Comprehensive Nursing Care Plan for Portal Hypertension
Evidence-based nursing interventions for effective management of portal hypertension
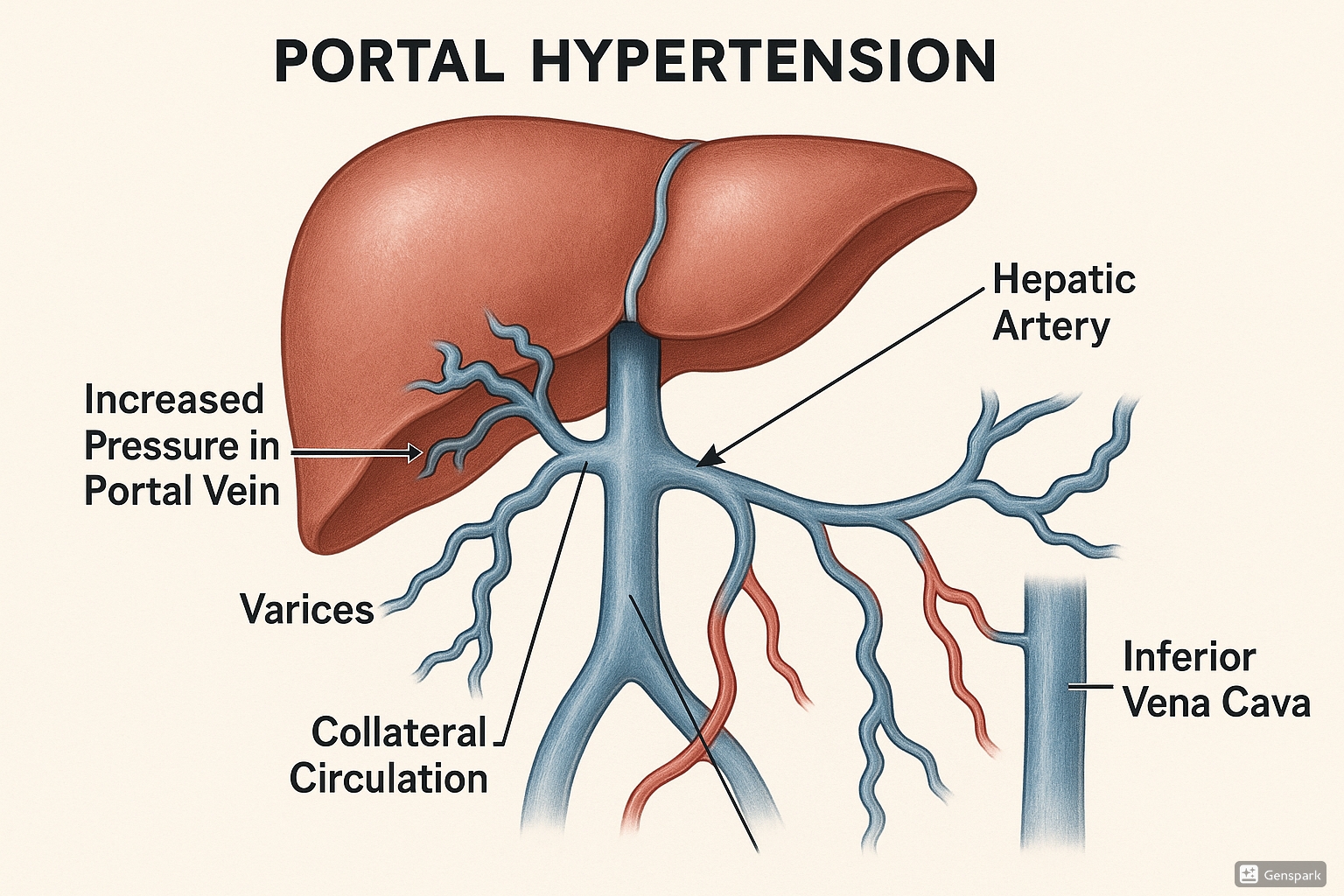
Portal Hypertension: Illustration showing increased pressure in the portal venous system with development of collateral circulation and varices
Table of Contents
Introduction to Portal Hypertension
Portal hypertension is defined as elevated pressure in the portal venous system, typically exceeding 10 mmHg. It is characterized by increased resistance to blood flow through the portal venous system, most commonly due to cirrhosis and other liver diseases. The increased pressure leads to the development of collateral circulation and potentially life-threatening complications such as esophageal varices, ascites, and hepatic encephalopathy.
