Mini Mental Status Examination (MMSE)
Comprehensive nursing notes for cognitive assessment
The Mini Mental Status Examination (MMSE) is a widely used screening tool designed to assess cognitive function in clinical settings. Developed by Folstein and colleagues in 1975, it has become the most commonly utilized cognitive assessment instrument in both clinical practice and research.
Quick Facts
- 11-question measure that takes 5-10 minutes to administer
- Tests five cognitive domains
- Maximum score of 30 points
- Scores ≥25 generally considered normal
- Proprietary but widely available
Clinical Applications
- Screening for cognitive impairment
- Estimating severity of cognitive decline
- Tracking cognitive changes over time
- Documenting response to treatment
- Initial assessment in suspected dementia
The MMSE evaluates cognitive function across five main domains. Understanding these components helps nurses properly administer the examination and interpret results accurately.
Orientation
Time & Place
10 points
Registration
Immediate Recall
3 points
Attention & Calculation
Serial 7s or WORLD
5 points
Recall
Delayed Memory
3 points
Language & Visuospatial
Naming, Repetition, Commands, Reading, Writing, Drawing
9 points
Detailed Breakdown of Components
1. Orientation (10 points)
Orientation to Time (5 points):
- What is the year? (1 point)
- What is the season? (1 point)
- What is the month? (1 point)
- What is the date? (1 point)
- What is the day of the week? (1 point)
Orientation to Place (5 points):
- What country are we in? (1 point)
- What state/province are we in? (1 point)
- What city/town are we in? (1 point)
- What is the name of this building/hospital? (1 point)
- What floor are we on? (1 point)
2. Registration (3 points)
The examiner names three unrelated objects clearly and slowly (e.g., “apple,” “table,” “penny”), then asks the patient to repeat all three objects.
- One point for each object correctly repeated on the first attempt
- If the patient doesn’t repeat all objects correctly, continue repeating them up to five times until all are learned
- Only the first attempt is scored
Nursing Tip: Speak clearly and at a normal pace. Pause briefly between words. The objects should be unrelated to each other.
3. Attention and Calculation (5 points)
Serial 7s:
- Ask the patient to count backward from 100 by sevens
- Stop after five subtractions (93, 86, 79, 72, 65)
- One point for each correct subtraction
Alternative – Spelling “WORLD” Backwards:
- Ask the patient to spell “WORLD” forwards first
- Then ask them to spell it backwards (“D-L-R-O-W”)
- One point for each letter in the correct position
Scoring WORLD Using the Line Method:
Draw lines to match letters from the correct response (DLROW) to the patient’s response. The score is the maximum number of lines that can be drawn without crossing any lines.
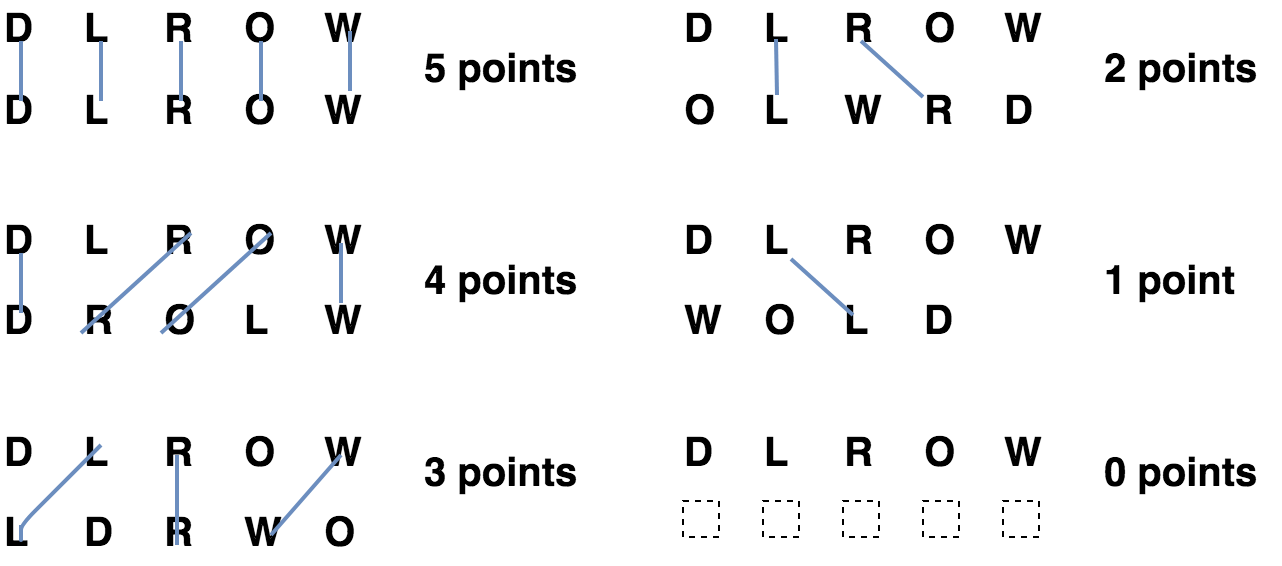
Nursing Tip: Use the better score between Serial 7s and WORLD spelling for the final MMSE score.
4. Recall (3 points)
Ask the patient to recall the three objects learned during the Registration component.
- One point for each object correctly recalled
- No hints or clues should be provided
