PNEUMONIA
Comprehensive Nursing Notes
Table of Contents
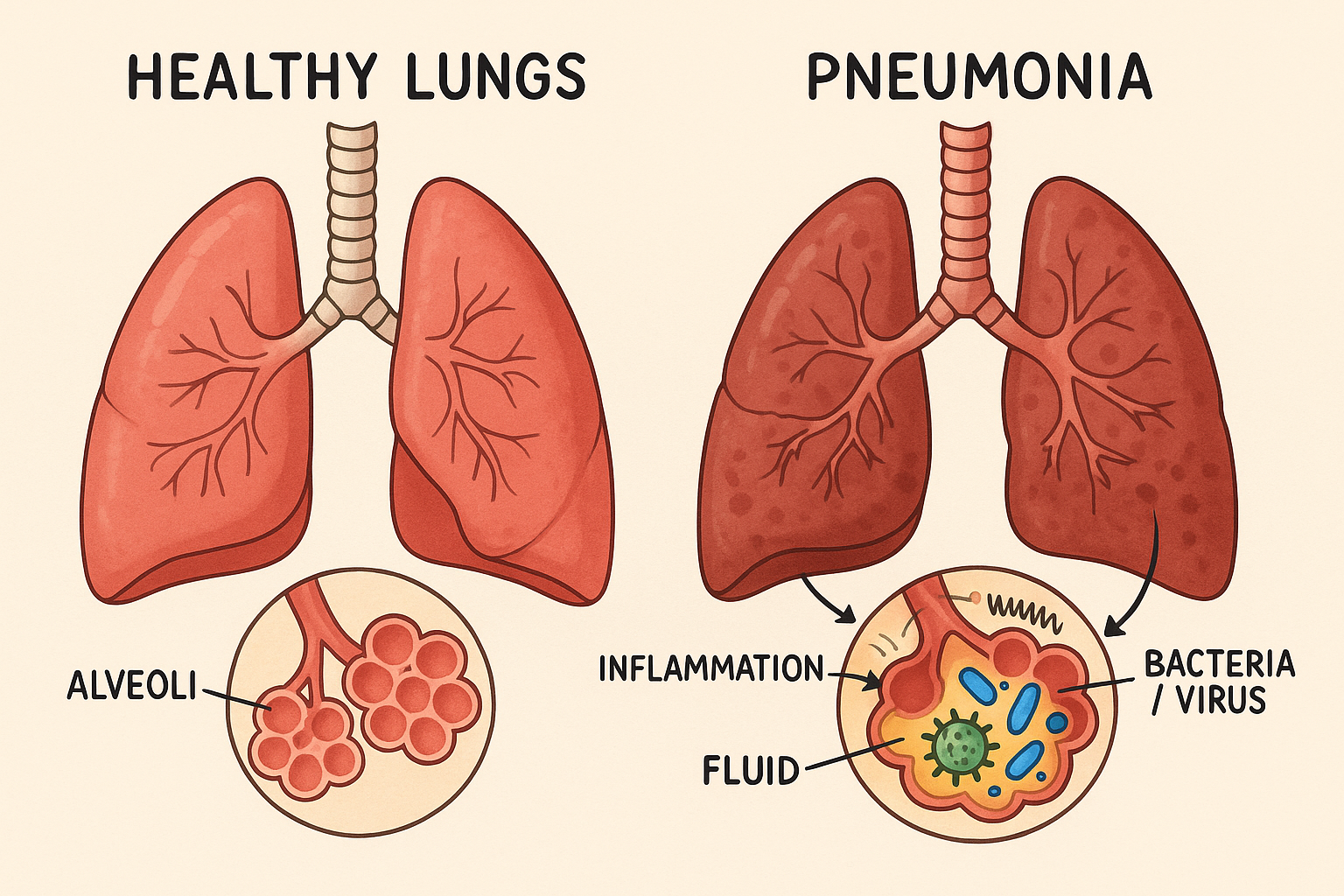
Figure 1: Anatomical comparison between healthy lungs and pneumonia-affected lungs showing inflammation and fluid accumulation
Definition
Key Definition
Pneumonia is an acute inflammatory condition of the lung parenchyma, specifically affecting the alveoli and terminal bronchioles. It is characterized by consolidation of lung tissue due to inflammatory exudate, resulting in impaired gas exchange and respiratory compromise.
