🩹 Other Parenteral Routes
Complete Guide for Nursing Students: Beyond Traditional Injections
📋 Table of Contents
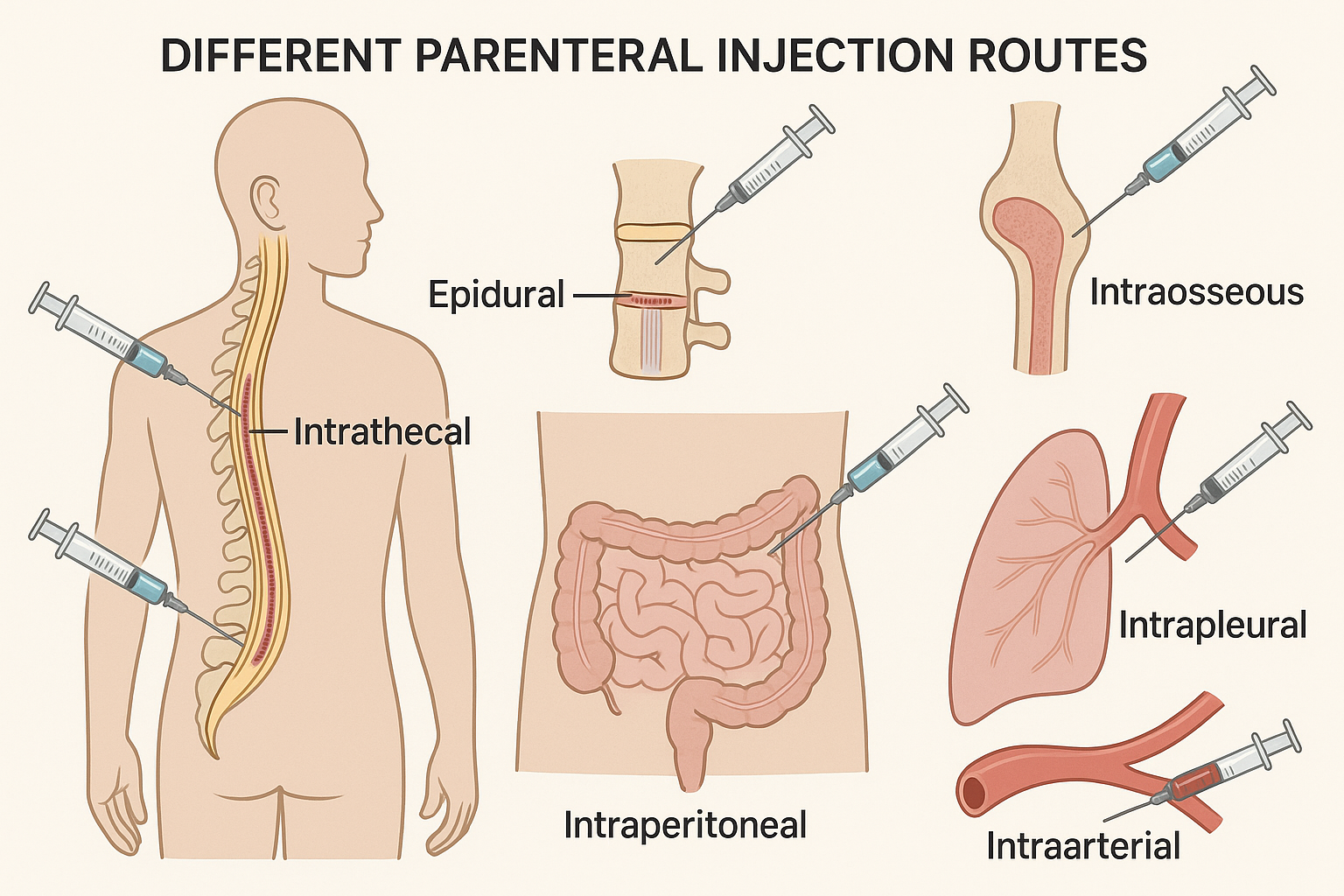
Specialized Parenteral Routes Overview
🎯 Introduction to Specialized Parenteral Routes
While traditional parenteral administration includes subcutaneous, intramuscular, and intravenous routes, advanced healthcare practices require knowledge of specialized delivery methods. These alternative parenteral routes offer targeted drug delivery for specific clinical scenarios where conventional methods may be inadequate or inappropriate.
