Nursing Care of Patients with Indwelling Urinary Catheters
Comprehensive Guide to Urinary Drainage Systems
Learning Objectives
Anatomy and Physiology Review
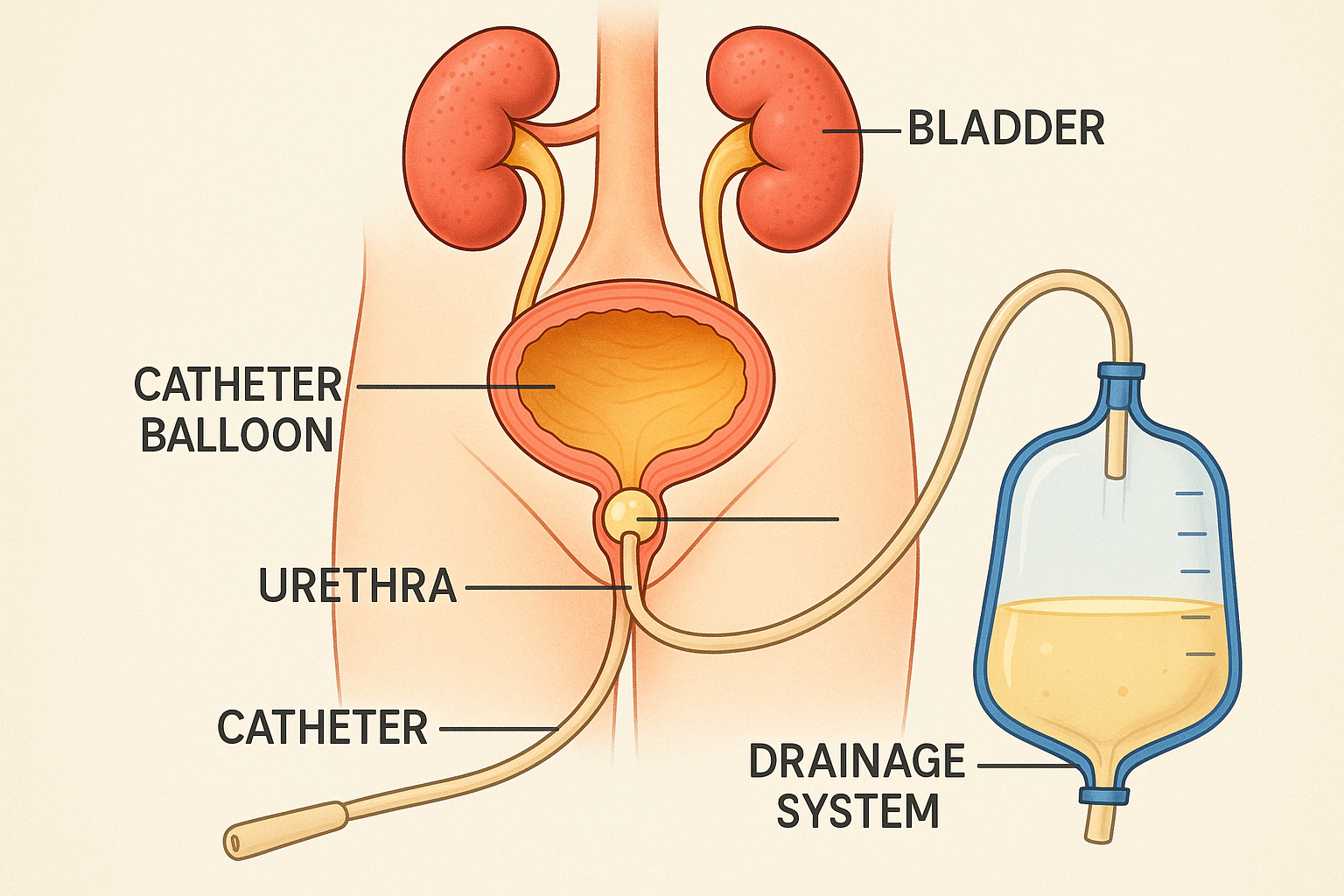
Figure 1: Cross-sectional view of the urinary system with properly placed indwelling catheter
Key Anatomical Structures
Bladder (Vesica Urinaria)
Hollow, muscular organ that stores urine. Capacity: 300-500 mL in adults
Urethra
Tube connecting bladder to external environment. Length: 3-4 cm (female), 15-20 cm (male)
Urethral Sphincters
Internal (involuntary) and external (voluntary) sphincters control urination
Physiological Considerations
Normal Urine Production
- Average output: 1-2 L/day (30-50 mL/hour)
- Minimum output: 0.5 mL/kg/hour
- Color: Pale yellow to amber
- Specific gravity: 1.003-1.030
Micturition Reflex
The bladder’s stretch receptors trigger the micturition reflex at ~150-200 mL capacity. Catheterization bypasses this normal mechanism.