Key Facts About Portal Hypertension
- Portal hypertension is most commonly caused by cirrhosis (70-90% of cases)
- Normal portal pressure: 5-10 mmHg; Portal hypertension: >10-12 mmHg
- Up to 90% of cirrhosis patients develop portal hypertension
- Major complications include variceal bleeding, ascites, and hepatic encephalopathy
- Portal hypertension is the most common cause of hospitalization and death in cirrhosis patients
Pathophysiology of Portal Hypertension
The pathophysiology of portal hypertension involves several mechanisms:
Mechanism of Development
Portal hypertension develops when there is increased resistance to blood flow through the portal venous system. This resistance can be:
- Prehepatic: Obstruction of the portal vein before it reaches the liver (e.g., portal vein thrombosis)
- Intrahepatic: Occurs within the liver (most common – caused by cirrhosis)
- Posthepatic: Obstruction of venous outflow from the liver (e.g., Budd-Chiari syndrome)
Hemodynamic Changes
As portal pressure rises, blood is redirected through collateral vessels to bypass the liver. These collateral vessels develop in locations such as:
- Gastroesophageal junction: Leading to esophageal and gastric varices
- Rectum: Causing hemorrhoids
- Anterior abdominal wall: Resulting in caput medusae (dilated periumbilical veins)
- Retroperitoneum: Creating various collateral pathways
The formation of these collateral vessels allows blood to bypass the liver and return to the systemic circulation, but this also means that:
- Toxins normally filtered by the liver enter systemic circulation (contributing to hepatic encephalopathy)
- Thin-walled varices are prone to rupture and bleeding
- Decreased effective circulating volume triggers sodium and water retention leading to ascites
Assessment of Portal Hypertension
Clinical Manifestations
The primary clinical manifestations of portal hypertension include:
| Manifestation | Description |
|---|---|
| Esophageal/Gastric Varices | Dilated, tortuous veins in the esophagus and stomach that can rupture and cause severe hemorrhage |
| Ascites | Accumulation of fluid in the peritoneal cavity causing abdominal distension and increased abdominal girth |
| Splenomegaly | Enlargement of the spleen due to congestion |
| Caput Medusae | Dilated periumbilical veins radiating from the umbilicus |
| Portal Hypertensive Gastropathy | Congestion and mucosal changes in the stomach that may cause chronic bleeding |
| Hepatic Encephalopathy | Neuropsychiatric symptoms resulting from liver’s inability to remove toxins from the blood |
| Hepatorenal Syndrome | Progressive renal failure in patients with advanced liver disease |
Physical Assessment Findings
- Abdominal distention and shifting dullness (indicating ascites)
- Palpable spleen (splenomegaly)
- Abdominal bruit (abnormal sound heard on auscultation)
- Spider angiomas on the skin
- Palmar erythema (reddening of the palms)
- Jaundice (yellowing of skin and sclera)
- Lower extremity edema
- Mental status changes (hepatic encephalopathy)
Diagnostic Tests
- Hepatic Venous Pressure Gradient (HVPG): Gold standard for measuring portal pressure
- Ultrasound with Doppler: Evaluates blood flow in portal system and identifies collateral vessels
- Upper Endoscopy: Identifies esophageal and gastric varices
- CT or MRI: Visualizes liver, portal vein, and collateral circulation
- Laboratory Tests: Liver function tests, coagulation studies, CBC, electrolytes
Nursing Diagnoses for Portal Hypertension
The following nursing diagnoses are commonly applicable to patients with portal hypertension. Each diagnosis includes specific interventions, rationales, and expected outcomes to guide comprehensive nursing care.
1. Risk for Bleeding related to portal hypertension and esophageal varices
- Patient will remain free from episodes of variceal bleeding
- Patient will demonstrate understanding of bleeding precautions
- Patient will recognize early signs of bleeding and seek prompt medical attention
Nursing Interventions for Risk for Bleeding:
1. Assess for and document signs of bleeding: hematemesis, melena, hematochezia, epistaxis, easy bruising, and petechiae.
Rationale: Early detection of bleeding enables prompt intervention. Gastrointestinal bleeding from varices can rapidly become life-threatening with mortality rates of 20-30% per episode.
2. Monitor vital signs frequently, noting tachycardia, hypotension, tachypnea, and decreased oxygen saturation.
Rationale: Changes in vital signs can indicate active bleeding before visible signs appear. Tachycardia and hypotension are early signs of hypovolemia due to blood loss.
3. Check laboratory values: hemoglobin, hematocrit, platelet count, PT/INR, and PTT.
Rationale: Decreasing hemoglobin and hematocrit levels indicate blood loss. Abnormal coagulation studies and thrombocytopenia indicate increased bleeding risk.
4. Administer prescribed medications such as beta-blockers (e.g., propranolol, nadolol) as ordered.
Rationale: Beta-blockers reduce portal pressure by decreasing cardiac output and causing splanchnic vasoconstriction, reducing the risk of first variceal bleeding by approximately 45%.
5. Use small-gauge needles for injections and apply prolonged pressure (3-5 minutes) to injection sites.
Rationale: Smaller gauge needles cause less tissue trauma and prolonged pressure allows for proper clot formation, reducing risk of hematoma formation.
6. Instruct patient to use soft toothbrush, electric razor, and avoid straining during defecation.
Rationale: These measures help prevent trauma to mucous membranes and increased portal pressure, which could trigger bleeding. Straining increases intra-abdominal pressure which is transmitted to the portal system.
7. Keep emergency equipment readily available: large-bore IV access supplies, airway equipment, and Sengstaken-Blakemore tube.
Rationale: Quick access to emergency equipment can improve outcomes when managing acute variceal bleeding, which has a high mortality rate if not promptly addressed.
