Professional Considerations in Nursing
Legal and Ethical Framework for Nursing Practice
Welcome to comprehensive study notes on professional considerations in nursing. These notes are designed to help nursing students understand the legal and ethical frameworks that guide nursing practice. The content is presented in an easy-to-understand format with visual aids, tables, and mnemonics to facilitate learning.
Understanding professional considerations in nursing is essential for providing safe, ethical, and legally sound patient care. As a nurse, your practice is governed by various regulatory bodies, codes of ethics, and legal frameworks that protect both patients and healthcare providers.
Table of Contents
1. Nursing as a Profession
2. Regulatory Bodies
3. Professional Ethics
4. Legal Aspects in Nursing
- 4.1 Consumer Protection Act and Patient Rights
- 4.2 Legal Terms Related to Practice
- 4.3 Types of Law, Tort Law & Liabilities
- 4.4 Laws Related to Nursing Practice
- 4.5 Negligence, Malpractice, and Breach
- 4.6 Invasion of Privacy and Defamation
5. Nursing Regulatory Mechanisms
- 5.1 Registration, Licensure, and Renewal
- 5.2 Accreditation and Nurse Practice Act
- 5.3 Regulation for Nurse Practitioners/Specialists
6. Learning Aids
1. Nursing as a Profession
1.1 Characteristics of a Professional Nurse
Nursing is recognized globally as a profession that requires specialized knowledge, skills, and attitudes. A profession differs from an occupation by several defining characteristics that nursing embodies.
- Specialized Education: Requires formalized education with theoretical and practical components
- Autonomy in Practice: Ability to make independent clinical judgments within scope of practice
- Self-Regulatory Body: Governed by professional nursing organizations that set standards
- Code of Ethics: Adheres to established ethical principles and guidelines
- Service Orientation: Focused on providing care that benefits society
- Research Base: Practice informed by evidence and ongoing research
- Professional Identity: Strong sense of identification with the nursing profession
- Continuing Education: Commitment to lifelong learning and professional development
- Accountability: Responsible for actions and decisions in practice
- Commitment: Long-term dedication to the profession and its values
Mnemonic: “PROFESSIONAL”
P – Practice based on specialized knowledge
R – Regulatory control by nursing bodies
O – Ongoing education and development
F – Formal code of ethics adherence
E – Evidence-based practice implementation
S – Service to society and patients
S – Self-regulation and discipline
I – Independent decision-making
O – Organizational membership
N – Nursing knowledge advancement
A – Accountability for actions
L – Licensure requirements fulfillment

Figure 1: Theoretical framework of nurses’ professional self-concept and influencing factors
1.2 Nursing Practice: Philosophy, Aim, and Objectives
Nursing Philosophy
A nursing philosophy is a statement of beliefs and values that guide nursing practice. It forms the foundation for how nurses approach patient care, interact with healthcare teams, and view their professional role in society.
Core Elements of Nursing Philosophy
- Dignity and worth of each person
- Holistic nature of humans
- Right to self-determination
- Unique biological, psychological, social, and spiritual needs
- Health as more than absence of disease
- Health as dynamic state of being
- Illness as opportunity for growth
- Health promotion as essential
- Advocacy for patients
- Therapeutic use of self
- Evidence-based practice
- Professional collaboration
Aims and Objectives of Nursing Practice
| Aim | Specific Objectives |
|---|---|
| Promote and restore health |
|
| Prevent illness and injury |
|
| Alleviate suffering |
|
| Advocate for patients |
|
| Advance the profession |
|
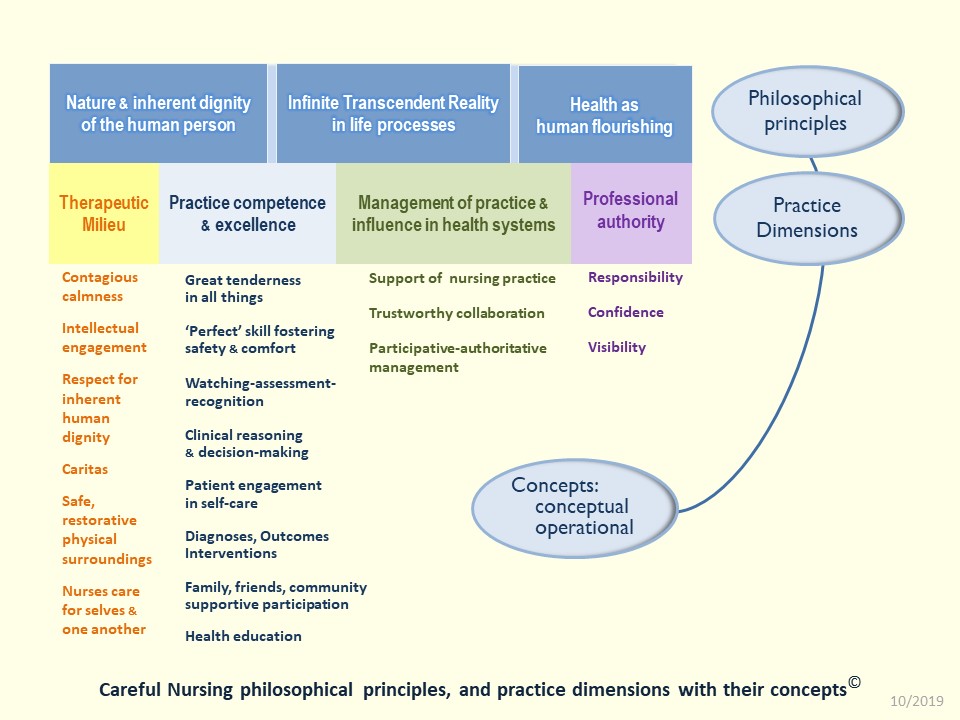
Figure 2: Professional Practice Model illustrating the dimensions of nursing practice
2. Regulatory Bodies
2.1 Indian Nursing Council (INC)
What is the Indian Nursing Council?
