Nursing Care of Eyes, Ears & Nose
Comprehensive Guide to Hygiene, Assessment & Management of Assistive Devices
Eye Care
Ear Care
Nose Care
Table of Contents
Introduction to Sensory Care Nursing
Anatomical overview of sensory organs requiring specialized nursing care
The care of eyes, ears, and nose represents a fundamental aspect of nursing practice that directly impacts patient comfort, safety, and overall quality of life. These sensory organs serve as vital gateways to our understanding of the world, making their proper care essential for maintaining optimal patient health outcomes.
Why Sensory Care Matters
Proper sensory care nursing encompasses far more than basic hygiene. It involves comprehensive assessment, skilled intervention, and thoughtful management of assistive devices that can significantly impact patient independence and dignity.
- Prevention of infections and complications
- Maintenance of optimal sensory function
- Enhancement of patient comfort and well-being
- Promotion of independence through proper device management
Eye Care
Visual health maintenance and ocular hygiene protocols
Ear Care
Auditory health and hearing aid management
Nose Care
Nasal hygiene and respiratory support
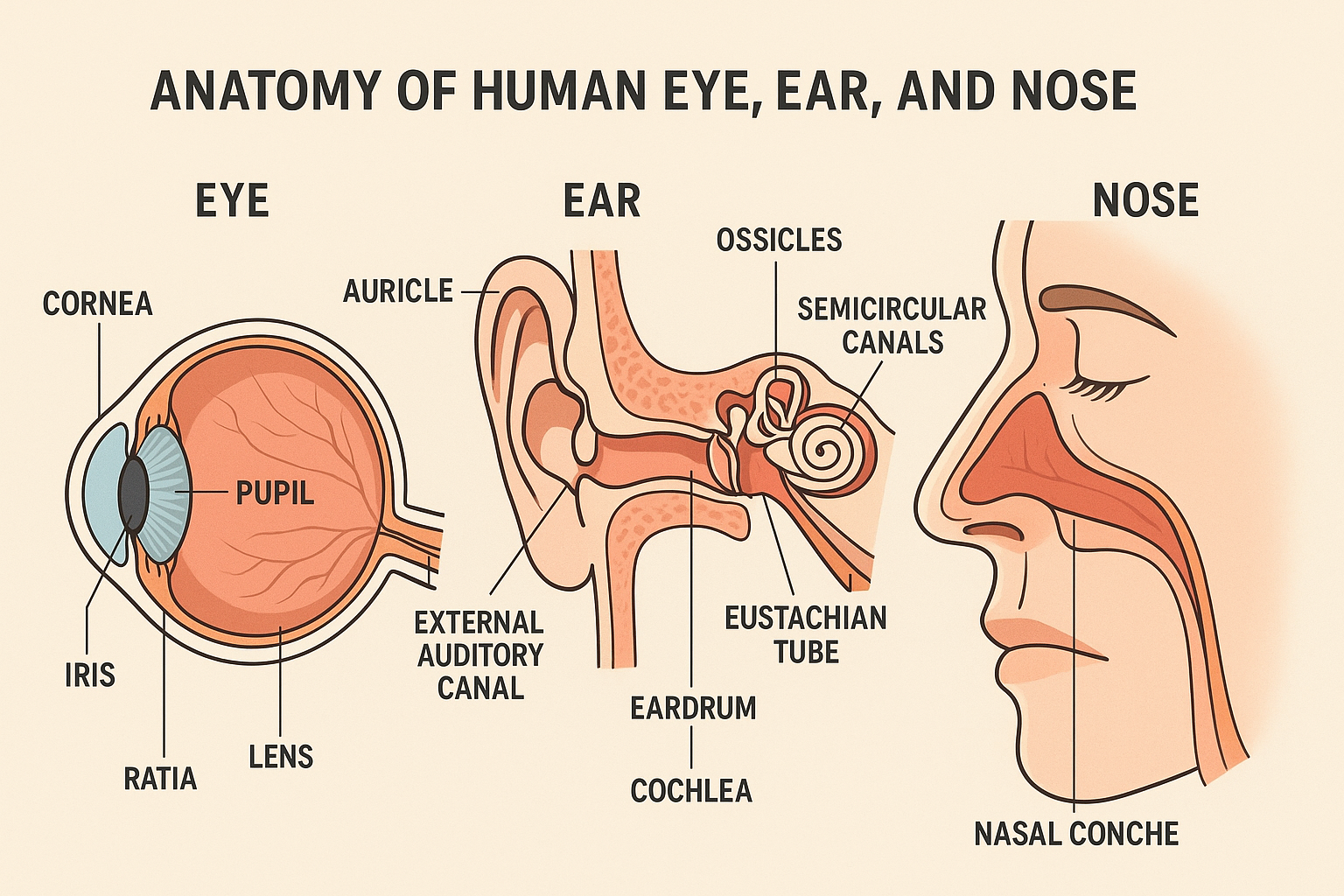
Anatomy & Physiology Overview
Understanding Sensory Structures
A thorough understanding of sensory organ anatomy is crucial for effective nursing care. Each organ has unique structures and functions that require specialized attention and care protocols.