Catheter Types and Sizing
Foley Catheter
- Design: Two-way with inflatable balloon
- Balloon volume: 5-30 mL
- Most common: 10 mL balloon
- Material: Latex or silicone
Three-way Catheter
- Design: Additional irrigation lumen
- Use: Continuous bladder irrigation
- Indication: Post-surgical bleeding
- Size: Typically 20-24 Fr
Suprapubic Catheter
- Insertion: Through abdominal wall
- Advantage: Reduced UTI risk
- Use: Long-term catheterization
- Size: 12-16 Fr typically
French Sizing System
| Patient Population | Recommended Size (Fr) | Color Code | Balloon Volume |
|---|---|---|---|
| Pediatric (2-12 years) | 5-10 Fr | Green/Blue | 3-5 mL |
| Adult Female | 12-14 Fr | Orange/Red | 10 mL |
| Adult Male | 14-16 Fr | Red/Brown | 10 mL |
| Hematuria/Clots | 18-24 Fr | Yellow/Purple | 30 mL |
Memory Aid: French Size Selection
“Small Kids Get Frustrated Making Big Decisions”
- Small (5-8 Fr) – Pediatric
- Kids (10-12 Fr) – Adolescent/Small Adult
- Get (12-14 Fr) – Adult Female
- Frustrated (14-16 Fr) – Adult Male
- Making (18-20 Fr) – Post-surgical
- Big (22-24 Fr) – Hematuria/Clots
- Decisions (26+ Fr) – Specialized procedures
Indications and Contraindications
Appropriate Indications
- Urinary retention – Acute or chronic inability to void
- Perioperative management – Major surgery with expected prolonged immobility
- Accurate I&O monitoring – Critically ill patients requiring precise fluid balance
- Neurogenic bladder – Spinal cord injury, multiple sclerosis
- Genitourinary surgery – Prostate, bladder, or urethral procedures
- Comfort care – End-of-life care to maintain dignity
Contraindications
- Urethral trauma – Suspected urethral injury or stricture
- Severe prostatitis – Acute inflammation of prostate
- Patient refusal – Competent patient refuses procedure
- Convenience purposes – Staff convenience, incontinence management
- Pelvic fracture – Risk of urethral injury
- Allergy to materials – Latex or catheter materials
Clinical Pearl: The “CAUTI-ous” Approach
Always ask yourself: “Is this catheter still necessary?”
Remember: Every day a catheter remains increases infection risk by 3-7%. The best catheter is no catheter when medically appropriate.
Sterile Insertion Procedure
Critical Safety Reminders
- Never force the catheter – Risk of urethral trauma
- Verify urine flow before balloon inflation – Prevents urethral damage
- Use only sterile water for balloon inflation – Prevents balloon rupture
Pre-Insertion Checklist
Patient Assessment
- ☐ Verify physician order
- ☐ Check allergies (latex, betadine)
- ☐ Assess cognitive status
- ☐ Evaluate mobility/positioning
- ☐ Review medical history
Equipment Preparation
- ☐ Sterile catheter kit
- ☐ Appropriate catheter size
- ☐ Sterile gloves
- ☐ Adequate lighting
- ☐ Privacy measures
Step-by-Step Insertion Procedure
Patient Preparation
Explain procedure, obtain consent, ensure privacy and comfort
Hand Hygiene and Gloving
Perform thorough hand hygiene, don sterile gloves
Sterile Field Setup
Open catheter kit, arrange supplies on sterile field
Perineal Cleansing
Clean urethral meatus with antiseptic solution
Catheter Insertion
Insert catheter slowly until urine flows, then advance 1-2 inches more
Balloon Inflation
Inflate balloon with sterile water as indicated on catheter
Secure and Connect
Gently pull back until resistance felt, connect to drainage bag
Memory Aid: “STERILE” Insertion
- Set up sterile field
- Test balloon before insertion
- Explain procedure to patient
- Retract foreskin (male) or separate labia (female)
- Insert catheter slowly until urine flows
- Lubricate catheter tip adequately
- Ensure balloon inflation after urine flow
Maintenance and Daily Care
Daily Care Routine
- Perineal hygiene – Clean with soap and water daily
- Catheter cleaning – Clean 4-6 inches of catheter from meatus outward
- Secure properly – Tape to thigh allowing catheter movement
- Maintain position – Keep drainage bag below bladder level
Drainage System Management
- Gravity drainage – Ensure unobstructed flow to bag
- Empty regularly – When 1/2 to 2/3 full or every 8 hours
- Avoid disconnection – Keep closed system intact
- Monitor output – Document color, clarity, and amount
Assessment Parameters
Urine Characteristics
- Color: Pale yellow to amber
- Clarity: Clear to slightly cloudy
- Odor: Mild, not foul
- Amount: 30-50 mL/hour minimum
Catheter Function
- Patency: Free-flowing drainage
- Position: Secure, no tension
- Balloon: Properly inflated
- Tubing: No kinks or obstructions
Patient Comfort
- Pain level: Minimal discomfort
- Urge to void: May persist initially
- Spasms: Bladder spasms may occur
- Mobility: Maintain as possible
