Pertussis (Whooping Cough)
Comprehensive Nursing Notes for Nursing Students
Table of Contents
Introduction to Pertussis
Pertussis (whooping cough) is a highly contagious acute respiratory infection caused by the gram-negative bacterium Bordetella pertussis. It remains one of the most common vaccine-preventable diseases in children under 5 years of age. The disease is characterized by its distinctive paroxysmal cough with an inspiratory “whoop,” which gives the disease its common name.
Key Facts about Pertussis:
- First identified in the 16th century
- Bordetella pertussis was isolated in 1906 by Jules Bordet and Octave Gengou
- Before vaccination, more than 200,000 cases were reported annually in the United States
- Despite vaccination, pertussis remains a significant cause of morbidity and mortality in infants
- Pertussis is reportable to public health authorities in the United States
Image: Pertussis (Whooping Cough) Overview – Source: Nurseslabs
Pathophysiology
Understanding the pathophysiology of pertussis is crucial for nursing assessment and management. The disease is primarily a toxin-mediated process affecting the respiratory tract.
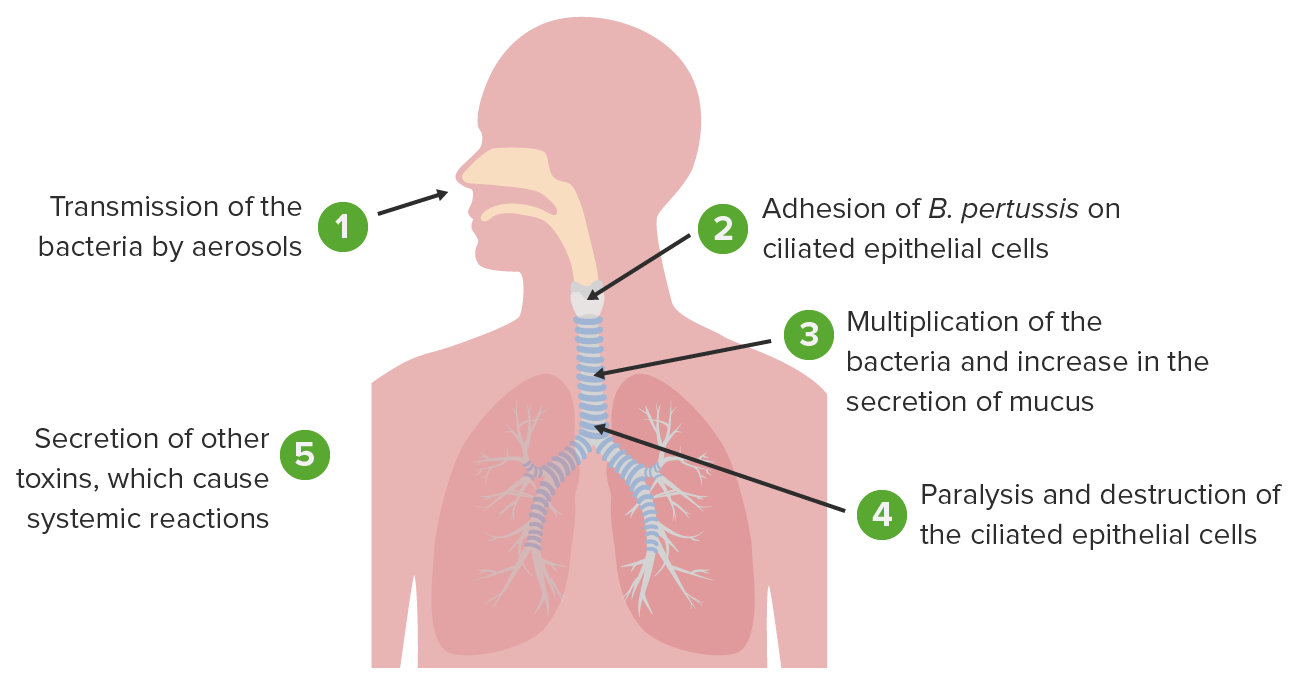
Image: Bordetella pertussis pathophysiology – Source: Lecturio
Causative Agent and Transmission
- Causative Agent: Bordetella pertussis, a gram-negative pleomorphic bacillus
- Reservoir: Humans are the sole reservoir for B. pertussis
- Transmission: Spread via aerosolized droplets produced by the cough of infected individuals or by direct face-to-face contact
- Highly Contagious: Secondary attack rates of 80% among susceptible household contacts
Disease Process
- Attachment: B. pertussis attaches to the cilia of respiratory epithelial cells, primarily in the bronchi and bronchioles
- Toxin Production: The bacteria produce multiple biologically active products:
- Pertussis toxin (PT)
- Filamentous hemagglutinin (FHA)
- Agglutinogens
- Adenylate cyclase
- Pertactin
- Tracheal cytotoxin
- Ciliary Paralysis: Toxins paralyze the cilia of respiratory epithelium
- Inflammation: Causes inflammation of the respiratory tract
