Organization of Geriatric Health Services in India
National Programme for Health Care of Elderly (NPHCE)
Comprehensive Notes for Nursing Students
Table of Contents
- Introduction to Elderly Care in India
- Geriatric Population Demographics
- Organization of Geriatric Health Services
- National Programme for Health Care of Elderly (NPHCE)
- Community Health Nursing Role in Elderly Care
- Geriatric Assessment Tools
- Useful Mnemonics for Geriatric Care
- Challenges and Future Directions
- Best Practices in Geriatric Care
- References
1. Introduction to Elderly Care in India
The unprecedented increase in human longevity in the 20th century has resulted in the phenomenon of population aging all over the world. Countries with large populations like India have experienced significant growth in their elderly population. Elderly care has become an essential component of healthcare delivery systems to address the unique health needs of this growing demographic.
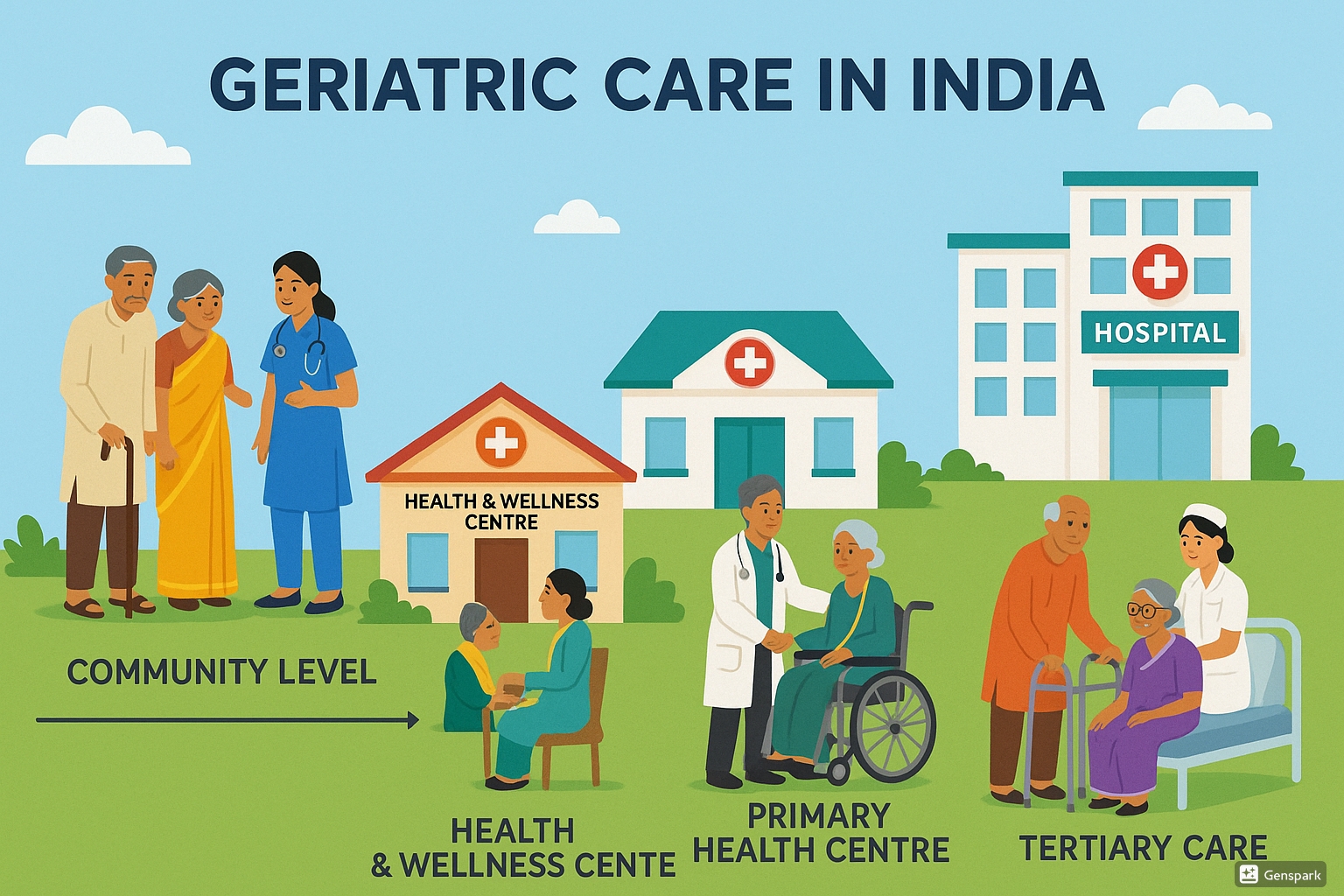
Geriatric healthcare services in India showing multiple levels of care from community to tertiary level
In India, elderly care faces unique challenges due to changing family structures, urbanization, and increasing burden of non-communicable diseases. Traditionally, elderly care was primarily provided within family settings, but demographic and social changes necessitate formal healthcare systems specifically designed for the elderly.