8. Prepare for and assist with endoscopic procedures such as band ligation or sclerotherapy as indicated.
Rationale: Endoscopic band ligation is the preferred first-line therapy for acute esophageal variceal bleeding, with a success rate of approximately 90% in controlling initial bleeding.
2. Excess Fluid Volume related to ascites formation, sodium retention, and decreased albumin production
- Ascites and abdominal distention
- Increased abdominal girth
- Peripheral edema
- Weight gain
- Shifting dullness on percussion
- Patient will demonstrate stable or decreasing abdominal girth
- Patient will maintain balanced fluid intake and output
- Patient will verbalize understanding of fluid and sodium restrictions
Nursing Interventions for Excess Fluid Volume:
1. Measure and record daily weight, abdominal girth, and intake and output.
Rationale: Provides objective data to evaluate fluid status and effectiveness of diuretic therapy. A 1 kg weight change represents approximately 1 liter of fluid.
2. Restrict sodium intake as prescribed (typically 2000 mg/day or less).
Rationale: Sodium restriction enhances the effectiveness of diuretics and helps prevent fluid retention. Sodium retention is a key pathophysiologic mechanism in ascites formation.
3. Administer diuretics as prescribed (spironolactone, furosemide) and monitor for effectiveness and side effects.
Rationale: Combination diuretic therapy with an aldosterone antagonist (spironolactone) and a loop diuretic (furosemide) is more effective than either agent alone in managing ascites.
4. Monitor serum electrolytes, BUN, and creatinine regularly.
Rationale: Diuretic therapy can cause electrolyte imbalances (particularly hyponatremia, hypokalemia) and may impair renal function, especially in patients at risk for hepatorenal syndrome.
5. Position patient with head elevated 30-45 degrees to reduce diaphragmatic pressure.
Rationale: Elevation helps reduce pressure on the diaphragm from ascites, improving ventilation and reducing dyspnea.
6. Assist with paracentesis as ordered and monitor for complications such as hypotension.
Rationale: Large-volume paracentesis (>5 liters) provides rapid relief of symptoms but may cause post-paracentesis circulatory dysfunction if not performed with albumin replacement (8g albumin per liter of ascites removed).
7. Apply elastic stockings and encourage elevation of extremities to reduce peripheral edema.
Rationale: Compression and elevation promote venous return and reduce peripheral edema by enhancing fluid reabsorption into the vascular space.
8. Administer albumin infusions as prescribed.
Rationale: Albumin increases plasma oncotic pressure, drawing fluid from interstitial spaces into the vascular compartment. It also improves response to diuretics and prevents complications of large-volume paracentesis.
3. Impaired Gas Exchange related to ascites causing diaphragmatic compression
- Dyspnea, especially when supine
- Orthopnea
- Tachypnea
- Decreased oxygen saturation
- Difficulty with deep breathing
- Patient will maintain oxygen saturation >92% on room air
- Patient will report decreased dyspnea
- Patient will demonstrate improved breathing patterns
Nursing Interventions for Impaired Gas Exchange:
1. Monitor respiratory rate, depth, and oxygen saturation every 4 hours and as needed.
Rationale: Regular monitoring allows for early detection of respiratory compromise and evaluation of the effectiveness of interventions.
2. Position patient in semi-Fowler’s or high Fowler’s position (30-60 degrees).
Rationale: Elevated head positioning decreases abdominal pressure on the diaphragm, maximizing lung expansion and ventilation.
3. Administer oxygen therapy as prescribed to maintain oxygen saturation >92%.
Rationale: Supplemental oxygen helps maintain adequate tissue oxygenation in patients with impaired gas exchange due to restrictive lung capacity.
4. Assist with management of ascites through diuretic therapy and paracentesis as ordered.
Rationale: Reducing ascites volume decreases pressure on the diaphragm, improving respiratory mechanics and gas exchange.
5. Teach and encourage deep breathing exercises and the use of incentive spirometer every 2 hours while awake.
Rationale: Deep breathing exercises promote alveolar expansion, prevent atelectasis, and improve ventilation when diaphragmatic movement is restricted.
6. Assist with thoracentesis if hepatic hydrothorax is present.
Rationale: Removing pleural fluid improves lung expansion and ventilation. Hepatic hydrothorax occurs in approximately 5-10% of patients with portal hypertension.
7. Monitor and document response to respiratory treatments and interventions.
Rationale: Documentation allows for evaluation of the effectiveness of interventions and guides adjustments to the treatment plan.
8. Provide frequent rest periods between activities to prevent oxygen desaturation.
Rationale: Activity increases oxygen demand, which may exceed supply in patients with impaired gas exchange. Rest periods help maintain oxygen balance.
4. Risk for Infection related to compromised immune function and ascites
- Patient will remain free of signs and symptoms of infection
- Patient will verbalize understanding of infection prevention measures
- Patient will demonstrate proper hand hygiene techniques
Nursing Interventions for Risk for Infection:
1. Monitor for signs and symptoms of infection, particularly spontaneous bacterial peritonitis (SBP): fever, abdominal pain, altered mental status, and worsening ascites.
