Comprehensive Nail Care for Nursing Students
Nursing Notes
Learning Objectives
Knowledge Goals:
- • Identify nail anatomy and physiology
- • Understand nail assessment techniques
- • Recognize common nail disorders
- • Apply evidence-based nursing interventions
Clinical Skills:
- • Perform systematic nail assessment
- • Implement appropriate nail care protocols
- • Educate patients on nail hygiene
- • Identify when to refer to specialists
Table of Contents
Part I: Foundations
- 1. Nail Anatomy & Physiology
- 2. Nail Growth & Development
- 3. Assessment Techniques
- 4. Normal vs. Abnormal Findings
Part II: Clinical Applications
- 5. Common Nail Disorders
- 6. Nursing Interventions
- 7. Special Populations
- 8. Patient Education
Part I: Foundations
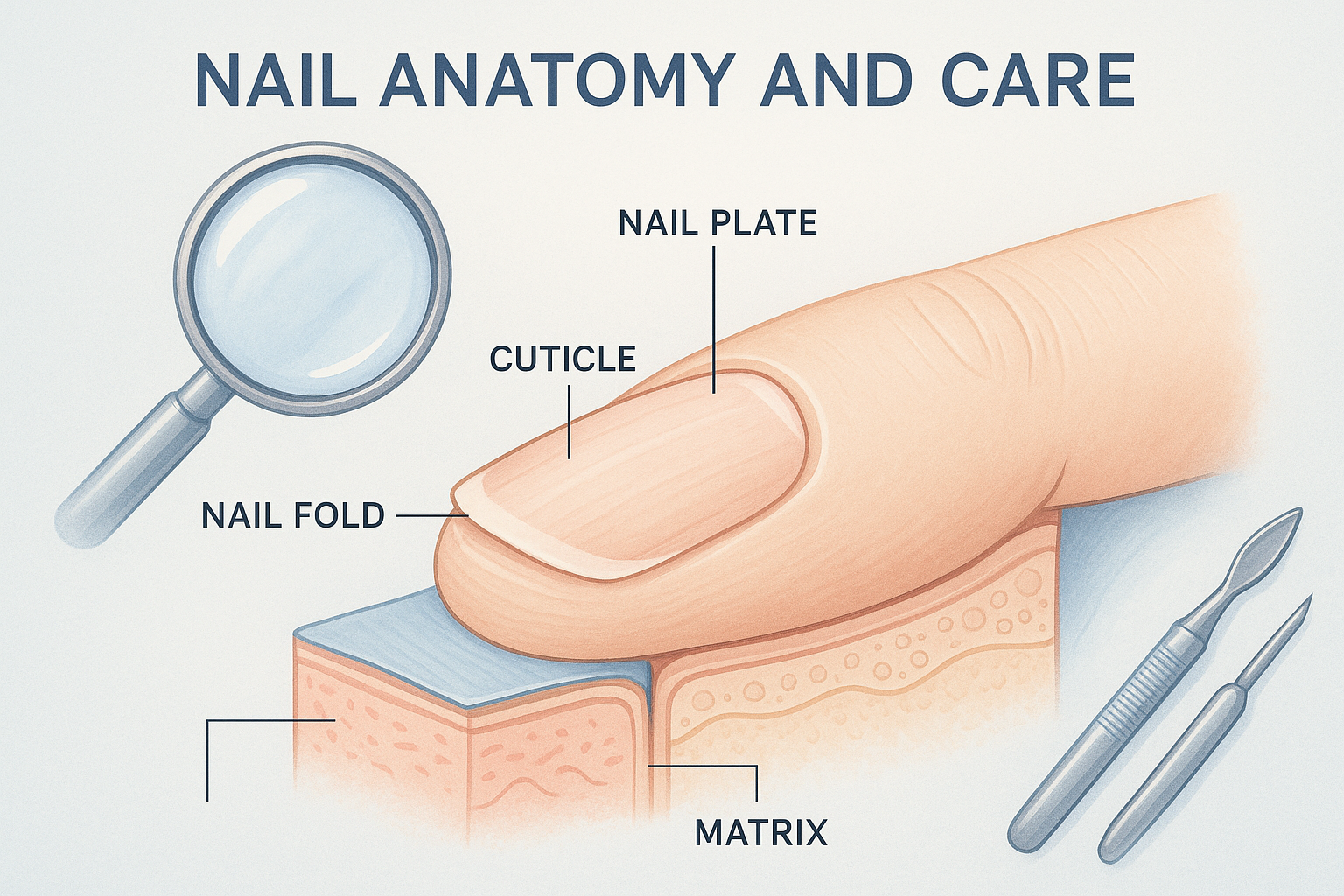
1. Nail Anatomy & Physiology
Nail Unit Structure
External Components:
- Nail Plate: Visible portion, composed of keratin
- Free Edge: Distal portion extending beyond fingertip
- Cuticle (Eponychium): Protective seal at nail base
- Nail Folds: Skin surrounding nail plate
- Lunula: Whitish crescent at nail base
Internal Components:
- Nail Matrix: Growth center beneath cuticle
- Nail Bed: Vascular tissue beneath nail plate
- Hyponychium: Tissue beneath free edge
- Nail Root: Embedded portion in nail groove
- Germinal Matrix: Produces nail cells
Memory Aid: “NAIL PARTS”
Nail Plate – Adherent to bed – Invested by folds – Lunula visible – Produced by matrix – Anchored at root – Regenerated continuously – Terminated at hyponychium – Sealed by cuticle
Clinical Pearl
The nail plate is a window to systemic health. Changes in color, texture, or growth patterns can indicate underlying cardiovascular, respiratory, or metabolic disorders.
2. Nail Growth & Development
Growth Characteristics
- Fingernails: 3-4 mm per month
- Toenails: 1-2 mm per month
- Complete renewal: 4-6 months (fingers), 12-18 months (toes)
- Growth rate factors: Age, health, season, hormones
Physiological Functions
- Protection: Shield finger/toe tips from trauma
- Sensation: Enhance tactile perception
