Psychopharmacology Notes
Antipsychotics & Antidepressants
Comprehensive review for nursing students
ANTIPSYCHOTICS
Overview
Antipsychotics are a class of medications primarily used to manage psychosis (including delusions, hallucinations, paranoia, or disordered thought), particularly in schizophrenia and bipolar disorder. They’re sometimes called neuroleptics or major tranquilizers.
Key Points
- First developed in the 1950s
- Work primarily by blocking dopamine receptors
- Divided into two main generations: typical (first-generation) and atypical (second-generation)
- Used for schizophrenia, bipolar disorder, severe depression, and other conditions
Classification of Antipsychotics
First-Generation (Typical)
First-generation antipsychotics are older drugs that primarily block dopamine D₂ receptors.
- Haloperidol (Haldol) – High potency
- Chlorpromazine (Thorazine) – Low potency
- Fluphenazine (Prolixin)
- Perphenazine (Trilafon)
- Thioridazine (Mellaril)
- Trifluoperazine (Stelazine)
Second-Generation (Atypical)
Second-generation antipsychotics block both dopamine D₂ and serotonin 5-HT₂A receptors.
- Clozapine (Clozaril) – First atypical
- Risperidone (Risperdal)
- Olanzapine (Zyprexa)
- Quetiapine (Seroquel)
- Ziprasidone (Geodon)
- Aripiprazole (Abilify)
- Paliperidone (Invega)
Typical vs. Atypical Comparison
| Feature | First-Generation (Typical) | Second-Generation (Atypical) |
|---|---|---|
| Primary receptor | Dopamine D₂ | Dopamine D₂ and Serotonin 5-HT₂A |
| EPS risk | Higher | Lower |
| Negative symptoms | Less effective | More effective |
| Metabolic effects | Lower risk | Higher risk |
| Cost | Less expensive | More expensive |
Mechanism of Action
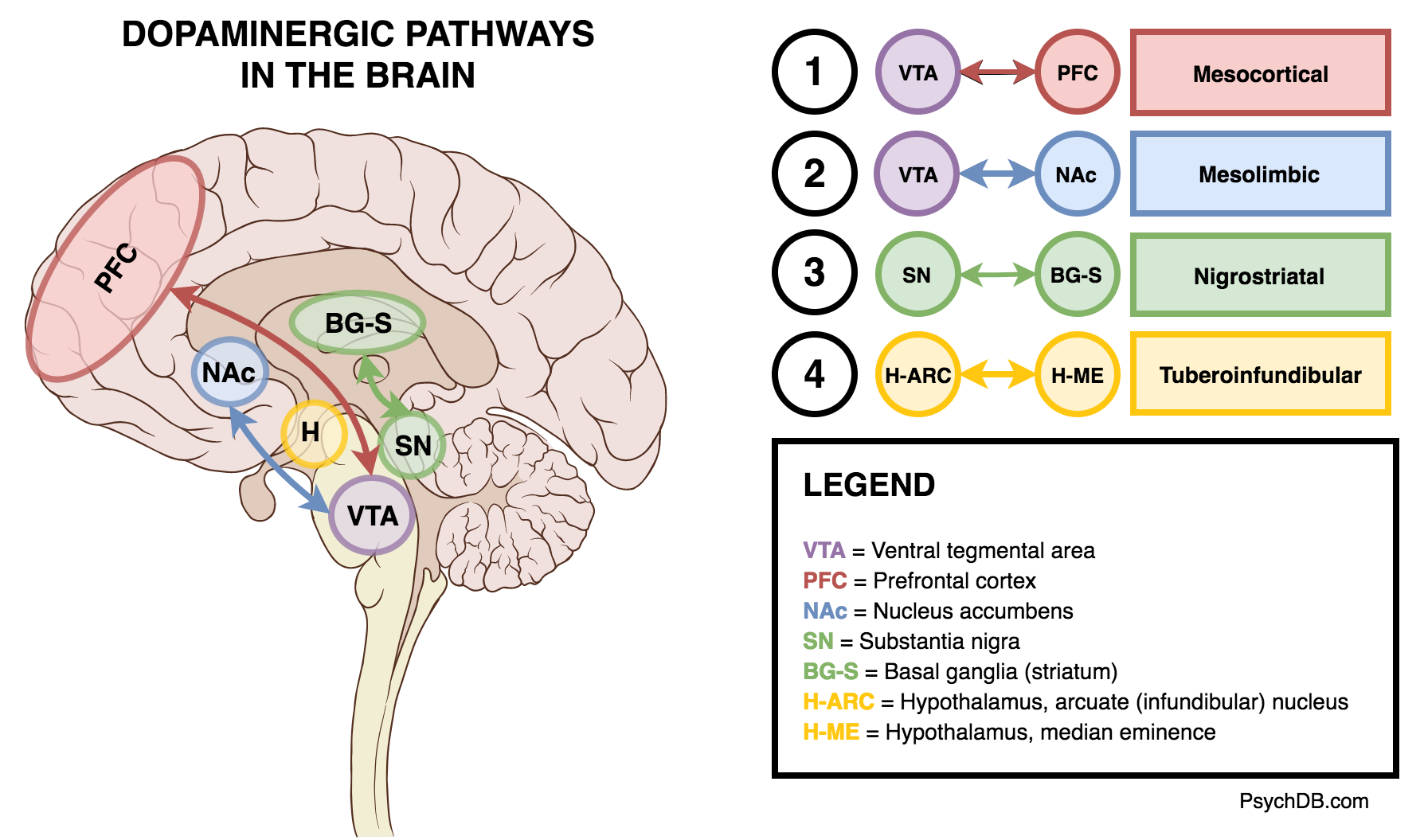
Figure: Dopamine pathways in the brain affected by antipsychotics.
Dopamine Hypothesis of Schizophrenia
The dopamine hypothesis suggests that schizophrenia symptoms result from excessive dopaminergic activity in the mesolimbic pathway (positive symptoms) and reduced dopaminergic activity in the mesocortical pathway (negative symptoms).
Typical Antipsychotics
- Block dopamine D₂ receptors
- Effective for positive symptoms (hallucinations, delusions)
- Less effective for negative symptoms (apathy, social withdrawal)
- Strong binding to D₂ receptors in all pathways