- Exudate Formation: A mucopurulent sanguineous exudate forms in the respiratory tract
- Airway Compromise: Exudate compromises small airways, leading to atelectasis, cough, cyanosis, and pneumonia
- Immune Evasion: Pertussis antigens allow the organism to evade host defenses – lymphocytosis is promoted but chemotaxis is impaired
Clinical Relevance: The pathophysiology explains the characteristic persistent paroxysmal cough. The cilia, which normally clear mucus from the airways, are paralyzed by pertussis toxin, leading to mucus accumulation and the classic whooping cough as patients struggle to clear airways against this obstruction.
Clinical Manifestations
Pertussis has a typical incubation period of 7-10 days (range: 4-21 days). The clinical course is classically divided into three stages, each with distinctive features.
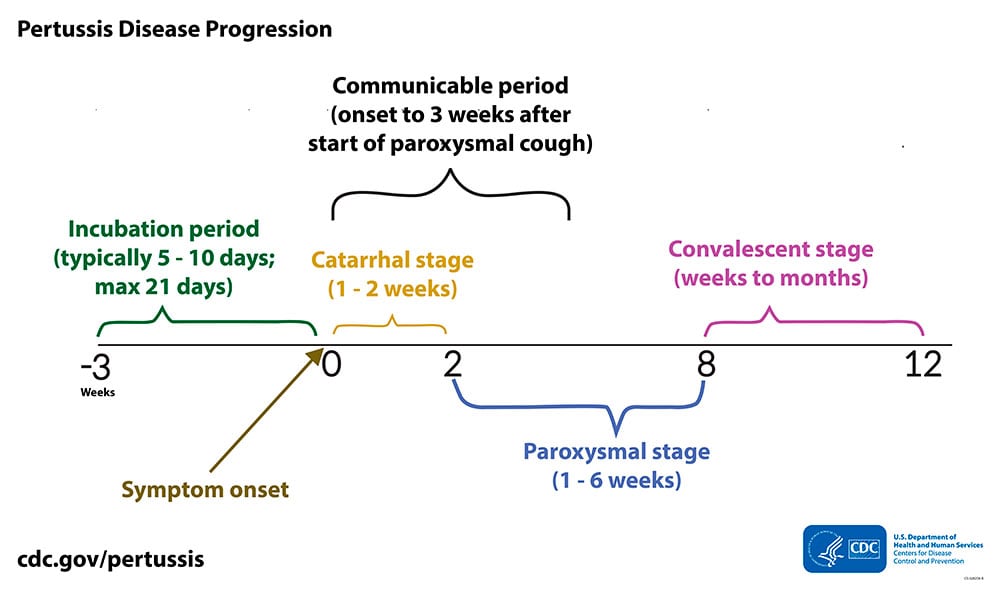
Image: Clinical course of pertussis – Source: CDC
Stage 1: Catarrhal Phase
Duration: 1-2 weeks
- Mild, cold-like symptoms
- Nasal congestion
- Rhinorrhea (runny nose)
- Sneezing
- Low-grade fever
- Mild, occasional cough
- Most infectious period
Stage 2: Paroxysmal Phase
Duration: 1-6 weeks
- Distinctive paroxysmal coughing
- Forceful, rapid coughs followed by inspiratory “whoop”
- Post-tussive vomiting
- Cyanosis during attacks
- Exhaustion following episodes
- Normal appearance between attacks
- Worse at night (avg. 15 attacks/24hrs)
Stage 3: Convalescent Phase
Duration: 2-3 weeks or longer
- Gradual recovery
- Decreasing frequency and severity of coughing episodes
- Cough becomes less paroxysmal
- Paroxysms may recur with subsequent respiratory infections for months
Special Considerations in Different Age Groups
| Age Group | Clinical Presentation | Nursing Considerations |
|---|---|---|
| Infants <6 months |
|
|
| Children |
|
|
| Adolescents & Adults |
|
|
| Previously Vaccinated |
|
|
Diagnosis and Assessment
Timely and accurate diagnosis of pertussis is essential for appropriate management and preventing transmission. Nursing assessment plays a critical role in identifying suspected cases.