📖 Definition of Parenteral Administration
Parenteral: Derived from Greek “para” (beside) and “enteron” (intestine), referring to any route of administration other than through the digestive tract. These specialized parenteral routes bypass the gastrointestinal system entirely, providing direct access to specific anatomical compartments.
Key Learning Objectives
- Understand anatomical considerations for each parenteral route
- Identify appropriate clinical indications and contraindications
- Master proper technique and safety protocols
- Recognize potential complications and nursing interventions
- Apply evidence-based practice principles
Definition & Anatomy
Epidural space is the potential space between the ligamentum flavum and the dura mater of the spinal cord. This parenteral route allows for regional anesthesia and analgesia by blocking nerve conduction at the spinal level.
📏 Anatomical Landmarks:
- Location: Between vertebrae L3-L4 or L4-L5
- Depth: Approximately 4-6 cm in adults
- Contents: Epidural fat, venous plexus, lymphatics
- Volume capacity: 20-30 mL
🎯 Clinical Indications
- Obstetric procedures: Labor analgesia, cesarean delivery
- Surgical anesthesia: Lower abdominal, pelvic, and lower extremity procedures
- Post-operative pain management: Major orthopedic and abdominal surgeries
- Chronic pain management: Cancer pain, chronic back pain
- Diagnostic procedures: Epidurography
⚕️ Procedure Overview
- Patient positioning: Lateral decubitus or sitting position
- Sterile technique: Full aseptic precautions
- Local anesthesia: Lidocaine 1-2% at insertion site
- Needle insertion: Loss of resistance technique using saline or air
- Catheter placement: Thread 3-5 cm into epidural space
- Test dose: Lidocaine with epinephrine to confirm placement
👩⚕️ Nursing Responsibilities
Pre-procedure:
- Verify informed consent and allergies
- Establish IV access and baseline vitals
- Position patient appropriately
- Prepare sterile equipment tray
During procedure:
- Monitor vital signs continuously
- Provide emotional support and positioning assistance
- Maintain sterile field integrity
- Document procedure details
Post-procedure:
- Assess motor and sensory function every 15 minutes initially
- Monitor blood pressure and respiratory status
- Secure catheter and maintain dressing
- Document pain scores and medication effectiveness
⚠️ Potential Complications
| Complication | Incidence | Signs/Symptoms | Management |
|---|---|---|---|
| Dural puncture | 0.5-5% | Severe headache, nausea | Blood patch, bed rest |
| Hypotension | 10-30% | BP drop >20% baseline | IV fluids, vasopressors |
| High/total spinal | <0.1% | Respiratory depression | Airway support, vasopressors |
| Infection | 0.2-0.3% | Fever, back pain | Antibiotics, removal |
Pain relief primary goal
Infection prevention critical
Dural puncture avoid
Under sterile conditions
Respiratory monitoring essential
Anesthesia level assessment
Loss of resistance technique
Definition & Anatomy
Intrathecal administration involves direct injection into the cerebrospinal fluid (CSF) within the subarachnoid space. This parenteral route provides immediate access to the central nervous system, bypassing the blood-brain barrier.