The Indian Nursing Council (INC) is a national regulatory body established under the Indian Nursing Council Act, 1947. It is an autonomous body under the Government of India, Ministry of Health & Family Welfare, responsible for regulating and maintaining uniform standards of nursing education throughout the country.
Establishment and Legal Framework
The INC was established as a result of the Indian Nursing Council Act of 1947, which provided the legal framework for the formation and functioning of this regulatory body. The Act empowers the INC to regulate nursing education and practice standards across India.
2.2 State Nursing Council (SNC)
What is a State Nursing Council?
State Nursing Councils (SNCs) are regulatory bodies established at the state level that work in coordination with the Indian Nursing Council. Each state and union territory in India has its own nursing council responsible for implementing the standards set by the INC and addressing state-specific nursing issues.
Relationship Between INC and SNCs
The relationship between the INC and SNCs is based on a cooperative regulatory framework:
- INC sets national standards and policies
- SNCs implement these standards at state level
- SNCs handle registration and licensing of nurses in their respective states
- INC recognizes qualifications approved by SNCs
- Both bodies work together to ensure uniform nursing education and practice across the country
2.3 Constitution and Functions
The INC consists of the following members:
- President appointed by the Central Government
- Vice-President elected from among the members
- Representatives from each state nursing council
- Representatives from central government and state governments
- Nursing education experts nominated by the government
- Representatives from medical and nursing professional associations
SNCs typically consist of:
- President appointed by the State Government
- Elected members from registered nurses in the state
- Representatives from state health department
- Representatives from nursing educational institutions
- Nursing experts nominated by the state government
- Ex-officio members from health services
Key Functions of Regulatory Bodies
| Function | Indian Nursing Council (INC) | State Nursing Council (SNC) |
|---|---|---|
| Educational Standards | Establishes uniform standards for nursing education programs across India | Ensures implementation of educational standards in state institutions |
| Curriculum Development | Develops and revises nursing curriculum at national level | Adapts curriculum to meet state needs while maintaining INC standards |
| Accreditation | Prescribes conditions for recognition of nursing qualifications | Inspects and accredits nursing educational institutions in the state |
| Registration | Maintains central registry of nurses with recognized qualifications | Registers nurses to practice in the state and maintains state registry |
| Professional Conduct | Establishes code of ethics and professional conduct | Enforces professional standards and handles misconduct cases |
| Continuing Education | Develops guidelines for continuing nursing education | Organizes continuing education programs for nurses in the state |
| Advisory Role | Advises central government on nursing matters | Advises state government on nursing issues at state level |
Important Note:
The regulatory framework of nursing in India follows a two-tier system where the INC sets national standards and SNCs implement these standards at the state level. This ensures both national uniformity and state-specific adaptation of nursing education and practice regulations.
3. Professional Ethics
3.1 Code of Ethics and Professional Conduct
What is a Code of Ethics?
A code of ethics in nursing is a formal statement of ethical values and principles that guides nurses in their professional practice. It outlines the moral obligations and duties of nurses toward patients, colleagues, the profession, and society at large.
INC Code of Ethics
The Indian Nursing Council’s Code of Ethics provides ethical guidelines for nurses in India. The code emphasizes:
- Respect for human dignity and rights
- Professional accountability and responsibility
- Competence and professional growth
- Truthfulness and honesty
- Cooperation with healthcare team members
- Maintenance of standards of personal conduct
- Participation in professional activities
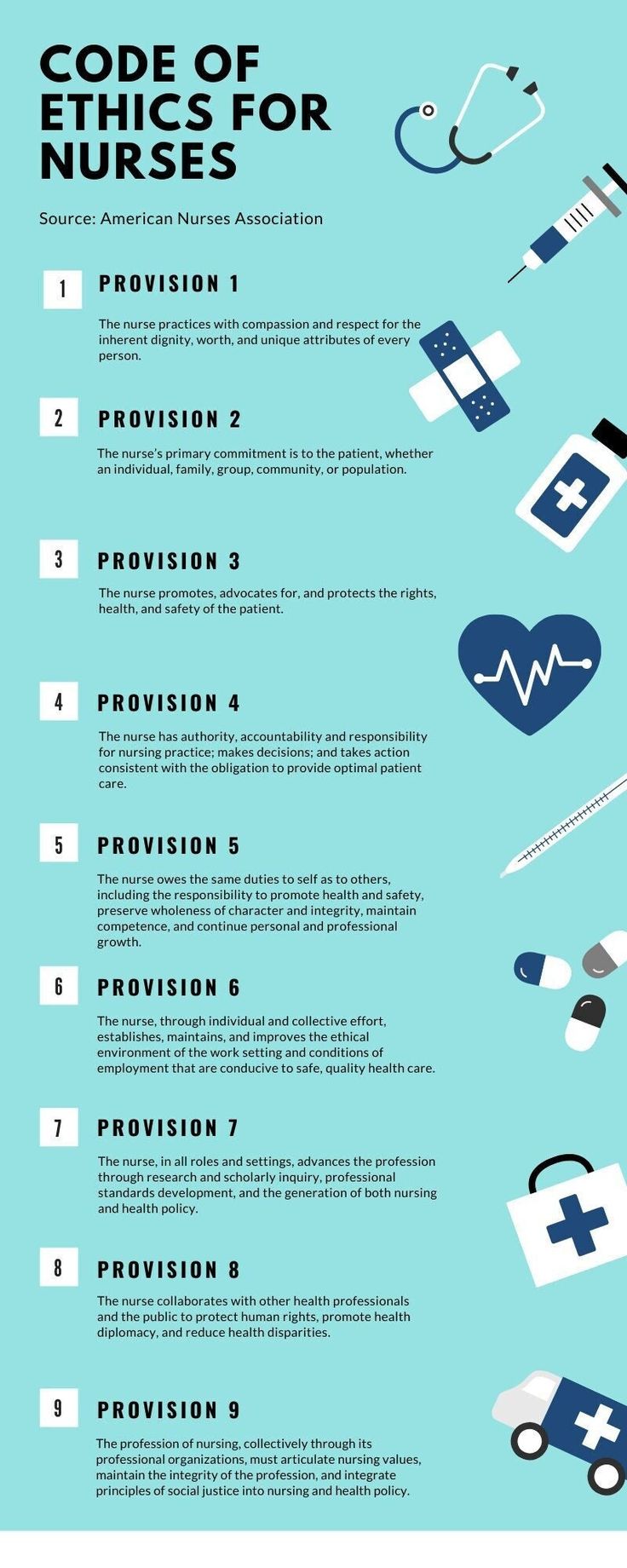
Figure 3: Code of Ethics for Nurses Infographic
Professional Conduct Guidelines
Professional conduct goes beyond ethical principles to include specific behaviors and actions expected of nurses in their professional role. The regulatory bodies provide guidelines for professional conduct that include:
- Providing safe, competent care
- Respecting patient privacy and confidentiality