Rationale: SBP occurs in 10-30% of cirrhotic patients with ascites and has a high mortality rate if not promptly diagnosed and treated. Early recognition is crucial for timely intervention.
2. Monitor white blood cell count, C-reactive protein, and ascitic fluid analysis (if obtained).
Rationale: An ascitic fluid neutrophil count >250 cells/mm³ is diagnostic of SBP. Laboratory values help identify infection and guide antibiotic selection.
3. Administer prophylactic antibiotics as prescribed (typically norfloxacin or trimethoprim-sulfamethoxazole).
Rationale: Antibiotic prophylaxis in high-risk patients (previous SBP, low ascitic protein, or advanced liver disease) reduces the risk of SBP by approximately 70-80%.
4. Use strict aseptic technique with procedures such as paracentesis and IV insertions.
Rationale: Aseptic technique minimizes the introduction of pathogens during invasive procedures, reducing the risk of iatrogenic infection.
5. Teach and reinforce hand hygiene to patient, family, and all healthcare workers.
Rationale: Hand hygiene is the most effective measure to prevent nosocomial infections. Patients with cirrhosis are particularly susceptible to healthcare-associated infections.
6. Ensure adequate nutrition to support immune function.
Rationale: Malnutrition is common in patients with portal hypertension and impairs immune function. Optimizing nutritional status can help reduce infection risk.
7. Rotate sites for injections and intravenous access to prevent tissue injury and infection.
Rationale: Site rotation prevents tissue damage and reduces the risk of localized infection, which can easily become systemic in immunocompromised patients.
8. Avoid unnecessary invasive procedures and catheterizations.
Rationale: Each invasive procedure increases the risk of infection. Use alternative approaches when possible to minimize the risk of iatrogenic infections.
5. Imbalanced Nutrition: Less than Body Requirements related to anorexia, nausea, and malabsorption
- Unintentional weight loss
- Muscle wasting
- Decreased appetite
- Low serum albumin and prealbumin
- Sarcopenia
- Patient will maintain or increase weight (excluding ascites)
- Patient will consume adequate calories and protein to meet metabolic needs
- Patient will demonstrate improved nutritional parameters (albumin, prealbumin)
Nursing Interventions for Imbalanced Nutrition:
1. Assess nutritional status using validated tools (e.g., Subjective Global Assessment, hand grip strength) and monitor dry weight (excluding ascites).
Rationale: Nutritional assessment tools provide objective data for evaluating nutritional status. Ascites can mask significant muscle and fat loss, making dry weight assessment essential.
2. Provide small, frequent meals (5-6 per day) with late evening snack.
Rationale: Small meals are better tolerated when ascites is present. A late evening snack reduces overnight fasting and improves protein balance by providing sustained energy.
3. Ensure adequate protein intake (1.2-1.5 g/kg/day) unless hepatic encephalopathy is present and not controlled by standard therapy.
Rationale: Protein restriction is generally not recommended as it worsens malnutrition. Only patients with severe, medication-refractory encephalopathy may need temporary protein modification.
4. Administer prescribed antiemetics before meals if nausea is present.
Rationale: Managing nausea improves oral intake and prevents further nutritional decline. Nausea is common due to portal hypertension causing gastric congestion.
5. Collaborate with dietitian for individualized meal planning that accommodates sodium restrictions while maximizing nutrient density.
Rationale: Dietitian expertise ensures that nutritional needs are met within necessary restrictions. Low-sodium diets can be unpalatable, requiring creative strategies to improve compliance and intake.
6. Provide oral nutritional supplements between meals, particularly those enriched with branched-chain amino acids (BCAAs) if indicated.
Rationale: High-calorie, high-protein supplements help meet nutritional requirements when oral intake is insufficient. BCAAs may be beneficial in patients with hepatic encephalopathy who require protein.
7. Monitor for and manage competing symptoms that affect intake (e.g., pain, fatigue).
Rationale: Symptom management improves comfort and ability to eat. Addressing pain, fatigue, and other symptoms can significantly improve nutritional intake.
8. Consult with healthcare provider regarding enteral nutrition if oral intake remains inadequate despite interventions.
Rationale: Enteral nutrition can prevent further nutritional decline when oral intake is insufficient. Nocturnal tube feeding can be particularly effective in preserving lean body mass.
6. Activity Intolerance related to fatigue, weakness, and respiratory compromise
- Dyspnea on exertion
- Fatigue
- Abnormal heart rate or blood pressure response to activity
- Exertional discomfort
- Difficulty performing activities of daily living
- Patient will demonstrate increased activity tolerance
- Patient will report decreased fatigue
- Patient will perform activities of daily living with minimal assistance
Nursing Interventions for Activity Intolerance:
1. Assess activity tolerance using standardized tools (e.g., 6-minute walk test) and monitor for signs of intolerance during activity.
Rationale: Objective assessment of activity tolerance provides a baseline for planning care and evaluating progress. Signs of intolerance include dyspnea, tachycardia, and dizziness.
2. Plan activities during periods of highest energy and schedule rest periods before and after activities.
Rationale: Energy conservation techniques help patients accomplish necessary activities while minimizing fatigue. Patients with portal hypertension often have limited energy reserves.
