Placental Separation and Expulsion
Comprehensive Guide for Nursing Students
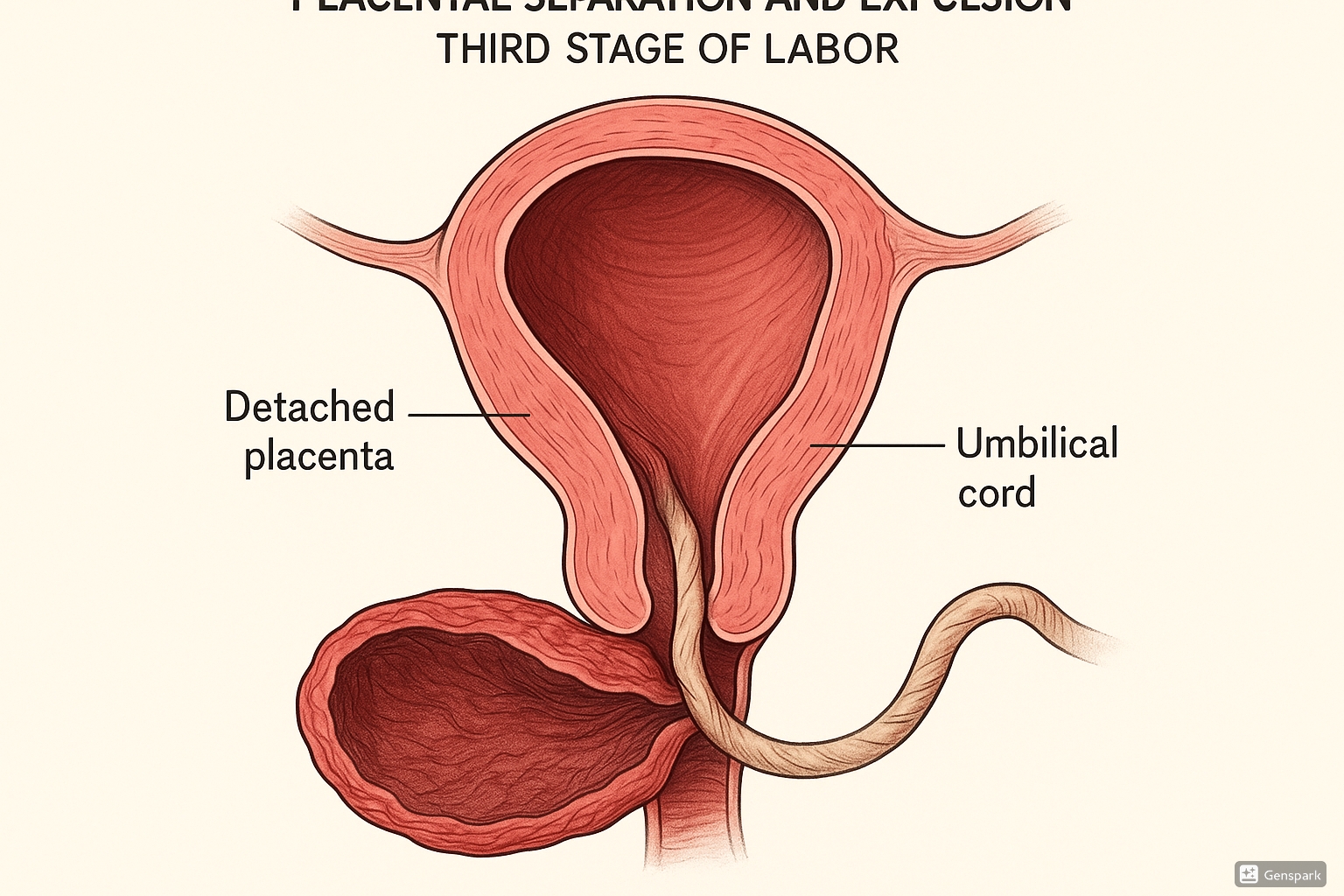
Medical illustration of placental separation and expulsion during third stage of labor
Table of Contents
Introduction to Placental Separation
The third stage of labor begins after the delivery of the baby and ends with the delivery of the placenta. This stage involves two crucial physiological processes: placental separation and expulsion. Understanding the physiology behind these processes is essential for nursing professionals to provide optimal care and prevent complications.
