Nursing Care Plan for Glaucoma
Notes for Nursing Students
What is Glaucoma?
Glaucoma is a group of eye conditions that damage the optic nerve, often due to abnormally high pressure in the eye (intraocular pressure or IOP). This increased pressure results from inadequate drainage of aqueous humor from the anterior chamber of the eye. The damage to the optic nerve leads to progressive, irreversible vision loss and can result in permanent blindness if untreated.
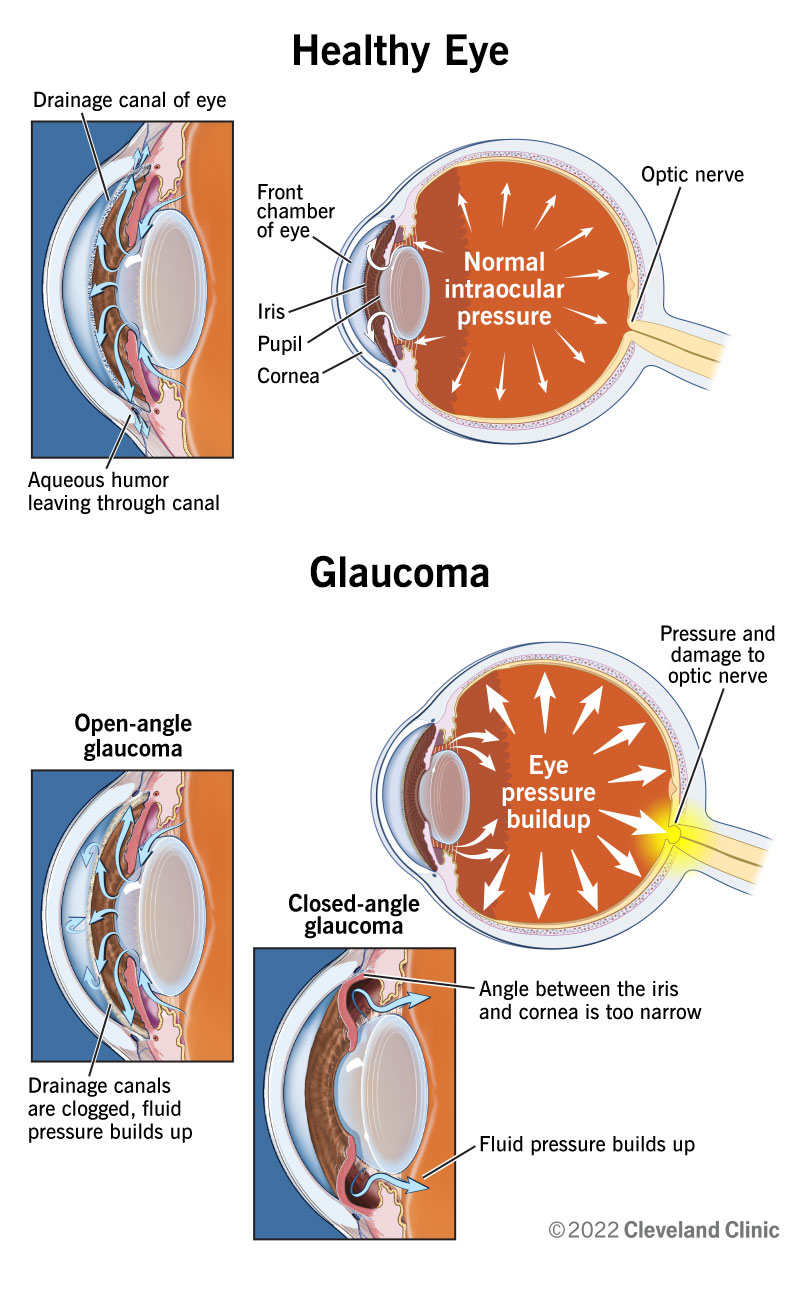
Illustration of glaucoma’s effect on the eye
Pathophysiology of Glaucoma
The primary pathophysiological mechanism in glaucoma is elevated intraocular pressure (IOP) that causes mechanical stress on the lamina cribrosa of the optic nerve, leading to optic nerve damage. This results in the loss of retinal ganglion cells and their axons, which transmit visual information to the brain.
