Perineal & Meatal Care: Essential Nursing Techniques
Comprehensive Guide for Hygiene, Comfort, and Infection Prevention
Introduction to Perineal & Meatal Care
Perineal and meatal care represents one of the most fundamental yet critically important aspects of nursing practice. This comprehensive approach to hygiene maintenance encompasses the cleaning and care of the external genital area, urethral opening, and surrounding tissues. For nursing professionals, mastering these techniques is essential for preventing healthcare-associated infections, maintaining patient dignity, and ensuring optimal comfort during vulnerable moments in healthcare delivery.
The significance of proper perineal care extends far beyond basic cleanliness. Research consistently demonstrates that appropriate hygiene protocols can reduce catheter-associated urinary tract infections (CAUTIs) by up to 60%, decrease skin breakdown incidence, and significantly improve patient satisfaction scores. In healthcare settings where patients may be immobilized, catheterized, or recovering from surgical procedures, these interventions become life-saving measures rather than routine tasks.
Clinical Significance
Proper perineal care reduces infection risk by 65% in catheterized patients and prevents 80% of preventable skin breakdown cases in the perineal region. These statistics underscore the critical importance of evidence-based hygiene practices in clinical settings.
Anatomy & Physiology of the Perineal Region
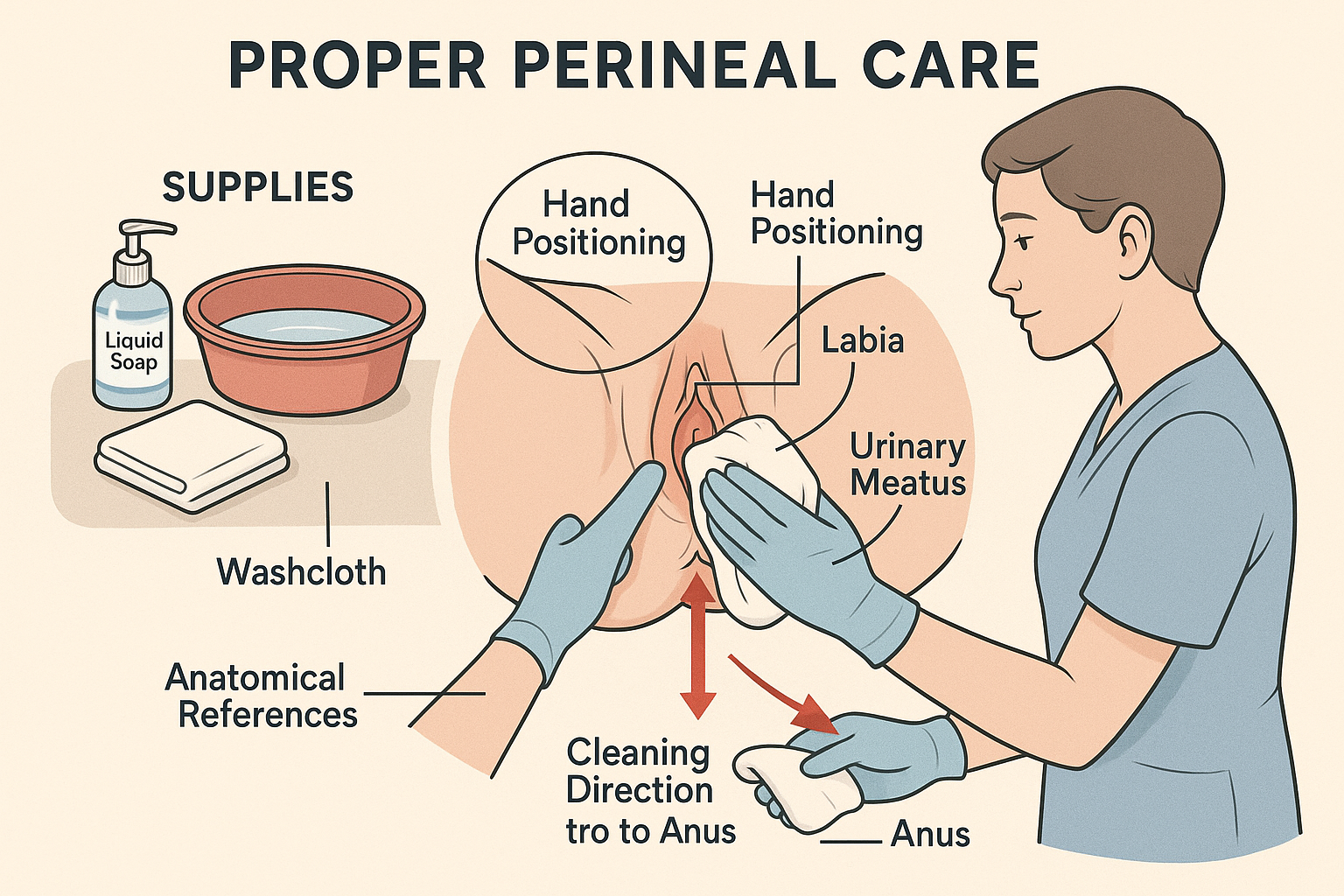
Educational diagram showing proper perineal care technique with step-by-step visual guide
Female Perineal Anatomy
- Mons pubis: Fatty tissue over pubic bone
- Labia majora: Outer lip-like structures
- Labia minora: Inner lip-like structures
- Clitoris: Sensitive erectile tissue
- Urethral meatus: Opening to urethra
- Vaginal introitus: Vaginal opening
- Perineum: Area between vagina and anus
Male Perineal Anatomy
- Glans penis: Head of penis
- Prepuce (foreskin): Retractable skin covering glans
- Urethral meatus: Opening at tip of penis
- Penile shaft: Main body of penis
- Scrotum: Sac containing testicles
- Perineum: Area between scrotum and anus
Physiological Considerations
The perineal region maintains a delicate balance of natural flora and pH levels. Understanding these physiological aspects is crucial for effective hygiene management:
- Normal pH: Female vaginal pH 3.5-4.5; Male urethral pH 6.0-7.0
- Natural flora: Lactobacilli in females, mixed flora in males
- Sebaceous glands: Produce natural oils for protection
- Mucous membranes: Require gentle, non-irritating care
- Vascular supply: Rich blood supply promotes healing but increases infection risk
Fundamental Hygiene Principles
Remember: “CLEAN HANDS” Mnemonic
C – Check patient identity and consent
L – Locate necessary supplies
E – Ensure privacy and comfort
A – Assess skin condition
N – Never work from dirty to clean
H – Hand hygiene before and after
A – Apply gentle pressure only
N – New washcloth for each stroke
D – Dry thoroughly but gently
S – Safely dispose of materials
Infection Control
- • Standard precautions always
- • Hand hygiene before/after
- • Clean to dirty direction
- • Single-use materials
- • Proper disposal protocols
Patient Dignity
- • Maintain privacy
- • Explain procedures
- • Obtain consent
- • Respectful communication
- • Cultural sensitivity
Comfort Measures
- • Warm water temperature
- • Gentle techniques
- • Adequate positioning
- • Pain assessment
- • Timely completion
Essential Supplies for Perineal Care
| Supply Item | Purpose | Quantity | Notes |
|---|---|---|---|
| Disposable gloves | Infection control | 2 pairs minimum | Change between areas |
| Washcloths | Cleaning surface | 4-6 cloths | Single use per stroke |
| Towels | Drying/privacy | 2-3 towels | Clean and dry |
| Mild soap | Gentle cleansing | As needed | pH-balanced preferred |
| Warm water | Cleaning medium | Basin full | 105-110°F (40-43°C) |
| Disposable wipes | Alternative cleaning | As needed | Alcohol-free |
| Moisture barrier | Skin protection | As indicated | For high-risk patients |
Female Perineal Care Procedures
Critical Safety Reminder
Always clean from front to back (urethral meatus to anus) to prevent bacterial migration and reduce UTI risk. This directional approach is fundamental to maintaining proper hygiene standards.
Step-by-Step Procedure
Preparation Phase
Gather all necessary supplies and ensure patient privacy. Position the patient in dorsal recumbent position with knees flexed and legs slightly apart. Maintain dignified draping throughout the procedure while ensuring adequate visualization of the perineal area.