Image: Algorithm for the diagnosis of pertussis – Source: ResearchGate
Nursing Assessment
Key Assessment Areas
- Airway patency: Maintaining a patent airway is always the first priority
- Respiratory assessment:
- Rate, depth, and pattern of respirations
- Work of breathing and use of accessory muscles
- Presence of nasal flaring
- Evidence of cyanosis (especially during coughing spells)
- Chest auscultation for normal or adventitious breath sounds
- Cough assessment:
- Character (paroxysmal, dry, productive)
- Presence of inspiratory “whoop”
- Frequency and duration of coughing episodes
- Triggers that initiate coughing spells
- Nutritional and hydration status:
- Frequency of posttussive vomiting
- Oral intake
- Urine output
- Weight changes
- Skin turgor and mucous membrane moisture
- Activity tolerance: Fatigue and exhaustion levels, especially after coughing episodes
Diagnostic Tests
| Diagnostic Test | Timing | Considerations |
|---|---|---|
| Culture (gold standard) | Early catarrhal and paroxysmal phases (first 2 weeks) |
|
| PCR (Polymerase Chain Reaction) | 0-3 weeks after cough onset (up to 4 weeks in unvaccinated) |
|
| Serology | 2-8 weeks after cough onset (up to 12 weeks) |
|
| WBC Count | Late catarrhal and paroxysmal phases |
|
| Chest X-ray | As indicated |
|
Nursing Implications for Diagnostic Testing:
- Explain procedures to patient/family in age-appropriate terms
- Proper specimen collection is critical for accurate results
- Support and comfort the child during nasopharyngeal swabbing (can trigger coughing)
- Document timing of symptom onset to guide test selection
- Implement isolation precautions while awaiting results
- Report suspected cases to public health authorities promptly
Complications
Pertussis can lead to serious complications, particularly in infants and young children. Understanding these complications guides nursing assessment and early intervention.
High-Risk Groups for Complications
- Infants <6 months of age: Highest risk group – account for 84% of pertussis deaths
- Unvaccinated or incompletely vaccinated children
- Individuals with chronic respiratory conditions
- Immunocompromised patients
Common Complications
| System | Complications | Nursing Assessment & Interventions |
|---|---|---|
| Respiratory |
|
|
| Neurological |
|
|
| Physical Trauma |
|
|
| Nutritional |
|
|
| Other |
|
|
Critical Nursing Point: Infants with pertussis may present with apnea or life-threatening events rather than typical coughing paroxysms. Respiratory monitoring is essential, and hospitalization should be considered for infants under 6 months of age with confirmed or suspected pertussis.
Medical Management
Medical management of pertussis consists of antimicrobial therapy, supportive care, and management of complications. The effectiveness of treatment is largely dependent on early initiation.