- Function: Assist in grasping and manipulation
- Cosmetic: Contribute to appearance and self-esteem
Important Note
Trauma to the nail matrix can result in permanent nail deformities. Always assess for matrix involvement in nail injuries.
3. Nail Assessment Techniques
Systematic Assessment Approach
Step 1: Inspection
Examine nail color, shape, surface texture, and surrounding tissue under good lighting
Step 2: Palpation
Assess nail thickness, adherence to nail bed, and surrounding tissue temperature
Step 3: Function Testing
Evaluate capillary refill time and nail bed circulation
Step 4: Documentation
Record findings using standardized terminology and measurement
Assessment Mnemonic: “NAIL EXAM”
Note the shape – Assess the color – Inspect the surface – Look at surrounding tissue – Evaluate capillary refill – Xamine for abnormalities – Assess adherence – Measure thickness
Normal Findings
- • Smooth, firm nail plate
- • Translucent with pink undertone
- • Capillary refill < 2 seconds
- • Intact cuticles
- • No clubbing or ridging
- • Appropriate nail length
Abnormal Findings
- • Discoloration (yellow, green, black)
- • Thickening or brittleness
- • Ridging or pitting
- • Clubbing or spooning
- • Separation from nail bed
- • Surrounding inflammation
4. Normal vs. Abnormal Findings
Normal Variants
- Longitudinal ridges: Age-related, benign
- Leukonychia: Small white spots from trauma
- Splinter hemorrhages: Occasional, from minor trauma
- Racial variations: Pigmentation differences
Concerning Findings
- Clubbing: Cardiovascular/respiratory disease
- Koilonychia: Iron deficiency anemia
- Beau’s lines: Systemic illness
- Terry’s nails: Liver disease
Urgent Findings
- Melanonychia: Potential melanoma
- Sudden color changes: Infection or malignancy
- Painful swelling: Acute paronychia
- Dystrophic changes: Severe infection
Clinical Pearl: Capillary Refill Test
Press nail bed until blanched, release pressure, observe return to pink color. Normal refill time is < 2 seconds in adults, < 3 seconds in elderly. Prolonged refill may indicate poor circulation or shock.