Atypical Antipsychotics
- Block dopamine D₂ and serotonin 5-HT₂A receptors
- 5-HT₂A antagonism increases dopamine release in nigrostriatal and mesocortical pathways
- Faster dissociation from D₂ receptors (“hit-and-run” binding)
- Improved efficacy for negative symptoms
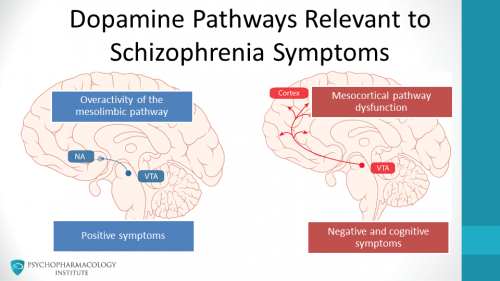
Figure: Mechanism of action of antipsychotic agents at the dopamine receptor.
Indications
| Primary Indications | Off-Label Uses |
|---|---|
|
|
Black Box Warning
Antipsychotics have a black box warning for increased mortality in elderly patients with dementia-related psychosis. They are not approved for treating dementia-related psychosis.
Specialized Uses
- Clozapine (Clozaril): Reserved for treatment-resistant schizophrenia due to risk of agranulocytosis
- Aripiprazole (Abilify): Partial agonist at D₂ receptors (“dopamine stabilizer”)
- Quetiapine (Seroquel): Often used for sleep and anxiety due to sedative effects
Side Effects
| System | Side Effects | Mechanism |
|---|---|---|
| CNS | Sedation, dizziness, headache, seizures (dose-dependent) | Histamine H₁ receptor antagonism |
| Cardiovascular | Orthostatic hypotension, QT prolongation, tachycardia | Alpha-1 adrenergic blockade, cardiac ion channel effects |
| Anticholinergic | Dry mouth, blurred vision, constipation, urinary retention | Muscarinic receptor antagonism |
| Metabolic | Weight gain, hyperglycemia, dyslipidemia, diabetes | H₁ antagonism, 5-HT₂C antagonism |
| Endocrine | Hyperprolactinemia (galactorrhea, gynecomastia, amenorrhea) | D₂ receptor blockade in tuberoinfundibular pathway |
| Neurological | Extrapyramidal symptoms (EPS), tardive dyskinesia | D₂ receptor blockade in nigrostriatal pathway |
| Severe | Neuroleptic malignant syndrome, agranulocytosis (clozapine) | D₂ blockade in hypothalamus, immune effects |
Mnemonic: “A DIME”
Common side effects of antipsychotics:
- Anticholinergic effects (dry mouth, constipation, urinary retention)
- Dizziness (orthostatic hypotension)
- Increased prolactin levels
- Metabolic effects (weight gain, diabetes)
- Extrapyramidal symptoms
Extrapyramidal Symptoms (EPS)
Extrapyramidal symptoms are movement disorders that result from dopamine blockade in the nigrostriatal pathway. They are more common with typical antipsychotics but can occur with atypicals as well.

