-up is needed to ensure patient safety?
Mnemonic: “TRUST” for the Five Rights of Delegation
- T – Task (Right Task)
- R – Reason/Rationale (Right Circumstances)
- U – Unique Individual (Right Person)
- S – Specific Instructions (Right Direction)
- T – Thoughtful Oversight (Right Supervision)
Teaching Delegation Through Mentorship
Effective mentors use a progressive approach to teaching delegation skills:
- Begin by modeling proper delegation while explaining reasoning
- Provide opportunities for mentees to practice delegation under supervision
- Facilitate structured reflection on delegation decisions and outcomes
- Gradually increase the complexity of delegation scenarios
- Encourage mentees to develop their own delegation style based on principles
Power & Politics in Nursing
Understanding power dynamics and political processes is crucial for effective mentorship and leadership in nursing. Mentors play a vital role in helping mentees navigate professional power structures and develop political competence to advance both patient care and the nursing profession.
Sources of Power in Nursing
Formal Power
Derived from position or role within an organization
- Legitimate power (authority from position)
- Reward power (ability to provide incentives)
- Coercive power (ability to enforce compliance)
Personal Power
Based on individual attributes and relationships
- Expert power (knowledge and skills)
- Referent power (respect and admiration)
- Connection power (relationships and networks)
Collective Power
Strength derived from group action
- Professional association membership
- Unionization
- Interprofessional collaboration
- Solidarity with patient advocacy groups
Power vs. Empowerment
While power refers to the ability to influence others and accomplish goals, empowerment involves enabling individuals to develop their own power. In mentorship, the goal is to help mentees recognize and develop their own sources of power rather than creating dependency on the mentor’s power.
Political Competence in Nursing
Political competence involves the skills needed to navigate organizational structures, influence decision-making processes, and advocate effectively for patients, the profession, and healthcare policy.
Organizational Politics
- Understanding formal and informal organizational structures
- Identifying key stakeholders and decision-makers
- Building strategic alliances and coalitions
- Advocating for resources and support
- Navigating interprofessional dynamics
Professional Politics
- Participation in professional organizations
- Advancing nursing’s voice in healthcare decisions
- Promoting evidence-based practice changes
- Securing recognition for nursing contributions
- Supporting the advancement of the profession
Policy Politics
- Understanding health policy development processes
- Advocating for patient-centered policy changes
- Engaging with legislative and regulatory bodies
- Participating in public health initiatives
- Contributing nursing perspective to policy debates
Mentoring for Political Competence
Mentors can develop mentees’ political competence through various strategies and experiences. This aspect of mentoring prepares nurses to be effective advocates and leaders.
| Mentoring Strategy | Description | Examples in Practice |
|---|---|---|
| Role Modeling | Demonstrating effective political engagement and advocacy |
|
| Strategic Introductions | Connecting mentees with influential people and networks |
|
| Guided Experiences | Providing structured opportunities for political engagement |
|
| Reflective Discussions | Analyzing political dynamics and developing strategies |
|
| Skill Development | Building specific competencies for political effectiveness |
|
Navigating Political Challenges
Mentors should prepare mentees for common political challenges they may face:
- Resistance to change: Strategies for overcoming organizational inertia
- Power imbalances: Approaches for advocating from positions with limited formal authority
- Competing interests: Techniques for finding common ground among stakeholders
- Ethical tensions: Frameworks for resolving conflicts between organizational demands and professional values
- Political burnout: Self-care practices to sustain long-term advocacy efforts
Empowerment in Nursing Leadership
Empowerment is a central concept in mentorship and nursing leadership. It involves creating conditions that enable nurses to develop confidence, competence, and autonomy in their practice. Empowered nurses are more effective advocates for patients, more satisfied in their roles, and better able to contribute to organizational success.
Definition
Nursing empowerment can be defined as “the ability to effectively motivate and mobilize self and others to accomplish positive outcomes in nursing practice and work environments.” It involves both structural and psychological dimensions.