Pathological Process
- Infection or irritation of lung tissue
- Inflammatory response activation
- Alveolar filling with exudate
- Impaired ventilation and perfusion
Clinical Significance
- Leading cause of infection-related death
- High morbidity in vulnerable populations
- Significant healthcare burden
- Preventable through vaccination
Types of Pneumonia
Memory Aid: “CAHNV”
Classification by Origin
Community-Acquired Pneumonia (CAP)
Infection occurring in non-hospitalized patients or within 48 hours of admission
Healthcare-Associated Pneumonia (HCAP)
Infection in patients with recent healthcare exposure
Nosocomial (Hospital-Acquired)
Develops 48+ hours after hospital admission
Classification by Pathogen
Bacterial Pneumonia
- • Streptococcus pneumoniae (most common)
- • Haemophilus influenzae
- • Staphylococcus aureus
- • Mycoplasma pneumoniae
- • Chlamydophila pneumoniae
- • Legionella pneumophila
Viral Pneumonia
Fungal & Other
Etiological Factors
Risk Factor Categories
Understanding risk factors is crucial for prevention, early detection, and targeted interventions in pneumonia management.
Host Factors
Age Extremes
- • Infants < 2 years
- • Adults > 65 years
- • Immature/declining immunity
Chronic Diseases
- • COPD, asthma
- • Diabetes mellitus
- • Heart failure
- • Chronic kidney disease
Immunocompromise
- • HIV/AIDS
- • Cancer treatment
- • Organ transplant
- • Corticosteroid use
Environmental
Exposure Risks
- • Healthcare facilities
- • Crowded living conditions
- • Poor ventilation
- • Air pollution
Occupational
- • Healthcare workers
- • Dust exposure
- • Chemical inhalation
- • Animal contact
Seasonal Factors
- • Winter months
- • Influenza season
- • Indoor crowding
- • Reduced humidity
Behavioral
Substance Use
- • Tobacco smoking
- • Alcohol abuse
- • Illicit drug use
- • Injection drug use
Lifestyle
- • Poor nutrition
- • Inadequate sleep
- • Sedentary lifestyle
- • Poor hygiene
Medical Compliance
- • Missed vaccinations
- • Medication non-adherence
- • Delayed healthcare seeking
- • Self-medication
High-Risk Populations
Pathophysiology
Pathophysiological Cascade
Pneumonia represents a complex inflammatory response involving multiple physiological systems, resulting in compromised gas exchange and systemic effects.
Disease Process Flow
1. Pathogen Entry
Inhalation, aspiration, or hematogenous spread
2. Alveolar Invasion
Pathogens reach and colonize alveoli
3. Inflammatory Response
Immune system activation, cytokine release
4. Vascular Changes
Increased permeability, vasodilation
5. Alveolar Consolidation
Fluid, cells, and debris fill alveoli
6. Impaired Gas Exchange
Hypoxemia and respiratory compromise
Inflammatory Process
Initial Response
- Alveolar macrophage activation
- Complement system activation
- Cytokine release (IL-1, TNF-α)
- Neutrophil recruitment
Vascular Changes
- Increased capillary permeability
- Vasodilation and hyperemia
- Plasma protein extravasation
- Fibrin deposition
Gas Exchange Impairment
V/Q Mismatch
Perfusion without ventilation in consolidated areas
Ventilation without perfusion due to vascular compromise
Systemic Effects
- Fever and systemic inflammatory response
- Increased metabolic demands
- Hypoxemic effects on organs
- Potential sepsis development
Classical Stages of Pneumonia
Signs & Symptoms
Memory Aid: “COUGHS”
Respiratory Manifestations
Primary Symptoms
- • Initially dry, then productive
- • Purulent, rust-colored, or bloody sputum
- • May be persistent and worsening
- • Shortness of breath on exertion
- • May progress to rest dyspnea
- • Tachypnea (>20 breaths/min)
- • Pleuritic (sharp, stabbing)
- • Worsens with inspiration
- • Localized to affected area
Physical Signs
Systemic Manifestations
Constitutional Symptoms
Often high-grade (>38.3°C/101°F)
Severe shivering episodes
Malaise, weakness
Loss of appetite
Severe/Complications
- • Cyanosis (central and peripheral)
- • Confusion, altered mental status
- • Oxygen saturation <90%
- • Hypotension (SBP <90 mmHg)
- • Tachycardia (HR >100 bpm)
- • Altered mental status
Special Populations
May present with confusion, falls, subtle symptoms
Rapid breathing, poor feeding, irritability
Atypical presentation, minimal inflammatory response
Severity Indicators
Mild
- • No dyspnea at rest
- • Normal mental status
- • Stable vital signs
- • SaO2 >90%
Moderate
- • Dyspnea with exertion
- • Tachypnea >24/min
- • SaO2 85-90%
- • Multilobar involvement
Severe
- • Respiratory failure
- • Hypotension/shock
- • Altered consciousness
- • SaO2 <85%
Assessment
Comprehensive Assessment Approach
Systematic evaluation combining clinical assessment, physical examination, and diagnostic investigations to establish diagnosis and severity.