- Obtaining informed consent
- Maintaining professional boundaries
- Advocating for patient rights
- Collaborating with healthcare team
- Communicating effectively
- Maintaining respectful relationships
- Addressing conflicts constructively
- Supporting colleagues
- Engaging in continuing education
- Maintaining competence
- Participating in research
- Advancing nursing knowledge
- Mentoring new nurses
Professional Misconduct
Failure to adhere to the code of ethics and professional conduct may lead to disciplinary action by regulatory bodies. Examples of professional misconduct include:
- Negligence in patient care
- Breach of confidentiality
- Practicing beyond scope of competence
- Falsification of records
- Substance abuse affecting practice
- Criminal behavior
- Violation of patient rights
3.2 Practice Standards for Nursing – INC
Practice standards are authoritative statements developed by regulatory bodies to define the legal and professional expectations of nursing practice. The Indian Nursing Council has established practice standards that serve as benchmarks for quality nursing care.
Key Components of INC Practice Standards
| Standard Category | Description | Examples |
|---|---|---|
| Assessment | Standards for collecting and analyzing patient data |
|
| Diagnosis | Standards for identifying patient problems and needs |
|
| Planning | Standards for developing care plans |
|
| Implementation | Standards for carrying out nursing interventions |
|
| Evaluation | Standards for assessing outcomes of care |
|
| Professional Development | Standards for maintaining competence |
|
| Quality of Practice | Standards for ensuring quality care |
|
Purpose of Practice Standards:
The practice standards established by regulatory bodies serve multiple purposes:
- Provide framework for nursing practice evaluation
- Guide development of nursing curricula
- Define expectations for employers and the public
- Serve as basis for quality improvement
- Provide legal reference for professional conduct
- Support professional self-regulation
3.3 International Council for Nurses (ICN)
What is the International Council for Nurses?
The International Council for Nurses (ICN) is a federation of national nursing associations representing nurses worldwide. Founded in 1899, it is the world’s first and widest reaching international organization for health professionals, working to ensure quality nursing care for all and sound health policies globally.
ICN Code of Ethics for Nurses
The ICN Code of Ethics for Nurses is a guide for action based on social values and needs. It has served as the standard for nurses worldwide since it was first adopted in 1953 and is regularly updated to reflect evolving nursing and healthcare practices.
The ICN Code has four principal elements that outline the standards of ethical conduct:
- Nurses and People: Respect for human rights, dignity, and cultural values
- Nurses and Practice: Personal responsibility and accountability for nursing practice
- Nurses and the Profession: Implementation of professional values and maintaining the integrity of the profession
- Nurses and Co-workers: Collaborative relationships with colleagues and others

Figure 4: ICN Code of Ethics for Nurses – Infographic Poster
Relationship Between ICN and National Regulatory Bodies
While the ICN is not a regulatory body, it influences nursing regulation worldwide through:
- Providing global ethical standards that inform national codes of ethics
- Developing position statements on nursing practice, education, and regulation
- Advocating for appropriate regulatory frameworks in different countries
- Supporting national nursing associations in their regulatory functions
- Promoting international consistency in nursing standards
- Facilitating global dialogue on nursing regulation issues
ICN’s Regulatory Initiatives
- ICN Nurse Practitioner/Advanced Practice Nursing Network: Supports regulation of advanced practice
- Regulatory Competencies Framework: Outlines competencies needed by nursing regulators
- Global Regulatory Atlas: Maps nursing regulatory systems worldwide
- Global Standards for Initial Nursing Education: Informs regulatory standards for education
- International Credentialing and Registration Framework: Guides mobility of nursing workforce
- Position Statement on Continuing Competence: Informs regulatory approaches to maintaining competence
4. Legal Aspects in Nursing
4.1 Consumer Protection Act and Patient Rights
Consumer Protection Act
The Consumer Protection Act is legislation designed to protect consumers from unfair trade practices, deficient services, and ensure the right to be informed about quality, quantity, and price of goods and services. In healthcare, patients are considered consumers of medical services.