Dimensions of Empowerment
Structural Empowerment
Environmental and organizational factors that provide access to:
- Opportunity: Growth and advancement possibilities
- Information: Knowledge needed for effective decision-making
- Support: Guidance, feedback, and emotional backing
- Resources: Time, materials, and personnel to accomplish goals
Psychological Empowerment
Individual’s internal sense of empowerment, including:
- Meaning: Value of work goals relative to personal values
- Competence: Belief in one’s ability to perform activities
- Self-determination: Sense of choice in initiating actions
- Impact: Perception of influencing outcomes at work
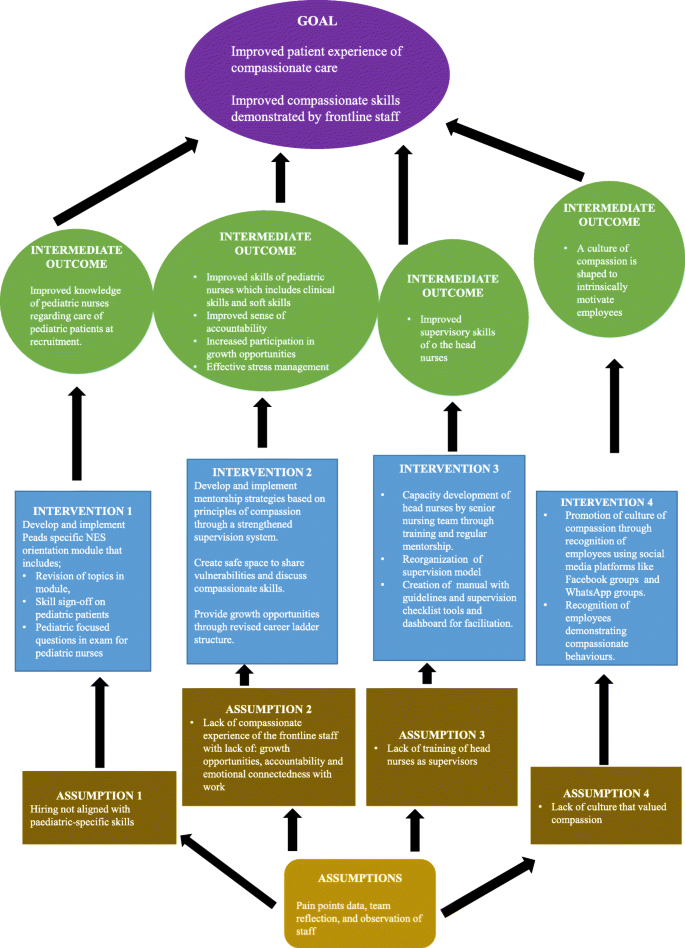
Figure 6: Framework showing how mentorship influences nursing empowerment and practice outcomes.
Strategies for Empowering Mentees
Create an Empowering Learning Environment
Establish psychological safety where questions are welcomed, mistakes are viewed as learning opportunities, and diverse perspectives are valued.
Provide Progressive Challenges
Gradually increase the complexity of assignments and responsibilities to build confidence and competence through successful experiences.
Offer Constructive Feedback
Provide specific, timely, and balanced feedback that acknowledges strengths while identifying areas for growth.
Support Decision-Making Autonomy
Encourage independent judgment while providing an appropriate safety net for consultation and guidance.
Share Information and Resources
Provide access to knowledge, tools, networks, and opportunities needed for success.
Recognize and Celebrate Growth
Acknowledge progress, achievements, and contributions to reinforce a sense of competence and impact.
Model Empowered Practice
Demonstrate confident, autonomous, and evidence-based practice while advocating for patients and the profession.
Empowerment Through Mentorship: A Cyclical Model
Relationship Building
Establishing trust, respect, and open communication
Transformational Learning
Creating experiences that challenge and expand thinking
Empowered Action
Supporting autonomous practice with appropriate guidance
Reflective Practice
Examining experiences to deepen learning and growth
Dependent Mentee
Empowered Colleague
“Powerless nurses are ineffective nurses. Powerless nurses are less satisfied with their jobs and more susceptible to burnout and depersonalization. Personal and professional empowerment can transform nurses and the nursing care they provide.”
— Laschinger & Havens, “Power and Empowerment in Nursing”
Mentoring & Coaching Techniques
While mentorship and coaching are related concepts, they represent distinct approaches to professional development in nursing. Both are valuable tools in nursing education and leadership, with different applications based on development needs and goals.