Primary Assessment (ABCs)
A Airway
- • Patency and clearance
- • Secretion management
- • Ability to cough effectively
B Breathing
- • Rate, depth, rhythm
- • Work of breathing
- • Oxygen saturation
- • Breath sounds
C Circulation
- • Heart rate and rhythm
- • Blood pressure
- • Perfusion status
- • Capillary refill
Secondary Assessment
Neurological Status
- • Level of consciousness (GCS)
- • Orientation and cognition
- • Signs of hypoxia/hypercapnia
Integumentary
- • Color (cyanosis, pallor)
- • Temperature and diaphoresis
- • Turgor and hydration status
Gastrointestinal
- • Appetite and nutrition
- • Nausea/vomiting
- • Bowel function
Genitourinary
- • Urine output
- • Fluid balance
- • Kidney function indicators
Physical Examination Techniques
Inspection
- • Chest movement
- • Use of accessory muscles
- • Breathing pattern
- • Skin color
Palpation
- • Tactile fremitus
- • Chest expansion
- • Lymph nodes
- • Skin temperature
Percussion
- • Dullness over consolidation
- • Hyperresonance
- • Diaphragmatic excursion
- • Organ borders
Auscultation
- • Breath sounds
- • Adventitious sounds
- • Voice sounds
- • Heart sounds
Pain Assessment
PQRST Assessment
Pain Characteristics
- • Pleuritic: Sharp, worsens with inspiration
- • Location: Usually unilateral
- • Aggravating: Movement, deep breathing
- • Relieving: Splinting, analgesics
Functional Assessment
Activity Tolerance
- • Dyspnea on exertion scale
- • Distance walked without SOB
- • Activities of daily living
- • Sleep quality
Nutritional Status
- • Appetite and intake
- • Weight loss/gain
- • Swallowing ability
- • Hydration status
Psychosocial
- • Anxiety and fear
- • Coping mechanisms
- • Support systems
- • Understanding of condition
Diagnosis
Diagnostic Approach
Pneumonia diagnosis combines clinical presentation, physical examination findings, and diagnostic investigations. Early and accurate diagnosis is crucial for optimal patient outcomes.