Antimicrobial Therapy
Timing is Critical: Antibiotics are most effective when started during the catarrhal stage or early paroxysmal stage (first 1-2 weeks of illness). Treatment after this period may not alter the clinical course but is still recommended to reduce communicability.
| Antibiotic | Age Group | Dosage & Duration | Special Considerations |
|---|---|---|---|
| Azithromycin (First-line) |
|
|
|
| Clarithromycin |
|
|
|
| Erythromycin |
|
|
|
| Trimethoprim-Sulfamethoxazole |
|
|
|
Supportive Care
Respiratory Support
- Oxygen therapy as needed to maintain adequate saturation
- Suctioning to clear secretions
- Hospitalization for severe cases or at-risk patients
- Mechanical ventilation may be required in severe cases
- Monitoring of respiratory status
Nutritional & Fluid Support
- Small, frequent feedings to reduce post-tussive vomiting
- IV fluids for dehydration or inability to maintain oral intake
- Nasogastric feeding may be needed for severe cases
- Monitoring of weight and nutritional status
Considerations for Hospitalization
Indications for Hospital Admission
- Infants <6 months of age with suspected or confirmed pertussis
- Patients with severe respiratory distress or cyanosis during paroxysms
- Inability to maintain adequate hydration or nutrition
- Presence of significant complications (pneumonia, seizures, encephalopathy)
- Apneic episodes
- Significant hypoxemia or respiratory failure
- Patients with pre-existing conditions that increase risk (prematurity, cardiac disease, pulmonary disease, immunodeficiency)
Evidence-Based Care Note: Cough suppressants, antihistamines, and bronchodilators are generally not effective for pertussis and should be avoided. The cough in pertussis is due to toxin effects on the respiratory epithelium, not histamine release or bronchospasm.
Nursing Management
Nursing management of pertussis focuses on respiratory support, monitoring for complications, education, and infection control. Care differs based on the setting (hospital vs. home).
Hospital Nursing Management
Respiratory Management
- Airway maintenance:
- Position patient to optimize respiratory function (e.g., Head of bed elevated 30-45°)
- Suction airway as needed to remove secretions
- Provide oxygen support as prescribed
- Coughing support:
- Teach optimal coughing techniques and positioning
- Show how to use pillow or hand splints during coughing episodes
- Guide in using abdominal muscles for more effective cough
- Monitoring:
- Continuous or frequent assessment of respiratory rate, effort, and pattern
- Pulse oximetry monitoring
- Monitor for signs of respiratory distress or fatigue
- Document frequency, duration, and severity of coughing episodes
Nutrition and Hydration
- Fluid intake:
- Encourage oral fluids when tolerated
- Administer IV fluids as prescribed
- Monitor intake and output
- Feeding strategies:
- Small, frequent feedings rather than large meals
- Feed after coughing episodes, when child is more relaxed
- Schedule meals to avoid times when coughing is typically worse
- Position upright during and after feeding
- Assessment:
- Monitor weight daily
- Assess skin turgor and mucous membranes
- Track frequency of vomiting episodes
Infection Control
- Isolation precautions:
- Droplet precautions until 5 days of appropriate antibiotic therapy completed
- Private room when possible
- Masks for healthcare workers and visitors
- Staff/visitor restrictions:
- Restrict non-essential personnel
- Screen visitors for symptoms and vaccination status
- Be especially cautious with pregnant visitors (last trimester) and infants
- Environmental controls:
- Proper disposal of tissues and contaminated items
- Regular cleaning of surfaces
- Hand hygiene education and enforcement
Medication Administration & Monitoring
- Antibiotic administration:
- Administer as prescribed, at correct times
- Monitor for side effects (especially GI symptoms with macrolides)
- For infants <1 month on macrolides, monitor for IHPS symptoms
- Other medications:
- Antipyretics for fever as needed
- Administration of any pre-existing medications
- Avoid cough suppressants (generally ineffective)
- Therapeutic response monitoring:
- Track changes in cough frequency and severity
- Document response to all medications
- Monitor for signs of complications
Home Nursing Management
Patient/Family Education
- Disease information:
- Explain the stages and typical course of pertussis
- Discuss expected duration of symptoms
- Explain that cough may persist for weeks to months