Eye Anatomy
- Cornea: Clear front layer
- Iris: Colored part of eye
- Pupil: Central opening
- Lens: Focuses light
- Retina: Light-sensitive tissue
- Conjunctiva: Protective membrane
Ear Anatomy
- External ear: Auricle and canal
- Eardrum: Tympanic membrane
- Middle ear: Ossicles (bones)
- Inner ear: Cochlea and vestibule
- Eustachian tube: Pressure equalizer
- Cerumen: Protective wax
Nose Anatomy
- Nostrils: External openings
- Nasal cavity: Air-filled space
- Turbinates: Scroll-like structures
- Nasal septum: Dividing wall
- Sinuses: Air-filled chambers
- Mucous membrane: Protective lining
Memory Aid: “SENSE” Assessment
Symptoms
Examination
Normal function
Safety measures
Education
Eye Care Nursing
Eye care nursing involves comprehensive attention to ocular health, from basic hygiene to complex interventions. Proper eye care is essential for maintaining sensory function and preventing complications that could lead to vision impairment.
Basic Eye Hygiene
-
1Hand hygiene: Perform thorough hand washing before any eye care procedure
-
2Gentle cleansing: Use sterile saline or prescribed solution from inner to outer canthus
-
3Separate supplies: Use different cotton balls/gauze for each eye
-
4Moisture removal: Gently pat dry without rubbing
Signs Requiring Immediate Attention
| Condition | Nursing Interventions | Patient Education |
|---|---|---|
| Dry Eyes | Apply artificial tears, maintain humidity, protect from wind | Blink frequently, use humidifier, avoid smoke |
| Conjunctivitis | Apply warm compresses, administer prescribed drops, isolate if infectious | Hand hygiene, avoid touching eyes, don’t share personal items |
| Post-surgical Care | Monitor for complications, apply eye shield, position appropriately | Activity restrictions, medication compliance, follow-up appointments |
| Eye Trauma | Assess extent, apply eye shield, prepare for emergency intervention | Immediate medical attention, avoid rubbing, protect unaffected eye |
Critical Safety Considerations
- Never use cotton swabs or pointed objects near the eye
- Always work from clean to dirty areas during eye care
- Use only sterile solutions and supplies for eye care
- Report any sudden changes in vision or eye appearance immediately
- Ensure proper lighting during eye care procedures
Ear Care Nursing
Ear care nursing focuses on maintaining auditory health and preventing complications while preserving the delicate structures of the ear. Proper ear care is vital for maintaining sensory function and preventing infections that could lead to hearing loss.