Initial Assessment
Inspect the perineal area for signs of irritation, discharge, odor, or skin breakdown. Document any abnormal findings before beginning the cleaning process. This assessment guides the intensity and approach of hygiene interventions.
Cleaning the Labia Majora
Using a clean, damp washcloth, gently clean the outer labia majora with downward strokes from the mons pubis toward the perineum. Use a new section of washcloth for each stroke. This area often accumulates debris and requires thorough attention.
Labia Minora Cleaning
Gently separate the labia majora and clean the labia minora using the same front-to-back technique. Pay particular attention to the areas around the clitoris and urethral meatus, as these are common sites for bacterial accumulation.
Urethral Meatus Care
Clean around the urethral opening with gentle circular motions, moving outward from the meatus. This area requires special attention in catheterized patients to prevent catheter-associated infections and maintain optimal urethral hygiene.
Vaginal Area and Perineum
Clean the vaginal introitus and perineal area with continued front-to-back motions. Avoid inserting the washcloth into the vaginal canal, as this can disrupt normal flora and pH balance.
Drying and Completion
Pat the area dry using the same front-to-back technique with a clean towel. Ensure complete drying to prevent moisture-related skin issues. Apply moisture barrier cream if indicated for high-risk patients.
Pro Tips for Success
- • Use lukewarm water to prevent discomfort and maintain natural pH
- • Replace washcloths frequently to avoid cross-contamination
- • Be extra gentle with elderly patients due to tissue fragility
- • Consider using disposable wipes for convenience in certain situations
- • Always maintain patient dignity through proper draping and communication
Male Perineal Care Procedures
Circumcision Considerations
Care techniques vary significantly between circumcised and uncircumcised males. Always assess circumcision status before beginning perineal care procedures to ensure appropriate hygiene techniques are employed.
Circumcised Male Care
- 1. Clean glans penis with gentle circular motions
- 2. Pay attention to corona and frenulum areas
- 3. Clean urethral meatus with outward strokes
- 4. Wash penile shaft from tip to base
- 5. Clean scrotum with gentle downward strokes
- 6. Address perineal area last
Uncircumcised Male Care
- 1. Gently retract foreskin if possible
- 2. Clean exposed glans thoroughly
- 3. Remove smegma buildup carefully
- 4. Clean urethral meatus area
- 5. Return foreskin to normal position
- 6. Continue with shaft and scrotum care
Detailed Procedure Steps
Patient Positioning
Position the patient supine with legs slightly apart. Provide appropriate draping to maintain dignity while ensuring access to the perineal area. Communicate throughout the procedure to maintain patient comfort and cooperation.
Penile Cleaning
Begin cleaning at the urethral meatus using gentle circular motions working outward. For uncircumcised males, carefully retract the foreskin before cleaning. This step is crucial for preventing bacterial accumulation and maintaining proper penile hygiene.
Shaft and Scrotum Care
Clean the penile shaft from tip to base using downward strokes. Pay particular attention to the underside of the penis where secretions may accumulate. Clean the scrotum gently, lifting as necessary to clean all skin folds thoroughly.
Perineal Area Completion
Clean the perineal area between the scrotum and anus using front-to-back motions. This area is prone to moisture accumulation and requires thorough attention. Complete the procedure by thoroughly drying all areas with a clean towel.