Figure: Types of extrapyramidal symptoms.
Types of EPS
| Type | Characteristics | Onset |
|---|---|---|
| Acute Dystonia | Sustained muscle contractions, twisted posture, oculogyric crisis | Hours to days |
| Akathisia | Subjective feeling of restlessness, inability to sit still | Days to weeks |
| Parkinsonism | Bradykinesia, rigidity, tremor, mask-like face | Weeks to months |
| Tardive Dyskinesia | Involuntary, repetitive movements (lips, tongue, face, limbs) | Months to years |
Management of EPS
- Acute Dystonia: IV/IM anticholinergics (benztropine, diphenhydramine)
- Akathisia: Beta-blockers (propranolol), benzodiazepines
- Parkinsonism: Anticholinergics (benztropine, trihexyphenidyl), amantadine
- Tardive Dyskinesia: Switch to atypical antipsychotic, consider VMAT2 inhibitors (valbenazine, deutetrabenazine)
Mnemonic: “ADAPT”
Timeline of EPS development:
- Acute Dystonia (hours to days)
- Akathisia (days to weeks)
- Parkinsonism (weeks to months)
- Tardive dyskinesia (months to years)
Nursing Considerations
Assessment
- Baseline mental status and psychiatric symptoms
- Baseline vitals, weight, BMI
- Extrapyramidal symptoms evaluation
- Metabolic parameters (glucose, lipids)
- ECG for QT interval (baseline)
- History of seizures, cardiovascular disease
- Medication history and potential interactions
Monitoring
- Effectiveness of therapy (symptom improvement)
- Signs of extrapyramidal symptoms
- Blood pressure and orthostatic changes
- Weight changes and metabolic parameters
- Medication adherence
- Suicidal ideation
- For clozapine: Regular WBC monitoring
Special Nursing Considerations
- Clozapine: Requires registration in REMS program, weekly WBC monitoring initially
- Depot/Long-Acting Injections: Observe for injection site reactions, administer using proper technique
- Elderly Patients: Use lower doses, monitor closely for falls and cognitive changes
- Pregnant Patients: Assess risk/benefit ratio, monitor for neonatal EPS if used in third trimester
Neuroleptic Malignant Syndrome (NMS)
A life-threatening emergency characterized by:
- Fever
- Muscle rigidity
- Altered mental status
- Autonomic instability
Action: Discontinue antipsychotic immediately, provide supportive care, transfer to emergency department.
Patient Education
Key Teaching Points
- Take medication as prescribed, even when feeling better
- Full therapeutic effect may take 4-6 weeks
- Do not abruptly stop medication (risk of withdrawal symptoms)
- Avoid alcohol and recreational drugs
- Use caution with driving or operating machinery until effects are known
- Use sunscreen and protective clothing (increased photosensitivity)
- Take with food if GI upset occurs
When to Seek Medical Care
- Muscle stiffness, tremors, restlessness, or abnormal movements
- Severe dizziness or fainting
- Significant weight gain or increased thirst/urination
- Fever with muscle stiffness and confusion
- Worsening of psychiatric symptoms
- Suicidal thoughts or behaviors
Lifestyle Recommendations
- Maintain regular physical activity to combat weight gain
- Follow a balanced diet low in simple sugars
- Stay hydrated (especially if experiencing dry mouth)
- Establish regular sleep patterns
- Use memory aids for medication adherence (pill boxes, phone alarms)
- Continue psychotherapy as recommended
ANTIDEPRESSANTS
Overview
Antidepressants are medications used to treat depression and various other disorders by correcting chemical imbalances of neurotransmitters in the brain. They primarily affect the levels of serotonin, norepinephrine, and dopamine.