Implications of Consumer Protection Act for Nursing Practice
The Consumer Protection Act has significant implications for nursing practice and healthcare delivery:
- Nurses can be held liable for deficiency in care provided to patients
- Healthcare services, including nursing, are covered under the purview of the Act
- Patients can seek compensation for damages resulting from negligent nursing care
- Hospitals and individual practitioners must provide services of professional standards
- Informed consent becomes legally mandatory before procedures
- Documentation and record-keeping are crucial as legal evidence
Patient Rights
Patient rights are fundamental principles that guide the relationship between patients and healthcare providers, including nurses. These rights are protected by various laws and regulatory frameworks:
- Right to Information: Clear, accurate information about condition, treatment options, risks, and benefits
- Right to Consent: Freedom to accept or refuse treatment after being informed
- Right to Confidentiality: Protection of personal and medical information
- Right to Dignity: Respectful and considerate care regardless of personal attributes
- Right to Safety: Care that avoids preventable harm
- Right to Continuity: Coordinated care across healthcare settings
- Right to Grievance: Process to address complaints about care
- Advocate for patients when rights are threatened
- Provide information in understandable language
- Respect cultural, religious, and personal preferences
- Maintain confidentiality of patient information
- Involve patients in care planning and decisions
- Document informed consent procedures
- Report violations of patient rights
- Support patient autonomy in healthcare decisions
Mnemonic: “PATIENT RIGHTS”
P – Privacy of personal information
A – Access to medical records
T – Treatment information and options
I – Informed consent before procedures
E – Equal treatment without discrimination
N – Nondisclosure of confidential information
T – Truth about diagnosis and prognosis
R – Refusal of treatment option
I – Involvement in care decisions
G – Grievance procedure access
H – Humane and dignified care
T – Treatment by qualified professionals
S – Safe environment for care
4.2 Legal Terms Related to Practice
Understanding legal terminology is essential for nurses to navigate the legal aspects of practice and ensure compliance with legal standards. Here are key legal terms relevant to nursing practice:
| Legal Term | Definition | Relevance to Nursing |
|---|---|---|
| Duty of Care | Legal obligation to adhere to a standard of reasonable care while performing acts that could foreseeably harm others | Establishes nurse’s responsibility to provide care according to professional standards |
| Standard of Care | Level of care that a reasonably prudent nurse would provide in similar circumstances | Benchmark against which nursing actions are legally evaluated |
| Informed Consent | Patient’s agreement to treatment after understanding the nature, risks, benefits, and alternatives | Nurses often responsible for ensuring proper informed consent process |
| Negligence | Failure to exercise proper care resulting in harm to another | Basis for malpractice claims against nurses |
| Statute of Limitations | Legal time limit for filing lawsuits after an alleged wrongdoing | Defines timeframe during which nurses may face legal action |
| Respondeat Superior | “Let the master answer” – employer’s liability for employee actions during employment | Hospitals may be liable for nursing actions, but doesn’t absolve individual nurse |
| Discovery Rule | Statute of limitations begins when patient discovers or should have discovered injury | Extends potential liability period for undetected injuries |
| Res Ipsa Loquitur | “The thing speaks for itself” – presumption of negligence when injury wouldn’t occur without negligence | Applied in cases of obvious nursing errors (e.g., wrong-site surgery) |
| Assault | Intentional creation of fear of harmful or offensive contact | Can occur if nurse threatens treatment without consent |
| Battery | Intentional touching without consent | Performing procedures without proper consent |
Legal Documentation in Nursing:
Documentation serves as legal evidence of nursing care. Legal principles of documentation include:
- Complete and accurate recording of assessments, interventions, and outcomes
- Objective rather than subjective descriptions
- Contemporaneous documentation (at or near the time of event)
- Clear identification of the nurse providing care
- Proper correction of errors (no erasures or covering up)
- Adherence to facility documentation policies
- Documentation of unusual occurrences or incidents
- Inclusion of patient responses to interventions
4.3 Types of Law, Tort Law & Liabilities
Major Legal Systems Affecting Nursing Practice
Definition: Law that regulates conduct considered harmful to society and carries potential incarceration as punishment.
Application to Nursing:
- Extreme cases of negligence resulting in death
- Practicing without valid license
- Medication theft or diversion
- Patient abuse or neglect
- Falsification of medical records
- Violation of narcotics laws
Definition: Law that regulates relationships between individuals or entities and provides remedies (usually monetary) for violations.
Application to Nursing:
- Malpractice claims
- Contract disputes
- Employment issues
- Patient privacy violations
- Informed consent failures
- Professional negligence
Tort Law and Nursing Liability
What is Tort Law?
Tort law is a branch of civil law that deals with wrongful acts or injuries caused by one party to another, where the injured party can seek compensation. In nursing, tort law governs most professional liability issues.
Types of Torts in Nursing Practice
Unintentional Torts
- Negligence: Failure to provide care that meets professional standards
- Malpractice: Professional negligence (most common basis for nursing liability)
- Corporate Negligence: Healthcare facility’s failure to fulfill duties
Intentional Torts
- Assault and Battery: Threats or unauthorized touching
- False Imprisonment: Unauthorized restraint of a patient
- Invasion of Privacy: Unauthorized disclosure of confidential information
- Defamation: False statements that harm reputation
Nurse Liability
Nursing liability refers to the legal responsibility of nurses for their professional actions or omissions. Types of liability include:
Individual responsibility for one’s own actions
Examples:
- Medication errors
- Failure to follow policy
- Practicing beyond scope
- Documentation errors
Employer’s responsibility for employee actions
Examples:
- Hospital liability for nurse actions
- Supervisor liability for subordinates
- Facility liability for contracted staff
Multiple parties sharing responsibility
Examples:
- Team-based errors
- System failures
- Communication breakdowns
- Handoff errors

Figure 5: The 4 D’s of Medical Malpractice: Duty, Dereliction, Direct Cause, Damages
4.4 Laws Related to Nursing Practice
Various laws at national and state levels govern nursing practice and establish the legal framework within which nurses must operate. Understanding these laws is essential for ensuring legal compliance and safe practice.