Nursing Tip: This tests short-term memory. The delay between Registration and Recall components should be at least 3-5 minutes.
5. Language and Visuospatial Abilities (9 points)
Naming (2 points):
- Show the patient a wristwatch and ask “What is this?” (1 point)
- Show a pencil and ask “What is this?” (1 point)
Repetition (1 point):
- Ask the patient to repeat the phrase: “No ifs, ands, or buts” (1 point)
Three-Stage Command (3 points):
- Give the patient a piece of paper and say: “Take this paper in your right hand, fold it in half, and put it on the floor.” (1 point for each correctly executed action)
Reading (1 point):
- Show the patient a card with “CLOSE YOUR EYES” written on it and ask them to do what it says (1 point)
Writing (1 point):
- Ask the patient to write a complete sentence of their choice (1 point)
- The sentence must contain a subject and verb and make sense
- Grammar and punctuation errors are not counted against the patient
Drawing (1 point):
- Ask the patient to copy a drawing of two intersecting pentagons (1 point)
- All 10 angles must be present and the two shapes must intersect to form a four-sided figure

The MMSE has a maximum score of 30 points. Higher scores indicate better cognitive performance. Interpretation of scores should always consider the patient’s age, education level, and cultural background.
Standard Score Interpretation:
Normal Cognitive Function: 24-30 points
Mild Cognitive Impairment: 18-23 points
Moderate Cognitive Impairment: 10-17 points
Severe Cognitive Impairment: 0-9 points
Important Factors Affecting MMSE Scores
- Age: Scores typically decline with advanced age, especially over 80
- Education: Lower scores are common in individuals with fewer years of formal education
- Cultural/Language Barriers: May result in artificially lower scores
- Sensory Impairments: Vision or hearing deficits may impact performance
- Time of Day: Scores may vary with “sundowning” effects in dementia patients
Average MMSE Scores by Age and Education Level
| Education Level | 18-24 | 25-29 | 30-39 | 40-49 | 50-59 | 60-69 | 70-79 | 80+ |
|---|---|---|---|---|---|---|---|---|
| 0-4 years | 22 | 25 | 24 | 23 | 23 | 22 | 21 | 19 |
| 5-8 years | 27 | 27 | 26 | 26 | 27 | 26 | 25 | 23 |
| 9-12 years | 29 | 29 | 29 | 28 | 28 | 28 | 27 | 25 |
| College or higher | 29 | 29 | 29 | 29 | 29 | 29 | 28 | 27 |
Source: Adapted from Crum et al., 1993
MMSE Applications in Different Dementias
| Dementia Type | Common MMSE Findings | Primary Impairments |
|---|---|---|
| Alzheimer’s Disease | Poor performance on recall of three words and orientation to time/place | Memory |
| Vascular Dementia | Worse on attention, three-step commands, writing and copying pentagons | Working memory, motor and visuospatial skills |
| Lewy Body Dementia | Similar to vascular pattern; fluctuations in scores common | Attention, visuospatial skills |
| Frontotemporal Dementia | Higher initial MMSE scores compared to Alzheimer’s; slower decline | Executive function (poorly detected by MMSE) |
| Parkinson’s Disease Dementia | Difficulties with visuospatial tasks and attention | Motor, constructional skills |
Other Clinical Uses for MMSE
Screening
- Initial cognitive assessment in primary care
- Pre-surgical cognitive screening for elderly