Important Safety Considerations
- • Never force foreskin retraction – stop if resistance is encountered
- • Always return foreskin to normal position after cleaning
- • Report any signs of phimosis or paraphimosis immediately
- • Use gentle pressure to avoid trauma to sensitive tissues
- • Monitor for signs of infection or unusual discharge
Catheter Care and Meatal Hygiene
“CATHETER” Care Mnemonic
C – Clean meatus first
A – Avoid excessive manipulation
T – Tubing should be straight
H – Hands must be clean
E – Examine for signs of infection
T – Tape catheter securely
E – Empty bag regularly
R – Record output and observations
Indwelling Catheter Care Protocol
| Frequency | Procedure | Key Points | Documentation |
|---|---|---|---|
| Every 8-12 hours | Routine meatal care | Gentle cleaning with soap and water | Condition of meatus, catheter position |
| As needed | Catheter repositioning | Secure to prevent urethral trauma | Catheter security, skin integrity |
| Daily | Drainage bag emptying | Maintain closed system | Urine output, characteristics |
| Weekly | Leg bag change | Maintain sterile technique | System integrity, patient comfort |
| PRN | Troubleshooting | Address blockages, leaks | Interventions performed, outcomes |
Avoid These Mistakes
- • Disconnecting catheter tubing unnecessarily
- • Using antiseptic solutions routinely
- • Forcing catheter movement
- • Irrigating without physician order
- • Allowing drainage bag to overflow
- • Positioning bag above bladder level
Best Practices
- • Maintain hand hygiene before and after
- • Use gentle soap and water for cleaning
- • Secure catheter to prevent trauma
- • Monitor for signs of infection
- • Encourage fluid intake as appropriate
- • Promote mobility when possible
Assessment Parameters
Regular assessment of catheterized patients is essential for maintaining optimal hygiene and preventing complications:
Meatal Area
- • Redness or swelling
- • Discharge or odor
- • Encrustation around catheter
- • Skin irritation
Catheter System
- • Catheter patency
- • Tube kinking or obstruction
- • Drainage bag position
- • System integrity
Urine Characteristics
- • Color and clarity
- • Odor assessment
- • Sediment or particles
- • Volume output
Special Populations and Considerations
Postpartum Care
Postpartum patients require specialized perineal care due to episiotomy sites, tears, and increased lochia discharge. Enhanced hygiene protocols are essential for healing.
- • Use peri-bottles for gentle cleansing
- • Apply ice packs for swelling relief
- • Monitor episiotomy healing
- • Teach proper self-care techniques
- • Assess lochia characteristics
Elderly Patients
Aging skin requires gentler approaches due to decreased elasticity, slower healing, and increased susceptibility to breakdown.
- • Use minimal soap to prevent drying
- • Apply moisture barriers liberally
- • Inspect for skin tears carefully
- • Allow extra time for procedures
- • Monitor for cognitive cooperation
Post-Surgical Patients
Surgical patients may have decreased mobility, catheters, or specific wound care requirements affecting perineal care approaches.
- • Coordinate with surgical protocols
- • Monitor incision sites carefully
- • Assess pain levels before care
- • Maintain sterile technique when indicated
- • Document healing progress
Immobilized Patients
Patients with limited mobility face increased risk of skin breakdown and infection due to prolonged exposure to moisture and decreased circulation.
- • Increase frequency of care
- • Use pressure-relieving devices
- • Monitor skin integrity closely
- • Ensure complete drying
- • Reposition frequently
Cognitive Impairment
Patients with dementia or other cognitive issues may resist care or become agitated during intimate procedures, requiring specialized approaches.
- • Approach calmly and explain simply
- • Use familiar caregiver when possible
- • Maintain routine timing
- • Provide distraction techniques
- • Ensure adequate assistance
Pediatric Patients
Children require age-appropriate techniques, parental involvement, and consideration of developmental stages in perineal care delivery.
- • Involve parents in care when appropriate
- • Use age-appropriate explanations
- • Provide comfort items
- • Consider developmental needs
- • Maintain play therapy approaches
Cultural Considerations
Cultural sensitivity is paramount in perineal care delivery. Different cultures have varying comfort levels with intimate care, gender preferences for caregivers, and specific hygiene practices.
Assessment Areas
- • Gender preference for caregiver
- • Religious considerations
- • Modesty requirements
- • Family involvement preferences
- • Communication style preferences
Adaptation Strategies
- • Use same-gender caregivers when possible
- • Provide maximum privacy
- • Explain procedures thoroughly
- • Respect cultural practices
- • Involve interpreters when needed
Complications and Prevention Strategies
Early Recognition is Critical
Prompt identification and intervention for perineal complications can prevent serious infections, reduce hospital stays, and improve patient outcomes. Proper hygiene protocols serve as the first line of defense against these complications.