🧠 Anatomical Features:
- Location: Between arachnoid and pia mater
- CSF volume: 120-150 mL total, 30-40 mL lumbar
- Pressure: 10-15 mmHg (normal)
- Circulation: Complete turnover every 6-8 hours
🎯 Clinical Applications
- Spinal anesthesia: Surgical procedures below T10 level
- Chemotherapy: CNS lymphomas, leukemia treatment
- Pain management: Cancer pain, chronic intractable pain
- Diagnostic procedures: CSF sampling, myelography
- Emergency situations: Severe pain unresponsive to systemic medications
- Infection treatment: CNS infections (antibiotics)
⚕️ Technical Procedure
- Patient preparation: Lateral decubitus or sitting position
- Site identification: L3-L4 or L4-L5 interspace
- Sterile technique: Surgical-level asepsis
- Needle insertion: 22-25 gauge spinal needle
- CSF confirmation: Clear fluid flow indicates correct placement
- Medication injection: Slow injection over 1-2 minutes
- Needle withdrawal: Smooth, controlled removal
💡 Clinical Pearls
- Volume considerations: Maximum 3-5 mL for single injection
- Osmolality: Must be isotonic to prevent neural damage
- pH requirements: Should be physiologic (7.35-7.45)
- Preservative-free: Only preservative-free medications should be used
👩⚕️ Nursing Management
Pre-procedure Assessment:
- Verify coagulation studies and platelet count
- Assess for increased intracranial pressure signs
- Check for skin infection at insertion site
- Document baseline neurological status
Post-procedure Monitoring:
- Neurological assessments every 15 minutes x 1 hour
- Vital signs monitoring per protocol
- Assess for headache development
- Monitor for signs of infection or bleeding
⚠️ Complications & Management
| Complication | Frequency | Prevention | Treatment |
|---|---|---|---|
| Post-dural puncture headache | 10-30% | Small needle, minimize attempts | Conservative care, epidural blood patch |
| Meningitis | <0.1% | Strict aseptic technique | Immediate antibiotics, supportive care |
| Spinal hematoma | Very rare | Check coagulation status | Emergency surgical evacuation |
| Neural injury | Extremely rare | Proper technique, anatomical landmarks | Neurological consultation |
Neurological monitoring vital
Technique must be sterile
Remove air bubbles first
Assess coagulation status
Test dose if applicable
Headache watch for
Emergency equipment ready
CSF pressure monitor
Anatomical landmarks crucial
Lateral position preferred
Definition & Physiology
Intraosseous (IO) access involves insertion of a specialized needle directly into the bone marrow cavity for rapid vascular access. This parenteral route utilizes the rich vascular network within bone marrow, which does not collapse during shock states.
🦴 Physiological Principles:
- Vascular anatomy: Bone marrow contains extensive venous sinusoids
- Flow characteristics: Direct communication with central circulation
- Absorption rate: Similar to central venous access
- Volume capacity: Can handle high-volume infusions with pressure
🎯 Clinical Indications
- Emergency situations: Cardiac arrest, severe trauma, shock
- Difficult IV access: Pediatric patients, obesity, dehydration
- Burns: When peripheral sites unavailable
- Mass casualty events: Rapid access for multiple patients
- Conscious sedation: When IV access fails
- Military/pre-hospital care: Field conditions
⚕️ Insertion Sites & Technique
🎯 Preferred Sites (Adults):
| Site | Landmarks | Advantages | Considerations |
|---|---|---|---|
| Proximal tibia | 2 cm below tibial tuberosity, medial aspect | Easy palpation, large target | Avoid growth plate in children |
| Proximal humerus | Greater tubercle, 2 cm below acromion | Higher flow rates possible | Requires specific positioning |
| Distal tibia | Medial malleolus, 2 cm proximal | Alternative when proximal unavailable | Lower flow rates |
🔧 Insertion Steps:
- Site preparation: Cleanse with antiseptic solution
- Local anesthesia: Lidocaine if patient conscious
- Needle insertion: 90-degree angle with rotating motion
- Penetration confirmation: Sudden decrease in resistance
- Stylet removal: Observe for bone marrow aspiration
- Flush test: 10 mL normal saline without resistance
👩⚕️ Nursing Management
Equipment Preparation:
- IO device (manual or powered)
- Antiseptic solution
- Local anesthetic (if conscious)
- Extension tubing and IV fluids
- Pressure bag for infusions
Monitoring Parameters:
- Flow assessment: Flush easily without resistance
- Infiltration check: No swelling at insertion site
- Pain management: Local anesthetic for conscious patients
- Site integrity: Secure stabilization to prevent displacement
Medication Administration:
- All IV medications can be given IO
- May require pressure for adequate flow
- Flush with 10 mL saline after each medication
- Monitor for signs of osteomyelitis with prolonged use
💡 Clinical Considerations
- Flow rates: Use pressure bags for rates >100 mL/hr
- Duration limits: Remove within 24-48 hours
- Pain management: Lidocaine 1-2% into marrow cavity before infusion
- Contraindications: Fracture at site, infection, previous orthopedic hardware
⚠️ Complications
- Infiltration: Most common, recognize early and reposition
- Osteomyelitis: Rare but serious, risk increases with duration
- Growth plate damage: Pediatric consideration
- Needle breakage: Extremely rare with proper technique
- Pain during infusion: Normal, managed with local anesthesia
Needle 90-degree angle
Tibia proximal preferred site
Rotating motion for insertion
Aspiration confirms placement
Osteomyelitis prevention priority
Saline flush test essential
Secure stabilization required
Emergency access primary use
Observe for infiltration
Use pressure for adequate flow
Short-term use recommended
Definition & Anatomy
Intraperitoneal administration involves injection of medications directly into the peritoneal cavity. This parenteral route utilizes the large surface area of the peritoneum for drug absorption and distribution.
