Nursing Information Systems:
Using Information in Healthcare Management
- 1. Introduction to Nursing Informatics
- 2. Components of Nursing Information Systems (NIS)
- 3. Functions of Nursing Information Systems
- 4. Healthcare Data Collection and Processing
- 5. Evaluation, Analysis and Presentation of Healthcare Data
- 6. Healthcare Decision-Making Based on Data
- 7. Implementation and Evaluation of NIS
- 8. Future Trends in Nursing Informatics
- 9. Summary
1. Introduction to Nursing Informatics
Nursing informatics represents the intersection of nursing science, computer science, and information science. It involves the collection, processing, and management of data and information to support nursing practice, administration, education, and research. The American Nurses Association (ANA) defines nursing informatics as “a specialty that integrates nursing science, computer science, and information science to manage and communicate data, information, knowledge, and wisdom in nursing practice.”
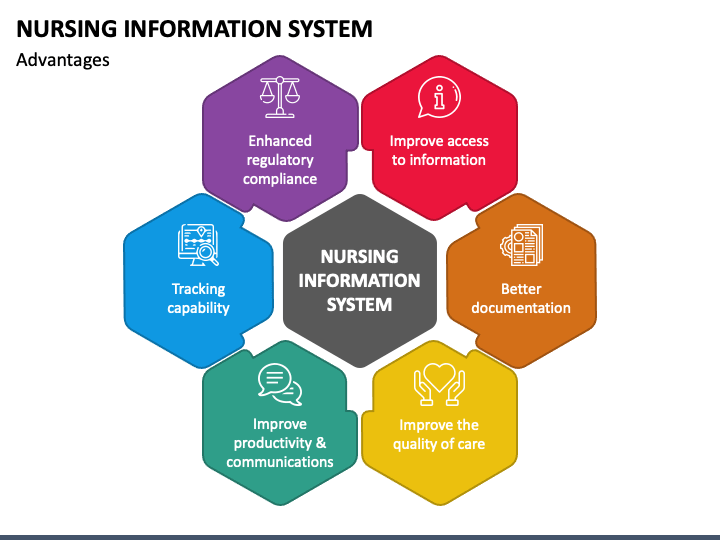
Figure 1: Overview of Nursing Information Systems
In today’s healthcare environment, nursing informatics plays a pivotal role in improving patient outcomes, enhancing workflow efficiency, and supporting evidence-based practice. As healthcare becomes increasingly data-driven, nurses must understand how information systems support clinical decision-making and healthcare management.
The evolution of nursing informatics has been driven by technological advancements, healthcare reform initiatives, and the growing recognition of the importance of data in healthcare decision-making. Today, nursing information systems (NIS) are integral components of healthcare organizations, supporting both clinical and administrative functions.
2. Components of Nursing Information Systems (NIS)
Nursing Information Systems comprise several interconnected components that work together to support nursing practice and healthcare management. Understanding these components is essential for nurses to effectively use and contribute to the development of these systems.

Figure 2: Health Information System Components based on Health Metrics Network (HMN) standards and framework
Software systems (EHR, clinical documentation, medication management)
Hardware infrastructure (servers, workstations, mobile devices)
Interfaces and networks (connectivity, information exchange)
People (users, support staff, management)
Security measures (access controls, encryption, compliance)
2.1 Hardware and Software Components
The physical infrastructure of NIS includes various hardware components:
- Central servers for data storage and processing
- Workstations and terminals at nursing stations
- Mobile devices (tablets, smartphones, laptops)
- Specialized medical hardware (barcode scanners, biometric devices)
- Networked printers and other output devices
Software components of NIS typically include:
| Software Category | Examples | Primary Functions |
|---|---|---|
| Electronic Health Records (EHR) | Epic, Cerner, MEDITECH | Patient record management, clinical documentation |
| Clinical Decision Support Systems (CDSS) | Micromedex, Lexicomp | Evidence-based guidance, alert systems |
| Nursing Documentation Systems | Integrated modules in EHR | Care planning, assessments, nursing notes |
| Medication Administration Systems | Barcode Medication Administration (BCMA) | Medication verification, administration recording |
| Staffing and Scheduling Software | ShiftWizard, Kronos | Workforce management, assignment allocation |
2.2 Network and Communication Systems
Modern NIS rely on robust network infrastructure to facilitate information exchange:
- Local Area Networks (LANs) connecting workstations within facilities