3. Implement a gradual, progressive activity plan in consultation with physical therapy.
Rationale: Gradual progression prevents overexertion while building endurance. Physical activity, when appropriately prescribed, can improve muscle mass and function in patients with cirrhosis.
4. Assist with management of ascites through diuretics and paracentesis to improve respiratory comfort during activity.
Rationale: Reducing ascites decreases diaphragmatic pressure, improving ventilation and reducing dyspnea during activity.
5. Monitor oxygen saturation before, during, and after activity; provide supplemental oxygen as needed.
Rationale: Oxygen saturation monitoring ensures adequate oxygenation during increased demand. Supplemental oxygen may be necessary to prevent desaturation during activity.
6. Prioritize activities based on patient’s goals and energy levels.
Rationale: Prioritization ensures that essential activities are accomplished without exhausting limited energy reserves.
7. Teach energy conservation techniques such as sitting while performing tasks when possible.
Rationale: Energy conservation techniques reduce oxygen demand and energy expenditure, allowing patients to accomplish more activities with available energy.
8. Address anemia and provide nutritional support to improve energy levels.
Rationale: Anemia contributes significantly to fatigue and activity intolerance. Improving nutritional status supports energy production and muscle function.
7. Impaired Skin Integrity related to edema, jaundice, and pruritus
- Skin excoriation from scratching
- Jaundice (yellowing of skin)
- Thin, fragile skin
- Edema
- Spider angiomas
- Patient will maintain skin integrity without breakdown
- Patient will demonstrate decreased scratching
- Patient will verbalize relief of pruritus
Nursing Interventions for Impaired Skin Integrity:
1. Assess skin condition daily, noting areas of breakdown, excoriation, and pressure risk.
Rationale: Regular assessment allows for early identification of skin problems and prompt intervention. Patients with portal hypertension have multiple risk factors for skin breakdown.
2. Administer prescribed antihistamines and bile acid sequestrants (e.g., cholestyramine) to manage pruritus.
Rationale: Cholestatic pruritus is caused by accumulated bile acids and other pruritogens. Antihistamines can provide symptomatic relief, while bile acid sequestrants address the underlying mechanism.
3. Apply emollients after bathing and throughout the day to maintain skin moisture.
Rationale: Well-hydrated skin is less prone to cracking and breakdown. Emollients create a barrier that reduces water loss and protects the skin.
4. Keep patient’s fingernails short and clean; consider cotton gloves at night if scratching is severe.
Rationale: Short nails minimize skin damage from scratching. Gloves provide a physical barrier against scratching during sleep when the patient has less conscious control.
5. Use mild, fragrance-free soaps and lukewarm water for bathing.
Rationale: Harsh soaps and hot water can exacerbate pruritus and dry skin. Gentle cleansing products minimize further skin irritation.
6. Reposition patient every 2 hours if mobility is limited.
Rationale: Regular repositioning reduces pressure and shear forces that can lead to pressure injuries, particularly in edematous areas where circulation is already compromised.
7. Use pressure-redistribution surfaces for patients with limited mobility.
Rationale: Specialty surfaces reduce pressure over bony prominences, decreasing the risk of pressure injuries in patients with impaired mobility and compromised skin.
8. Teach distraction techniques and applying cold compresses to manage pruritus.
Rationale: Distraction can temporarily reduce the perception of itch. Cold compresses can provide local relief by numbing nerve endings that transmit itch sensations.
8. Acute Pain related to liver enlargement, ascites, and abdominal distention
- Self-report of pain, typically in right upper quadrant or diffuse abdominal pain
- Guarding behavior
- Facial expressions of pain
- Changes in vital signs during acute pain
- Patient will report pain at acceptable level (≤3 on 0-10 scale)
- Patient will demonstrate improved comfort as evidenced by relaxed posture and facial expression
- Patient will use non-pharmacological pain management techniques effectively
Nursing Interventions for Acute Pain:
1. Assess pain comprehensively, including location, quality, intensity, and aggravating/relieving factors.
Rationale: Thorough assessment guides appropriate interventions and helps distinguish between pain due to portal hypertension and pain signaling complications (e.g., infection, bleeding).
2. Administer prescribed analgesics cautiously, avoiding NSAIDs and monitoring for adverse effects.
Rationale: NSAIDs can precipitate renal dysfunction and increase bleeding risk in patients with portal hypertension. Acetaminophen in reduced doses (≤2g/day) is generally safe for most patients with stable liver disease.
3. Position patient for comfort, typically with head elevated and knees flexed to reduce abdominal tension.
Rationale: Semi-Fowler’s position with knees flexed relaxes abdominal muscles and reduces tension on the distended abdomen, providing relief from discomfort.
4. Support abdomen with pillows or abdominal binder if ascites is causing discomfort.
Rationale: External support helps distribute the weight of ascites and reduces pulling on the abdominal wall and surrounding structures, decreasing discomfort.
5. Collaborate with healthcare provider regarding paracentesis if ascites is causing significant pain or respiratory distress.
Rationale: Large-volume paracentesis can provide rapid relief of pain and respiratory symptoms caused by tense ascites when medical management is insufficient.