🔬 Anatomical Considerations:
- Peritoneal surface area: Approximately 1.5-2 m² (similar to skin)
- Peritoneal fluid volume: 50-100 mL in healthy adults
- Absorption mechanism: Lymphatic drainage and capillary absorption
- Circulation pattern: Continuous fluid movement from diaphragm to pelvis
🎯 Clinical Applications
- Peritoneal dialysis: Chronic kidney disease management
- Chemotherapy delivery: Ovarian, gastric, and colon cancers
- Infection treatment: Peritonitis, intra-abdominal infections
- Pain management: Chronic abdominal pain syndromes
- Fluid resuscitation: Historical use in pediatric emergency care
- Diagnostic procedures: Peritoneal lavage for trauma assessment
⚕️ Access Methods
🏥 Catheter Types:
| Catheter Type | Indication | Duration | Characteristics |
|---|---|---|---|
| Tenckhoff catheter | Peritoneal dialysis | Long-term (years) | Tunneled, cuffed design |
| Port systems | Chemotherapy | Intermittent use | Implanted, accessed with needle |
| Acute catheters | Temporary procedures | Hours to days | Trocar or Seldinger technique |
🔧 Insertion Technique:
- Patient positioning: Supine with slight Trendelenburg
- Site selection: Lateral to rectus muscle, below umbilicus
- Sterile preparation: Full surgical asepsis
- Local anesthesia: Lidocaine through all tissue layers
- Catheter placement: Guide into pelvis, confirm free drainage
- Securing: Suture and sterile dressing application
👩⚕️ Nursing Care
Peritoneal Dialysis Management:
- Exchange procedure: Fill, dwell, drain cycles
- Infection prevention: Meticulous sterile technique
- Exit site care: Daily cleaning and assessment
- Fluid balance monitoring: Daily weights and intake/output
Chemotherapy Administration:
- Pre-medication: Anti-emetics and pain control
- Drug preparation: Verify concentration and volume
- Instillation technique: Warm solution, gravity drainage
- Post-procedure monitoring: Vital signs, abdominal assessment
Assessment Parameters:
- Abdominal girth and distension
- Respiratory status (diaphragmatic pressure)
- Fluid volume status and electrolyte balance
- Signs of infection or peritonitis
⚠️ Complications & Prevention
| Complication | Incidence | Risk Factors | Prevention |
|---|---|---|---|
| Peritonitis | 0.3-0.5 episodes/year | Poor technique, contamination | Strict aseptic technique, exit site care |
| Catheter dysfunction | 10-20% | Omentum wrapping, fibrin clots | Proper positioning, heparin flushes |
| Fluid leak | 5-10% | Early use, high pressures | Healing time, gradual volume increase |
| Hernia formation | 5-15% | Increased abdominal pressure | Proper technique, avoid straining |
💡 Best Practice Guidelines
- Volume limits: Adults 2-3L per exchange, children 30-40 mL/kg
- Temperature: Warm solutions to body temperature
- Dwell time: Varies by indication (30 minutes to 8 hours)
- Contraindications: Recent abdominal surgery, extensive adhesions
Navigate catheter carefully
Temperature warm solutions
Respiratory status monitor
Aseptic technique crucial
Peritonitis prevention priority
Exit site care essential
Record fluid balance accurately
Infection signs watch for
Tunneled catheter long-term
Outflow should drain freely
Needdle access for ports
Equipment sterile maintain
Abdominal assessment routine
Large surface area available
Definition & Anatomy
Intrapleural administration involves injection of medications directly into the pleural space between the visceral and parietal pleura. This parenteral route provides regional anesthesia and targeted drug delivery to the thoracic cavity.