Key Points
- Multiple classes with different mechanisms of action
- Usually take 2-4 weeks for full therapeutic effect
- Used for depression, anxiety disorders, OCD, PTSD, and other conditions
- Selection based on symptoms, side effect profile, and patient history
Classification of Antidepressants
| Class | Examples | Primary Mechanism |
|---|---|---|
| Selective Serotonin Reuptake Inhibitors (SSRIs) | Fluoxetine (Prozac), Sertraline (Zoloft), Escitalopram (Lexapro), Paroxetine (Paxil), Citalopram (Celexa) | Inhibit serotonin reuptake |
| Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) | Venlafaxine (Effexor), Duloxetine (Cymbalta), Desvenlafaxine (Pristiq) | Inhibit serotonin and norepinephrine reuptake |
| Tricyclic Antidepressants (TCAs) | Amitriptyline, Nortriptyline, Imipramine, Desipramine | Inhibit serotonin and norepinephrine reuptake; anticholinergic effects |
| Monoamine Oxidase Inhibitors (MAOIs) | Phenelzine (Nardil), Tranylcypromine (Parnate), Selegiline (Emsam) | Inhibit monoamine oxidase enzyme |
| Atypical Antidepressants | Bupropion (Wellbutrin), Mirtazapine (Remeron), Trazodone | Various mechanisms including dopamine/norepinephrine reuptake inhibition |

Figure: Simplified algorithm for antidepressant selection.
Selective Serotonin Reuptake Inhibitors (SSRIs)

Figure: Mechanism of action of SSRIs.
Common SSRIs
- Fluoxetine (Prozac): Longest half-life, most activating
- Sertraline (Zoloft): Moderate side effect profile, mild dopaminergic activity
- Escitalopram (Lexapro): Fewest drug interactions, well-tolerated
- Paroxetine (Paxil): Most anticholinergic, higher withdrawal risk
- Citalopram (Celexa): Dose-dependent QT prolongation
Indications
- Major depressive disorder
- Generalized anxiety disorder
- Panic disorder
- Social anxiety disorder
- Obsessive-compulsive disorder
- Post-traumatic stress disorder
- Premenstrual dysphoric disorder
Mnemonic: “SSRI Fun PECs”
Common SSRIs:
- Fluoxetine (Prozac)
- Paroxetine (Paxil)
- Escitalopram (Lexapro)
- Citalopram (Celexa)
- Sertraline (Zoloft)
Side Effects of SSRIs
- Nausea, vomiting, diarrhea (usually transient)
- Headache, insomnia or somnolence
- Sexual dysfunction (decreased libido, delayed orgasm)
- Increased anxiety (initially)
- Weight changes (usually minimal)
- Serotonin syndrome (with other serotonergic medications)
- Increased risk of bleeding (with NSAIDs, anticoagulants)
Black Box Warning
SSRIs carry a black box warning for increased risk of suicidal thinking and behavior in children, adolescents, and young adults up to 24 years of age.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)

Figure: Mechanism of action of SNRIs.
Common SNRIs
- Venlafaxine (Effexor): Dose-dependent NE effects, discontinuation symptoms
- Duloxetine (Cymbalta): Approved for pain conditions, diabetic neuropathy
- Desvenlafaxine (Pristiq): Active metabolite of venlafaxine
- Levomilnacipran (Fetzima): More balanced 5-HT/NE effects
Indications
- Major depressive disorder
- Generalized anxiety disorder
- Pain conditions (fibromyalgia, chronic musculoskeletal pain)
- Diabetic peripheral neuropathic pain
- Stress urinary incontinence (duloxetine)
Side Effects of SNRIs
- Similar to SSRIs: nausea, dry mouth, headache, insomnia
- Increased blood pressure and heart rate (noradrenergic effect)
- Excessive sweating
- Sexual dysfunction
- Withdrawal symptoms if discontinued abruptly
SNRIs may be more effective than SSRIs for pain conditions and depression with prominent fatigue or psychomotor retardation.
Tricyclic Antidepressants (TCAs)

Figure: Mechanism of action of TCAs.