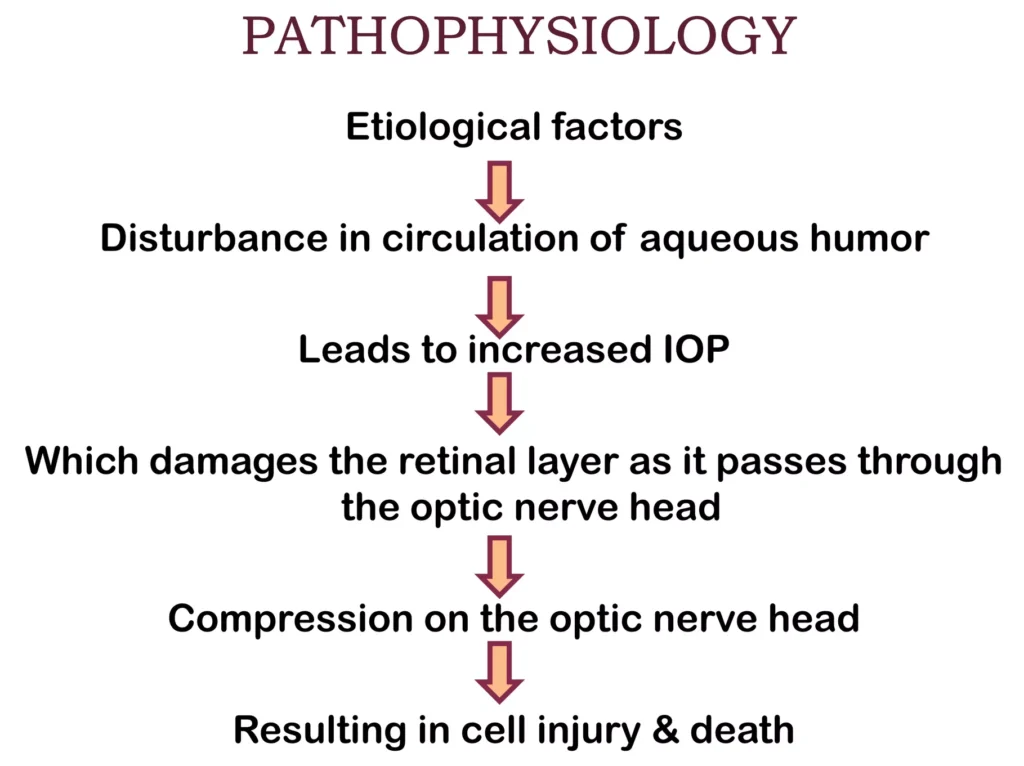
Pathophysiological process of glaucoma
- Obstruction of aqueous humor outflow
- Increased intraocular pressure
- Mechanical pressure on optic nerve
- Optic nerve damage and atrophy
- Progressive loss of visual field
- Eventual blindness if untreated
Types of Glaucoma
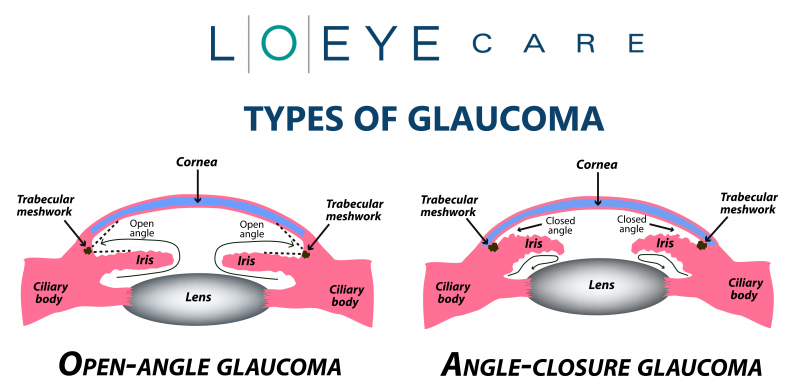
Comparison of different glaucoma types
1. Open-Angle Glaucoma (Primary Open-Angle Glaucoma)
- Most common type (90% of all cases)
- Develops slowly and painlessly
- Associated with diabetes and myopia
- Can develop in both eyes simultaneously
- Characterized by gradual loss of peripheral vision
2. Angle-Closure Glaucoma (Narrow-Angle Glaucoma)
- Less common but more severe form
- Can be acute (medical emergency) or chronic
- May be associated with eye trauma, inflammatory processes
- Characterized by sudden, excruciating pain, blurred vision, and ocular redness
- May lead to sudden blindness if not treated promptly
Open-angle glaucoma:
- Open drainage angle
- Painless
- Ensues gradually
- No acute symptoms
Closed-angle glaucoma:
- Closed drainage angle
- Lots of pain (acute form)
- Ocular redness
- Sudden onset
- Emergency treatment needed
Nursing Assessment for Glaucoma
Subjective Data (Symptoms)
- Gradual loss of peripheral vision
- Blurred or hazy vision
- Halos around lights
- Eye pain or pressure (especially in angle-closure glaucoma)
- Headaches
- Eye strain
- Nausea and vomiting (in acute angle-closure attacks)
Objective Data (Signs)
- Increased intraocular pressure (>21 mmHg)
- Optic nerve damage on ophthalmoscopy
- Visual field defects
- Redness of the eye (in acute glaucoma)
- Fixed, mid-dilated pupil (in angle-closure glaucoma)
- Cloudy cornea (in advanced cases)
- G – Gauge intraocular pressure (normal: 10-21 mmHg)
- L – Look for visual field defects
- A – Assess optic nerve for cupping and pallor
- U – Understand risk factors (family history, age, race)
- C – Check for corneal changes
- O – Observe pupillary reactions
- M – Monitor for pain, headaches, nausea
- A – Assess peripheral vision
Table of Contents: Nursing Diagnoses
- Impaired Visual Function related to increased intraocular pressure and optic nerve damage
- Risk for Injury related to impaired peripheral vision and potential falls
- Deficient Knowledge related to glaucoma and its management
- Anxiety related to diagnosis of glaucoma and potential vision loss
- Risk for Ineffective Management of Therapeutic Regimen related to complexity of medication schedule
- Chronic Pain related to increased intraocular pressure
- Disturbed Body Image related to vision loss and use of visual aids
- Risk for Social Isolation related to visual impairment
1. Impaired Visual Function
Related to: Increased intraocular pressure and optic nerve damage
Defining Characteristics:
- Decreased visual acuity
- Loss of peripheral vision
- Progressive visual field defects