- Medication management:
- Importance of completing the full course of antibiotics
- Administration techniques for children
- Potential side effects and when to report them
- Home care instructions:
- Coughing techniques and positioning
- Creating a calm environment (stress can trigger coughing)
- Room humidification
- Avoiding irritants (tobacco smoke, strong odors)
- Warning signs:
- Signs of respiratory distress requiring emergency care
- Indicators of dehydration
- Signs of secondary infections or complications
Home Care Strategies
- Environmental modifications:
- Maintain adequate room humidity
- Ensure good ventilation
- Remove environmental irritants
- Keep air temperature moderate
- Comfort measures:
- Rest periods throughout the day
- Quiet activities to reduce coughing triggers
- Supportive positioning during sleep
- Gentle back rubs and relaxation techniques
- Family support:
- Respite care suggestions
- Strategies for managing other children’s needs
- Coping mechanisms for prolonged illness
- Community resources and support
- Return to school/daycare guidance:
- Timing (after 5 days of appropriate antibiotics)
- Communication with school nurses/staff
- Gradual return if fatigue is an issue
Critical Nursing Interventions for Paroxysmal Episodes:
- Stay with the child during coughing paroxysms
- Maintain a calm presence
- Support the child in an upright position
- Have suction equipment ready if available
- Provide tissues for secretions
- Offer small sips of water after episode subsides
- Document frequency, duration, and severity of episodes
Prevention and Control
Prevention of pertussis revolves around vaccination, prompt treatment of cases, and prophylaxis for contacts. Nurses play a crucial role in all aspects of prevention.

Image: CDC pertussis case classification flowchart – Source: ResearchGate
Vaccination Recommendations
Vaccination Schedule
| Age Group | Vaccine | Schedule |
|---|---|---|
| Infants & Children | DTaP |
|
| Adolescents | Tdap |
|
| Adults | Tdap |
|
| Pregnant Women | Tdap |
|
| Healthcare Workers | Tdap |
|
Cocoon Strategy: A “cocoon” of protection can be created around vulnerable infants by ensuring all close contacts (parents, siblings, grandparents, childcare providers) are vaccinated against pertussis.
Post-Exposure Prophylaxis (PEP)
PEP Recommendations
- Who should receive PEP:
- All household contacts of a pertussis case
- Close contacts at high risk for severe disease (infants, pregnant women in third trimester)
- Individuals who will have contact with high-risk persons
- Healthcare workers with direct exposure to respiratory secretions
- Timing: As soon as possible after exposure
- Medications: Same antibiotics and dosing as for treatment (azithromycin, clarithromycin, erythromycin, or TMP-SMX)
- Vaccination: Incomplete or unvaccinated contacts should be brought up to date with pertussis-containing vaccines
Infection Control Measures
Healthcare Settings
- Isolation:
- Droplet precautions
- Private room when possible
- Continue until 5 days of appropriate antibiotics completed
- Personal protective equipment:
- Masks for all entering room
- Gloves for contact with respiratory secretions
- Gowns if significant contamination risk
- Healthcare worker exposures:
- Provide PEP to exposed staff
- Consider furlough for unprotected exposed staff who work with high-risk patients
- Maintain vaccination records of all staff
- Environmental cleaning:
- Routine cleaning of surfaces
- Proper disposal of contaminated materials
Community Settings
- Home isolation:
- Patients should stay home from school, work, and public places until completing 5 days of appropriate antibiotics
- If untreated, isolation for 21 days after cough onset
- School/daycare settings:
- Notification of potential exposures
- Exclusion of cases until properly treated
- PEP for high-risk contacts
- Consider prophylaxis for classroom contacts in outbreak situations
- Public health reporting:
- Report all suspected cases to local public health department
- Participate in contact investigations
- Follow health department guidance for outbreak control
- General prevention education:
- Cover coughs and sneezes
- Proper hand hygiene
- Avoiding close contact with symptomatic individuals
- Staying up to date on vaccinations
Nursing Care Plan for Pertussis
The nursing care plan for a patient with pertussis focuses on key nursing diagnoses related to respiratory function, nutrition, prevention of spread, and family education.