- Wide Area Networks (WANs) connecting multiple healthcare facilities
- Wireless networks supporting mobile device usage
- Health Information Exchanges (HIEs) for inter-organizational data sharing
- Interfaces with other clinical and administrative systems
Communication components are crucial for timely information exchange:
- Secure messaging systems for healthcare team communication
- Alert and notification systems
- Telehealth and remote monitoring interfaces
- Patient portals and communication platforms
2.3 Data Management Systems
Effective data management is central to NIS functionality:
- Database management systems (relational, NoSQL)
- Data warehouses for analytical processing
- Data backup and recovery systems
- Data integration and interoperability frameworks
- Terminology services (standardized nursing terminologies like NANDA, NIC, NOC)
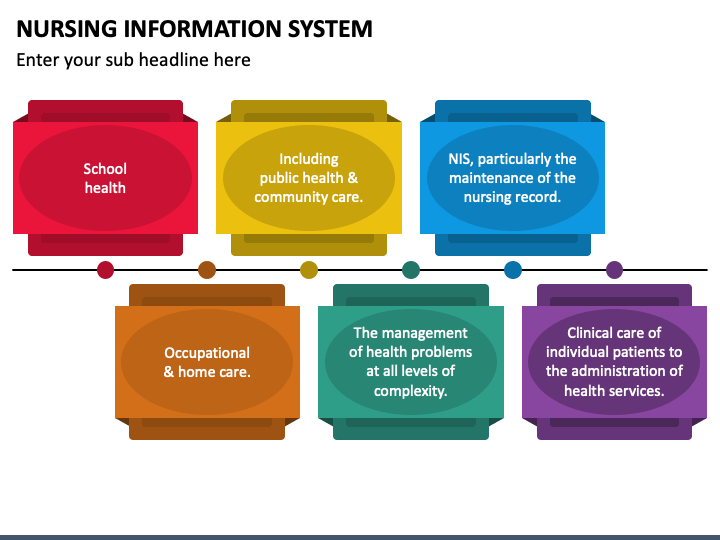
Figure 3: Data Flow in Nursing Information Systems
2.4 User Interface and Human Factors
The user interface is the point of interaction between nurses and information systems:
- Graphical User Interfaces (GUIs) designed for intuitive navigation
- Customizable dashboards for personalized views
- Mobile interfaces optimized for tablet and smartphone use
- Voice-activated and speech recognition systems
- Ergonomic considerations in hardware and software design
2.5 Security and Privacy Measures
Security components are essential for protecting sensitive healthcare information:
- Authentication systems (username/password, biometrics, smart cards)
- Authorization and access control mechanisms
- Encryption technologies for data in transit and at rest
- Audit trail and monitoring systems
- Physical security controls for hardware
- Disaster recovery and business continuity systems
3. Functions of Nursing Information Systems
Nursing Information Systems (NIS) serve multiple functions in healthcare environments, supporting both clinical practice and administrative operations. These functions evolve as technology advances and as healthcare needs change, but several core functions remain essential.
Patient Care
Documentation
Medication
Staffing
Analytics
Education
3.1 Patient Care Management
The primary function of NIS is to support direct patient care activities:
| Function | Description | Benefits |
|---|---|---|
| Nursing Assessment | Structured data collection tools for patient assessment | Comprehensive documentation, reduced omissions |
| Care Planning | Templates and tools for developing individualized care plans | Standardized yet personalized care, evidence-based interventions |
| Documentation | Electronic recording of nursing activities and patient responses | Improved legibility, accessibility, and completeness |
| Medication Management | Electronic medication administration record (eMAR) and barcode verification | Reduced medication errors, improved patient safety |
| Clinical Decision Support | Alerts, reminders, and evidence-based recommendations | Enhanced clinical decision-making, reduced practice variation |
Care planning and coordination
Health assessment and monitoring
Administration of medications and treatments
Recording outcomes and patient responses
Transition management and discharge planning
3.2 Administrative Functions
NIS also supports a range of administrative functions critical to healthcare operations:
- Workload assessment and management
- Staff scheduling and assignment
- Resource allocation and utilization tracking
- Inventory management for nursing supplies
- Billing and reimbursement support
- Regulatory compliance documentation
- Quality improvement monitoring
Effective administrative functions in NIS can lead to:
- Optimized staffing levels based on patient acuity
- Improved resource utilization and cost management