The healthcare needs of the elderly are complex and multidimensional, requiring an integrated approach that includes preventive, promotive, curative, and rehabilitative services. To address these needs, India has developed comprehensive geriatric health services and implemented specific programs like the National Programme for Health Care of Elderly (NPHCE).
Key Concept: What is Elderly Care?
Elderly care refers to the specialized care and services provided to older adults to meet their unique medical, physical, social, and psychological needs. It encompasses various aspects including healthcare, nutrition, mobility assistance, cognitive support, and social engagement aimed at maintaining dignity, independence, and quality of life for elderly individuals.
2. Geriatric Population Demographics
India’s elderly population has been steadily increasing over the decades. According to the 2011 census, the elderly population (aged 60 years and above) was 8.14% of the total population, which has significantly grown from 7.7% in 2001.
| Year | Projected Elderly Population (millions) | Percentage of Total Population |
|---|---|---|
| 2021 | 133.32 | ~10% |
| 2031 | 178.59 | ~12% |
| 2041 | 236.01 | ~14% |
| 2051 | 300.96 | ~19% |
Health Profile of Elderly in India
According to various National Sample Surveys and the Longitudinal Ageing Study in India (LASI), the health profile of elderly Indians shows:
- 75.68% of elderly people have one or more chronic diseases
- 53.63% have one chronic disease
- 20.83% have two chronic diseases
- 3.01% have three chronic diseases
The disability profile among elderly people in India shows:
- 40% have one or more disabilities
- 38.39% have one disability
- 15.44% have two disabilities
- 5.88% have three disabilities
Important Note for Nursing Students
Understanding demographic trends is crucial for planning elderly care services. The rapid growth of the elderly population in India indicates the increasing importance of specialized geriatric care in community health nursing practice.
3. Organization of Geriatric Health Services
The organization of elderly care services in India follows a hierarchical structure that aims to provide comprehensive care at different levels of the healthcare system. This organization ensures that elderly patients receive appropriate care based on their needs and the complexity of their health conditions.
Levels of Geriatric Care Services
| Level | Key Features | Functions |
|---|---|---|
| National Level |
|
|
| State Level |
|
|
| District Level |
|
|
| CHC Level |
|
|
| PHC Level |
|
|
| Sub-Centre/ Health & Wellness Centre |
|
|
4. National Programme for Health Care of Elderly (NPHCE)
4.1 Background and Rationale
The Ministry of Health & Family Welfare launched the “National Programme for the Health Care of Elderly” (NPHCE) during 2010-11 to address various health-related problems of elderly people. The program was introduced in recognition of the growing elderly population and their unique healthcare needs.
The NPHCE is an articulation of international and national commitments of the Government as envisaged under:
- UN Convention on the Rights of Persons with Disabilities (UNCRPD)
- National Policy on Older Persons (NPOP) adopted in 1999
- Section 20 of “The Maintenance and Welfare of Parents and Senior Citizens Act, 2007”
The NPHCE recognizes that elderly individuals have distinct physical, emotional, social, and economic needs that require specialized healthcare services. The program was designed to be state-oriented with a basic thrust to provide dedicated healthcare facilities to senior citizens (>60 years) at various levels of primary, secondary, and tertiary healthcare.