When to Empty Drainage Bag
- Timing: Every 8 hours or when 1/2 to 2/3 full
- Technique: Use separate collection container for each patient
- Hygiene: Clean hands before and after, don’t touch drainage spout
- Documentation: Record amount, color, clarity, and odor
CAUTI Prevention Strategies
CAUTI: A Serious Healthcare Challenge
Statistics
- • 75% of UTIs are catheter-associated
- • 3-7% daily infection risk increase
- • $1,000+ additional cost per case
- • Increased length of stay
Risk Factors
- • Female gender
- • Advanced age
- • Prolonged catheterization
- • Immunocompromised state
Evidence-Based Prevention Bundle
Insertion Best Practices
- ✓ Sterile technique always
- ✓ Trained personnel only
- ✓ Smallest appropriate catheter
- ✓ Sterile, single-use lubricant
- ✓ Proper hand hygiene
Maintenance Excellence
- ✓ Maintain closed system
- ✓ Keep bag below bladder
- ✓ Secure catheter properly
- ✓ Empty bag regularly
- ✓ Daily necessity assessment
Daily CAUTI Prevention Checklist
Morning Assessment
- ☐ Is catheter still needed?
- ☐ Any signs of infection?
- ☐ System integrity intact?
- ☐ Proper positioning?
Ongoing Care
- ☐ Perineal hygiene completed
- ☐ Catheter cleaned
- ☐ Bag emptied appropriately
- ☐ Output documented
End of Shift
- ☐ Removal criteria met?
- ☐ Patient education provided
- ☐ Family involved in care
- ☐ Documentation complete
Memory Aid: “PREVENT” CAUTI
- Position bag below bladder
- Remove catheter ASAP
- Empty bag regularly
- Verify necessity daily
- Ensure closed system
- No routine irrigation
- Training for all staff
Complications and Management
Catheter-Associated Urinary Tract Infection (CAUTI)
Signs and Symptoms
- • Fever >38°C (100.4°F)
- • Suprapubic tenderness
- • Cloudy, foul-smelling urine
- • Increased urgency/frequency
- • Flank pain
- • Altered mental status (elderly)
Nursing Interventions
- • Obtain urine specimen for C&S
- • Assess for removal criteria
- • Monitor vital signs
- • Increase fluid intake if appropriate
- • Administer antibiotics as ordered
- • Document findings thoroughly
Catheter Obstruction
Causes
- • Blood clots
- • Sediment/debris
- • Kinking of tubing
- • Encrustation
- • Balloon malposition
Management
- • Check for kinks in tubing
- • Ensure proper positioning
- • Gentle milking of tubing
- • Irrigation if ordered
- • Consider catheter replacement
Urethral Trauma
Prevention
- • Never force catheter insertion
- • Use appropriate lubrication
- • Proper catheter size selection
- • Gentle insertion technique
- • Secure catheter properly
Signs of Trauma
- • Bleeding from urethra
- • Severe pain during insertion
- • Inability to advance catheter
- • Hematuria
- • Swelling around meatus
Bladder Spasms
Contributing Factors
- • Large catheter balloon
- • Catheter irritation
- • Bladder infection
- • Anxiety/stress
- • Constipation
Management Strategies
- • Antispasmodic medications
- • Proper catheter securing
- • Patient education/reassurance
- • Bladder training if appropriate
- • Address underlying causes
When to Notify Healthcare Provider
- Immediate notification: No urine output for 2 hours, gross hematuria, severe pain
- Within 1 hour: Signs of infection, catheter displacement, system compromise
- Next routine contact: Decreased output, minor complications, patient concerns
Patient and Family Education
Home Care Instructions
- Daily hygiene: Clean catheter and surrounding area with soap and water
- Bag management: Keep below bladder level, empty regularly
- Fluid intake: Maintain adequate hydration unless restricted
- Activity: Resume normal activities as tolerated
- Monitoring: Watch for signs of infection or complications
When to Seek Help
- Emergency: No urine output, severe pain, fever >101°F
- Call healthcare provider: Cloudy/foul-smelling urine, burning sensation
- Urgent care: Catheter falls out, bag leaking, persistent bleeding
- Routine follow-up: Scheduled appointments, catheter changes
Teaching Points by Development Stage
Pediatric Considerations
- • Age-appropriate explanations
- • Involve parents/caregivers
- • Use play therapy techniques
- • Address body image concerns
- • Maintain dignity and privacy
Adult Education
- • Detailed care instructions
- • Return demonstration
- • Written materials provided
- • Support resources
- • Encourage questions
Geriatric Considerations
- • Cognitive assessment
- • Simplified instructions
- • Caregiver involvement
- • Mobility adaptations
- • Frequent reinforcement
Nursing Implementation in Clinical Practice
Comprehensive Nursing Assessment
Physical Assessment
- • Bladder distension palpation
- • Urethral meatus inspection
- • Catheter positioning check