- Difficulty seeing in low-light conditions
- Reports of halos around lights
Expected Outcomes:
- Patient will maintain current visual field/acuity without further loss
- Patient will adapt to visual changes by using suggested compensatory techniques
- Patient will demonstrate proper use of prescribed medications to control intraocular pressure
Nursing Interventions:
1. Monitor intraocular pressure and assess for changes in visual function
Regular monitoring helps detect changes that require immediate intervention and prevents further vision loss.
2. Administer prescribed eye medications as scheduled (e.g., prostaglandin analogs, beta-blockers, alpha-adrenergic agonists)
Direct-acting topical medications help lower intraocular pressure by either reducing aqueous humor production or increasing its outflow.
3. Assist with environmental modifications to accommodate visual deficits
Reducing clutter, improving lighting, arranging furniture out of travel paths, and using high-contrast colors helps patients navigate their environment safely despite visual impairment.
4. Teach patient techniques to optimize remaining vision
Techniques such as turning the head to view objects in the peripheral field and using proper lighting improve the patient’s ability to function with visual deficits.
5. Prepare patient for surgical interventions if indicated
Surgical procedures like laser trabeculoplasty or iridectomy may be necessary to create alternative drainage pathways for aqueous humor when medical management is insufficient.
2. Risk for Injury
Related to: Impaired peripheral vision and potential falls
Risk Factors:
- Decreased visual field
- Impaired depth perception
- Reduced contrast sensitivity
- Poor adaptation to changes in light intensity
- Compromised mobility due to visual deficits
Expected Outcomes:
- Patient will remain free from injury
- Patient will implement safety measures in the home environment
- Patient will demonstrate safe mobility techniques
Nursing Interventions:
1. Conduct a comprehensive home safety assessment
Identifying potential hazards allows for proactive modifications to prevent falls and injuries.
2. Educate on environmental modifications
Improvements such as removing throw rugs, installing handrails, using nightlights, and marking steps with bright tape reduce fall risk.
3. Teach techniques for safe ambulation
Techniques such as scanning the environment, using proper lighting, and utilizing adaptive devices help compensate for visual field defects.
4. Encourage use of assistive devices as appropriate
Walking aids, talking watches, large-print materials, and other assistive devices promote independence and safety.
5. Refer to occupational therapy for adaptive techniques
Occupational therapists can provide specialized training for daily activities and recommend specific modifications to enhance safety and independence.