Common TCAs
- Amitriptyline: Most sedating, strongest anticholinergic effects
- Nortriptyline: Better tolerated, therapeutic window
- Imipramine: Balanced 5-HT/NE effects
- Desipramine: Most noradrenergic, least anticholinergic
- Clomipramine: Strong for OCD due to serotonergic effects
Indications
- Major depressive disorder (second-line)
- Neuropathic pain
- Migraine prophylaxis
- Obsessive-compulsive disorder (clomipramine)
- Nocturnal enuresis in children
- Insomnia (low-dose amitriptyline, doxepin)
Mnemonic: “TCA Side Effects – SAD ABCS”
- Sedation (antihistaminic)
- Anticholinergic effects (dry mouth, constipation, urinary retention)
- Dizziness (alpha-1 blockade)
- Arrhythmias (QT prolongation, heart block)
- Blood pressure changes (alpha-1 blockade)
- Cardiotoxicity in overdose
- Seizure threshold lowered
TCA Toxicity
TCAs have a narrow therapeutic index and can be lethal in overdose. Signs of toxicity include:
- Anticholinergic crisis (hyperthermia, delirium, tachycardia)
- Cardiovascular effects (prolonged QRS, arrhythmias)
- Seizures
- Coma
Monoamine Oxidase Inhibitors (MAOIs)

Figure: Mechanism of action of MAOIs.
Common MAOIs
- Phenelzine (Nardil)
- Tranylcypromine (Parnate)
- Selegiline (Emsam) – transdermal patch, more selective for MAO-B
- Isocarboxazid (Marplan)
Indications
- Treatment-resistant depression
- Atypical depression
- Depression with prominent anxiety or panic
- Social anxiety disorder
- Parkinson’s disease (selegiline)
Hypertensive Crisis Risk
MAOIs can cause potentially fatal hypertensive crises when combined with:
- Tyramine-containing foods (aged cheeses, cured meats, draft beer, fermented foods)
- Sympathomimetic medications (decongestants, stimulants)
- Serotonergic medications (risk of serotonin syndrome)
Symptoms include severe headache, neck stiffness, nausea, vomiting, sweating, and dramatically elevated blood pressure.
Mnemonic: “MAOI – Tyramine Foods”
Foods to avoid with MAOIs: “CATS”
- Cheese (aged)
- Alcohol (especially red wine, beer)
- Tofu/Tempeh (fermented)
- Sausage/Salami (cured meats)
Antidepressant Side Effects Comparison
| Side Effect | SSRIs | SNRIs | TCAs | MAOIs |
|---|---|---|---|---|
| Anticholinergic | + | + | ++++ | ++ |
| Sedation | + | + | +++ | ++ |
| Sexual dysfunction | +++ | +++ | ++ | ++ |
| GI effects | +++ | +++ | ++ | ++ |
| Weight gain | ++ | + | +++ | ++ |
| Cardiac effects | + | ++ | +++ | ++ |
| Withdrawal | ++ | +++ | ++ | + |
| Dietary restrictions | No | No | No | Yes |
| Overdose lethality | + | ++ | ++++ | +++ |
+ = minimal/mild, ++ = moderate, +++ = significant, ++++ = severe
Serotonin Syndrome
A potentially life-threatening condition caused by excessive serotonergic activity, usually from combining multiple serotonergic medications.
Symptoms: The triad of altered mental status, autonomic instability, and neuromuscular abnormalities.
- Agitation, confusion, delirium
- Hyperthermia, diaphoresis, tachycardia, hypertension
- Hyperreflexia, clonus, tremor, muscle rigidity
Action: Discontinue serotonergic agents, provide supportive care, consider benzodiazepines, and in severe cases, consider serotonin antagonists like cyproheptadine.