Distinguishing Mentoring from Coaching
| Aspect | Mentoring | Coaching |
|---|---|---|
| Primary Focus | Holistic professional development and career advancement | Specific performance improvement or skill development |
| Timeframe | Long-term relationship (months to years) | Short-term, goal-oriented approach (weeks to months) |
| Relationship Dynamic | Often more personal; involves role modeling and sharing experiences | More structured and formal; focused on achieving specific outcomes |
| Guidance Approach | Often includes advice, suggestions, and shared experiences | Primarily questioning and facilitation to draw out solutions from the coachee |
| Expertise Requirement | Mentor typically has significant experience in the mentee’s field | Coach may not need domain-specific expertise, but requires coaching skills |
| Direction | Often mentor-guided, though collaborative | Coachee-driven, with coach facilitating the process |
Complementary Approaches
In nursing education and development, mentoring and coaching are not mutually exclusive. An effective mentor often employs coaching techniques when appropriate, and a structured mentorship program may include specific coaching components for skill development.
Key Mentoring Techniques
Storytelling & Case Sharing
Sharing experiences and lessons learned from the mentor’s career to provide context, perspective, and practical wisdom.
Example: Describing how the mentor navigated a challenging ethical dilemma to illustrate professional decision-making.
Role Modeling
Demonstrating professional behaviors, attitudes, and skills through the mentor’s own practice for the mentee to observe and emulate.
Example: Inviting the mentee to observe the mentor conducting a complex family meeting or clinical intervention.
Networking Facilitation
Introducing mentees to professional contacts and creating opportunities for building their own professional networks.
Example: Connecting the mentee with colleagues in their area of interest or bringing them to professional events.
Career Navigation
Providing guidance on career pathways, advancement opportunities, and strategic professional development choices.
Example: Advising on educational pursuits, certification options, or committee involvement to align with career goals.
Protection & Advocacy
Advocating for the mentee’s interests and helping them navigate organizational politics and challenges.
Example: Supporting the mentee’s innovative idea in a committee meeting or helping them respond to criticism constructively.
Key Coaching Techniques
Powerful Questioning
Using open-ended questions that promote reflection, insight, and self-discovery rather than providing direct answers.
Example: “What factors do you think contributed to that outcome?” rather than “You should have checked the medication twice.”
Active Listening
Demonstrating full attention, comprehension, and retention of what the coachee is communicating, both verbally and non-verbally.
Example: Maintaining eye contact, summarizing key points, and checking understanding before responding.
Goal Setting & Action Planning
Collaboratively establishing specific, measurable, achievable, relevant, and time-bound (SMART) goals with concrete action steps.
Example: Breaking down the goal of improving communication skills into specific behaviors to practice with weekly targets.
Feedback Techniques
Providing specific, objective, constructive feedback that focuses on behaviors rather than personality traits.
Example: “I noticed you asked three clarifying questions during the handoff, which helped ensure complete information transfer” rather than “Good job on the handoff.”
Accountability Structures
Creating frameworks for regular check-ins, progress reviews, and adjustment of plans to maintain momentum and focus.
Example: Establishing weekly brief meetings to review progress on action steps and adjust plans as needed.