Laboratory Studies
Blood Tests
- • Leukocytosis (>11,000/μL) with left shift
- • May have leukopenia in severe cases
- • Increased bands (>10%)
- • Elevated (>100 mg/L suggests bacterial)
- • Helps differentiate bacterial vs viral
- • Monitors treatment response
- • >0.25 ng/mL suggests bacterial infection
- • Guides antibiotic therapy
- • Lower in viral pneumonia
Microbiological Studies
- • Gram stain and culture
- • Quality: <25 epithelial cells per lpf
- • >25 neutrophils per lpf
- • Before antibiotic administration
- • Positive in 10-20% of CAP
- • Higher yield in severe pneumonia
- • Streptococcus pneumoniae
- • Legionella pneumophila
- • Rapid results
Imaging Studies
Chest X-Ray
- • Lobar consolidation (bacterial)
- • Interstitial infiltrates (viral/atypical)
- • Air bronchograms
- • Pleural effusion
- • May be normal in early disease
- • Dehydration may mask infiltrates
- • Immunocompromised patients
CT Chest
- • Complicated pneumonia
- • Suspected lung abscess
- • Failed response to treatment
- • Immunocompromised patients
- • Better detection of complications
- • Assessment of pleural disease
- • Guide interventional procedures
Other Studies
- • Hypoxemia (PaO2 <60 mmHg)
- • Respiratory alkalosis initially
- • May progress to acidosis
- • If significant effusion present
- • Differentiate exudate vs transudate
- • Culture and sensitivity
Pneumonia Severity Assessment
CURB-65 Score
- • 0-1: Low risk (outpatient treatment)
- • 2: Moderate risk (short hospital stay)
- • 3-5: High risk (hospitalization/ICU)
Pneumonia Severity Index (PSI)
- • Malignancy, liver disease, CHF, CVD, renal disease
- • Altered mental status (+20)
- • Respiratory rate >30 (+20)
- • SBP <90 mmHg (+20)
- • Temperature <35°C or >40°C (+15)
- • Pulse >125 bpm (+10)
- • pH <7.35 (+30), BUN >30 (+20)
- • Na <130 (+20), Glucose >250 (+10)
- • Hematocrit <30% (+10), PaO2 <60 (+10)
Differential Diagnosis
Respiratory Conditions
- • Pulmonary edema
- • Pulmonary embolism
- • Lung cancer
- • Tuberculosis
- • COPD exacerbation
Cardiac Conditions
- • Myocardial infarction
- • Heart failure
- • Pericarditis
- • Aortic dissection
Other Conditions
- • Viral upper respiratory infection
- • Gastroesophageal reflux
- • Anxiety/panic disorder
- • Drug-induced pneumonitis
Medical Management
Treatment Goals
Antibiotic Therapy
Community-Acquired Pneumonia
- • First-line: Amoxicillin 1g TID x 5-7 days
- • Alternative: Macrolide (Azithromycin)
- • Atypical coverage: Add if suspected
- • First-line: Amoxicillin-clavulanate + Macrolide
- • Alternative: Fluoroquinolone (Levofloxacin)
- • β-lactam allergy: Macrolide + Doxycycline
- • Preferred: β-lactam + Macrolide
- • Alternative: Respiratory fluoroquinolone
- • Examples: Ceftriaxone + Azithromycin
Healthcare-Associated Pneumonia
- • Anti-pseudomonal β-lactam
- • Plus anti-MRSA agent
- • Consider local resistance patterns
- • Piperacillin-tazobactam + Vancomycin
- • Cefepime + Linezolid
- • Meropenem + Vancomycin
Supportive Care
Respiratory Support
- • Target SaO2 94-98% (88-92% if COPD)
- • Nasal cannula, face mask, or high-flow
- • Monitor closely for improvement
- • Respiratory failure (PaO2/FiO2 <200)
- • Altered mental status
- • Inability to protect airway
Fluid & Electrolyte Management
- • Maintain adequate hydration
- • Avoid fluid overload
- • Monitor input/output
- • Correct hyponatremia (common)
- • Monitor potassium levels
- • Replace as needed
Symptomatic Treatment
- • Acetaminophen for fever/pain
- • NSAIDs (caution with kidney function)
- • Opioids for severe pleuritic pain
- • Usually avoid suppressants
- • Expectorants may help
- • Codeine for severe cough
Treatment Duration & Monitoring
Duration Guidelines
- CAP (uncomplicated): 5-7 days
- HAP/VAP: 7-8 days
- Atypical pneumonia: 10-14 days
- Complicated cases: Extended duration
Monitoring Parameters
- Temperature normalization
- Vital signs improvement
- Oxygen requirements
- Laboratory normalization
Complications & Management
Respiratory Complications
- • ARDS: Mechanical ventilation, lung-protective strategies
- • Pleural effusion: Thoracentesis if large
- • Empyema: Chest tube drainage
- • Lung abscess: Prolonged antibiotics, drainage
Systemic Complications
- • Septic shock: Vasopressors, fluid resuscitation
- • Multi-organ failure: Supportive care
- • Coagulopathy: Blood product support
- • Acute kidney injury: Renal replacement therapy
Cardiac Complications
- • Myocarditis: Supportive care, avoid exertion
- • Pericarditis: Anti-inflammatory therapy
- • Arrhythmias: Monitor, treat as indicated
- • Heart failure: Diuretics, afterload reduction
Nursing Management
Nursing Care Priorities
Comprehensive nursing care focusing on respiratory support, infection control, symptom management, and patient education to optimize recovery and prevent complications.