Nursing Considerations
Assessment
- Baseline depressive/anxiety symptoms using standardized scales
- Suicidal ideation and risk assessment
- History of bipolar disorder (risk of inducing mania)
- Medication history and potential interactions
- Baseline vital signs, weight
- Cardiac status (especially for TCAs)
- Liver and kidney function
Monitoring
- Therapeutic response (2-4 weeks for initial effects)
- Suicidal ideation, especially in first few weeks
- Side effects specific to drug class
- Weight changes
- Blood pressure (especially with SNRIs, MAOIs)
- For TCAs: Cardiac symptoms, QT interval
- Medication adherence
Increased Suicide Risk
Closely monitor for increased suicidal thoughts, especially:
- During the first few weeks of treatment
- When dosage is changed (increased or decreased)
- In children, adolescents, and young adults
Administration Considerations
- SSRIs: Can be taken with or without food, usually in the morning (except for sedating ones)
- SNRIs: Take with food to reduce GI side effects
- TCAs: Often given at bedtime to minimize daytime sedation
- MAOIs: Ensure patient understands dietary restrictions
- Do not abruptly discontinue any antidepressant
- Many antidepressants have significant drug interactions
Patient Education
Key Teaching Points
- Take medication as prescribed, even when feeling better
- Full therapeutic effect may take 2-4 weeks
- Do not stop medication abruptly (risk of discontinuation syndrome)
- Avoid alcohol (increases CNS depression)
- Report any thoughts of self-harm immediately
- Use caution with driving or operating machinery until effects are known
- Take medication at the same time each day
When to Seek Medical Care
- Thoughts of suicide or self-harm
- Unusual changes in mood, behavior, or energy level
- Severe agitation, restlessness, or panic attacks
- Signs of serotonin syndrome
- Severe headache (with MAOIs)
- Persistent or severe side effects
- Symptoms of allergic reaction
Mnemonic: “WARM HELP”
Antidepressant discontinuation syndrome symptoms:
- Wooziness (dizziness)
- Affective symptoms (irritability, anxiety)
- Returning symptoms (depression)
- Movement problems (tremor, unsteady gait)
- Headache
- Electric shocks (brain zaps)
- Lethargy
- Paresthesias (tingling, numbness)
Lifestyle Recommendations
- Regular exercise (helps improve mood)
- Balanced diet
- Regular sleep schedule
- Stress management techniques
- Support groups or therapy
- Avoid caffeine if experiencing anxiety or insomnia
- Use memory aids for medication adherence
Summary: Medication Selection Quick Guide
Antipsychotics
- First episode psychosis: Second-generation (lower EPS risk)
- Treatment-resistant schizophrenia: Clozapine
- Acute agitation: Haloperidol, olanzapine, risperidone
- Negative symptoms: Second-generation preferred
- Elderly patients: Low-dose second-generation
- Bipolar disorder: Olanzapine, quetiapine, risperidone, aripiprazole
Antidepressants
- First-line depression: SSRIs (fluoxetine, sertraline, escitalopram)
- Depression with pain: Duloxetine or other SNRIs
- Insomnia with depression: Mirtazapine, trazodone, or sedating TCA
- Anxiety disorders: SSRIs, SNRIs
- OCD: SSRIs (higher doses), clomipramine
- Treatment-resistant: Augmentation strategies, MAOIs
Final Thoughts
Psychopharmacology requires an individualized approach. Medication selection should consider:
- Symptom profile
- Previous response to medications
- Side effect profile and tolerability
- Medical comorbidities
- Potential drug interactions
- Patient preferences
Remember that medication is often most effective when combined with appropriate psychotherapy and lifestyle modifications.
Created by Soumya Ranjan Parida for nursing education purposes. Last updated: April 2025.
Mood Stabilizers & Anxiolytics
Nursing Pharmacology | Comprehensive Notes
Introduction
Mood stabilizers and anxiolytics are two crucial classes of psychotropic medications used to treat various psychiatric conditions. This comprehensive guide explores their mechanisms, indications, side effects, and important nursing considerations to help you provide optimal care for patients receiving these medications.
Mood Stabilizers
Medications that help control the extreme highs (mania) and lows (depression) of bipolar disorder and other mood disorders.
- Lithium (the gold standard)
- Anticonvulsants (Valproic acid, Carbamazepine, Lamotrigine)
- Atypical antipsychotics (also used as mood stabilizers)
Anxiolytics
Medications that reduce symptoms of anxiety, nervousness, and psychological distress.