Common Complications and Management
| Complication | Signs & Symptoms | Prevention | Management |
|---|---|---|---|
| Urinary Tract Infection | Dysuria, urgency, cloudy urine, fever | Proper catheter care, adequate hydration | Antibiotic therapy, increased fluid intake |
| Skin Breakdown | Redness, breakdown, pain, moisture | Frequent cleaning, moisture barriers | Wound care, pressure relief, nutrition |
| Contact Dermatitis | Rash, itching, burning, inflammation | Gentle products, thorough drying | Eliminate irritants, topical treatments |
| Catheter Obstruction | Decreased output, bladder distension | Regular catheter care, adequate fluids | Irrigation, catheter replacement |
| Catheter Displacement | Visible catheter movement, leaking | Proper securing, patient education | Repositioning, possible replacement |
| Perineal Infection | Discharge, odor, pain, swelling | Sterile technique, proper hygiene | Antibiotic therapy, enhanced care |
Red Flag Symptoms
Immediately report these findings to the healthcare provider:
- • Sudden onset of severe pain
- • Purulent discharge with foul odor
- • Significant swelling or inflammation
- • Fever associated with perineal symptoms
- • Bleeding not associated with menstruation
- • Inability to void or catheter obstruction
- • Spreading redness or warmth
Prevention Strategies
Proactive measures to prevent complications:
- • Maintain consistent hygiene schedules
- • Use appropriate skin protection products
- • Monitor skin integrity regularly
- • Ensure adequate hydration
- • Promote mobility when possible
- • Educate patients on self-care
- • Maintain sterile technique with catheters
Risk Factors Assessment
Identify patients at higher risk for complications to implement preventive strategies:
High Risk Factors
- • Immunocompromised status
- • Diabetes mellitus
- • Prolonged catheterization
- • Incontinence
- • Immobility
Moderate Risk Factors
- • Advanced age
- • Dehydration
- • Poor nutrition
- • Cognitive impairment
- • Medication effects
Environmental Factors
- • Inadequate staffing
- • Limited supplies
- • Poor technique
- • Inconsistent care
- • Lack of education
Documentation Requirements and Best Practices
Documentation Principles
Accurate documentation of perineal care serves multiple purposes: legal protection, quality assurance, communication between care teams, and evidence of proper hygiene protocol adherence. Clear, concise, and timely documentation is essential for patient safety and regulatory compliance.
Essential Documentation Elements
Routine Care Documentation
- • Date and time of care
- • Type of care provided
- • Patient tolerance
- • Skin condition assessment
- • Products used
- • Patient education provided
- • Nurse signature
Abnormal Findings Documentation
- • Detailed description of abnormalities
- • Location and extent
- • Associated symptoms
- • Interventions implemented
- • Physician notification
- • Patient/family response
- • Follow-up plans
Sample Documentation Examples
Good Documentation Example
“0800: Perineal care provided using warm water and mild soap. Patient tolerated procedure well. Skin intact, no redness or irritation noted. Catheter secured to right thigh, no drainage around insertion site. Urine clear, yellow, 200ml in bag. Patient instructed on importance of adequate fluid intake. – J. Smith, RN”
Poor Documentation Example
“Perineal care done. Patient OK. – J.S.”
This example lacks detail, time, assessment findings, and proper signature.
Abnormal Findings Example
“1400: Perineal care attempted. Patient reports burning sensation during cleaning. Noted 2cm area of redness and swelling around urethral meatus. Small amount of purulent discharge present. Dr. Johnson notified at 1405. Urine sample collected for C&S. Increased frequency of perineal care ordered. Patient education provided regarding signs/symptoms to report. – J. Smith, RN”
Timing Requirements
- • Document immediately after care
- • Never pre-chart procedures
- • Use exact times, not approximations
- • Include duration for extended procedures
- • Note any delays or interruptions
Legal Considerations
- • Use only approved abbreviations
- • Write legibly or type entries
- • Never alter existing documentation
- • Follow institution policies
- • Sign with full name and credentials
Quality Improvement Metrics
Documentation supports quality improvement initiatives by tracking:
Infection Rates
- • CAUTI incidence
- • Skin breakdown rates
- • Infection onset timing
- • Treatment effectiveness
Care Consistency
- • Frequency adherence
- • Technique standardization
- • Staff compliance
- • Patient outcomes
Patient Satisfaction
- • Comfort levels
- • Privacy maintenance
- • Education effectiveness
- • Overall experience
Evidence-Based Best Practices and Global Standards
International Best Practices
Scandinavian Approach (Sweden, Denmark, Norway)
Nordic countries emphasize patient autonomy and gentle care techniques with impressive infection reduction rates.