6. Teach and assist with non-pharmacological pain management techniques such as relaxation breathing, guided imagery, and distraction.
Rationale: Non-pharmacological techniques can effectively supplement analgesics, reducing the need for higher medication doses and associated risks.
7. Apply cold or heat therapy as appropriate, with caution due to potential skin fragility.
Rationale: Cold therapy can reduce inflammation and dull pain, while heat therapy can relax muscles and improve blood flow. Careful application is necessary due to potential skin changes with liver disease.
8. Monitor and document pain levels and response to interventions regularly.
Rationale: Regular reassessment allows for evaluation of intervention effectiveness and guides adjustments to the pain management plan.
9. Deficient Knowledge related to unfamiliarity with condition, complications, and management
- Verbalized lack of understanding
- Inaccurate follow-through of instructions
- Inappropriate or exaggerated behaviors
- Multiple questions or statements revealing misunderstanding
- Patient will verbalize understanding of portal hypertension and its complications
- Patient will demonstrate proper self-care techniques
- Patient will identify warning signs requiring medical attention
Nursing Interventions for Deficient Knowledge:
1. Assess patient’s current knowledge, learning style, and readiness to learn.
Rationale: Assessment allows for tailored education that builds on existing knowledge and addresses specific knowledge gaps using appropriate teaching methods.
2. Provide education about portal hypertension, its causes, complications, and warning signs.
Rationale: Understanding the condition and its potential complications empowers patients to participate in self-care and recognize when to seek medical attention.
3. Teach about medication regimen, including name, purpose, dosage, schedule, and side effects.
Rationale: Medication adherence is essential for managing portal hypertension and preventing complications. Understanding promotes proper use and early recognition of adverse effects.
4. Instruct on dietary restrictions, particularly sodium limitation and protein management.
Rationale: Dietary adherence directly impacts ascites management and nutritional status. Practical guidance improves the likelihood of compliance with dietary recommendations.
5. Demonstrate and have patient return demonstration of skills such as weight monitoring, abdominal girth measurement, and symptom monitoring.
Rationale: Return demonstration confirms understanding and ability to perform self-monitoring techniques correctly, which are essential for early detection of complications.
6. Provide written materials at appropriate reading level and in preferred language.
Rationale: Written materials reinforce verbal education and serve as a reference after discharge. Materials must be accessible and understandable to be effective.
7. Include family members or caregivers in education sessions when appropriate.
Rationale: Family involvement increases support for the patient and creates additional resources for adherence to the treatment plan, especially if cognitive impairment is present.
8. Review warning signs that require immediate medical attention: hematemesis, melena, increasing abdominal distention, fever, confusion, or jaundice.
Rationale: Early recognition of complications allows for prompt intervention, potentially reducing morbidity and mortality associated with complications such as variceal bleeding or SBP.
10. Risk for Impaired Liver Function related to progression of underlying disease
- Patient will maintain stable liver function tests
- Patient will avoid hepatotoxic substances
- Patient will adhere to liver-protective regimen
Nursing Interventions for Risk for Impaired Liver Function:
1. Monitor liver function tests (ALT, AST, bilirubin, albumin, PT/INR) and MELD score regularly.
Rationale: Regular monitoring allows for early detection of deteriorating liver function and prompt intervention. The MELD score helps predict short-term mortality and need for transplantation.
2. Assess all medications for potential hepatotoxicity and consult with healthcare provider regarding alternatives when appropriate.
Rationale: Medications metabolized by the liver may accumulate and cause toxicity or further liver damage. Dose adjustments or alternative medications may be necessary.
3. Educate patient about complete abstinence from alcohol.
Rationale: Alcohol abstinence is the most effective intervention for alcoholic liver disease and can slow progression in other types of liver disease. Even small amounts of alcohol can worsen portal hypertension.
4. Provide hepatitis A and B vaccination if patient is not immune.
Rationale: Superimposed viral hepatitis in patients with existing liver disease can cause acute decompensation. Vaccination prevents additional liver injury from these preventable infections.
5. Encourage weight management for patients with non-alcoholic fatty liver disease (NAFLD).
Rationale: Weight loss of 7-10% can improve steatosis and inflammation in NAFLD, potentially slowing progression to cirrhosis and portal hypertension.
6. Administer prescribed medications for the underlying liver disease (e.g., antivirals for viral hepatitis).
Rationale: Treating the underlying cause of liver disease can slow progression and stabilize or improve portal hypertension. Antiviral therapy can achieve viral suppression or elimination in hepatitis B and C.
7. Instruct patient to avoid taking over-the-counter medications, supplements, or herbal products without consulting healthcare provider.
Rationale: Many over-the-counter products can be hepatotoxic or interact with prescribed medications. Patients should consult healthcare providers before taking any non-prescribed substances.
8. Monitor for and promptly report signs of liver decompensation: increasing jaundice, worsening coagulopathy, altered mental status.
Rationale: Early recognition of decompensation allows for prompt intervention, potentially preventing further deterioration and complications such as hepatic encephalopathy or hepatorenal syndrome.