External Ear Care
Assessment Parameters
Memory Aid: “HEAR” Assessment
Hearing ability
External appearance
Auditory canal
Red flags/pain
| Condition | Signs & Symptoms | Nursing Interventions |
|---|---|---|
| Otitis Externa | Ear pain, discharge, itching, hearing loss | Keep ear dry, apply topical medications, pain management |
| Cerumen Impaction | Feeling of fullness, hearing loss, tinnitus | Ear irrigation, wax softening drops, professional removal |
| Hearing Loss | Difficulty hearing, asking for repetition | Audiometry referral, hearing aid evaluation, communication strategies |
| Tinnitus | Ringing, buzzing, or clicking sounds | Identify triggers, stress management, sound therapy |
Ear Care Safety Guidelines
DO:
- • Use proper lighting during examination
- • Follow sterile technique for procedures
- • Document all findings accurately
- • Provide patient education on ear care
DON’T:
- • Insert anything into the ear canal
- • Use excessive force during cleaning
- • Ignore patient complaints of pain
- • Perform ear irrigation if eardrum is perforated
Nose Care Nursing
Nose care nursing encompasses maintaining nasal hygiene, managing respiratory function, and preventing complications related to nasal conditions. Proper nasal care is essential for maintaining sensory function including smell and taste, as well as supporting respiratory health.
Nasal Hygiene Techniques
Common Nasal Conditions
Epistaxis (Nosebleed) Management
Immediate Actions:
- 1. Stay calm and reassure patient
- 2. Position patient upright, leaning forward
- 3. Apply direct pressure to soft part of nose
- 4. Hold pressure for 10-15 minutes continuously
- 5. Apply cold compress to bridge of nose
When to Seek Help:
- • Bleeding continues after 20 minutes
- • Heavy bleeding with difficulty breathing
- • Signs of hypovolemic shock
- • Recurrent episodes
- • Associated with trauma or medication
| Assessment Area | Normal Findings | Abnormal Findings | Nursing Actions |
|---|---|---|---|
| External Nose | Symmetric, no deformity | Swelling, deformity, trauma | Document, assess for fracture |
| Nasal Patency | Clear airflow bilaterally | Obstruction, mouth breathing | Identify cause, promote drainage |
| Nasal Discharge | Minimal clear secretions | Purulent, bloody, excessive | Culture if indicated, monitor |
| Smell Function | Intact olfactory sense | Decreased or absent smell | Assess cause, refer if needed |
Best Practices for Nasal Care
Prevention:
- • Maintain adequate humidity
- • Avoid nasal trauma
- • Use saline rinses regularly
- • Manage allergies effectively
Intervention:
- • Gentle suction techniques
- • Proper medication administration
- • Monitor for complications
- • Ensure patient comfort
Education:
- • Proper nose blowing technique
- • When to seek medical care
- • Medication compliance
- • Environmental modifications
Hygiene Practices for Sensory Organs
Proper hygiene practices are fundamental to maintaining optimal sensory organ health and preventing infections. These practices must be adapted to each patient’s individual needs, condition, and level of independence.
Independent Patients
Dependent Patients
Memory Aid: “CLEAN” Hygiene Protocol
Clean hands first
Light positioning
Explain procedure
Assess before/after
Note observations
| Organ System | Frequency | Supplies Needed | Special Considerations |
|---|---|---|---|
| Eyes | Daily or as needed | Sterile saline, cotton balls, gloves | Inner to outer canthus, separate supplies per eye |
| Ears | Weekly or as needed | Soft cloth, warm water, towel | External cleaning only, no insertion |
| Nose | As needed | Saline solution, soft tissues, suction | Gentle technique, monitor for bleeding |
| All Systems | Before procedures | Hand sanitizer, PPE, documentation | Standard precautions, patient dignity |
Quality Assurance in Hygiene Care
Documentation Requirements:
- • Time and date of care provided
- • Patient response and tolerance
- • Abnormal findings or concerns
- • Supplies used and techniques employed
- • Patient education provided
Continuous Improvement:
- • Regular competency assessments
- • Patient feedback collection
- • Infection control monitoring
- • Staff education updates
- • Equipment maintenance schedules
Assessment Techniques for Sensory Organs
Comprehensive assessment of sensory organs requires systematic evaluation using multiple techniques. These assessments help identify problems early, monitor treatment effectiveness, and guide nursing interventions.