3. Deficient Knowledge
Related to: Lack of information about glaucoma and its management
Defining Characteristics:
- Verbalization of misconceptions about glaucoma
- Incorrect use of prescribed medications
- Questions about condition and treatment
- Lack of adherence to follow-up appointments
- Expression of uncertainty about managing the condition
Expected Outcomes:
- Patient will verbalize understanding of glaucoma, its progression, and treatment
- Patient will demonstrate correct administration of eye medications
- Patient will identify signs/symptoms requiring medical attention
- Patient will verbalize the importance of regular follow-up
Nursing Interventions:
1. Assess patient’s current knowledge and learning needs
Understanding the patient’s baseline knowledge helps tailor education to address specific gaps and misconceptions.
2. Provide education about glaucoma pathophysiology, progression, and treatment options
Clear, accurate information helps patients understand the chronic nature of glaucoma and the importance of ongoing management.
3. Demonstrate proper technique for eye drop administration
Correct administration ensures therapeutic effectiveness and minimizes side effects.
Key Eye Drop Administration Steps:
- Wash hands thoroughly
- Tilt head back or lie down
- Pull lower eyelid down to form a pocket
- Hold dropper above eye (avoid touching the eye)
- Instill prescribed number of drops
- Close eye for 1-2 minutes (don’t blink excessively)
- Apply gentle pressure to inner corner of eye for 1 minute
- Wait 5 minutes between different eye medications
4. Explain the importance of medication adherence and regular follow-up
Consistent adherence to treatment and monitoring helps prevent vision loss and allows for timely adjustment of treatment when needed.
5. Provide written materials and resources about glaucoma
Written information reinforces verbal teaching and serves as a reference after the patient leaves the healthcare setting.
4. Anxiety
Related to: Diagnosis of glaucoma and potential vision loss
Defining Characteristics:
- Expressed concerns about potential blindness
- Increased tension, restlessness, or nervousness
- Focus on worst-case scenarios
- Difficulty concentrating
- Reports of insomnia or sleep disturbances
Expected Outcomes:
- Patient will report reduced anxiety to a manageable level
- Patient will verbalize adaptive coping strategies
- Patient will demonstrate relaxation techniques when feeling anxious
Nursing Interventions:
1. Assess level of anxiety and identify specific concerns
Understanding the specific fears and concerns allows for targeted interventions and reassurance.
2. Provide accurate, honest information about glaucoma and treatment outcomes
Factual information about the effectiveness of treatment in preventing further vision loss can alleviate catastrophic thinking.
3. Create a calm and supportive environment
A quiet environment with soft lighting reduces stimulation that can exacerbate anxiety.
4. Teach relaxation techniques (deep breathing, progressive muscle relaxation, guided imagery)
These techniques activate the parasympathetic nervous system, countering the physiological effects of anxiety.
5. Refer to support groups and counseling services
Connecting with others who share similar experiences and concerns provides emotional support and practical coping strategies.
5. Risk for Ineffective Management of Therapeutic Regimen
Related to: Complexity of medication schedule and chronic nature of glaucoma
Risk Factors:
- Multiple medications with different administration schedules
- Lack of symptoms in early glaucoma (reduced motivation)
- Side effects from medications
- Visual or cognitive impairment affecting ability to administer medications
- Financial constraints affecting access to medications
Expected Outcomes:
- Patient will demonstrate adherence to prescribed medication regimen
- Patient will maintain a medication schedule/log
- Patient will attend scheduled follow-up appointments
- Patient will report addressing barriers to treatment adherence
Nursing Interventions:
1. Assess barriers to medication adherence
Identifying specific obstacles allows for targeted interventions to improve compliance.
2. Develop a simplified medication schedule
A clear, easy-to-follow schedule linked to daily activities improves consistency in medication administration.
3. Recommend medication aids (timers, pill organizers, smartphone apps)
These tools provide reminders and help track medication administration.
4. Educate about medication side effects and their management
Understanding potential side effects and how to manage them increases willingness to continue treatment.
5. Connect patients with financial assistance programs if needed
Addressing financial barriers ensures continuous access to necessary medications.
6. Chronic Pain
Related to: Increased intraocular pressure (especially in angle-closure glaucoma)
Defining Characteristics:
- Reports of eye pain or pressure
- Associated headaches
- Facial expressions of discomfort
- Altered sleep patterns
- Protective behavior of affected eye
Expected Outcomes:
- Patient will report decreased eye pain and discomfort
- Patient will demonstrate effective pain management strategies
- Patient will maintain normal activities despite occasional discomfort
Nursing Interventions:
1. Assess pain characteristics (location, intensity, duration, aggravating/relieving factors)
Detailed pain assessment helps determine appropriate interventions and track effectiveness of treatment.