11. Disturbed Sleep Pattern related to discomfort, pruritus, and fatigue
- Difficulty falling or staying asleep
- Reports of not feeling rested
- Irritability and fatigue
- Day-night reversal
- Dark circles under eyes
- Patient will report improved sleep quality
- Patient will demonstrate increased daytime alertness
- Patient will use effective sleep hygiene practices
Nursing Interventions for Disturbed Sleep Pattern:
1. Assess sleep patterns, including quality, duration, interruptions, and daytime napping.
Rationale: Comprehensive assessment identifies specific sleep disturbances and guides targeted interventions. Sleep disorders are common in patients with liver disease and affect quality of life.
2. Administer medications for pruritus and discomfort before bedtime.
Rationale: Nocturnal pruritus is common in liver disease and can significantly disrupt sleep. Controlling symptoms before bedtime improves sleep initiation and maintenance.
3. Schedule diuretic administration earlier in the day to minimize nighttime urination.
Rationale: Administering diuretics in the morning and early afternoon allows peak effect to occur before bedtime, reducing nighttime awakenings for urination.
4. Promote good sleep hygiene: consistent sleep schedule, comfortable environment, limiting daytime naps.
Rationale: Sleep hygiene practices help regulate sleep-wake cycles and improve sleep quality. Regular sleep schedules help normalize circadian rhythms, which are often disrupted in liver disease.
5. Assist with positioning using pillows to support abdomen and relieve pressure.
Rationale: Proper positioning can reduce discomfort from ascites and organ distention, facilitating better sleep. Left side positioning may be most comfortable for patients with ascites.
6. Implement relaxation techniques such as guided imagery or progressive muscle relaxation before bedtime.
Rationale: Relaxation techniques decrease anxiety and physical tension, promoting sleep onset. These techniques can be particularly helpful for patients with anxiety about their condition.
7. Minimize environmental stimuli during the night while maintaining safety monitoring.
Rationale: Reduced noise, light, and disruptions promote sleep maintenance. Hospital environments often contribute to sleep disruption, necessitating intentional interventions to provide a conducive sleep environment.
8. Monitor for and address signs of hepatic encephalopathy, which can manifest as sleep disturbances.
Rationale: Hepatic encephalopathy commonly presents with sleep-wake cycle disturbances and day-night reversal. Addressing the underlying encephalopathy improves sleep patterns.
12. Ineffective Coping related to chronic nature of illness and poor prognosis
- Verbalization of inability to cope
- Expressed feelings of helplessness or hopelessness
- Anxiety or depression
- Poor adherence to treatment regimen
- Destructive behavior toward self
- Patient will verbalize improved ability to cope with illness
- Patient will demonstrate adaptive coping strategies
- Patient will adhere to treatment regimen
Nursing Interventions for Ineffective Coping:
1. Assess coping mechanisms, support systems, and psychological status.
Rationale: Assessment identifies existing coping strengths and areas needing support. Depression and anxiety are common in patients with chronic liver disease and affect quality of life and adherence.
2. Establish a therapeutic relationship by demonstrating empathy and non-judgmental attitude.
Rationale: A therapeutic relationship provides emotional support and creates a safe environment for expressing concerns. This is particularly important for patients who may feel stigmatized, especially those with alcoholic liver disease.
3. Encourage verbalization of feelings, concerns, and questions about the condition.
Rationale: Expressing feelings and concerns can reduce anxiety and help identify specific areas of distress that can be addressed through targeted interventions.
4. Teach and reinforce positive coping strategies such as relaxation techniques, mindfulness, and problem-solving.
Rationale: Adaptive coping strategies help patients manage stress and enhance their sense of control over the situation, potentially improving quality of life and treatment adherence.
5. Facilitate referral to mental health professional if signs of severe anxiety, depression, or substance use disorder are present.
Rationale: Professional mental health support provides specialized interventions for psychological comorbidities. Depression in patients with liver disease is associated with poorer outcomes and increased mortality.
6. Connect patient with support groups specific to liver disease or portal hypertension.
Rationale: Peer support provides understanding, practical advice, and emotional support from others with similar experiences. Support groups can reduce feelings of isolation and normalize experiences.
7. Include family members in education and support, with patient’s permission.
Rationale: Family involvement strengthens the patient’s support system and helps family members understand how to provide effective support. Family understanding is essential for creating a supportive home environment.
8. Assist patient in identifying realistic goals and breaking down complex self-care tasks into manageable steps.
Rationale: Setting achievable goals promotes a sense of accomplishment and self-efficacy. Breaking down complex regimens into smaller steps makes self-care less overwhelming and more sustainable.