Key Laws Affecting Nursing Practice
| Law/Regulation | Purpose and Scope | Nursing Implications |
|---|---|---|
| Nursing Act | Establishes legal framework for nursing practice, education, and regulation | Defines scope of practice, education requirements, and regulatory mechanisms |
| Medical Council Act | Regulates medical practice and affects interprofessional relationships | Influences nurse-physician collaboration and delegation parameters |
| Pharmacy Act | Regulates pharmaceutical practices and medication management | Impacts medication administration, storage, and prescription protocols |
| Mental Health Act | Governs care of patients with mental health conditions | Defines procedures for involuntary treatment, restraint, and patient rights in psychiatric care |
| Consumer Protection Act | Protects patients as consumers of healthcare services | Establishes liability for deficient care and standards for service delivery |
| Right to Information Act | Ensures transparency and access to information | Affects disclosure of healthcare information and patient access to records |
| Biomedical Waste Management Rules | Regulates handling and disposal of biomedical waste | Requires compliance with waste segregation, handling, and disposal protocols |
| Narcotics and Psychotropic Substances Act | Controls use and distribution of controlled substances | Governs controlled medication administration, storage, and documentation |
| Clinical Establishments Act | Regulates healthcare facilities and standards | Affects nursing practice environments and quality assurance measures |
Legal Compliance in Nursing
To maintain legal compliance in practice, nurses should:
- Stay informed about current laws and regulations affecting practice
- Adhere to facility policies that implement legal requirements
- Maintain current licensure and required certifications
- Practice within defined scope as established by regulatory bodies
- Document care accurately and completely
- Obtain appropriate informed consent before procedures
- Protect patient confidentiality and privacy
- Report illegal or unethical practices through proper channels
- Maintain professional liability insurance
4.5 Negligence, Malpractice, and Breach
Negligence
Failure to exercise the degree of care that a reasonably prudent person would exercise under similar circumstances, resulting in harm to another.
Malpractice
Professional negligence – failure of a professional to meet the standard of care expected in their profession, causing harm to a client or patient.
Breach
Violation of a legal duty or failure to comply with a legal obligation, contract term, or standard of care.
Elements of Nursing Negligence
For a negligence claim to be successful against a nurse, four elements must be established:
-
Duty: A nurse-patient relationship existed, creating a duty of care
Example: Nurse assigned to care for a patient
-
Breach: The nurse failed to meet the standard of care
Example: Administering wrong medication or dose
-
Causation: The breach directly caused harm to the patient
Example: Wrong medication led to adverse reaction
-
Damages: The patient suffered actual harm or injury
Example: Patient required additional treatment
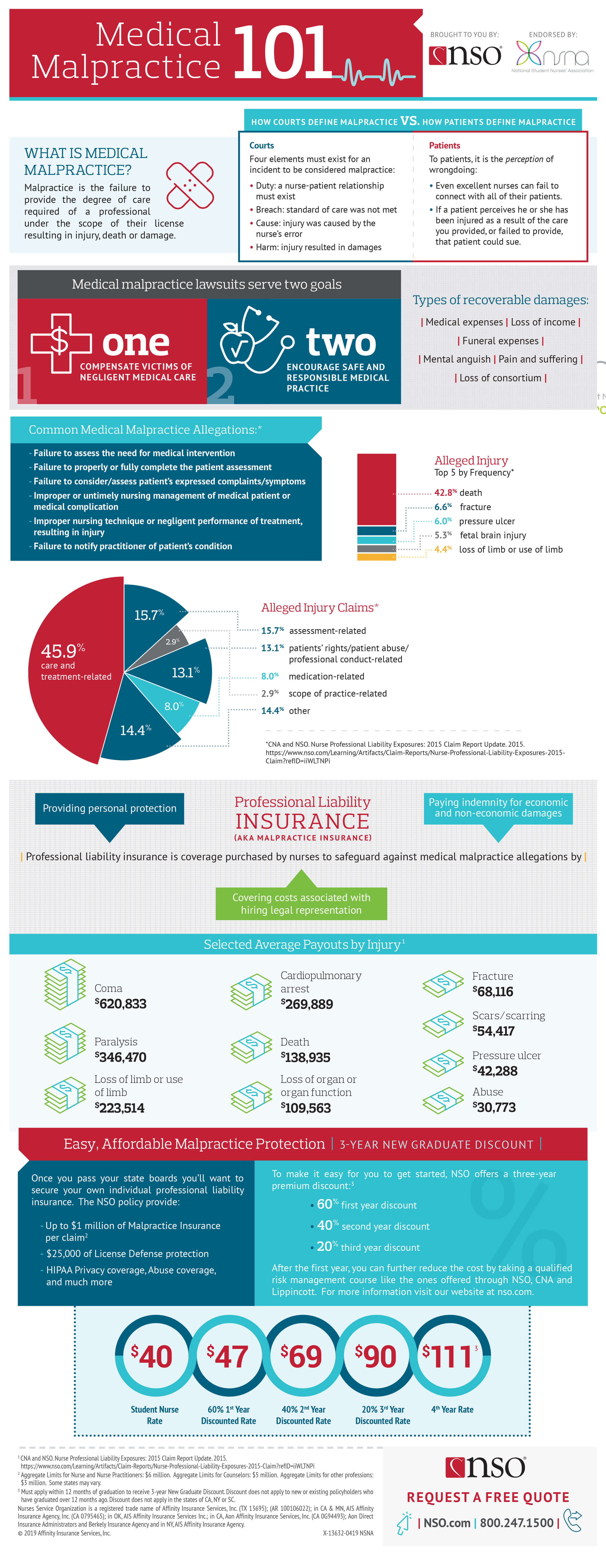
Figure 6: Medical Malpractice Elements and Prevention
Common Areas of Nursing Negligence
| Area of Practice | Examples of Negligence | Prevention Strategies |
|---|---|---|
| Medication Administration |
|
|
| Patient Monitoring |
|
|
| Documentation |
|
|
| Communication |
|
|
| Patient Safety |
|
|
Penalties for Nursing Negligence and Malpractice
When found negligent or guilty of malpractice, nurses may face various penalties and consequences:
- Monetary damages to patients
- Legal costs and attorney fees
- Criminal charges in severe cases
- Settlements or judgments
- License suspension or revocation
- Practice limitations or restrictions
- Mandated remedial education
- Professional probation
- Reporting to national databases
- Termination of employment
- Disciplinary actions
- Performance improvement plans