4.2 Vision and Objectives
The vision of the NPHCE encompasses:
- Providing accessible, affordable, and high-quality long-term, comprehensive and dedicated care services to an aging population
- Creating a new “architecture” for Aging
- Building a framework to create an enabling environment for “a Society for all Ages”
- Promoting the concept of Active and Healthy Aging
Specific objectives of NPHCE include:
- To provide easy access to promotional, preventive, curative and rehabilitative services through community-based primary healthcare approach
- To identify health problems in the elderly and provide appropriate health interventions
- To build capacity of the medical and paramedical professionals as well as caregivers within the family
- To provide referral services to elderly patients through district hospitals and regional medical institutions
- To create convergence with National Rural Health Mission (NRHM), AYUSH, and other line departments
4.3 Implementation Structure
The NPHCE is implemented through a structured framework that ensures effective delivery of services at all levels. The institutional framework for implementation includes:
| Level | Implementation Body | Role |
|---|---|---|
| National | Ministry of Health & Family Welfare | Overall policy, guidelines, and funding |
| State | State Health Society (SHS) | State-level implementation, fund management |
| District | District Health Society (DHS) | District-level implementation, coordination |
| Facility | Medical Colleges, District Hospitals, CHCs, PHCs, Sub-centers | Service delivery at respective levels |
Financial Management Groups (FMG) of Program Management support units at state and district levels are responsible for the maintenance of accounts, release of funds, expenditure reports, utilization certificates, and audit arrangements. The funds are released to States/UTs through the State Health Society to carry out activities at different levels.
4.4 Service Packages at Different Levels
The NPHCE provides different packages of services at various levels of healthcare delivery:
Sub-Centre Level
- Health Education related to healthy aging
- Domiciliary visits for attention and care to home-bound/bedridden elderly
- Training to family caregivers for looking after disabled elderly
- Arranging suitable supportive devices from PHC to elderly disabled persons
- Linkage with other support groups and day care centers
Primary Health Centre Level
- Weekly geriatric clinic run by a trained Medical Officer
- Maintaining records of elderly using standard format during first visit
- Conducting routine health assessment based on simple clinical examination
- Provision of medicines and proper advice on chronic ailments
- Public awareness on geriatric health during health camps
- Referral for diseases needing further investigation and treatment
Community Health Centre Level
- First Referral Unit (FRU) for elderly from PHCs
- Geriatric Clinic twice a week
- Rehabilitation Unit for physiotherapy and counseling
- Domiciliary visits by rehabilitation workers for bed-ridden elderly
- Counseling of family members for home-based care
- Health promotion and prevention activities
- Referral of complex cases to District Hospital
District Hospital Level
- Geriatric Clinic for regular dedicated OPD services
- Laboratory investigations for diagnosis and provision of medicines
- Ten-bedded Geriatric Ward for in-patient care
- Services through specialties like General Medicine, Orthopedics, Ophthalmology, ENT, etc.
- Services for referred elderly patients from CHCs/PHCs
- Conducting camps for Geriatric Services in PHCs/CHCs
- Referral services for severe cases to tertiary level hospitals
Regional Geriatric Centre Level
- Geriatric Clinic (Specialized OPD)
- 30-bedded Geriatric Ward for in-patient care
- Dedicated beds in various specialties (Surgery, Orthopedics, Psychiatry, etc.)
- Laboratory investigations with special sample collection center
- Tertiary healthcare for referred cases from district hospitals
National Center for Aging Level
- High-level tertiary care with multidisciplinary clinical services
- Specialized clinics (memory clinic, fall and syncope clinic, frail elderly clinic, etc.)
- Day care centers for investigations, rehabilitation, respite care
- Inpatient care including intensive care and rehabilitation
- Human resource development in geriatric sub-specialties
- Development of evidence-based treatment protocols
- Special focus on the care for 75+ aged population
4.5 Progress and Achievements
Since its inception, the NPHCE has made significant progress in expanding elderly care services across India:
- Expansion of primary & secondary Geriatric care services to all districts: Initially 100 districts were sanctioned in the 11th plan period, followed by 421 districts in the 12th plan period. By 2019-20, all 713 districts have been sanctioned for geriatric services.
- Development of tertiary care services: 19 Regional Geriatric Centres (RGCs) have been established in 18 states, providing specialized services.
- Two National Centres for Aging (NCA) have been developed one at Madras Medical College, Chennai and another at AIIMS, New Delhi.
Operational achievements (as of 2020):
- Daily Geriatric OPD services in 584 District Hospitals, 3,111 CHCs, and 10,180 PHCs
- Inpatient services in 507 District Hospitals and 16 RGCs
- Physiotherapy services in 445 District Hospitals, 1,131 CHCs, and 14 RGCs
- Laboratory services in 539 District Hospitals, 2,408 CHCs, and 13 RGCs
Service Provision (2019-20)
| Service Type | Number of Elderly Served |
|---|---|
| OPD care services | 26.59 million |
| Indoor admissions | 968,244 |
| Physiotherapy care | 1.53 million |
| Laboratory tests | 9.07 million |
| Elderly screened and given health cards | 2.11 million |
| Home care services provided | 241,271 |
Training and Capacity Building:
Three sets of Training modules have been developed for Medical Officers, Nurses, and Community-based workers. State-level Training of Trainers has been conducted in several states, generating approximately 236 State-level Master Trainers and 85 National Master Trainers.