Image: Pertussis nursing care – Source: NurseStudy.Net
Nursing Diagnosis 1: Ineffective Airway Clearance
Related to: Copious and tenacious bronchial secretions, paroxysmal coughing
Expected Outcomes:
- Patient will maintain clear, open airways as evidenced by normal breath sounds, normal rate and depth of respirations
- Patient will effectively cough up secretions after treatments and deep breaths
- Patient will demonstrate increased air exchange
Nursing Interventions:
- Assess respiratory status:
- Monitor respiratory rate, pattern, depth, and effort
- Auscultate lungs for adventitious sounds
- Assess for signs of respiratory distress
- Monitor oxygen saturation
- Promote effective coughing:
- Teach optimal positioning (sitting position)
- Demonstrate use of pillow or hand splints when coughing
- Guide in use of abdominal muscles for more forceful cough
- Teach quad and huff techniques as age-appropriate
- Maintain adequate hydration:
- Encourage oral fluid intake to 3 liters per day (if appropriate)
- Administer IV fluids as prescribed
- Monitor intake and output
- Provide supportive respiratory care:
- Position for optimal respiratory function
- Provide humidified oxygen as prescribed
- Perform chest physiotherapy if ordered
- Suction as needed to clear secretions
- Administer medications:
- Antibiotics as prescribed
- Evaluate effectiveness and monitor for side effects
Evaluation:
- Patient maintains respiratory rate within normal limits for age
- Breath sounds are clear or improving
- Patient demonstrates effective coughing technique
- Oxygen saturation remains within normal parameters
- Frequency and severity of coughing paroxysms decrease over time
Nursing Diagnosis 2: Risk for Deficient Fluid Volume
Related to: Frequent vomiting after coughing paroxysms, increased insensible losses due to tachypnea, decreased oral intake due to fatigue
Expected Outcomes:
- Patient will maintain adequate hydration as evidenced by moist mucous membranes, good skin turgor, and age-appropriate urine output
- Patient will consume/receive adequate fluid intake for age and condition
- Patient will maintain stable weight
Nursing Interventions:
- Monitor hydration status:
- Assess skin turgor, mucous membranes, fontanels (in infants)
- Monitor vital signs for indicators of dehydration
- Track intake and output
- Monitor urine specific gravity if indicated
- Promote oral hydration:
- Offer small amounts of fluids frequently
- Provide preferred fluids when possible
- Schedule fluid intake after coughing episodes
- Use age-appropriate fluid delivery methods
- Manage vomiting:
- Position to minimize aspiration risk during vomiting
- Clean mouth after vomiting episodes
- Replace fluids and electrolytes lost through vomiting
- Document frequency and amount of emesis
- Administer IV therapy as prescribed:
- Maintain patent IV access
- Administer fluids at prescribed rate
- Monitor for signs of fluid overload
- Monitor nutritional status:
- Weigh daily at same time, same scale, similar clothing
- Document caloric intake
- Consult with dietitian as needed
Evaluation:
- Patient maintains adequate hydration as evidenced by moist mucous membranes and good skin turgor
- Urine output remains within normal parameters for age
- Weight remains stable or returns to baseline
- No signs of dehydration present
Nursing Diagnosis 3: Risk for Infection Transmission
Related to: Presence of communicable disease, aerosolized respiratory droplets during coughing
Expected Outcomes:
- Patient/family will demonstrate understanding of infection control measures
- Transmission to others will be prevented
- Patient/family will verbalize understanding of isolation period requirements
Nursing Interventions:
- Implement isolation precautions:
- Maintain droplet precautions until 5 days of appropriate antibiotic therapy completed
- Use private room when possible
- Ensure all healthcare workers and visitors wear appropriate PPE
- Limit visitors, especially those at high risk
- Educate about disease transmission:
- Teach proper cough etiquette (cover mouth and nose)