- Benzodiazepines (rapid-acting anxiolytics)
- Buspirone (non-benzodiazepine anxiolytic)
- SSRIs & SNRIs (for long-term anxiety management)
- Beta-blockers (for specific anxiety situations)
Mood Stabilizers
Lithium
Mechanism of Action
Lithium works through multiple mechanisms, including:
- Inhibition of inositol monophosphatase, decreasing inositol recycling
- Inhibition of glycogen synthase kinase-3 (GSK-3)
- Modulation of neurotransmitter release (serotonin, dopamine, norepinephrine)
- Regulation of second messenger systems
Indications
- Acute manic episodes in bipolar disorder
- Maintenance treatment for bipolar disorder
- Augmentation in treatment-resistant depression
- Prevention of suicide in mood disorders
Therapeutic Blood Levels
- Acute mania: 0.8-1.2 mEq/L
- Maintenance therapy: 0.6-0.8 mEq/L
- Toxicity risk: >1.5 mEq/L
- Geriatric patients: 0.4-0.8 mEq/L
Adverse Effects
- L – Loss of appetite
- I – Increased urination (polyuria)
- T – Tremor (fine hand tremor)
- H – Hyperreflexia
- I – Impaired coordination
- U – Upset stomach (nausea/vomiting)
- M – Muscle weakness
- T – Thirst (polydipsia)
- O – Obtundation (at toxic levels)
- X – Xerostomia (dry mouth)
- I – Irregular heartbeat
- C – Confusion
Nursing Considerations
- Monitor serum lithium levels regularly (every 3-6 months for stable patients)
- Check thyroid and kidney function at baseline and periodically
- Monitor electrolytes, especially sodium (hyponatremia increases lithium toxicity risk)
- Weigh patient regularly to track fluid retention or weight changes
- Assess for signs of toxicity at each visit
- Draw lithium levels 12 hours after the last dose
Patient Education
- Maintain consistent salt and fluid intake
- Take medication with food to reduce GI upset
- Avoid NSAIDs as they can increase lithium levels
- Report symptoms of toxicity immediately
- Avoid sudden medication discontinuation
- Use reliable contraception (teratogenic in pregnancy)
- Report plans for pregnancy to healthcare provider
Anticonvulsants as Mood Stabilizers
| Drug | Mechanism of Action | Primary Indication | Key Side Effects | Monitoring |
|---|---|---|---|---|
| Valproic Acid (Depakote) |
|
|
|
|
| Carbamazepine (Tegretol) |
|
|
|
|
| Lamotrigine (Lamictal) |
|
|
|
|
Valproic Acid Focus
Chemical Structure
Often first-line for mania, particularly effective for mixed episodes and rapid cycling. Has the greatest weight gain potential of these three medications.
Pregnancy Category X – contraindicated in pregnancy due to neural tube defects risk.
Carbamazepine Focus
Chemical Structure
Strong CYP450 inducer – causes many drug interactions. Requires auto-induction dosing adjustment after initiation. Effective for mood episodes with irritability or aggression.