Visual Assessment
- Inspection: External structures, symmetry, discharge
- Visual acuity: Snellen chart, near vision card
- Visual fields: Confrontation test
- Pupil response: PERRLA assessment
- Extraocular movements: Six cardinal directions
Auditory Assessment
- Inspection: External ear, canal, tympanic membrane
- Hearing tests: Whisper test, Weber test, Rinne test
- Otoscopic exam: Ear canal and eardrum visualization
- Balance assessment: Romberg test, gait evaluation
- Symptom evaluation: Tinnitus, vertigo, pain
Nasal Assessment
- External inspection: Shape, symmetry, skin condition
- Patency test: Airflow assessment each nostril
- Smell testing: Olfactory function evaluation
- Internal examination: Nasal speculum inspection
- Sinus assessment: Palpation and percussion
PERRLA Assessment Technique
Pupils
Size and shape
Equal
Symmetric response
Reactive
To light
Round
Circular shape
Light
Accommodation
| Assessment Tool | Purpose | Normal Findings | Abnormal Findings |
|---|---|---|---|
| Snellen Chart | Visual acuity testing | 20/20 vision | 20/40 or worse, refer for evaluation |
| Weber Test | Hearing lateralization | Sound heard equally in both ears | Sound lateralized to one ear |
| Rinne Test | Bone vs air conduction | Air conduction > bone conduction | Bone conduction > air conduction |
| Otoscope | Ear canal and eardrum exam | Clear canal, intact gray tympanic membrane | Wax impaction, inflammation, perforation |
Red Flag Findings Requiring Immediate Attention
Eye:
- • Sudden vision loss
- • Unequal pupil size
- • Severe eye pain
- • Flashing lights/floaters
- • Chemical exposure
Ear:
- • Sudden hearing loss
- • Severe ear pain
- • Bloody discharge
- • Facial paralysis
- • Severe vertigo
Nose:
- • Severe nosebleeds
- • Nasal trauma
- • Complete obstruction
- • CSF leak (clear fluid)
- • Severe facial pain
Management of Assistive Devices
Proper management of assistive devices is crucial for maintaining sensory function and patient independence. These devices require specialized care, regular maintenance, and patient education to ensure optimal performance and safety.
Eyeglasses & Contact Lenses
Eyeglasses Care:
- • Clean with microfiber cloth and lens solution
- • Store in protective case when not in use
- • Check for loose screws or damage regularly
- • Ensure proper fit and comfort
Contact Lens Care:
- • Follow strict hygiene protocols
- • Use appropriate cleaning solutions
- • Monitor for signs of infection
- • Respect wearing time limits
Hearing Aids
Daily Maintenance:
- • Check battery levels regularly
- • Clean with dry cloth or special brush
- • Remove at night and store properly
- • Protect from moisture and heat
Troubleshooting:
- • No sound: Check battery, clean device
- • Whistling: Adjust fit, check for blockage
- • Weak sound: Replace battery, clean
- • Discomfort: Check fit, consult audiologist
Memory Aid: “CARE” for Assistive Devices
Clean regularly
Assess function
Replace when needed
Educate patient
| Device Type | Cleaning Method | Storage | Replacement Schedule |
|---|---|---|---|
| Eyeglasses | Mild soap and water, lens cleaner | Protective case, avoid heat | As needed for damage/prescription change |
| Contact Lenses | Approved cleaning solutions only | Clean case with fresh solution | Daily, weekly, or monthly per type |
| Hearing Aids | Dry brush, wax removal tools | Dry case, remove batteries | 5-7 years, batteries weekly |
| Magnifying Devices | Gentle cleaning with soft cloth | Protective case, avoid drops | As needed for damage |
Patient Education for Device Management
Teaching Points:
- • Proper insertion and removal techniques
- • Daily care and maintenance routines
- • Signs of malfunction or damage
- • When to seek professional help
- • Backup options and emergency procedures
Documentation:
- • Device type and specifications
- • Patient competency in use
- • Problems encountered and solutions
- • Follow-up appointments scheduled
- • Patient understanding of care requirements
Infection Prevention in Sensory Care
Infection prevention is paramount in sensory organ care due to the delicate nature of these structures and their proximity to the brain. Proper infection control measures protect both patients and healthcare providers while maintaining optimal therapeutic outcomes.