5. Community Health Nursing Role in Elderly Care
Community health nurses play a vital role in the delivery of elderly care services in India. They serve as the frontline healthcare providers who connect elderly individuals with the healthcare system and ensure comprehensive care at the community level.
Key Roles and Responsibilities
Assessment and Screening
- Conducting initial screening using preliminary Comprehensive Geriatric Assessment for elderly twice a year
- Identifying elderly individuals at risk and with specific health needs in the community
- Regular monitoring of vital signs and health parameters
- Early recognition of deterioration in health status
Health Education and Promotion
- Generating awareness about healthy lifestyle practices for active and healthy aging
- Educating elderly and their families about disease management
- Promoting adequate nutrition, physical activity, and regular health check-ups
- Facilitating environmental modifications for safety
Domiciliary Care
- Conducting weekly visits to home-bound/bed-bound elderly
- Providing basic nursing care and monitoring health status
- Assisting with medication management and adherence
- Supporting family caregivers through training and guidance
Community Mobilization
- Facilitating formation of Elderly Support Groups (“Sanjeevini”)
- Organizing caregiver support groups
- Working with community organizations to create supportive environments
- Linking elderly with social welfare schemes and benefits
Referral and Follow-up
- Referring elderly requiring advanced care to appropriate facilities
- Ensuring follow-up care after hospital discharge
- Coordinating care between different healthcare system levels
- Maintaining continuity of care for chronic conditions
Rehabilitation Support
- Delivering passive physiotherapy services under supervision
- Supporting the use of assistive devices
- Promoting functional independence in activities of daily living
- Monitoring progress in rehabilitation
Community Health Nursing Approach to Elderly Care
The community health nursing approach to elderly care in India emphasizes holistic care that addresses physical, psychological, and social dimensions of health. By working at the grassroots level, community health nurses can effectively bridge the gap between elderly individuals and the formal healthcare system, ensuring that care reaches even the most vulnerable elderly populations in remote areas.
6. Geriatric Assessment Tools
Comprehensive assessment is essential for effective elderly care. The following assessment tools are commonly used in geriatric care settings in India:
Activities of Daily Living (ADL) Assessment
| Activity | Independent (1 point) | Dependent (0 points) |
|---|---|---|
| Bathing | Bathes self completely or needs help with a single part of the body | Needs help with bathing more than one part of the body |
| Dressing | Gets clothes and puts them on with or without help tying shoes | Needs help with dressing or must be completely dressed |
| Toileting | Goes to toilet, cleans self without help | Needs help transferring to toilet or cleaning self |
| Transferring | Moves in and out of bed/chair unassisted | Needs help in moving or requires complete transfer |
| Continence | Controls urination and bowel movements completely | Partially or totally incontinent |
| Feeding | Gets food from plate into mouth without help | Needs partial or total help with feeding |
Score: 6 = High independence, 0 = Low independence (very dependent)
Geriatric Depression Scale (Short Form)
- Are you basically satisfied with your life? (No = 1)
- Have you dropped many of your activities and interests? (Yes = 1)
- Do you feel that your life is empty? (Yes = 1)
- Do you often get bored? (Yes = 1)
- Are you in good spirits most of the time? (No = 1)
- Are you afraid that something bad is going to happen to you? (Yes = 1)
- Do you feel happy most of the time? (No = 1)
- Do you often feel helpless? (Yes = 1)
- Do you prefer to stay at home rather than going out? (Yes = 1)
- Do you feel you have more problems with memory than most? (Yes = 1)
- Do you think it is wonderful to be alive now? (No = 1)
- Do you feel worthless the way you are now? (Yes = 1)
- Do you feel full of energy? (No = 1)
- Do you feel your situation is hopeless? (Yes = 1)
- Do you think most people are better off than you are? (Yes = 1)
Scoring: Score > 5 points suggests probable depression. Score ≥ 10 points indicates depression.
Risk Assessment for Falls
| Question | Yes | No |
|---|---|---|
| Have you fallen in the last year? | □ | □ |
| Are you taking more than 4 types of medicines? | □ | □ |
| Do you have conditions like anxiety, depression, or loss of judgment? | □ | □ |
| Have you experienced dizziness when getting up from bed in the last year? | □ | □ |
Interpretation: Positive responses to >2 questions indicate high risk for falls and require referral.