Mnemonic: “COACH” Framework for Effective Coaching Conversations
- C – Clarify the current situation and desired outcome
- O – Open exploration of options and possibilities
- A – Acknowledge obstacles and develop strategies
- C – Commit to specific actions and timeline
- H – Hold accountable through follow-up and support
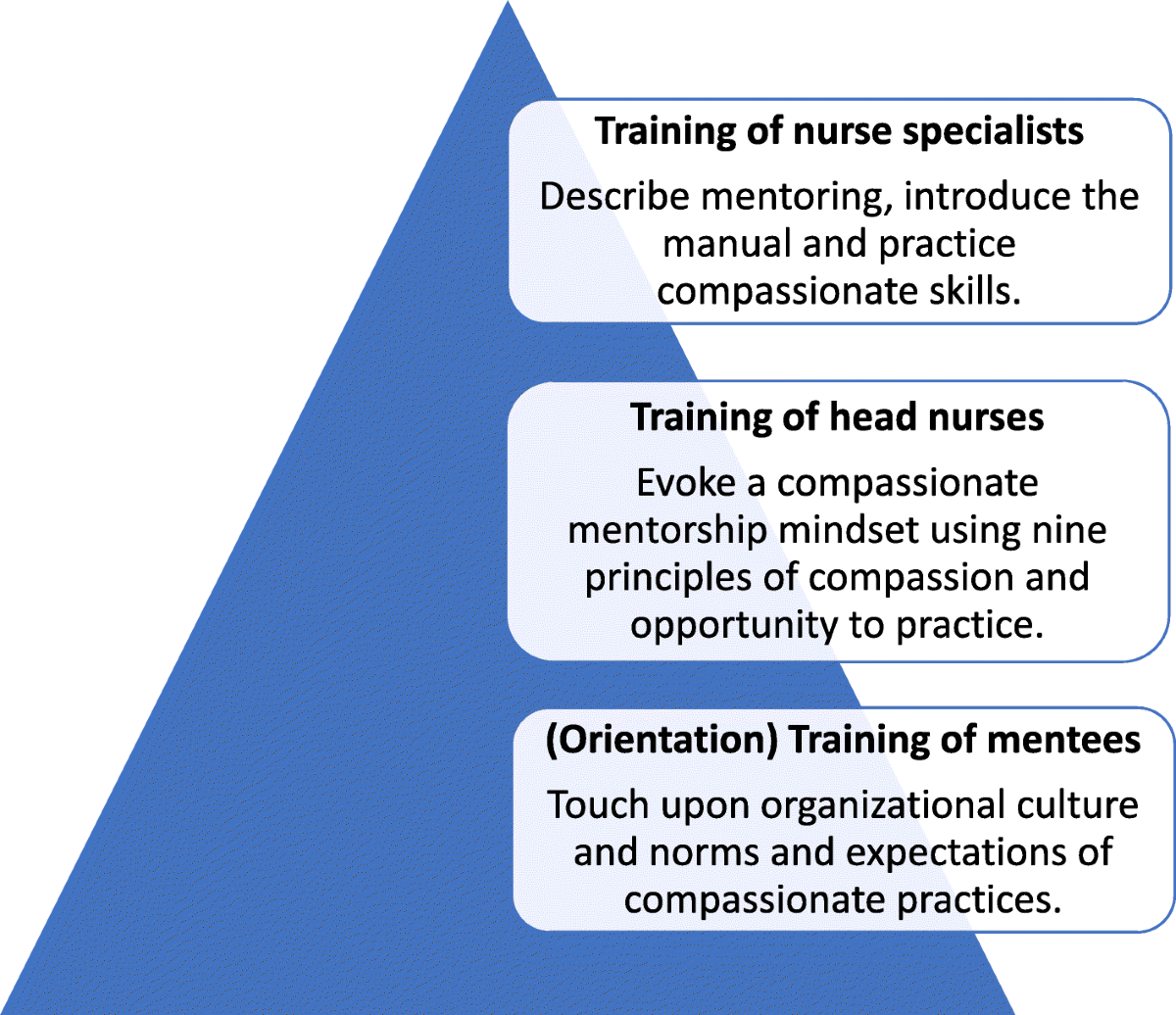
Figure 7: Framework for implementing coaching and mentoring techniques in nursing practice.
Developing Effective Mentoring Relationships
Creating and maintaining successful mentoring relationships requires intentional effort from both mentors and mentees. These relationships evolve over time and pass through distinct phases, each requiring different approaches and skills.