Part II: Clinical Applications
5. Common Nail Disorders
Paronychia
Definition & Pathophysiology
Infection of the nail fold, commonly caused by Staphylococcus aureus or Streptococcus species. Results from breaks in the skin barrier around the nail.
Clinical Presentation
- • Acute: Pain, swelling, erythema, purulent drainage
- • Chronic: Thickened nail fold, minimal pain
- • May involve single or multiple digits
- • Warmth and tenderness to touch
Risk Factors
- • Nail biting or picking
- • Aggressive manicuring
- • Frequent hand washing
- • Diabetes mellitus
- • Immunocompromised state
Nursing Interventions
- • Warm soaks 3-4 times daily
- • Topical or systemic antibiotics
- • Drainage if abscess present
- • Patient education on prevention
Onychomycosis (Fungal Nail Infection)
Definition & Pathophysiology
Fungal infection of the nail plate, commonly caused by dermatophytes (Trichophyton rubrum), yeasts, or molds. Accounts for 40% of all nail disorders.
Clinical Presentation
- • Discoloration (yellow, brown, white)
- • Thickening and brittleness
- • Subungual debris
- • Nail separation (onycholysis)
- • Typically painless
Risk Factors
- • Advanced age
- • Immunosuppression
- • Diabetes mellitus
- • Peripheral vascular disease
- • Trauma to nail
- • Communal bathing facilities
Nursing Interventions
- • Fungal culture confirmation
- • Topical antifungal therapy
- • Oral antifungals for severe cases
- • Nail hygiene education
- • Environmental modifications
Ingrown Nails (Onychocryptosis)
Definition & Pathophysiology
Condition where nail edge grows into surrounding skin, causing pain, inflammation, and potential infection. Most common in great toes.
Clinical Presentation
- • Pain and tenderness
- • Erythema and swelling
- • Granulation tissue formation
- • Purulent drainage if infected
- • Difficulty wearing shoes
Risk Factors
- • Improper nail trimming
- • Tight-fitting shoes
- • Genetic predisposition
- • Nail trauma
- • Hyperhidrosis
Nursing Interventions
- • Conservative management: soaks, cotton placement
- • Proper nail trimming technique
- • Footwear modifications
- • Referral for surgical intervention
- • Infection prevention strategies
Disorder Memory Aid: “PIO”
Paronychia – Painful, purulent, proximal nail fold infection
Ingrown nail – Inward growth causing inflammation
Onychomycosis – Opportunistic fungal infection
6. Nursing Interventions
General Nail Care Protocol
Nail Care Assessment & Intervention Flowchart
→ Preventive Care
→ Therapeutic Care
→ Immediate Referral
Preventive Interventions
- Education: Proper nail hygiene techniques
- Trimming: Straight across, not too short
- Moisturizing: Cuticle and nail bed care
- Footwear: Proper fit and ventilation
- Environmental: Dry, clean conditions
- Nutrition: Adequate protein and vitamins
Therapeutic Interventions
- Soaking: Warm water with antiseptic
- Debridement: Removal of diseased tissue
- Topical therapy: Antifungal or antibiotic
- Systemic therapy: Oral medications
- Surgical referral: For severe cases
- Wound care: Proper dressing techniques
Clinical Pearl: Nail Trimming Technique
Use clean, sharp nail clippers. Cut nails straight across, then gently round corners with an emery board. Avoid cutting too short to prevent ingrown nails. For thick nails, soften with warm water first.
7. Special Populations
Diabetic Patients
Special Considerations
- • Impaired wound healing
- • Increased infection risk
- • Peripheral neuropathy
- • Vascular compromise
- • Higher complication rates
Assessment Priorities
- • Daily foot inspection
- • Circulation assessment
- • Sensation testing
- • Glycemic control status
Nursing Interventions
- • Professional nail care only
- • Gentle cleaning and moisturizing
- • Proper footwear education
- • Early intervention for problems
- • Multidisciplinary team approach
Patient Education
- • Never cut nails too short
- • Report changes immediately
- • Maintain good blood sugar control
- • Avoid over-the-counter treatments
Elderly Patients
Age-Related Changes
- • Slower nail growth
- • Increased thickness
- • Reduced circulation
- • Decreased mobility
- • Multiple comorbidities
Nursing Considerations
- • Assess self-care ability
- • Provide or arrange nail care
- • Monitor for complications
- • Adapt techniques for limitations
- • Involve family caregivers
High-Risk Patient Alert
Patients with diabetes, peripheral vascular disease, or immunocompromised states require specialized nail care protocols. Never attempt nail care on high-risk patients without proper training and assessment.