Priority Nursing Diagnoses
1. Impaired Gas Exchange
Related to: Inflammatory process in lung parenchyma
AEB: Dyspnea, hypoxemia, abnormal ABGs
2. Ineffective Airway Clearance
Related to: Excessive secretions, weak cough
AEB: Productive cough, adventitious sounds
3. Hyperthermia
Related to: Infectious process
AEB: Elevated temperature, diaphoresis
4. Acute Pain
Related to: Pleuritic chest pain
AEB: Verbal reports, guarding behavior
5. Activity Intolerance
Related to: Impaired oxygenation
AEB: Fatigue, weakness, dyspnea on exertion
6. Knowledge Deficit
Related to: Unfamiliarity with condition
AEB: Questions, misconceptions
Respiratory Interventions
Oxygenation Support
- • Monitor respiratory rate, depth, rhythm q4h
- • Assess oxygen saturation continuously
- • Observe for cyanosis, use of accessory muscles
- • Auscultate lungs q8h and PRN
- • Administer oxygen as prescribed
- • Position in semi-Fowler’s or high-Fowler’s
- • Encourage deep breathing and coughing
- • Provide rest periods between activities
Airway Clearance
- • Assess sputum characteristics
- • Encourage fluid intake (2-3L/day unless contraindicated)
- • Perform chest physiotherapy as ordered
- • Suction if unable to clear secretions
- • Teach diaphragmatic breathing
- • Incentive spirometry q2h while awake
- • Pursed-lip breathing technique
- • Splinting for cough effectiveness
General Care
Temperature Management
- • Temperature q4h and PRN
- • Watch for patterns and trends
- • Monitor for signs of sepsis
- • Administer antipyretics as ordered
- • Cooling measures (tepid sponging)
- • Ensure adequate fluid intake
- • Light clothing and bedding
Pain Management
- • Use pain scale (0-10)
- • Assess pain characteristics
- • Monitor effectiveness of interventions
- • Administer analgesics as prescribed
- • Position for comfort
- • Splinting techniques for cough
- • Heat/cold application as appropriate
Nutrition & Hydration
- • Monitor intake and output
- • Provide high-calorie, high-protein diet
- • Small, frequent meals
- • Consider nutritional supplements
- • Encourage fluid intake unless contraindicated
- • Monitor for dehydration signs
- • IV fluids as prescribed
- • Electrolyte monitoring
Infection Control Measures
Standard Precautions
- • Hand hygiene before/after patient contact
- • Use of PPE as appropriate
- • Safe disposal of contaminated materials
- • Proper handling of patient equipment
Droplet Precautions
- • Surgical mask within 3 feet
- • Patient mask during transport
- • Private room if possible
- • Educate patient on cough etiquette
Environmental Control
- • Regular room cleaning and disinfection
- • Proper ventilation
- • Tissue disposal at bedside
- • Hand sanitizer availability
Monitoring Parameters
Respiratory
- • Respiratory rate
- • Oxygen saturation
- • Breath sounds
- • Dyspnea scale
Cardiovascular
- • Heart rate
- • Blood pressure
- • Perfusion status
- • Fluid balance
Neurological
- • Level of consciousness
- • Orientation
- • Confusion/agitation
- • Pain assessment
General
- • Temperature
- • Nutrition/hydration
- • Skin integrity
- • Laboratory values
Nursing Implementation
Implementation Framework
Systematic approach to implementing evidence-based nursing interventions across the continuum of care, from acute management to discharge planning and prevention.
Acute Phase (First 24-48 hours)
Immediate Priorities
- • Continuous pulse oximetry monitoring
- • Initiate oxygen therapy per protocol
- • Position patient for optimal ventilation
- • Assess respiratory status q2-4h
- • Obtain cultures before first antibiotic dose
- • Administer within 4 hours of presentation
- • Monitor for allergic reactions
- • Document time of administration
Supportive Care
- • Start IV access if not present
- • Monitor fluid balance closely
- • Encourage oral fluids if tolerated
- • Watch for signs of overload
- • Administer antipyretics for fever >38.5°C
- • Provide pain relief for chest pain
- • Implement comfort measures