Mini-Mental State Examination (MMSE)
A 30-point questionnaire used to measure cognitive impairment, assessing:
- Orientation to time and place (10 points)
- Registration of three objects (3 points)
- Attention and calculation (5 points)
- Recall of three objects (3 points)
- Language abilities (8 points)
- Visual construction (1 point)
Interpretation:
- Score < 24 suggests cognitive impairment for those with education above 8th class
- Score < 21 suggests cognitive impairment for those with education below 8th class
Practical Note for Nursing Students:
Assessment tools should be used as part of a comprehensive geriatric assessment and not in isolation. Cultural adaptations may be necessary for the Indian context. Always consider the literacy level, language preferences, and cultural background of elderly individuals when conducting assessments.
7. Useful Mnemonics for Geriatric Care
Mnemonics are valuable memory aids for nursing students dealing with complex geriatric conditions. Here are some helpful mnemonics for elderly care practice:
FRAIL – Comprehensive Geriatric Assessment
- Falls/Functional decline
- Reactions (medication)
- Altered mental status
- Illnesses (multiple)
- Living situation (social support)
DEHYDRATION – Simple Screen for Dehydration in Elderly
- Drugs, e.g., diuretics
- End of life
- High fever
- Yellow urine turns dark
- Dizziness (orthostasis)
- Reduced oral intake
- Axilla dry
- Tachycardia
- Incontinence (fear of)
- Oral problems/sippers
- Neurological impairment (confusion)
- Sunken eyes
DEMENTIA – Potential Reversible Causes
- Drugs
- Eyes, ears (sensory deficits)
- Metabolic (e.g., thyroid, calcium)
- Emotion (i.e., depression)
- Normal pressure hydrocephalus
- Tumor (or other space-occupying lesion)
- Infection (e.g., neurosyphilis)
- Anemia (i.e., B12 deficiency)
SIG E CAPS – Signs and Symptoms of Depression
- Sleep problems
- Interest (lack of) (Anhedonia)
- Guilt/”Worthlessness”
- Energy (lack of)
- Concentration problems
- Appetite problems
- Psychomotor retardation
- Suicide ideations
5Ms of Geriatrics
- Mobility (promoting function and preventing falls)
- Mind (cognitive health and mental wellbeing)
- Medications (optimizing medication use)
- Multicomplexity (addressing multiple comorbidities)
- Matters Most (aligning care with individual’s goals)
While mnemonics are helpful memory aids, they should be used in conjunction with comprehensive assessment and clinical judgment. Always refer to standard protocols and guidelines when making clinical decisions in elderly care.
8. Challenges and Future Directions
Despite the progress made in elderly care services in India, several challenges remain:
Human Resource Challenges
- Shortage of trained geriatricians and geriatric nurses
- Limited training opportunities in geriatrics for healthcare professionals
- High workload on existing healthcare workers
- Lack of specialized skills for managing complex geriatric conditions
Infrastructure and Resource Constraints
- Insufficient geriatric beds in secondary and tertiary care facilities
- Limited availability of rehabilitation services
- Inadequate equipment and assistive devices
- Uneven distribution of resources across regions
Integration and Coordination Issues
- Fragmented care delivery across different levels
- Limited coordination between healthcare and social welfare services
- Weak referral systems
- Inadequate follow-up mechanisms
Accessibility and Awareness
- Limited access to services in rural and remote areas
- Low awareness about available services among elderly
- Stigma associated with seeking mental health care
- Financial barriers to accessing care
Future Directions
To address these challenges and strengthen elderly care services in India, several future directions are proposed:
Enhanced Training and Capacity Building
Expanding training programs in geriatrics for all healthcare professionals, including dedicated courses for community health nurses.
Strengthening Primary Care
Increasing the focus on geriatric services at primary care level through Health and Wellness Centres.
Technology Integration
Leveraging telehealth and digital health solutions to expand reach of geriatric services.
Community Participation
Promoting greater community involvement in elderly care through support groups and volunteer networks.
Research and Evidence Generation
Encouraging more research on elderly health issues specific to the Indian context.
Policy Integration
Better coordination between health and social care policies for comprehensive elderly care.
Public-Private Partnerships
Exploring collaborations with private sector to expand service availability.
Focus on Preventive Care
Emphasizing preventive and promotive health measures for healthy aging.