Key Concept: The third stage of labor typically lasts 5-15 minutes but can extend up to 30 minutes in physiological management. A third stage lasting longer than 30 minutes is considered prolonged and may require intervention.
Physiology of Placental Separation
Placental separation is initiated by myometrial contractions following the birth of the baby. These contractions cause the uterus to decrease in size, reducing the surface area where the placenta is attached. This reduction creates shearing forces at the decidua-placental interface.
The Separation Process
Separation occurs at the decidua basalis layer, specifically at the spongy layer. The physiological mechanism involves:
| Process | Description | Physiological Significance |
|---|---|---|
| Myometrial Contraction | Uterine muscles contract, reducing placental site surface area | Creates shearing forces at the placental-decidual interface |
| Cleavage Formation | Separation occurs through spongy layer of decidua basalis | Leaves some decidua attached to maternal surface of placenta |
| Retroplacental Hematoma | Blood accumulates between separated placenta and uterine wall | May aid in complete placental separation |
| Vascular Changes | Thrombosis of uteroplacental vessels | Helps prevent excessive bleeding during separation |
Memory Aid: “The DISC Method”
Decidual layer separation
Interface at spongy layer
Shearing forces from contractions
Clevage formation completes separation
Mechanisms of Placental Expulsion
After separation, the placenta must be expelled from the uterus. There are two primary mechanisms of placental expulsion:
Schultz Mechanism
The placenta separates from the center first, with the fetal surface (shiny, gray) presenting first. Blood is trapped behind the membranes, giving a “shiny” appearance. This mechanism occurs in approximately 80% of births.
Matthews Duncan Mechanism
The placenta separates from the periphery first, with the maternal surface (rough, red) presenting first. Blood can escape as separation occurs, potentially resulting in higher blood loss. This mechanism occurs in approximately 20% of births.
Memory Aid: “S-F-S and D-M-R”
Schultz – Fetal surface first – Shiny appearance
Duncan – Maternal surface first – Rough appearance
Homeostasis During Third Stage
Maintaining homeostasis during placental separation is crucial to prevent excessive blood loss. The body employs several mechanisms to ensure hemostasis:
Physiological Hemostasis
| Mechanism | Process | Nursing Implications |
|---|---|---|
| Myometrial Contraction | Uterine muscles contract around blood vessels (living ligatures) | Monitor uterine tone; encourage breastfeeding to stimulate oxytocin |
| Coagulation Cascade | Activation of clotting factors at placental site | Monitor for signs of coagulopathy; assess bleeding pattern |
| Oblique Muscle Fibers | “Living ligatures” compress blood vessels | Assess fundal firmness regularly |
| Hormonal Influence | Oxytocin release causes uterine contraction | Facilitate skin-to-skin contact and early breastfeeding |
Key Concept: During physiological placental separation, the average blood loss is approximately 500ml or less. The body compensates for this normal blood loss through increased cardiac output and fluid shifts from the extravascular to intravascular space.