- Difficulty securing future employment
- Increased supervision requirements
Mnemonic: “PREVENT”
To avoid negligence and malpractice claims, remember:
P – Practice within your scope and competence
R – Record all care thoroughly and accurately
E – Educate yourself continuously on standards and best practices
V – Verify orders, allergies, and identities before interventions
E – Evaluate patient conditions regularly and document changes
N – Notify providers promptly about significant findings
T – Take appropriate safety precautions for all patients
4.6 Invasion of Privacy and Defamation
Invasion of Privacy
Invasion of privacy in healthcare refers to the unauthorized intrusion into a patient’s personal information or private affairs. It includes unauthorized disclosure of confidential information, intrusion into private spaces, or inappropriate exposure of a patient.
Types of Privacy Invasion in Nursing
- Breach of Confidentiality: Sharing patient information without authorization
- Unauthorized Access: Viewing patient records without legitimate purpose
- Public Disclosure: Exposing private facts about a patient to others
- Intrusion: Entering patient’s physical or digital space without justification
- Inappropriate Photography: Taking images without proper consent
- Social Media Violations: Posting patient information on personal accounts
Defamation of Character
Defamation involves communication of false statements about a person that harm their reputation. In nursing, defamation can occur when false information is communicated about patients, colleagues, or other healthcare professionals.
Types of Defamation
- Libel: Written defamatory statements (e.g., in medical records or emails)
- Slander: Spoken defamatory statements (e.g., verbal reports or gossip)
Elements of Defamation
- False statement of fact (not opinion)
- Communication to a third party
- Statement causes harm to reputation
- Statement made with at least negligence regarding truth
Legal and Professional Consequences
| Issue | Legal Consequences | Professional Consequences |
|---|---|---|
| Invasion of Privacy |
|
|
| Defamation |
|
|
Prevention Strategies
- Access patient information only when necessary for care
- Use privacy screens for computers and cover patient charts
- Conduct sensitive discussions in private areas
- Obtain proper consent before taking photographs
- Never share patient information on social media
- Log out of electronic health records when not in use
- Verify identity before providing information by phone
- Properly dispose of documents containing protected information
- Document objectively using facts, not opinions or assumptions
- Avoid gossip about patients, colleagues, or facilities
- Make statements based on verified information
- Use professional language in all communications
- Follow chain of command for reporting concerns
- Keep professional and personal communications separate
- Respect confidentiality in all professional discussions
- Review documentation for accuracy before finalizing
Social Media Caution:
Social media has created new risks for privacy violations and defamation. Nurses should:
- Never post any patient information or images, even without identifying details
- Avoid discussing workplace incidents or colleagues online
- Consider all online communications potentially discoverable in legal proceedings
- Maintain professional boundaries with patients on social platforms
- Follow facility social media policies and guidelines
- Remember that privacy settings do not guarantee protection from disclosure
5. Nursing Regulatory Mechanisms
5.1 Registration, Licensure, and Renewal
Registration
The process of entering a person’s name in the official roster maintained by the regulatory body, recognizing them as qualified to practice nursing.
Licensure
The granting of permission by a governmental authority to engage in nursing practice, following verification of minimum competency for safe practice.
Renewal
The periodic revalidation of a nursing license, typically requiring evidence of continuing education, practice hours, and good standing.