8. Patient Education
Home Care Instructions
- Daily hygiene: Wash and dry thoroughly
- Proper trimming: Straight across, not curved
- Moisturizing: Use appropriate lotions
- Footwear: Clean, dry, well-fitting shoes
- Inspection: Daily examination for changes
- Seeking help: When to contact healthcare provider
Prevention Strategies
- Avoid trauma: Protect nails from injury
- Proper tools: Use clean, appropriate instruments
- Professional care: Regular podiatrist visits
- Environmental control: Avoid damp conditions
- Nutrition: Adequate protein and vitamins
- Lifestyle: Smoking cessation, exercise
Patient Education Mnemonic: “CLEAN NAILS”
Cut straight across – Limit moisture exposure – Examine daily – Avoid tight shoes – Never share tools – Nourish with moisturizer – Always use clean instruments – Inspect for changes – Limit trauma – Seek professional help when needed
Teaching Strategy
Use demonstrate-practice-return demonstration technique. Provide written instructions with visual aids. Tailor education to patient’s literacy level and cultural background. Include family members in education sessions.
Clinical Application Scenarios
Scenario 1: Diabetic Patient
Situation: 65-year-old diabetic patient with thick, yellowish toenails
Assessment:
- • Check circulation and sensation
- • Assess for signs of infection
- • Review glycemic control
- • Document nail appearance
Intervention:
- • Refer to podiatrist
- • Educate on daily inspection
- • Recommend proper footwear
- • Schedule regular follow-ups
Scenario 2: Acute Paronychia
Situation: 30-year-old with painful, swollen finger nail fold
Assessment:
- • Evaluate pain level and swelling
- • Check for purulent drainage
- • Assess for systemic symptoms
- • Document progression
Intervention:
- • Initiate warm soaks
- • Administer prescribed antibiotics
- • Provide pain management
- • Monitor for improvement
Quick Reference Guide
Normal Assessment
- • Smooth, translucent nail plate
- • Pink nail bed
- • Capillary refill < 2 seconds
- • Intact cuticles
- • No pain or tenderness
- • Appropriate thickness
Warning Signs
- • Sudden color changes
- • Persistent pain
- • Swelling or warmth
- • Purulent drainage
- • Nail separation
- • Systemic symptoms
Immediate Action Required
- • Cellulitis spreading
- • Abscess formation
- • Diabetic with infection
- • Severe trauma
- • Suspected melanoma
- • Compromised circulation
Key Takeaways
Clinical Competencies
- • Systematic nail assessment is essential for early detection of disorders
- • Proper nail care prevents complications and promotes healing
- • Patient education is crucial for long-term nail health
- • Special populations require individualized approaches
Professional Responsibilities
- • Recognize when to refer to specialists
- • Maintain sterile technique during procedures
- • Document findings accurately and completely
- • Stay current with evidence-based practices
References
- 1. National Center for Biotechnology Information. (2023). Integumentary Assessment – Nursing Skills. https://www.ncbi.nlm.nih.gov/books/NBK593218/
- 2. American Academy of Family Physicians. (2022). Optimal diagnosis and management of common nail disorders. https://pmc.ncbi.nlm.nih.gov/articles/PMC8896184/
- 3. Nurseslabs. (2024). Nail Care and Hygiene. https://nurseslabs.com/nail-care-and-hygiene/
- 4. StatPearls Publishing. (2023). Paronychia. https://www.ncbi.nlm.nih.gov/books/NBK544307/
- 5. American Nurse Journal. (2024). Foot assessment and care. https://www.myamericannurse.com/foot-assessment-and-care/