2. Administer prescribed pain medications and eye drops
Medication reduces intraocular pressure, which is the underlying cause of pain.
3. Apply cool compresses to closed eyes as appropriate
Cool compresses can reduce discomfort and inflammation in some cases.
4. Teach stress reduction techniques
Stress can exacerbate pain perception; relaxation techniques can help modulate pain response.
5. Modify environment to reduce eye strain (proper lighting, reduced glare)
Environmental modifications can reduce factors that aggravate ocular discomfort.
7. Disturbed Body Image
Related to: Vision loss and need for visual aids
Defining Characteristics:
- Verbalization of negative feelings about visual impairment
- Reluctance to use visual aids in public
- Withdrawal from social activities
- Expressed concerns about others’ perceptions
- Avoidance of discussing visual limitations
Expected Outcomes:
- Patient will express acceptance of visual changes
- Patient will use assistive devices as needed without embarrassment
- Patient will maintain social interactions and activities
Nursing Interventions:
1. Encourage expression of feelings about visual changes
Acknowledging and processing feelings is an essential step toward acceptance.
2. Provide information about discreet visual aids
Modern assistive devices are often designed to be less conspicuous, which may increase willingness to use them.
3. Connect with peer support groups
Interacting with others who have successfully adjusted to visual impairment provides both emotional support and practical coping strategies.
4. Focus on abilities rather than limitations
Emphasizing what the patient can still do helps maintain a positive self-concept.
5. Encourage gradual reintegration into social activities
Successful social interactions build confidence and reinforce adaptive coping.
8. Risk for Social Isolation
Related to: Visual impairment affecting mobility and social interaction
Risk Factors:
- Difficulty with transportation due to vision loss
- Challenges in recognizing faces or social cues
- Decreased confidence in navigating unfamiliar environments
- Embarrassment about visual limitations
- Fear of being a burden to others
Expected Outcomes:
- Patient will maintain social connections and relationships
- Patient will participate in meaningful social activities
- Patient will utilize resources to overcome barriers to social participation
Nursing Interventions:
1. Assess current social support system and level of engagement
Understanding the patient’s baseline social network helps identify resources and areas needing support.
2. Provide information about transportation services for visually impaired
Access to transportation is crucial for maintaining independence and social connections.
3. Connect with local vision support organizations
These organizations offer social activities designed for people with visual impairments and provide valuable resources.
4. Teach communication strategies for social situations
Simple techniques, such as informing others about visual limitations and asking for specific assistance, can improve social interactions.
5. Encourage use of technology for social connection
Adaptive technology and accessible social media platforms can help maintain relationships when in-person interaction is challenging.
Pharmacological Management of Glaucoma

Visual comparison of open vs. closed-angle glaucoma
| Drug Class | Mechanism of Action | Examples | Nursing Considerations |
|---|---|---|---|
| Prostaglandin Analogs | Increase outflow of aqueous humor through the uveoscleral pathway | Latanoprost (Xalatan), Travoprost (Travatan), Bimatoprost (Lumigan) |
|
| Beta-Blockers | Decrease production of aqueous humor | Timolol (Timoptic), Betaxolol (Betoptic), Levobunolol (Betagan) |
|
| Alpha-Adrenergic Agonists | Decrease production and increase outflow of aqueous humor | Brimonidine (Alphagan), Apraclonidine (Iopidine) |
|
| Carbonic Anhydrase Inhibitors | Decrease production of aqueous humor | Dorzolamide (Trusopt), Brinzolamide (Azopt), Acetazolamide (Diamox) – oral |
|
| Cholinergic Agents (Miotics) | Increase outflow of aqueous humor by constricting the pupil | Pilocarpine, Carbachol |
|
| Combination Products | Combined mechanisms for enhanced effect | Cosopt (Dorzolamide/Timolol), Combigan (Brimonidine/Timolol) |
|
- D – Dorzolamide (Carbonic anhydrase inhibitor)
- R – Rho kinase inhibitors (Netarsudil)
- O – Ocular hypotensive agents (General category)
- P – Prostaglandin analogs (Latanoprost, Travoprost)