Common Infections
Eye Infections:
- • Conjunctivitis (bacterial, viral, allergic)
- • Stye (hordeolum)
- • Chalazion
- • Keratitis
Ear Infections:
- • Otitis externa (swimmer’s ear)
- • Otitis media
- • Mastoiditis
- • Fungal infections
Prevention Strategies
Standard Precautions:
- • Hand hygiene before and after care
- • Use of appropriate PPE
- • Proper disposal of contaminated materials
- • Equipment disinfection
Transmission Prevention:
- • Avoid cross-contamination between eyes/ears
- • Use sterile supplies for each procedure
- • Isolate patients with contagious conditions
- • Educate patients on prevention measures
Infection Control Protocols
Pre-Procedure:
- 1. Assess patient for signs of infection
- 2. Perform hand hygiene
- 3. Gather sterile supplies
- 4. Don appropriate PPE
- 5. Explain procedure to patient
During Procedure:
- 1. Maintain sterile technique
- 2. Use separate supplies for each eye/ear
- 3. Avoid contamination of clean areas
- 4. Monitor for patient discomfort
- 5. Document all observations
Post-Procedure:
- 1. Dispose of contaminated materials
- 2. Remove PPE properly
- 3. Perform hand hygiene
- 4. Clean and disinfect equipment
- 5. Monitor for complications
| Infection Type | Early Signs | Nursing Interventions | Isolation Precautions |
|---|---|---|---|
| Bacterial Conjunctivitis | Purulent discharge, redness, pain | Antibiotic drops, warm compresses | Contact precautions until 24h treatment |
| Viral Conjunctivitis | Watery discharge, itching, URI symptoms | Supportive care, cold compresses | Contact precautions, highly contagious |
| Otitis Externa | Ear pain, discharge, hearing loss | Topical antibiotics, pain management | Standard precautions |
| Sinusitis | Facial pain, congestion, fever | Decongestants, antibiotics if bacterial | Standard precautions |
High-Risk Situations Requiring Special Attention
Patient Risk Factors:
- • Immunocompromised patients
- • Diabetes mellitus
- • Recent surgery or trauma
- • Use of contact lenses
- • Chronic conditions (allergies, dry eyes)
Environmental Risks:
- • Healthcare facility-acquired infections
- • Contaminated water or solutions
- • Shared equipment or supplies
- • Poor ventilation systems
- • Inadequate cleaning protocols
Patient Education for Sensory Care
Effective patient education is essential for promoting optimal sensory health and preventing complications. Education should be tailored to individual patient needs, learning styles, and health literacy levels to ensure comprehension and compliance.
Teaching Strategies
Demonstration:
Show proper techniques for eye care, ear cleaning, and device management
Return Demonstration:
Have patient perform procedures to confirm understanding
Written Materials:
Provide clear, illustrated instructions for home reference
Multimedia Resources:
Use videos, apps, and interactive tools for learning
Family Involvement
Caregiver Training:
Educate family members on proper care techniques
Support Systems:
Encourage family participation in care planning
Emergency Procedures:
Teach recognition of problems requiring immediate attention
Communication:
Provide strategies for effective communication with healthcare team
Memory Aid: “TEACH” Method
Tell them what to do
Explain why it’s important
Allow practice time
Check understanding
Help with follow-up
| Topic Area | Key Teaching Points | Demonstration Required | Follow-up Needed |
|---|---|---|---|
| Eye Care | Proper handwashing, medication administration, signs of infection | Eye drop instillation, cleaning technique | Vision changes, medication effects |
| Ear Care | Hearing aid maintenance, when to clean ears, infection prevention | Hearing aid insertion, battery replacement | Hearing changes, device problems |
| Nasal Care | Proper blowing technique, humidity importance, medication use | Nasal rinse procedure, medication administration | Breathing difficulties, medication effectiveness |
| Device Care | Cleaning schedules, storage methods, replacement timelines | Proper cleaning technique, insertion/removal | Device function, comfort issues |
Evaluation of Patient Learning
Assessment Methods:
- • Return demonstration of skills
- • Verbal explanation of procedures
- • Problem-solving scenarios
- • Written or oral quizzes
- • Observation of home care practices
Success Indicators:
- • Correct technique performance
- • Appropriate problem identification
- • Timely medication administration
- • Infection-free outcomes
- • Confident self-care abilities
Global Best Practices in Sensory Care
Learning from international best practices enhances sensory care quality and patient outcomes. These evidence-based approaches have been successfully implemented in various healthcare systems worldwide.