🫁 Pleural Space Anatomy:
- Normal volume: 5-10 mL of pleural fluid
- Surface area: Large absorptive surface
- Pressure: Negative pressure (-5 to -10 cmH₂O)
- Lymphatic drainage: Rich lymphatic network for absorption
🎯 Clinical Applications
- Post-operative analgesia: Thoracic and upper abdominal surgery
- Cancer treatment: Malignant pleural effusions (pleurodesis)
- Pain management: Chronic chest wall pain, rib fractures
- Diagnostic procedures: Pleural biopsy anesthesia
- Infection treatment: Empyema management
- Research applications: Regional chemotherapy delivery
⚕️ Access Techniques
🎯 Insertion Methods:
| Method | Equipment | Indications | Advantages |
|---|---|---|---|
| Percutaneous catheter | 14-16 gauge catheter | Single dose or short-term | Simple insertion, low cost |
| Chest tube modification | Existing chest tube | Post-surgical patients | Utilize existing access |
| Tunneled catheter | Specialized pleural catheter | Long-term therapy | Reduced infection risk |
🔧 Insertion Procedure:
- Patient positioning: Lateral decubitus or sitting upright
- Site selection: 7th-8th intercostal space, posterior axillary line
- Ultrasound guidance: Identify pleural space and avoid organs
- Sterile technique: Full sterile barriers and preparation
- Local anesthesia: Lidocaine to pleura
- Catheter insertion: Over-the-needle technique
- Position confirmation: Aspiration test or imaging
👩⚕️ Nursing Management
Pre-procedure Preparation:
- Verify informed consent and coagulation status
- Establish IV access and baseline vitals
- Position patient appropriately
- Prepare emergency equipment (chest tube tray)
During Administration:
- Medication preparation: Preservative-free solutions
- Volume considerations: Usually 20-30 mL maximum
- Injection rate: Slow installation over 2-3 minutes
- Patient positioning: May require position changes for distribution
Post-procedure Monitoring:
- Chest X-ray to rule out pneumothorax
- Respiratory assessment every 15 minutes x 1 hour
- Pain assessment and management
- Monitor for signs of systemic absorption
⚠️ Potential Complications
| Complication | Frequency | Early Signs | Management |
|---|---|---|---|
| Pneumothorax | 2-5% | Chest pain, dyspnea | Chest X-ray, possible chest tube |
| Systemic absorption | Variable | Hypotension, sedation | Supportive care, monitor vitals |
| Infection | <1% | Fever, chest pain | Antibiotics, catheter removal |
| Pleural irritation | 10-20% | Chest discomfort | Analgesics, position changes |
💡 Clinical Considerations
- Drug selection: Local anesthetics, steroids, chemotherapy agents
- Contraindications: Coagulopathy, skin infection, severe COPD
- Optimal positioning: Affected side dependent for 30 minutes post-injection
- Duration of effect: 8-24 hours depending on agent used
Negative pressure present
Thoracic procedures common use
Respiratory monitoring essential
Avoid pneumothorax complication
Position patient appropriately
Local anesthetics frequently used
Emergency equipment standby
Ultrasound guidance helpful
Radiograph post-procedure
Absorption can be systemic
Lymphatic drainage active
Definition & Physiology
Intraarterial administration involves direct injection of medications into arterial circulation. This parenteral route provides immediate, high-concentration drug delivery to specific organ systems while minimizing systemic exposure.