- Baseline assessment for new patients
Monitoring
- Track progression of cognitive disorders
- Evaluate medication effects
- Document changes after interventions
Research
- Standard measure across studies
- Inclusion criteria for clinical trials
- Outcome measurement
Nursing Considerations During Administration
- Environment: Conduct in a quiet, well-lit room with minimal distractions
- Patient Comfort: Ensure the patient is comfortable, not fatigued, and has necessary assistive devices (glasses, hearing aids)
- Building Rapport: Begin with casual conversation to reduce anxiety
- Pain/Discomfort: Address any pain or physical discomfort before beginning
- Timing: Avoid testing during medication transitions or when patient is heavily sedated
- Cultural Sensitivity: Consider cultural and educational factors when interpreting results
- Emotional Support: Be supportive and non-judgmental, especially if patient becomes frustrated
- Documentation: Record verbatim responses when possible, especially for qualitative items
Limitations of the MMSE
- Low sensitivity for mild cognitive impairment (MoCA is preferred)
- Poor detection of executive function impairment
- Educational and cultural biases affect scores
- Ceiling effect in highly educated individuals
- Floor effect in severely impaired individuals
- Does not identify specific causes of cognitive impairment
- Now proprietary and requires licensing for some uses
MMSE Components Mnemonic: “ORAL CL”
Orientation
Time & Place (10 points)
Registration
3 objects (3 points)
Attention & Calculation
Serial 7s or WORLD (5 points)
Language
Naming, repeating, etc. (8 points)
CLosing your eyes
Visual construction (1 point)
MMSE Score Interpretation Mnemonic: “30-24-18-10”
Normal
Mild Impairment
Moderate Impairment
Severe Impairment
Assessment
- Administer MMSE according to standardized guidelines
- Note baseline cognitive status
- Observe behavioral cues during examination
- Document specific areas of difficulty
- Consider contributing factors (medications, environment)
Nursing Diagnoses
- Impaired Memory related to cognitive impairment
- Chronic Confusion related to dementia
- Risk for Injury related to cognitive deficits
- Disturbed Thought Processes
- Self-Care Deficit related to cognitive impairment
Planning & Implementation
- Establish individualized care plan based on cognitive abilities
- Implement safety measures for patients with impairment
- Use clear, simple communication techniques
- Provide orientation cues (clocks, calendars)
- Establish consistent routines to reduce confusion
- Educate family on cognitive status and appropriate expectations
- Refer to appropriate specialists based on findings
Evaluation
- Regularly reassess cognitive status using MMSE
- Monitor for changes in cognitive function over time
- Evaluate effectiveness of interventions
- Assess patient’s ability to maintain independent functioning
- Document progression or improvement
- Adjust care plan based on changes in cognitive status
Case Study 1: Alzheimer’s Disease
Mrs. Johnson, 78, arrives at the clinic with her daughter who reports that her mother has been increasingly forgetful over the past year, getting lost while driving, and has difficulty managing finances.