Registration and Licensure Process
- Education Completion: Graduate from a recognized nursing education program
- Examination: Pass the nursing licensure examination administered by the regulatory body
- Application Submission: Submit application for registration with required documents to state nursing council
- Background Verification: Undergo character and background checks
- Fee Payment: Pay registration and licensing fees
- Registration Approval: Receive registration number and certificate from nursing council
- License Issuance: Receive license to practice nursing
- Application form completed and signed
- Nursing education program completion certificate
- Examination passing certificate
- Birth certificate or proof of age
- Identity proof
- Address proof
- Character certificate
- Clinical experience certificates
- Passport-sized photographs
- Fee payment receipt
License Renewal Requirements
Nursing licenses must be renewed periodically as per regulatory body requirements. The renewal process typically includes:
| Requirement | Description | Purpose |
|---|---|---|
| Continuing Nursing Education (CNE) | Completion of specified number of education hours (typically 30-150 hours depending on jurisdiction) | Ensure ongoing professional development and knowledge currency |
| Practice Hours | Documentation of minimum nursing practice hours during license period | Verify continued clinical competence |
| Renewal Application | Submission of completed renewal form with updated information | Maintain current database of practicing nurses |
| Professional Conduct Declaration | Disclosure of any disciplinary actions, criminal convictions, or practice restrictions | Protect public safety by identifying potential concerns |
| Renewal Fee | Payment of prescribed renewal fee | Support regulatory functions of nursing council |
| Identity Verification | Confirmation of identity through documents or biometric methods | Prevent fraudulent renewal applications |
Consequences of Practicing Without Valid Registration/License:
Practicing nursing without current registration or license can lead to serious consequences:
- Legal penalties including fines and potential imprisonment
- Ineligibility for professional liability insurance coverage
- Difficulty obtaining future licensure
- Employment termination
- Disciplinary action by regulatory bodies
- Personal liability for adverse patient outcomes
- Professional reputation damage
5.2 Accreditation and Nurse Practice Act
Accreditation
Accreditation is a process by which nursing education programs and healthcare facilities are evaluated and certified as meeting predetermined quality standards by recognized authorities.
Types of Accreditation in Nursing
- Educational Program Accreditation: Recognition of nursing education programs meeting quality standards
- Healthcare Facility Accreditation: Certification of hospitals and other health facilities meeting quality care standards
- Specialty Certification Accreditation: Recognition of certification programs for specialized nursing areas
Accreditation Process
- Self-assessment and application by institution
- Document submission showing compliance with standards
- On-site evaluation by accreditation team
- Assessment report and recommendations
- Accreditation decision by authorizing body
- Periodic re-evaluation for continued accreditation
Nurse Practice Act
A Nurse Practice Act is state-level legislation that defines the scope of nursing practice, establishes regulatory boards, and sets the legal framework for nursing regulation in that jurisdiction.
Key Components of a Nurse Practice Act
- Definition of Nursing: Legal definition of what constitutes nursing practice
- Scope of Practice: Authorized activities and boundaries for nurses
- Education Requirements: Minimum educational standards for licensure
- Regulatory Board Structure: Composition and authority of nursing board
- Licensing Process: Requirements and procedures for obtaining license
- Disciplinary Provisions: Grounds and processes for disciplinary actions
- Continuing Competence: Requirements for maintaining practice currency
Importance of Accreditation and Nurse Practice Acts
| Stakeholder | Benefits of Accreditation | Benefits of Nurse Practice Act |
|---|---|---|
| Patients/Public |
|
|
| Nurses |
|
|
| Educational Institutions |
|
|
| Healthcare Facilities |
|
|
| Regulatory Bodies |
|
|
Relationship Between Accreditation and Nurse Practice Act
Accreditation and Nurse Practice Acts work together to ensure quality nursing practice:
- Nurse Practice Acts provide the legal authority for nursing education and practice standards
- Accreditation processes verify compliance with those standards
- Nursing boards established by Practice Acts often require graduation from accredited programs for licensure
- Accreditation standards typically align with the requirements outlined in Nurse Practice Acts
- Both mechanisms contribute to public protection through quality assurance
- Both provide frameworks for addressing substandard education or practice
5.3 Regulation for Nurse Practitioners/Specialists
Advanced Practice Nursing
Advanced Practice Nursing refers to nursing roles that require additional education, training, and competencies beyond basic nursing preparation. These roles include Nurse Practitioners, Clinical Nurse Specialists, Nurse Anesthetists, and Nurse Midwives.
Specialized Regulatory Framework
Advanced practice nurses are subject to additional regulatory requirements beyond those for general nursing practice:
- Advanced Education: Master’s or doctoral degree in nursing specialty
- Specialized Certification: National certification in specialty area
- Advanced Practice License: Additional licensure or recognition beyond RN
- Expanded Scope: Legal authorization for expanded practice activities
- Prescriptive Authority: Legal permission to prescribe medications