- Enhanced workforce planning and development
- Streamlined regulatory reporting and accreditation processes
- Data-driven quality improvement initiatives
3.3 Reporting and Analytics
Modern NIS include robust reporting and analytics capabilities:
- Standard reports for operational metrics
- Customizable dashboards for performance monitoring
- Advanced analytics for trend identification
- Predictive modeling for planning and forecasting
- Benchmarking against internal and external standards
- Clinical outcome reporting and tracking
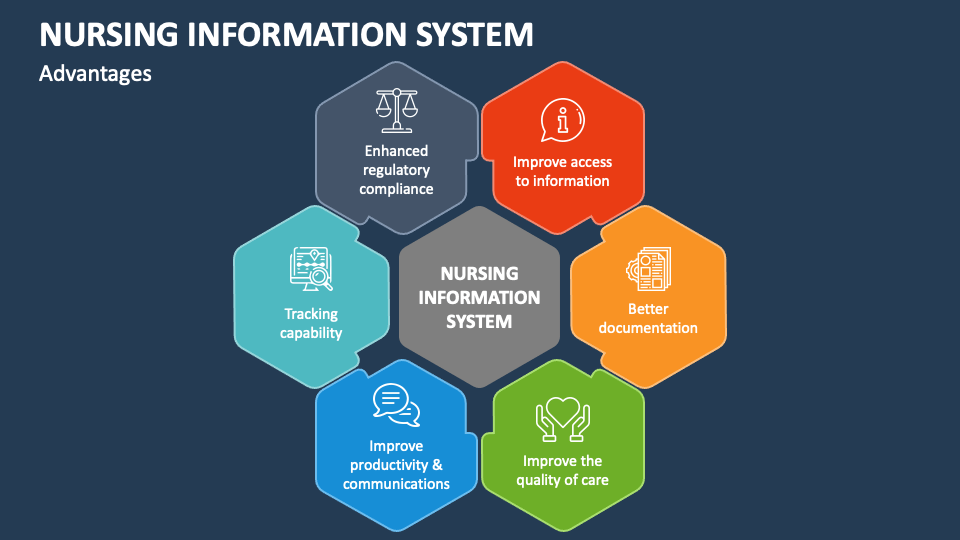
Figure 4: Key Functions of Nursing Information Systems
4. Healthcare Data Collection and Processing
Effective healthcare data collection and processing form the foundation of nursing informatics and healthcare information management. Understanding how data flows from collection to use is essential for nurses working with information systems.
4.1 Sources of Healthcare Data
Healthcare data comes from numerous sources, each contributing valuable information to the patient record and healthcare operations:
| Data Source Category | Examples | Type of Data Generated |
|---|---|---|
| Direct Patient Care | Assessment findings, vital signs, nursing notes | Clinical, subjective and objective |
| Diagnostic Systems | Laboratory results, imaging, monitoring devices | Diagnostic, physiological |
| Administrative Systems | Admissions, discharges, transfers, billing | Demographic, financial |
| Pharmacy Systems | Medication orders, dispensing records | Medication-related |
| Patient-Generated | Self-reported symptoms, wearable device data | Lifestyle, health behaviors |
| External Sources | Health information exchanges, referrals | Historical, contextual |
Internal clinical systems (EHR, lab, pharmacy)
Nursing documentation and assessments
Patient-provided information and devices
Utility systems (ADT, billing, scheduling)
Telehealth and remote monitoring
Secondary sources (referrals, outside records)
4.2 Data Quality and Integrity
High-quality data is essential for effective healthcare decision-making. Key dimensions of data quality include:
- Accuracy: Data correctly reflects the reality it represents
- Completeness: All required data elements are present
- Timeliness: Data is available when needed for decision-making
- Consistency: Data values are uniform across the system
- Relevance: Data collected supports the intended use
- Reliability: Data collection produces the same results under similar conditions
Strategies for maintaining data quality in nursing information systems include:
- Standardized terminology and classification systems
- Data validation rules and constraints
- User education and training on documentation practices
- Regular data audits and quality improvement processes
- Automated data verification and cross-checking
4.3 Healthcare Data Lifecycle
Healthcare data moves through a lifecycle from creation to archival or deletion:
- Data Creation/Acquisition: Collection of patient information during care delivery
- Data Storage: Secure preservation of data in databases and repositories
- Data Processing: Transformation of raw data into usable information
- Data Access/Sharing: Retrieval of data by authorized users for care delivery
- Data Analysis: Examination of data to identify patterns and insights
- Data Reporting: Presentation of analyzed data for decision-making
- Data Archiving/Disposal: Long-term storage or secure deletion according to retention policies
5. Evaluation, Analysis and Presentation of Healthcare Data
Once healthcare data is collected and processed, it must be analyzed and presented effectively to inform decision-making. This section explores the methods and tools used to transform raw healthcare data into actionable insights.