- Demonstrate proper hand hygiene technique
- Explain importance of completing full course of antibiotics
- Discuss isolation period requirements
- Coordinate post-exposure prophylaxis:
- Identify close contacts who need prophylaxis
- Provide information about antibiotic regimens
- Facilitate communication with healthcare providers for contacts
- Promote vaccination:
- Assess vaccination status of family members
- Educate about importance of pertussis vaccines
- Facilitate referrals for vaccination as needed
Evaluation:
- Patient/family demonstrates proper infection control techniques
- Close contacts receive appropriate prophylaxis as indicated
- Family verbalizes understanding of isolation requirements and complies with recommendations
- No secondary cases occur among close contacts
Nursing Diagnosis 4: Anxiety (Patient/Family)
Related to: Unpredictable and distressing nature of coughing paroxysms, prolonged illness course, concerns about complications
Expected Outcomes:
- Patient/family will verbalize decreased anxiety
- Patient/family will demonstrate effective coping strategies
- Patient/family will express understanding of disease course and expectations
Nursing Interventions:
- Provide anticipatory guidance:
- Explain typical disease progression
- Prepare family for paroxysmal episodes
- Discuss expected duration of symptoms
- Address common concerns and misconceptions
- Teach coping strategies:
- Demonstrate techniques to support child during coughing episodes
- Suggest ways to create calm environment
- Discuss importance of adequate rest for caregivers
- Encourage expression of feelings and concerns
- Provide supportive presence:
- Remain with patient/family during severe episodes
- Offer reassurance and accurate information
- Listen to concerns and validate feelings
- Maintain calm, confident demeanor
- Connect to resources:
- Provide information about support groups
- Identify community resources
- Consider referral for respite care if needed
- Offer educational materials
Evaluation:
- Patient/family verbalizes decreased anxiety
- Patient/family demonstrates effective management of coughing episodes
- Patient/family expresses realistic understanding of disease course
- Patient/family utilizes appropriate coping strategies
Documentation Guidelines for Pertussis:
- Individual assessment findings, including respiratory status and coughing patterns
- Frequency, duration, and severity of coughing paroxysms
- Presence of post-tussive vomiting or cyanosis
- Intake and output measurements
- Responses to interventions and treatments
- Educational topics covered and family’s understanding
- Isolation precautions implemented
- Communication with healthcare team and public health authorities
- Attainment or progress toward expected outcomes
References
- Centers for Disease Control and Prevention. (2024). Pertussis (Whooping Cough): Clinical overview. https://www.cdc.gov/pertussis/hcp/clinical-overview/index.html
- Centers for Disease Control and Prevention. (2024). Treatment of Pertussis. https://www.cdc.gov/pertussis/hcp/clinical-care/index.html
- Centers for Disease Control and Prevention. (2024). Chapter 16: Pertussis | Pink Book. https://www.cdc.gov/pinkbook/hcp/table-of-contents/chapter-16-pertussis.html
- Nurseslabs. (2023). Pertussis (Whooping Cough) – Nurseslabs. https://nurseslabs.com/pertussis-whooping-cough/
- Havers, F.P., Moro, P.L., Hariri, S., & Skoff, T. (2023). Pertussis. In Centers for Disease Control and Prevention, Pink Book.
- Kilgore, P.E., Salim, A.M., & Zervos, M.J. (2016). Pertussis: Microbiology, disease, treatment, and prevention. Clinical Microbiology Reviews, 29(3), 449-486.
- American Academy of Pediatrics. (2018). Pertussis. In D. Kimberlin, M. Brady, M. Jackson, & S. Long (Eds.), Red Book: 2018 Report of the Committee on Infectious Diseases (31st ed., pp. 620-634). Itasca, IL: American Academy of Pediatrics.
- Spratling, R., & Carmon, M. (2010). Pertussis: An overview of the disease, immunization, and trends for nurses. Pediatric Nursing, 36, 239-243.