Scandinavian Model
Preventive Focus:
Emphasis on early detection and preventive care through regular screenings
Interprofessional Teams:
Collaborative approach with audiologists, optometrists, and nurses
Patient-Centered Care:
Individualized care plans based on patient preferences and needs
Canadian Approach
Quality Indicators:
Standardized metrics for measuring sensory care quality
Technology Integration:
Electronic health records with specialized sensory assessment tools
Community Support:
Strong links between hospital and community care services
Evidence-Based Innovations
Japanese Precision:
- • Micro-surgical techniques
- • Advanced diagnostic equipment
- • Minimal invasive procedures
- • Detailed documentation protocols
Australian Innovation:
- • Telehealth sensory consultations
- • Mobile assessment units
- • AI-assisted diagnostics
- • Rural care delivery models
Netherlands Efficiency:
- • Streamlined care pathways
- • Nurse-led clinics
- • Predictive analytics
- • Cost-effective solutions
| Country/Region | Key Innovation | Implementation Strategy | Measured Outcomes |
|---|---|---|---|
| Singapore | Integrated sensory care centers | One-stop multidisciplinary clinics | Reduced wait times, improved satisfaction |
| United Kingdom | Nurse specialist programs | Advanced practice nurses in sensory care | Enhanced quality, reduced costs |
| Germany | Preventive screening protocols | Mandatory workplace assessments | Early detection, reduced complications |
| South Korea | Digital health platforms | Mobile apps for sensory monitoring | Improved adherence, better outcomes |
Implementing Best Practices
Adaptation Strategies:
- • Assess current practice gaps
- • Pilot small-scale implementations
- • Gather stakeholder feedback
- • Modify based on local context
- • Scale successful interventions
Success Factors:
- • Strong leadership support
- • Adequate resource allocation
- • Staff training and education
- • Continuous quality monitoring
- • Patient and family engagement
Conclusion
The nursing care of eyes, ears, and nose represents a critical component of comprehensive healthcare that directly impacts patient quality of life and independence. Throughout this comprehensive guide, we have explored the multifaceted nature of sensory care nursing, from basic hygiene practices to complex assistive device management.
Key Takeaways
- Proper sensory care requires comprehensive assessment and individualized interventions
- Infection prevention is paramount in maintaining sensory organ health
- Patient education empowers individuals to maintain optimal sensory function
- Assistive devices require specialized knowledge and careful management
Future Directions
- Integration of technology in sensory care delivery
- Advanced practice roles in specialized sensory nursing
- Preventive care models focusing on early intervention
- Research-driven improvements in patient outcomes
The Impact of Quality Sensory Care
When nurses provide excellent sensory care, the benefits extend far beyond the immediate clinical outcomes. Patients experience:
Improved Quality of Life
Enhanced Independence
Better Social Connection
Reduced Complications
Continuing Professional Development
Excellence in sensory care nursing requires ongoing commitment to learning and professional growth. Consider these development opportunities:
Formal Education:
- • Specialty certification programs
- • Advanced practice degrees
- • Continuing education courses
- • Professional conferences
Professional Networks:
- • Specialty nursing organizations
- • Research collaborations
- • Mentorship programs
- • Quality improvement initiatives
By mastering the principles and practices outlined in this guide, nursing professionals can provide exceptional sensory care that truly makes a difference in patients’ lives. The journey of learning and improvement in sensory care nursing is ongoing, and every step forward contributes to better patient outcomes and enhanced quality of life.