🫀 Vascular Principles:
- High pressure system: 90-120 mmHg systolic pressure
- Pulsatile flow: Requires specialized monitoring
- Rich oxygen content: 95-100% oxygen saturation
- Direct organ perfusion: Bypasses venous circulation initially
🎯 Clinical Applications
- Diagnostic procedures: Angiography, arterial sampling
- Interventional procedures: Angioplasty, stent placement
- Chemotherapy delivery: Hepatic arterial infusion, limb perfusion
- Thrombolytic therapy: Acute stroke treatment, peripheral artery occlusion
- Emergency medications: Cardiac arrest (rarely used)
- Blood pressure monitoring: Continuous arterial monitoring
- Research applications: Organ-specific drug studies
⚕️ Access Sites & Techniques
🎯 Common Access Sites:
| Artery | Location | Advantages | Considerations |
|---|---|---|---|
| Radial artery | Wrist, lateral aspect | Superficial, good collateral flow | Perform Allen test first |
| Femoral artery | Groin, below inguinal ligament | Large caliber, easy access | Higher bleeding risk |
| Brachial artery | Antecubital fossa | Alternative upper extremity | Risk of compartment syndrome |
| Axillary artery | Axilla, below clavicle | Alternative to femoral | Nerve proximity concern |
🔧 Seldinger Technique:
- Site preparation: Sterile field, local anesthesia
- Needle insertion: 18-gauge needle at 30-45 degree angle
- Arterial confirmation: Pulsatile, bright red blood return
- Guidewire insertion: Flexible guidewire through needle
- Catheter placement: Over guidewire into artery
- System connection: Pressure monitoring and flush system
👩⚕️ Specialized Nursing Care
Pre-procedure Assessment:
- Coagulation studies: PT, PTT, INR, platelet count
- Vascular assessment: Pulses, collateral circulation
- Allen test: Verify ulnar collateral flow for radial access
- Allergies: Contrast agents, medications
During Procedure:
- Continuous monitoring: Arterial waveform, vital signs
- Heparinization: Maintain catheter patency
- Pressure monitoring: Invasive blood pressure measurement
- Contrast administration: Monitor for allergic reactions
Post-procedure Management:
- Hemostasis: Manual compression or closure device
- Pulse checks: Distal circulation assessment
- Bleeding surveillance: Access site and retroperitoneal
- Activity restrictions: Bed rest duration per protocol
⚠️ Major Complications
| Complication | Incidence | Risk Factors | Prevention/Management |
|---|---|---|---|
| Bleeding/Hematoma | 2-7% | Anticoagulation, hypertension | Adequate compression, pressure monitoring |
| Arterial occlusion | 0.5-2% | Small vessel, spasm | Heparinization, vasodilators |
| Pseudoaneurysm | 0.5-1% | Inadequate hemostasis | Ultrasound compression, surgical repair |
| Arteriovenous fistula | <0.5% | Through-and-through puncture | Surgical consultation, monitoring |
| Stroke/Embolism | <0.1% | Air embolism, clot formation | Careful flushing, anticoagulation |
💡 Advanced Practice Considerations
- Medication compatibility: Check pH and osmolality before injection
- Injection rate: Slow push to prevent vasospasm
- Volume limits: Small volumes to prevent hemodynamic changes
- Specialized training: Requires advanced certification and competency
- Equipment requirements: Pressure monitoring, fluoroscopy capability
⚠️ Critical Safety Considerations
- Never inject air: Risk of air embolism and stroke
- Continuous pressure monitoring: Loss of waveform indicates displacement
- Immediate recognition: Arterial bleeding requires immediate intervention
- Specialized expertise: Should only be performed by trained practitioners
Never inject air bubbles
Training specialized required
Radial artery common site
Allen test perform first
Anticoagulation monitor closely
Recognize bleeding immediately
Thrombosis prevention priority
Embolism risk always present
Remove catheter carefully
Invasive monitoring essential
Access site compress adequately
Large bore equipment ready
📊 Comparative Analysis of Parenteral Routes
Route Characteristics Comparison
| Route | Onset | Duration | Volume Limit | Skill Level | Complications |
|---|---|---|---|---|---|
| Epidural | 10-20 minutes | 2-6 hours | 20-30 mL | Advanced | Dural puncture, hypotension |
| Intrathecal | Immediate | 3-8 hours | 3-5 mL | Expert | PDPH, meningitis |
| Intraosseous | Immediate | Variable | Unlimited* | Intermediate | Infiltration, osteomyelitis |
| Intraperitoneal | 30-60 minutes | 4-8 hours | 2-3 L | Advanced | Peritonitis, catheter dysfunction |
| Intrapleural | 15-30 minutes | 8-24 hours | 20-30 mL | Advanced | Pneumothorax, systemic absorption |
| Intraarterial | Immediate | Variable | Small volumes | Expert | Bleeding, thrombosis, embolism |
*With pressure assistance
💡 Route Selection Criteria