5.1 Healthcare Data Analysis Techniques
Several analytical approaches are used in healthcare informatics:
| Analysis Technique | Description | Application in Healthcare |
|---|---|---|
| Descriptive Analysis | Summarizes historical data to identify patterns | Patient census trends, resource utilization patterns |
| Diagnostic Analysis | Examines why events occurred | Root cause analysis of adverse events, infection rate variations |
| Predictive Analysis | Uses data patterns to forecast future outcomes | Readmission risk prediction, staffing needs forecasting |
| Prescriptive Analysis | Recommends actions based on predicted outcomes | Clinical pathway optimization, resource allocation |
| Comparative Analysis | Evaluates performance against benchmarks | Quality metrics comparison, best practice adherence |

Figure 5: Flow Chart of Data Analysis Process
Acquire relevant data from various sources
Define questions and analytical objectives
Analyze using appropriate statistical methods
Present findings in meaningful visualizations
Translate insights into actionable recommendations
5.2 Data Visualization and Presentation
Effective data visualization is essential for communicating complex healthcare information:
- Charts and Graphs: Bar charts, line graphs, pie charts for quantitative data
- Dashboards: Interactive displays of key performance indicators
- Heat Maps: Visual representation of data density or intensity
- Statistical Process Control Charts: Monitoring process performance over time
- Infographics: Visual summaries combining data with explanatory text
- Geographic Information Systems (GIS): Spatial analysis and mapping
Principles for effective healthcare data visualization:
- Choose appropriate visualization types for the data and message
- Maintain simplicity and clarity in design
- Use color and contrast purposefully
- Provide context and explanation for complex data
- Ensure accessibility for diverse users
- Present data honestly without distortion
5.3 Statistical Methods in Healthcare Data Analysis
Statistical methods commonly used in healthcare data analysis include:
| Statistical Method | Purpose | Example Application |
|---|---|---|
| Descriptive Statistics | Summarize and describe data characteristics | Average length of stay, patient demographic profiles |
| Correlation Analysis | Measure relationships between variables | Relationship between staffing levels and patient outcomes |
| Regression Analysis | Model relationships and predict outcomes | Factors influencing hospital readmission rates |
| Time Series Analysis | Analyze data points collected over time | Seasonal patterns in hospital admissions |
| Survival Analysis | Analyze time until an event occurs | Time to recovery or readmission after discharge |
Tools for healthcare data analysis include:
- Integrated analytics modules within EHR systems
- Business intelligence platforms (Tableau, Power BI)
- Statistical software (SPSS, SAS, R)
- Specialized healthcare analytics platforms
- Natural language processing tools for unstructured data analysis
6. Healthcare Decision-Making Based on Data
The ultimate purpose of healthcare data collection, analysis, and presentation is to inform decision-making at all levels of healthcare organizations. Data-driven decision-making has become increasingly important in modern healthcare as organizations strive to improve quality, reduce costs, and enhance patient outcomes.