- T – Timolol (Beta-blocker)
- H – Hyperosmotic agents (for acute angle-closure)
- E – Epinephrine derivatives (Alpha agonists)
- P – Pilocarpine (Cholinergic/Miotic)
- R – Reduced aqueous production (goal of many medications)
- E – Enhanced outflow (goal of many medications)
- S – Surgical options when medications fail
- S – Side effects (always consider)
- U – Use as prescribed (stress adherence)
- R – Regular monitoring (essential)
- E – Educate patients thoroughly
Patient Education Essentials
1. Understanding Glaucoma
- Explain that glaucoma damages the optic nerve, usually due to increased eye pressure
- Emphasize that vision lost cannot be regained, making prevention crucial
- Clarify that treatment aims to prevent further vision loss, not restore lost vision
2. Medication Management
- Teach proper eye drop instillation technique
- Stress the importance of taking medications exactly as prescribed
- Explain the need for continued medication even when feeling well
- Advise waiting 5 minutes between different eye medications
3. Lifestyle Modifications
- Recommend moderate exercise (may help lower intraocular pressure)
- Advise against activities that increase intraocular pressure:
- Heavy lifting
- Straining during bowel movements
- Positions with head below heart level
- Encourage adequate fluid intake to prevent dehydration
- Suggest smoking cessation (smoking can increase intraocular pressure)
4. Follow-Up Care
- Stress importance of regular eye exams and intraocular pressure checks
- Encourage adherence to follow-up appointments even when asymptomatic
- Explain the need for lifelong monitoring
5. When to Seek Medical Attention
- Sudden eye pain or redness
- Nausea or vomiting with eye pain
- Sudden vision changes or loss
- Halos around lights
- Persistent headache
6. Family Screening
- Encourage first-degree relatives to get regular glaucoma screenings
- Emphasize higher risk in family members, particularly African Americans
Glaucoma Management Flowchart

Flowchart for glaucoma care process
Latest Advances in Glaucoma Treatment (2024)
1. Sustained-Release Medication Delivery Systems
New implantable devices like Glaukos’ iDose TR can provide continuous drug therapy inside the eye for up to three years, improving compliance and reducing the burden of daily eye drops.
2. Minimally Invasive Glaucoma Surgery (MIGS)
These procedures offer lower risk alternatives to traditional glaucoma surgery, with shorter recovery times and fewer complications.
3. Remote Monitoring Platforms
New technologies allow patients to monitor intraocular pressure at home, with results transmitted to healthcare providers for continuous management.
4. Stem Cell Therapy
Experimental treatments using healthy retinal ganglion cells to replace damaged ones show promise for potentially restoring visual function.
5. Neuroprotection
Research focuses on medications that can protect the optic nerve from damage, even in the presence of elevated intraocular pressure.
Preventive Measures for Glaucoma

Preventive strategies for glaucoma management
- Regular Eye Exams – Especially important for those over 40 or with risk factors
- Early Detection – Regular intraocular pressure checks and optic nerve examinations
- Medication Adherence – Following prescribed treatment regimens consistently
- Eye Protection – Preventing eye injuries that can lead to secondary glaucoma
- Healthy Lifestyle – Regular exercise, smoking cessation, and maintaining a healthy weight
- Family Awareness – Encouraging family members to get regular screenings
References
- Nurseslabs. (2024). Glaucoma Nursing Care Plans. https://nurseslabs.com/glaucoma-nursing-care-plans/
- Made For Medical. (2023). Nursing Care Plan for Glaucoma. https://www.madeformedical.com/nursing-care-plan-for-glaucoma/
- RNpedia. (2024). Glaucoma Nursing Care Plan & Management. https://www.rnpedia.com/nursing-notes/medical-surgical-nursing-notes/glaucoma-nursing-management/
- Glaucoma Research Foundation. (2024). Exploring The Latest Breakthroughs In Glaucoma Research. https://glaucoma.org/articles/exploring-the-latest-breakthroughs-in-glaucoma-research
- Mayo Clinic. (2024). Glaucoma – Diagnosis and treatment. https://www.mayoclinic.org/diseases-conditions/glaucoma/diagnosis-treatment/drc-20372846
- BrightFocus. (2024). Glaucoma Treatments in 2024. https://www.brightfocus.org/resource/glaucoma-treatments-in-2024/
- National Center for Biotechnology Information. (2024). Glaucoma (Nursing) – StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK568748/