Hormonal Changes
Several hormones play critical roles in maintaining homeostasis during the third stage:
- Oxytocin: Primary hormone responsible for uterine contractions, released through nipple stimulation during breastfeeding
- Prostaglandins: Enhance uterine contractions and promote vasoconstriction
- Catecholamines: Released during stress, can inhibit oxytocin release and potentially prolong the third stage
Memory Aid: “OPC for Homeostasis”
Oxytocin makes the uterus contract
Prostaglandins enhance contractions
Catecholamines (stress hormones) can inhibit the process
Physiological Management of Third Stage
Physiological (expectant) management of the third stage allows placental separation and expulsion to occur with minimal intervention. This approach relies on the body’s natural mechanisms and includes:
| Component | Action | Rationale |
|---|---|---|
| Delayed Cord Clamping | Wait at least 1-3 minutes before clamping the cord | Increases neonatal blood volume and iron stores |
| Skin-to-Skin Contact | Place baby on mother’s chest immediately after birth | Stimulates oxytocin release through touch and breastfeeding |
| Gravity and Position | Upright maternal position | Uses gravity to aid placental descent |
| Watchful Waiting | Observe for signs of separation | Allows natural separation process to occur |
| Maternal Effort | Mother pushes when urge is felt | Uses natural expulsive reflexes |
Signs of Placental Separation
Nurses should be vigilant for these signs indicating placental separation has occurred:
- Cord Lengthening: The umbilical cord appears to lengthen as the placenta descends into the lower uterine segment
- Gush of Blood: Small gush of blood as the placenta separates from the uterine wall
- Uterine Rise: The uterus rises upward in the abdomen as the placenta moves downward
- Uterine Shape Change: The uterus becomes globular and firmer
Memory Aid: “CLUG Signs”
Cord lengthening
Leakage of blood
Uterine rise
Globular shape change
Best Practices & Recent Updates
Best Practice #1: Delayed Cord Clamping
Current evidence supports delaying cord clamping for at least 1-3 minutes in term infants and up to 60 seconds in preterm infants, when possible. This practice has been shown to improve neonatal iron stores for up to six months after birth and reduce the risk of iron deficiency anemia. This is now recommended by WHO, ACOG, and Royal College of Midwives for both term and preterm infants when immediate resuscitation isn’t required.
Best Practice #2: Skin-to-Skin Contact
Immediate and uninterrupted skin-to-skin contact between mother and baby during the third stage promotes physiological placental separation through natural oxytocin release. Recent research indicates that this practice not only facilitates third stage labor but also improves neonatal adaptation, stabilizes vital signs, and promotes successful initiation of breastfeeding.
Best Practice #3: Individualized Third Stage Management
Current evidence supports an individualized approach to third stage management based on risk assessment. While active management (with uterotonics) remains standard in many settings, physiological management may be appropriate for low-risk women who prefer this approach. Hybrid approaches are gaining recognition, combining elements of both methods such as delayed cord clamping with oxytocin administration after placental delivery.
Complications & Nursing Interventions
Despite physiological mechanisms ensuring successful placental separation and expulsion, complications can occur. Nurses should be prepared to identify and manage these situations:
| Complication | Signs/Symptoms | Nursing Interventions |
|---|---|---|
| Retained Placenta | No signs of separation after 30 minutes; incomplete delivery of placenta | Monitor vital signs; prepare for manual removal; anticipate oxytocic medication |
| Postpartum Hemorrhage | Blood loss >500mL; continued heavy bleeding; uterine atony | Fundal massage; initiate emergency protocols; administer uterotonics as ordered |
| Placenta Accreta Spectrum | Placenta fails to separate due to abnormal attachment | Anticipate surgical intervention; prepare for potential massive transfusion |
| Uterine Inversion | Uterus turns inside out; severe pain; hemorrhage | Immediate recognition; call for help; attempt manual replacement; fluid resuscitation |
Key Concept: The most common cause of postpartum hemorrhage is uterine atony, which occurs when the uterus fails to contract adequately after placental separation. Prompt recognition and treatment are essential to prevent complications.
Memory Aid: “The 4 Ts of Hemorrhage”
Tone: Uterine atony (most common)
Tissue: Retained placental tissue
Trauma: Lacerations, hematomas
Thrombin: Coagulation disorders
Summary
Understanding the physiological processes of placental separation and expulsion is essential for nursing care during the third stage of labor. By recognizing normal mechanisms, maintaining homeostasis, and implementing evidence-based practices, nurses can facilitate a safe transition through this critical period while being prepared to identify and respond to potential complications.
Remember: The key to successful management of placental separation is allowing physiological processes to occur while maintaining vigilant observation for deviations from normal patterns that may indicate complications requiring intervention.