6.1 Evidence-Based Decision-Making
Evidence-based practice (EBP) integrates the best available research evidence with clinical expertise and patient values. In nursing informatics, this approach is enhanced by data from information systems:
- Systematic use of data to identify practice patterns and variations
- Integration of research findings with local clinical data
- Measurement of intervention effectiveness in real-world settings
- Continuous quality improvement based on outcome data
- Development and refinement of clinical guidelines using aggregated data
Define the clinical question or problem
Acquire relevant evidence and data
Translate evidence into potential actions
Assess outcomes and adjust approach
The relationship between data, evidence, and practice forms a continuous cycle:
- Clinical questions arise from practice
- Data is collected and analyzed to address questions
- Findings are translated into practice changes
- New data is collected to evaluate effectiveness
- The cycle continues, driving continuous improvement
6.2 Clinical Decision Support Systems
Clinical Decision Support Systems (CDSS) are informatics tools that provide clinicians with knowledge and patient-specific information to enhance decision-making:
| CDSS Type | Description | Nursing Application |
|---|---|---|
| Alert and Reminder Systems | Notify clinicians about potential issues | Medication interaction alerts, fall risk notifications |
| Order Sets and Care Plans | Standardized groups of interventions | Evidence-based nursing care plans for specific conditions |
| Diagnostic Support | Assist in clinical reasoning and diagnosis | Wound assessment algorithms, sepsis screening tools |
| Reference Information | Context-specific knowledge resources | Procedure guides, medication information |
| Predictive Analytics | Identify patients at risk for complications | Pressure injury risk prediction, deterioration early warning |
6.3 Administrative and Management Decisions
Beyond clinical care, data drives administrative and management decisions in healthcare organizations:
- Resource Allocation: Determining staffing levels, equipment needs, and budget priorities based on workload and utilization data
- Performance Improvement: Identifying areas for process optimization and efficiency gains
- Strategic Planning: Using trend data to guide long-term organizational direction
- Regulatory Compliance: Monitoring and reporting quality metrics for accreditation and reimbursement
- Risk Management: Identifying patterns of adverse events to implement preventative measures
The data-driven management cycle includes:
- Setting measurable goals and objectives
- Collecting relevant data to track progress
- Analyzing performance against targets
- Implementing changes based on findings
- Continuing measurement to evaluate impact
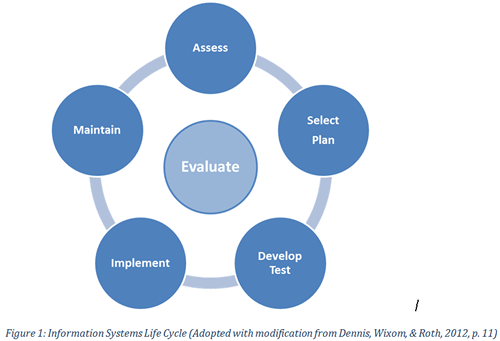
Figure 6: Healthcare Data Evaluation Cycle
7. Implementation and Evaluation of NIS
Successfully implementing and evaluating Nursing Information Systems (NIS) requires careful planning, execution, and ongoing assessment. This section explores the key considerations and best practices in NIS implementation and evaluation.
7.1 Steps in NIS Implementation
Implementing a nursing information system typically follows a structured approach:
- Needs Assessment and Planning:
- Identify organizational goals and requirements
- Engage stakeholders, especially frontline nurses
- Develop implementation strategy and timeline
- Establish governance structure and project team
- System Selection:
- Define functional and technical requirements
- Evaluate available systems against requirements
- Conduct vendor demonstrations and site visits
- Select system based on comprehensive evaluation
- System Design and Customization:
- Configure system to align with nursing workflows
- Develop or adapt documentation tools and templates
- Integrate with existing systems and data sources
- Test system functionality and usability
- Training and Education:
- Develop comprehensive training plan for all users
- Train super-users to provide ongoing support
- Provide role-specific education on system use
- Create accessible reference materials and resources
- Implementation and Go-Live:
- Develop detailed go-live plan
- Consider phased vs. “big bang” implementation approach
- Provide intensive support during transition
- Address issues and concerns promptly
- Post-Implementation Support and Optimization:
- Monitor system performance and user adoption
- Provide ongoing education and support
- Gather feedback for continuous improvement
- Implement refinements and enhancements
Stakeholder engagement and needs assessment
Infrastructure preparation and technical readiness
Meticulous planning of workflow integration
Progressive training and education approaches
Launch with adequate support resources
Evaluation and continuous improvement
7.2 Evaluation Metrics and Methods
Evaluating the effectiveness of NIS implementations involves multiple dimensions and metrics:
| Evaluation Dimension | Key Metrics | Evaluation Methods |
|---|---|---|
| System Performance | Response time, uptime, reliability | Technical monitoring, downtime tracking |
| Usability | User satisfaction, efficiency, error rates | Surveys, observations, usability testing |
| Clinical Outcomes | Quality indicators, patient outcomes | Pre/post comparisons, clinical audits |
| Workflow Impact | Documentation time, task efficiency | Time-motion studies, workflow analysis |
| Financial Impact | ROI, cost savings, revenue impact | Financial analysis, cost-benefit studies |
| Adoption and Use | Utilization rates, feature usage | System logs, user interviews |
A comprehensive evaluation framework should include:
- Baseline measurements before implementation
- Short-term evaluation during and immediately after go-live
- Long-term assessment of sustained impact
- Both quantitative and qualitative evaluation methods
- Input from diverse stakeholders, especially end-users
- Continuous monitoring of key performance indicators
7.3 Challenges and Solutions
Common challenges in NIS implementation and potential solutions include:
| Challenge | Impact | Potential Solutions |
|---|---|---|
| Resistance to Change | Low adoption, workarounds, negative attitudes | Early stakeholder involvement, clear communication, addressing concerns, demonstrating benefits |
| Workflow Disruption | Decreased efficiency, frustration, potential safety issues | Thorough workflow analysis, careful design, phased implementation, adequate support during transition |
| Integration Issues | Data silos, duplicate entry, missing information | Comprehensive interface planning, data mapping, middleware solutions, integration testing |
| Inadequate Training | Improper system use, errors, underutilization | Role-based training, multiple learning methods, ongoing education, super-user support model |
| Technical Problems | System failures, slow performance, data issues | Rigorous testing, adequate infrastructure, contingency planning, responsive technical support |
8. Future Trends in Nursing Informatics
The field of nursing informatics continues to evolve rapidly, driven by technological advancements, healthcare transformation, and changing patient needs. Understanding emerging trends helps nurses prepare for future developments in healthcare information management.