Phases of Mentoring Relationships
Initiation Phase
- Establishing expectations
- Building initial trust
- Identifying learning needs
- Creating the foundation
Cultivation Phase
- Deepening of trust
- Active learning and growth
- Regular engagement
- Expanding challenges
Separation Phase
- Increasing independence
- Transitioning support
- Redefining relationship
- Celebrating achievements
Redefinition Phase
- Evolving to collegiality
- Mutual professional support
- Potential friendship
- Legacy building
Essential Elements of Effective Mentoring Relationships
For Mentors
- Commitment: Dedicating time and energy to the relationship
- Authenticity: Being genuine and transparent about experiences
- Availability: Being accessible for questions and support
- Patience: Allowing time for growth and learning
- Adaptability: Adjusting approach to meet evolving needs
- Emotional intelligence: Understanding and managing emotions
- Professional boundaries: Maintaining appropriate relationship parameters
For Mentees
- Initiative: Taking active responsibility for learning
- Receptivity: Being open to feedback and guidance
- Preparation: Coming to meetings with questions and updates
- Follow-through: Acting on agreed-upon steps and commitments
- Gratitude: Acknowledging the mentor’s investment
- Reflection: Processing experiences to maximize learning
- Growth mindset: Viewing challenges as opportunities
Creating a Mentorship Agreement
A structured mentorship agreement can establish clear expectations and provide a framework for the relationship. Key components include:
- Goals and objectives: What specific outcomes are being sought
- Roles and responsibilities: What each party commits to do
- Meeting frequency and format: How often and how interactions will occur
- Communication preferences: Best ways to contact each other
- Confidentiality boundaries: What will remain private vs. shared
- Evaluation process: How progress will be measured
- Duration and conclusion: Expected timeframe and end conditions
Overcoming Common Challenges in Mentoring Relationships
| Challenge | Prevention Strategies | Resolution Approaches |
|---|---|---|
| Time Constraints |
|
|
| Mismatched Expectations |
|
|
| Communication Barriers |
|
|
| Dependency Issues |
|
|
| Power Imbalances |
|
|
Mnemonic: “RELATE” for Building Effective Mentoring Relationships
- R – Respect for each other’s time, expertise, and boundaries
- E – Expectations that are clear, realistic, and mutually understood
- L – Listening actively and empathetically to each other
- A – Adaptability to changing needs and circumstances
- T – Trust built through consistency, honesty, and support
- E – Engagement that is genuine, committed, and growth-oriented
Conclusion & Future Directions
Mentorship and preceptorship represent essential cornerstones of nursing professional development. Through effective mentoring relationships, nurses develop the clinical competence, leadership skills, and professional identity needed to advance practice, improve patient outcomes, and strengthen the nursing profession as a whole.
Key Takeaways
Core Concepts
- Mentorship and preceptorship serve distinct but complementary purposes in nursing development
- Various mentorship models can be applied based on organizational context and individual needs
- Effective delegation is a critical skill that develops through mentored practice
- Understanding power dynamics and political processes enhances nursing influence
- Empowerment through mentorship creates confident, competent nurse leaders
- Both mentoring and coaching techniques contribute to professional development
Best Practices
- Establish clear expectations and structured agreements for mentoring relationships
- Match mentorship approaches to developmental needs and organizational context
- Apply the Five Rights of Delegation as a framework for safe delegation practices
- Create conditions for both structural and psychological empowerment
- Adapt mentoring techniques based on relationship phase and mentee needs
- Address challenges proactively through open communication and flexibility
Future Directions for Mentorship in Nursing
Technology-Enhanced Mentoring
Expanding virtual mentoring approaches, digital mentoring platforms, and AI-assisted mentoring tools to overcome geographic barriers and extend mentoring access.
Diversity-Focused Mentoring
Developing mentoring programs specifically designed to support nurses from underrepresented groups and address equity gaps in nursing leadership.
Interprofessional Mentoring
Creating cross-disciplinary mentoring relationships to enhance collaboration, broaden perspective, and develop team-based leadership skills.
Evidence-Based Mentoring Practices
Expanding research on mentoring outcomes and effectiveness to develop more rigorous, evidence-based approaches to mentoring program design.
Organizational Mentoring Cultures
Moving beyond individual mentoring relationships to create comprehensive mentoring cultures that embed development into all aspects of nursing practice.
Global Mentoring Networks
Establishing international mentoring connections to share best practices, expand cultural competence, and address global health challenges.
Final Thoughts
Effective mentorship in nursing transcends simple knowledge transfer—it represents the profession’s commitment to its future. Through mentoring relationships, the wisdom, values, and expertise of nursing are passed from generation to generation, strengthening the profession and improving healthcare outcomes. As nursing faces complex challenges of the future, strong mentorship will remain essential to developing the leaders and practitioners who will shape healthcare delivery and advance the nursing profession.
Embrace the Journey of Mentorship
“The delicate balance of mentoring someone is not creating them in your own image, but giving them the opportunity to create themselves.” — Steven Spielberg