MMSE Findings:
- Total Score: 19/30
- Orientation: 5/10 (unable to recall date, day, year, floor, and building name)
- Registration: 3/3
- Attention/Calculation: 2/5
- Recall: 0/3 (unable to recall any objects after 5 minutes)
- Language/Visuospatial: 9/9
Nursing Interpretation:
Mrs. Johnson’s MMSE score of 19 suggests mild cognitive impairment. Her pattern of deficits, particularly in orientation and recall with relatively preserved language skills, is consistent with early to moderate Alzheimer’s disease. The complete failure of delayed recall is particularly significant. Nursing interventions should focus on safety measures, memory aids, and caregiver education.
Case Study 2: Delirium vs. Dementia
Mr. Rodriguez, 82, is admitted to the hospital with pneumonia. The night nurse reports confusion, agitation, and hallucinations that worsened during the evening. The medical record indicates a previous MMSE score of 25/30 from his primary care visit 3 months ago.
Current MMSE Findings:
- Total Score: 15/30
- Orientation: 3/10 (significantly disoriented to time and place)
- Registration: 3/3
- Attention/Calculation: 0/5 (unable to concentrate on task)
- Recall: 1/3
- Language/Visuospatial: 8/9
Nursing Interpretation:
The sudden and significant drop in MMSE score (from 25 to 15) with marked attention deficits, worsening in the evening, and presence of hallucinations suggests delirium superimposed on possible mild dementia. The acute change in cognition correlates with his active infection. Nursing priorities include treating the underlying pneumonia, maintaining hydration, frequent reorientation, and ensuring a safe environment until the delirium resolves.
Case Study 3: Depression with Cognitive Effects
Mrs. Garcia, 67, presents with complaints of memory problems and difficulty concentrating for the past 2 months. Her daughter mentions that these symptoms began after her husband’s death, along with poor appetite, disrupted sleep, and social withdrawal.
MMSE Findings:
- Total Score: 24/30
- Orientation: 9/10 (missed current date)
- Registration: 3/3
- Attention/Calculation: 3/5 (struggled with concentration)
- Recall: 2/3 (recalled 2 objects, recognized 3rd with prompting)
- Language/Visuospatial: 7/9 (some difficulty with the intersecting pentagons)
Nursing Interpretation:
Mrs. Garcia’s MMSE score falls at the borderline between normal and mild impairment. The pattern shows primarily attention/concentration deficits rather than significant memory impairment. Combined with her recent bereavement and depressive symptoms, this cognitive pattern is suggestive of “pseudodementia” from depression rather than a primary neurodegenerative disorder. Nursing approach should include depression screening, grief support, and follow-up cognitive testing after treating the depression.
1. Which of the following MMSE scores would indicate moderate cognitive impairment?
A. 26/30
B. 22/30
C. 15/30
D. 8/30
Answer: C. 15/30 (moderate impairment is 10-17)
2. A patient correctly names the year, season, and day of the week, but cannot state the month or date. Which domain of the MMSE is affected, and what would be their score for this section?
A. Registration, 3/5
B. Orientation to time, 3/5
C. Orientation to place, 3/5
D. Language, 3/5
Answer: B. Orientation to time, 3/5
3. A nurse is administering the MMSE to a patient with suspected cognitive impairment. The patient is asked to copy a drawing of intersecting pentagons. This task assesses which of the following?
A. Registration
B. Attention
C. Language
D. Visuospatial ability
Answer: D. Visuospatial ability
4. When scoring the MMSE, a patient spells “WROLD” instead of “WORLD” backwards. Using the line method of scoring, what would their score be?
A. 0/5
B. 3/5
C. 4/5
D. 5/5
Answer: B. 3/5 (Letters D, L, and O are in the correct positions)
5. Which pattern of MMSE deficits would be most consistent with Alzheimer’s disease?
A. Poor attention/calculation with preserved memory
B. Poor recall and orientation with relatively preserved language
C. Poor visuospatial skills with preserved orientation
D. Equal impairment across all domains
Answer: B. Poor recall and orientation with relatively preserved language