9. Best Practices in Geriatric Care
Several best practices have emerged in the field of elderly care that can be adopted by community health nurses in India:
Mobile Elderly Classification System
Categorizing elderly individuals based on their mobility status helps in prioritizing care:
- Mobile Elderly: Independent in movement and activities of daily living
- Restricted Mobility Elderly: Requiring personal assistance or mobility devices
- Bed-bound/Home-bound Elderly: Requiring continuous care and assistance
This classification guides the type and intensity of care needed, enabling efficient resource allocation and personalized care planning.
Elderly Support Groups (Sanjeevini)
Formation of support groups for elderly individuals has shown positive outcomes:
- Providing emotional and social support
- Sharing experiences and coping strategies
- Promoting peer education on health matters
- Encouraging adoption of assistive devices and healthy behaviors
- Creating a sense of community and belonging
Caregiver Training and Support
Empowering family caregivers through training and support:
- Basic nursing skills for care of bedridden patients
- Wound care and pressure ulcer prevention
- Safe transfer techniques and assistance with activities of daily living
- Medication management
- Psychological support for caregivers to prevent burnout
Environmental Modification
Creating safer home environments for elderly:
- Removing trip hazards and installing grab bars
- Improving lighting, especially in pathways and stairs
- Making bathrooms elder-friendly with non-slip surfaces
- Arranging furniture to allow easier movement
- Ensuring essential items are within reach
Intergenerational Bonding Programs
Promoting interactions between elderly and younger generations:
- Youth volunteers assisting elderly with daily activities
- Knowledge and skill transfer programs
- Collaborative community activities
- Digital literacy training by younger volunteers
- Storytelling and cultural heritage preservation
“Month of the Elderly” Campaign
Organized around International Day for Older Persons (October 1):
- Concentrated efforts for identifying and screening elderly
- Health camps and awareness activities
- Distribution of assistive devices
- Social events celebrating contributions of elderly
- Connecting elderly with available welfare schemes
Community Health Nursing Innovation
Some regions in India have implemented innovative approaches like mobile geriatric clinics, telehealth consultations for remote elderly, and training community volunteers as “elderly friends” who make regular visits to check on isolated elderly individuals. These practices can be adapted and scaled according to local contexts and resources.
10. References
- Ministry of Health and Family Welfare. (2011). National Program for Health Care of the Elderly (NPHCE): Operational Guidelines. New Delhi: Director General of Health Services, MOHFW, Government of India.
- Central Statistics Office. (2011). Situation Analysis of the Elderly in India. New Delhi: Central Statistics Office Ministry of Statistics and Programme Implementation, Government of India.
- Ministry of Health and Family Welfare. (2021). Detailed Brief of NPHCE. Retrieved from https://mohfw.gov.in/sites/default/files/Detailed%20Breif%20of%20NPHCE.pdf
- National Health Systems Resource Centre. (2021). Operational Guidelines for Elderly Care at Health and Wellness Centre. Retrieved from https://nhsrcindia.org/sites/default/files/2021-06/Operational%20Guidelines%20for%20Elderly%20Care%20at%20HWC.pdf
- Verma, R., & Khanna, P. (2013). National Program of Health-Care for the Elderly in India: A Hope for Healthy Ageing. International Journal of Preventive Medicine, 4(10), 1103-1107.
- Agarwal, A., Lubet, A., Mitgang, E., Mohanty, S., & Bloom, D. E. (2016). Population Aging in India: Facts, Issues, and Options. IZA Discussion Papers, No. 10162.
- Longitudinal Ageing Study in India (LASI) Wave-1 Report. (2021). Retrieved from https://www.iipsindia.ac.in/content/lasi-publications
- World Health Organization. (2015). World report on ageing and health. Geneva: World Health Organization.
- Sheikh, J.L., & Yesavage, J.A. (1986). Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. Clinical Gerontology, 5(1-2), 165-173.
- Thomas, D.R., et al. (2008). Simple screen for dehydration. Journal of the American Medical Directors Association.
- Flaherty, J.H. (1998). Commonly prescribed and over-the-counter medications: Causes of confusion. Clinics in Geriatric Medicine, 14(1), 101-127.
- Inouye, S.K., et al. (1999). A multicomponent intervention to prevent delirium in hospitalized older patients. New England Journal of Medicine, 340(9), 669-676.
2025 Comprehensive Geriatric Care Notes for Nursing Students
Prepared for educational purposes only