AI & ML
Mobile Health
Remote Care
IoT Devices
Privacy Focus
Key trends shaping the future of nursing informatics include:
- Artificial Intelligence and Machine Learning:
- Predictive analytics for early intervention and preventive care
- Natural language processing to extract insights from unstructured data
- Clinical decision support systems with advanced reasoning capabilities
- Automated documentation assistants to reduce documentation burden
- Interoperability and Data Exchange:
- Implementation of FHIR and other standardized data exchange formats
- Seamless information flow across care settings and organizations
- Enhanced health information exchanges with patient-centered data sharing
- Blockchain applications for secure health information exchange
- Patient Engagement and Connected Health:
- Integration of patient-generated data from wearables and monitoring devices
- Patient portals and applications with enhanced functionality
- Remote patient monitoring and telehealth expansion
- Personalized health information and education delivery
- Big Data and Analytics:
- Population health management through comprehensive data analysis
- Real-time analytics for clinical and operational decision-making
- Integration of social determinants of health data
- Advanced visualization tools for complex healthcare data
- Virtual and Augmented Reality:
- Immersive training environments for nursing education
- AR-guided procedures and interventions
- Virtual patient simulation for clinical reasoning development
- Therapeutic applications for patient care and rehabilitation
Implications for nursing practice and education:
- Growing need for nurses with specialized informatics skills and knowledge
- Integration of informatics competencies throughout nursing education
- Evolving nurse roles focused on data analysis, system optimization, and implementation
- Increased nurse involvement in technology design and evaluation
- Enhanced focus on ethical considerations in healthcare technology
- Continuing education to keep pace with technological change
9. Summary
This comprehensive exploration of Nursing Information Systems (NIS) and healthcare data management has covered several critical areas that form the foundation of nursing informatics practice. Key takeaways include:
- Nursing Information Systems comprise multiple interconnected components, including hardware, software, networks, data management systems, user interfaces, and security measures, all working together to support nursing practice and healthcare management.
- NIS serve diverse functions, supporting direct patient care through assessment, care planning, and documentation tools, while also facilitating administrative functions such as staffing, resource management, and quality monitoring.
- Healthcare data flows through a lifecycle from collection to analysis and use, with data quality and integrity being essential for effective decision-making.
- The evaluation, analysis, and presentation of healthcare data require appropriate analytical techniques, effective visualization methods, and sound statistical approaches to transform raw data into actionable insights.
- Data-driven decision-making in healthcare encompasses evidence-based clinical practice, clinical decision support systems, and administrative management, all aimed at improving quality, efficiency, and patient outcomes.
- Successful implementation of NIS requires careful planning, stakeholder engagement, thorough training, and ongoing evaluation to ensure systems meet users’ needs and organizational goals.
- Future trends in nursing informatics include AI and machine learning applications, enhanced interoperability, patient engagement technologies, advanced analytics, and immersive technologies, all of which will continue to transform nursing practice.
As healthcare continues to evolve in an increasingly digital world, nursing informatics will play an ever more important role in ensuring that information systems support high-quality, patient-centered care. Nurses at all levels must develop the knowledge and skills to effectively use information systems, critically evaluate healthcare data, and participate in the ongoing development and optimization of these essential tools.
By understanding the components, functions, and applications of Nursing Information Systems, nurses can become more effective advocates for systems that truly support nursing practice and improve patient outcomes. As both healthcare providers and knowledge workers, nurses bring a unique and valuable perspective to healthcare informatics that ensures technology serves the fundamental goals of healthcare: improving health, enhancing care experiences, and creating more efficient and effective healthcare systems.