- • Drainage system evaluation
- • Skin integrity assessment
Functional Assessment
- • Cognitive status evaluation
- • Mobility and self-care ability
- • Pain assessment (0-10 scale)
- • Quality of life impact
- • Psychosocial adjustment
Nursing Diagnosis and Care Planning
Risk for Infection
Related to: Invasive procedure, compromised urinary tract
Interventions: Maintain sterile technique, monitor for signs of infection, implement CAUTI prevention bundle
Impaired Urinary Elimination
Related to: Urinary retention, neurogenic bladder, obstruction
Interventions: Monitor I&O, assess catheter patency, plan for removal when appropriate
Disturbed Body Image
Related to: Presence of catheter, altered elimination pattern
Interventions: Provide emotional support, encourage verbalization, maintain dignity
Quality Indicators and Outcomes
Process Measures
- • Appropriate catheter utilization
- • Adherence to insertion protocol
- • Daily necessity assessment
- • Maintenance bundle compliance
Outcome Measures
- • CAUTI rate reduction
- • Catheter-days minimized
- • Patient satisfaction scores
- • Complication rates
Interprofessional Collaboration
Physician/NP
- • Order verification
- • Complication management
- • Removal criteria
Infection Control
- • Surveillance data
- • Policy development
- • Staff education
Patient/Family
- • Education and support
- • Shared decision-making
- • Discharge planning
Documentation and Legal Considerations
Essential Documentation Elements
- Insertion: Date, time, size, type, difficulty level, patient response
- Daily care: Catheter assessment, perineal care, system integrity
- Output: Amount, color, clarity, odor, specific gravity
- Complications: Signs, symptoms, interventions, provider notification
- Education: Patient/family teaching provided and understood
Legal and Ethical Considerations
- Informed consent: Patient understanding of risks and benefits
- Privacy: Maintain dignity during procedures and care
- Competency: Ensure trained personnel perform procedures
- Advocacy: Question unnecessary catheter use
- Standards: Follow evidence-based guidelines
Sample Documentation Templates
Insertion Note
“14 Fr Foley catheter inserted per sterile technique for urinary retention. 10 mL sterile water used to inflate balloon. Clear yellow urine returned immediately. Catheter secured to right thigh with StatLock. Patient tolerated procedure well with minimal discomfort. Drainage bag positioned below bladder level.”
Daily Assessment
“Foley catheter patent and draining clear yellow urine. Catheter secured appropriately, no signs of infection at insertion site. Perineal care completed. Drainage bag emptied of 350 mL urine. Patient denies pain or discomfort. Necessity for continued catheterization discussed with provider.”
Key Takeaways and Summary
Critical Success Factors
- 1. Use catheters only when medically necessary
- 2. Maintain sterile technique during insertion
- 3. Implement comprehensive CAUTI prevention strategies
- 4. Assess daily for removal criteria
- 5. Educate patients and families thoroughly
- 6. Document all care comprehensively
Final Memory Aid: “CATHETER”
- Clean technique always
- Assess necessity daily
- Teaching patients/families
- Hygiene maintenance
- Early removal when possible
- Trouble signs recognition
- Evidence-based practice
- Remove ASAP safely
Excellence in Catheter Care
Excellence in indwelling urinary catheter care requires a commitment to evidence-based practice, continuous education, and patient-centered care. By implementing comprehensive prevention strategies, maintaining meticulous technique, and advocating for appropriate catheter use, nurses play a crucial role in preventing complications and optimizing patient outcomes. Remember that every catheter-day avoided is a victory in infection prevention and patient safety.
References and Further Reading
- 1. Centers for Disease Control and Prevention. (2024). Guidelines for Prevention of Catheter-Associated Urinary Tract Infections. CDC Guidelines
- 2. American Nurses Association. (2023). CAUTI Prevention Tool. ANA Resources
- 3. Association for Professionals in Infection Control and Epidemiology. (2023). CAUTI Prevention Guidelines. APIC Guidelines
- 4. Healthcare Infection Control Practices Advisory Committee. (2023). Guideline for Prevention of Catheter-Associated Urinary Tract Infections. HICPAC Guidelines
- 5. Society of Urologic Nurses and Associates. (2023). Clinical Practice Guidelines for Urinary Catheter Management. SUNA Guidelines
- 6. American Association of Family Physicians. (2023). Urinary Catheter Management. AAFP Guidelines