Home Care Management for Portal Hypertension
Effective home care is essential for patients with portal hypertension to prevent complications and improve quality of life. The following recommendations should be provided to patients and caregivers:
Diet and Nutrition
- Follow sodium restriction as prescribed (typically 2000 mg/day or less)
- Consume 5-6 small meals throughout the day and include a late evening snack
- Maintain adequate protein intake (1.2-1.5 g/kg/day) unless otherwise directed
- Read food labels to identify hidden sodium in processed foods
- Use herbs, spices, and salt-free seasonings to enhance flavor
- Consume adequate calories (30-35 kcal/kg/day) to prevent weight loss
- Consider consulting with a dietitian for meal planning that meets nutritional needs within restrictions
Medication Management
- Take medications exactly as prescribed, especially beta-blockers and diuretics
- Do not skip doses or adjust dosages without consulting healthcare provider
- Take diuretics early in the day to minimize nighttime urination
- Avoid NSAIDs (e.g., ibuprofen, naproxen) and use acetaminophen with caution (≤2g/day)
- Consult healthcare provider before taking any over-the-counter medications, supplements, or herbal products
- Maintain an updated medication list and bring it to all appointments
- Use pill organizers or reminder apps to improve medication adherence
Self-Monitoring
- Weigh daily at the same time, wearing similar clothing
- Measure abdominal girth at the level of the umbilicus as directed
- Report weight gain of more than 2 pounds in a day or 5 pounds in a week
- Monitor for increased abdominal distention or new-onset edema
- Check for signs of bleeding: black or bloody stools, vomiting blood, easy bruising
- Monitor for changes in mental status, confusion, or personality changes
- Keep a symptom diary to discuss with healthcare provider at appointments
Bleeding Precautions
- Use soft toothbrush and electric razor to minimize trauma
- Avoid straining during bowel movements; use stool softeners if prescribed
- Apply pressure to injection sites or wounds for longer than usual
- Avoid activities with high risk of trauma or injury
- Keep nails short and clean to prevent skin damage if scratching occurs
- Avoid blowing nose forcefully or heavy lifting
- Have family members learn basic first aid for bleeding
Skin Care
- Use mild, fragrance-free soaps and lukewarm water for bathing
- Apply emollients to damp skin after bathing and throughout the day
- Use cool compresses or prescribed medications for itching
- Wear loose, cotton clothing to minimize skin irritation
- Inspect skin daily for breakdown, especially in areas of edema
- Change positions frequently if mobility is limited
- Use pressure-relieving devices if at risk for pressure injuries
Activity and Rest
- Maintain a balance of activity and rest throughout the day
- Follow prescribed exercise plan, typically including light to moderate activity
- Avoid strenuous activity that increases intra-abdominal pressure
- Use energy conservation techniques (sitting while performing tasks, prioritizing activities)
- Establish a regular sleep schedule with consistent bedtime and wake time
- Create a sleep-conducive environment (cool, dark, quiet)
- Limit daytime napping to 30 minutes or less
When to Seek Medical Attention
Contact healthcare provider immediately or go to emergency department if experiencing:
- Vomiting blood (may be bright red or coffee-ground appearance)
- Black, tarry stools or visible blood in stool
- Sudden increase in abdominal distention or pain
- Fever above 101°F (38.3°C)
- Increasing confusion, disorientation, or extreme drowsiness
- Jaundice (yellowing of skin or eyes) that suddenly worsens
- Difficulty breathing or severe shortness of breath
- Inability to keep medications down due to vomiting
- Significant increase in swelling of legs, feet, or abdomen
Lifestyle Modifications
- Abstain completely from alcohol
- Avoid exposure to hepatitis viruses: practice safe sex, don’t share personal items like razors or toothbrushes
- Get vaccinated against hepatitis A and B if not already immune
- Manage weight through healthy diet and appropriate physical activity if overweight
- Manage diabetes and other metabolic conditions that can worsen liver disease
- Join support groups for emotional support and practical advice
- Practice stress reduction techniques such as meditation, deep breathing, or gentle yoga
Follow-up Care
- Keep all scheduled medical appointments
- Complete laboratory tests as directed
- Undergo surveillance endoscopy for varices as recommended
- Bring a list of questions, concerns, and symptom diary to appointments
- Update healthcare provider about any changes in symptoms, medications, or overall health
- Consider having a caregiver or family member attend appointments to help remember information
- Discuss advance care planning and preferences for future care
References
- Cleveland Clinic. (2022). Portal Hypertension. https://my.clevelandclinic.org/health/diseases/4912-portal-hypertension
- RNpedia. (2022). Portal Hypertension Nursing Management. https://www.rnpedia.com/nursing-notes/medical-surgical-nursing-notes/portal-hypertension-nursing-management/
- Nurseslabs. (2022). Liver Cirrhosis Nursing Care Plans. https://nurseslabs.com/liver-cirrhosis-nursing-care-plans/
- Mayo Clinic. (2025). Esophageal varices – Diagnosis and treatment. https://www.mayoclinic.org/diseases-conditions/esophageal-varices/diagnosis-treatment/drc-20351544
- RNpedia. (2022). Esophageal Varices Nursing Management. https://www.rnpedia.com/nursing-notes/medical-surgical-nursing-notes/esophageal-varices-nursing-management/
- Drugs.com. (2025). Portal Hypertension – What You Need to Know. https://www.drugs.com/cg/portal-hypertension.html
- NANDA International. (2021). Nursing Diagnoses: Definitions and Classification 2021-2023. Thieme.
- Herdman, T.H., Kamitsuru, S., & Lopes, C.T. (2021). NANDA International Nursing Diagnoses: Definitions and Classification 2021-2023. Thieme.