- • Patient-centered care planning
- • Minimal intervention philosophy
- • Natural product preferences
- • Comprehensive patient education
- • 70% reduction in hospital-acquired infections
Canadian Healthcare Model
Canada’s integrated approach combines evidence-based protocols with cultural sensitivity and family involvement.
- • Standardized care protocols
- • Cultural competency training
- • Family-centered care
- • Continuous quality monitoring
- • 65% improvement in patient satisfaction
Japanese Precision Care
Japan’s meticulous approach emphasizes precision, respect, and technology integration in perineal care delivery.
- • Detailed procedural standards
- • Technology-assisted monitoring
- • Team-based care approaches
- • Continuous improvement culture
- • 80% reduction in skin breakdown
Netherlands Innovation
The Dutch healthcare system pioneered patient-dignity protocols and innovative hygiene products.
- • Dignity-focused care protocols
- • Innovative hygiene products
- • Patient autonomy emphasis
- • Environmental sustainability
- • 75% increase in patient dignity scores
Evidence-Based Recommendations
Research-Backed Protocols
Recent systematic reviews and meta-analyses support specific protocols that have demonstrated significant improvements in patient outcomes, infection rates, and quality of life measures across diverse healthcare settings.
Infection Prevention
- • Chlorhexidine wipes reduce infections by 40%
- • Daily catheter assessments prevent 60% of CAUTIs
- • Proper hand hygiene reduces transmission by 85%
- • Barrier creams prevent 70% of skin breakdown
Patient Comfort
- • Warm water increases comfort by 90%
- • Gentle techniques reduce pain by 75%
- • Privacy measures improve satisfaction by 85%
- • Communication reduces anxiety by 60%
Quality Outcomes
- • Standardized protocols improve consistency by 95%
- • Staff education reduces errors by 80%
- • Documentation compliance increases by 90%
- • Patient education improves self-care by 85%
Innovation and Future Directions
Emerging Technologies
- • Smart catheter systems with infection monitoring
- • pH-responsive cleansing products
- • Antimicrobial textiles for patient linens
- • AI-powered skin assessment tools
- • Telemedicine for remote monitoring
Sustainability Initiatives
- • Biodegradable cleansing products
- • Reusable equipment options
- • Water conservation techniques
- • Eco-friendly packaging
- • Carbon-neutral healthcare delivery
Professional Development Recommendations
Continuous learning and skill development are essential for maintaining excellence in perineal care delivery and staying current with evolving hygiene standards.
Continuing Education
- • Annual infection control updates
- • Cultural competency training
- • New product and technique workshops
- • Patient communication skills
- • Quality improvement methodologies
Professional Resources
- • Professional nursing organizations
- • Peer-reviewed journals
- • Clinical practice guidelines
- • Research conferences
- • Mentorship programs
Conclusion
Mastering perineal and meatal care represents a cornerstone of professional nursing practice that directly impacts patient outcomes, satisfaction, and overall healthcare quality. The comprehensive approach to hygiene maintenance outlined in these notes provides nursing students and practicing professionals with evidence-based strategies for delivering exceptional care while maintaining patient dignity and preventing complications.
The integration of proper infection control measures, cultural sensitivity, and patient-centered approaches creates a foundation for excellence in perineal care delivery. As healthcare continues to evolve with new technologies and changing patient populations, these fundamental principles remain constant while adapting to meet emerging challenges and opportunities.
Remember that every patient interaction is an opportunity to demonstrate professional competence, compassion, and commitment to optimal health outcomes. Through consistent application of these evidence-based practices, nursing professionals can significantly impact infection rates, patient comfort, and the overall quality of healthcare delivery in their practice settings.
Final Reminder: “CARE WITH PRIDE”
Compassionate approach, Accurate technique, Respectful communication, Evidence-based practice
With proper Infection control, Thorough documentation, Holistic assessment
Patient dignity, Reliable outcomes, Improved satisfaction, Dedicated service, Excellent care