- Collaborative Agreements: Formal relationships with physicians or healthcare facilities
- Additional Continuing Education: Specialty-specific ongoing education
- Full Practice Authority: Independent practice with direct licensing by nursing board
- Reduced Practice: Collaborative practice with physicians with some independent functions
- Restricted Practice: Practice under physician supervision or delegation
- Dual Regulation: Oversight by both nursing and medical regulatory boards
- Title Protection Only: Regulation of title use without specific scope provisions
Regulatory Issues Specific to Advanced Practice
| Regulatory Issue | Description | Implications |
|---|---|---|
| Scope of Practice | Definition of authorized activities for advanced practitioners | Determines services that can be legally provided and boundaries of practice |
| Prescriptive Authority | Legal permission to prescribe medications and controlled substances | Affects ability to provide comprehensive care and practice autonomy |
| Physician Collaboration | Requirements for formal relationships with physicians | Influences practice independence and geographic distribution of services |
| Reimbursement Policies | Regulations affecting payment for advanced practice services | Impacts financial viability of practice and access to services |
| Title Protection | Legal restrictions on who can use advanced practice titles | Protects public from misrepresentation and unqualified practitioners |
| Interstate Practice | Regulations governing practice across jurisdictional boundaries | Affects mobility and ability to provide telehealth services |
| Specialty Recognition | Formal acknowledgment of specialized competencies | Influences career advancement and practice opportunities |
Role of Professional Organizations in Advanced Practice Regulation
Professional nursing organizations play vital roles in shaping the regulatory environment for advanced practice nurses:
- Developing and maintaining specialty certification examinations
- Establishing standards for advanced practice education programs
- Advocating for appropriate scope of practice legislation
- Providing continuing education for specialty competency maintenance
- Developing evidence-based practice guidelines
- Representing advanced practice concerns to regulatory bodies
- Conducting research on advanced practice outcomes and effectiveness
Advanced Practice Compliance:
Advanced practice nurses must be particularly vigilant about regulatory compliance due to their expanded responsibilities:
- Maintain clear understanding of scope boundaries in their jurisdiction
- Keep specialty certifications and advanced practice licenses current
- Adhere to collaboration agreement requirements where applicable
- Follow prescriptive authority regulations and limitations
- Document practice activities according to advanced practice standards
- Maintain appropriate professional liability insurance for advanced practice
- Stay informed about legislative and regulatory changes affecting practice
6. Learning Aids
6.1 Mnemonics for Key Concepts
Mnemonics are memory aids that help you remember complex information. Here are some useful mnemonics for professional considerations in nursing:
“ETHICAL” – Ethical Principles in Nursing
E – Equality and justice for all patients
T – Truth-telling and honesty in communication
H – Human dignity and respect for all
I – Integrity in professional practice
C – Confidentiality of patient information
A – Autonomy of patient decisions
L – Loyalty to patients and profession
“REGULATE” – Regulatory Functions in Nursing
R – Registration of qualified nurses
E – Education standards establishment
G – Guidance for professional practice
U – Upholding professional conduct
L – Licensure of nursing professionals
A – Accreditation of nursing programs
T – Testing competency through examinations
E – Enforcement of practice standards
“SCOPE” – Elements of Nursing Scope of Practice
S – Skills and competencies required
C – Clinical judgment and decision-making
O – Obligations to patients and profession
P – Practice boundaries and limitations
E – Education and qualifications needed
“LEGAL” – Legal Aspects in Nursing
L – Licensure requirements compliance
E – Evidence-based practice standards
G – Governance by nursing practice acts
A – Accountability for professional actions
L – Liability awareness and prevention
“NEGLIGENCE” – Elements and Prevention of Negligence
N – Notice the standard of care required
E – Establish a duty of care to the patient
G – Guard against breaching that duty
L – Link between breach and harm must exist (causation)
I – Injury or damage must be present
G – Good documentation is essential
E – Education to maintain competence
N – Never practice beyond your scope
C – Consult when uncertain about care
E – Evaluate outcomes of interventions
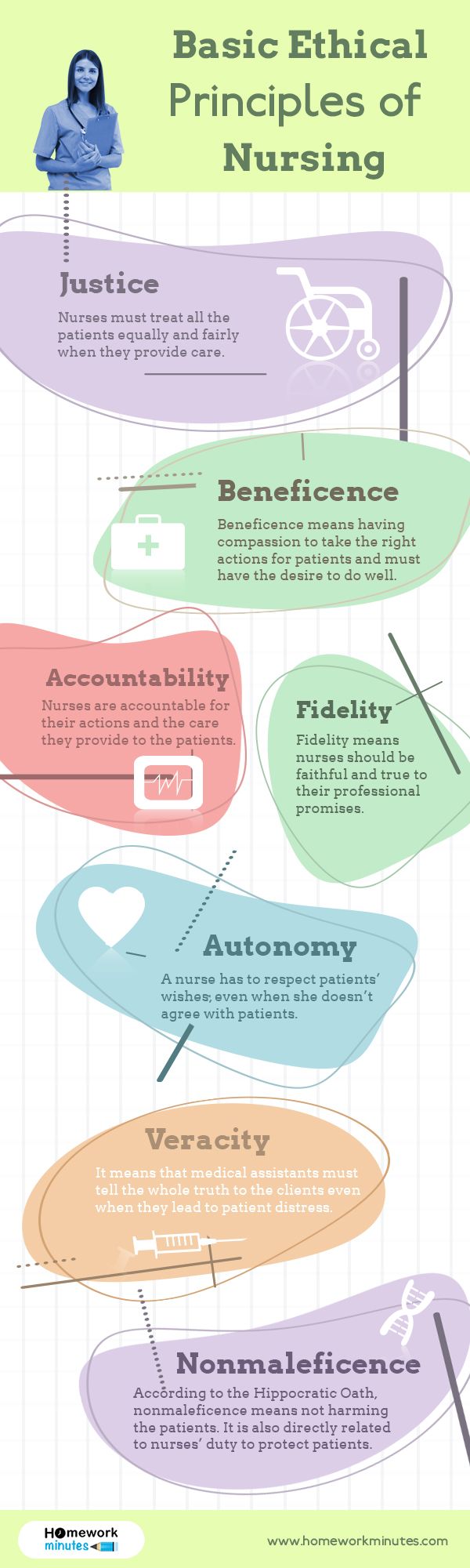
Figure 7: Basic Ethical Principles in Nursing Practice
6.2 Summary and Key Takeaways
Nursing as a Profession
- Nursing is characterized by specialized knowledge, autonomy, ethics, service orientation, and commitment
- Nursing philosophy guides practice through beliefs about humans, health, and nursing roles
- Professional nursing aims to promote health, prevent illness, alleviate suffering, and advance the profession
Regulatory Bodies
- INC and SNCs establish and enforce standards for nursing education and practice
- These bodies protect the public through registration, accreditation, and professional standard-setting
- A two-tier regulatory system allows both national uniformity and state-specific adaptations
Professional Ethics
- Codes of ethics provide guidance for professional conduct and ethical decision-making
- Practice standards establish benchmarks for quality nursing care
- ICN influences nursing ethics and regulation worldwide through global standards
Legal Aspects in Nursing
- Consumer protection and patient rights establish legal obligations for nurses
-