- Patient condition: Hemodynamic stability, consciousness level
- Clinical indication: Type of medication, desired effect
- Practitioner expertise: Training level and competency
- Equipment availability: Specialized tools and monitoring
- Risk-benefit ratio: Complication potential vs. therapeutic benefit
👩⚕️ Comprehensive Nursing Considerations
Universal Precautions for All Parenteral Routes
🔐 Pre-procedure Essentials:
- Informed consent: Verify understanding and obtain signature
- Allergy assessment: Medications, latex, antiseptics
- Laboratory review: Coagulation studies when indicated
- Baseline vitals: Establish comparison parameters
- Equipment check: Functionality and expiration dates
🎯 During Procedure:
- Sterile technique: Maintain throughout procedure
- Patient positioning: Optimal access and comfort
- Vital sign monitoring: Continuous or frequent assessment
- Communication: Explain each step, provide reassurance
- Documentation: Real-time recording of events
📋 Post-procedure Protocol:
- Immediate assessment: Vital signs and complications
- Site evaluation: Bleeding, swelling, signs of infection
- Function testing: Neurological or circulatory checks
- Patient education: Warning signs and care instructions
- Follow-up planning: Schedule appropriate monitoring
🚨 Red Flag Symptoms – Immediate Action Required
| Symptom | Possible Cause | Immediate Action |
|---|---|---|
| Severe headache with neck stiffness | Meningitis, dural puncture | Neurological consultation, antibiotics |
| Sudden dyspnea, chest pain | Pneumothorax, embolism | Chest X-ray, oxygen, emergency response |
| Rapid expansion of hematoma | Arterial bleeding | Direct pressure, surgical consultation |
| Loss of pulse distal to site | Arterial occlusion | Vascular surgery, anticoagulation |
| High fever with rigors | Systemic infection | Blood cultures, broad-spectrum antibiotics |
💡 Quality Improvement Strategies
- Competency validation: Regular skills assessment and training
- Checklist utilization: Standardized safety protocols
- Peer review: Case discussions and learning opportunities
- Technology integration: Ultrasound guidance, pressure monitoring
- Patient outcomes tracking: Complication rates and satisfaction scores
🌍 Global Best Practices in Specialized Parenteral Administration
🇺🇸 United States – Johns Hopkins Hospital
Innovation: Implementation of ultrasound-guided intraosseous access in emergency departments has reduced failed IV attempts by 65%. Their protocol includes mandatory competency validation every 6 months and real-time quality metrics tracking.
🇸🇪 Sweden – Karolinska Institute
Safety Protocol: Developed standardized checklists for epidural procedures that reduced dural puncture rates from 2.1% to 0.8%. Their approach includes two-person verification system and post-procedure neurological assessment protocols.
🇯🇵 Japan – Tokyo Medical Center
Technology Integration: Pioneered robotic-assisted intraarterial catheter placement for stroke interventions, achieving 95% success rates in first-attempt arterial access. Their training program includes virtual reality simulation before live procedures.
🇨🇦 Canada – Toronto General Hospital
Patient Safety: Implemented comprehensive infection prevention protocols for intraperitoneal catheter management, reducing peritonitis rates to 0.15 episodes per patient-year, well below international benchmarks.
🇦🇺 Australia – Royal Melbourne Hospital
Education Excellence: Developed simulation-based training programs for intrapleural procedures, with mandatory annual competency assessments. Their program has achieved zero pneumothorax complications in the past 18 months.
🇬🇧 United Kingdom – NHS Innovation
Standardization: Created national guidelines for specialized parenteral routes that standardized equipment, techniques, and monitoring protocols across all NHS trusts. This initiative reduced inter-facility variation by 80%.
🎓 Key Takeaways for Nursing Success
Mastering specialized parenteral routes requires dedication to continuous learning, strict adherence to safety protocols, and commitment to evidence-based practice. Each route presents unique challenges and opportunities for improving patient outcomes through skilled nursing intervention.
Remember: Patient safety is paramount. When in doubt, consult with experienced colleagues, refer to institutional protocols, and prioritize patient wellbeing above all else. Your competence in these advanced skills can make the difference between life and death in critical situations.
This educational resource is designed to supplement, not replace, formal clinical training and institutional protocols. Always follow your facility’s specific guidelines and seek appropriate supervision when learning new procedures.