Patients of Asian descent should undergo HLA-B*1502 testing before starting due to increased Stevens-Johnson syndrome risk.
Lamotrigine Focus
Chemical Structure
Most effective for bipolar depression. Requires slow titration to minimize rash risk. Has minimal weight gain and cognitive side effects, making it well-tolerated long-term.
Valproic acid increases lamotrigine levels – dose must be reduced by 50% when used together.
Nursing Considerations for Anticonvulsant Mood Stabilizers
- Monitor for signs of rash, especially with lamotrigine
- Assess for suicidal ideation (FDA warning for all anticonvulsants)
- Check liver function tests regularly with valproic acid
- Monitor complete blood count with carbamazepine
- Evaluate medication adherence at each visit
- Assess for drug interactions due to CYP450 effects
- Monitor serum levels when clinically indicated
Patient Education for Anticonvulsant Mood Stabilizers
- Take medication exactly as prescribed, including titration schedules
- Report any rash immediately, especially with lamotrigine
- Do not stop medication abruptly as this may trigger seizures or mood episodes
- Women of childbearing age should use effective contraception
- Avoid alcohol as it may increase sedation
- Be aware of potential drug interactions, including with oral contraceptives
- Regular blood tests are essential to monitor for side effects
Decision-Making Algorithm: Mood Stabilizer Selection
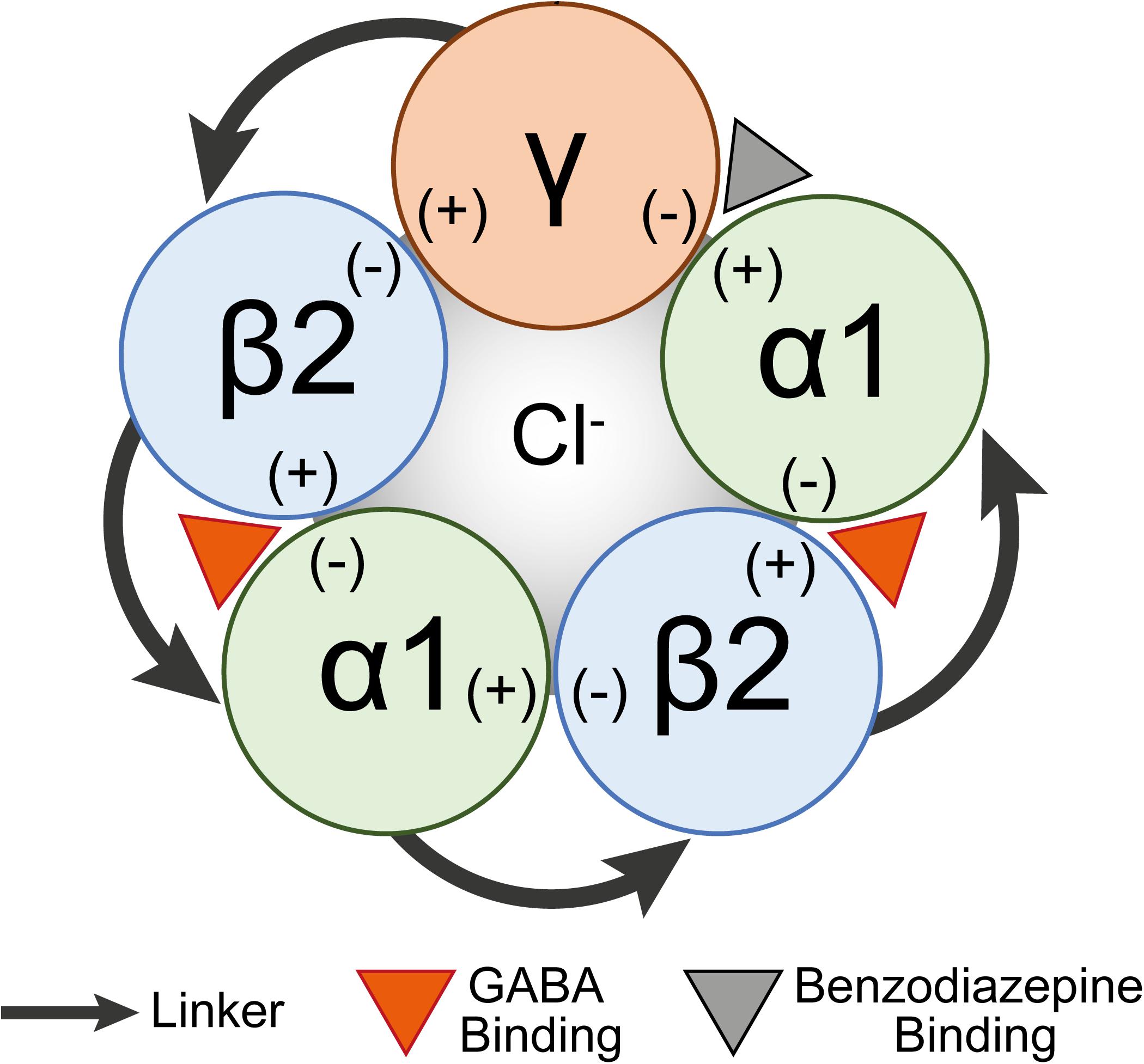
Anxiolytics (Anti-anxiety Agents)
Benzodiazepines
Mechanism of Action
Benzodiazepines enhance the effect of gamma-aminobutyric acid (GABA), the main inhibitory neurotransmitter in the CNS:
- Bind to a specific site on the GABAA receptor
- Act as positive allosteric modulators
- Increase frequency of chloride channel opening
- Result in hyperpolarization of neurons
- Decrease neuronal excitability
Common Benzodiazepines: Duration of Action and Uses
| Drug | Onset | Duration | Half-life | Primary Indications | Special Considerations |
|---|---|---|---|---|---|
| Alprazolam (Xanax) |
Rapid 30-60 min |
Short-acting | 12-15 hrs |
|
|
| Diazepam (Valium) |
Rapid 15-30 min |
Long-acting | 20-100 hrs (with active metabolites) |
|
|
| Lorazepam (Ativan) |
Intermediate 1-2 hrs (PO) 5-20 min (IV) |
Intermediate-acting | 10-20 hrs |
|
|
| Clonazepam (Klonopin) |
Intermediate 1-4 hrs |
Long-acting | 18-50 hrs |
|
|
| Triazolam (Halcion) |
Rapid 15-30 min |
Ultra-short-acting | 2-5 hrs |
|
|
Adverse Effects
- B – Balance problems, ataxia
- E – Elderly (more sensitive to effects)
- N – Nystagmus
- Z – Zzzz… (excessive sedation)
- O – Oversedation
- D – Dependence and tolerance
- I – Impaired coordination
- A – Anterograde amnesia
- Z – Zero alcohol (dangerous combination)
- E – Euphoria (risk for abuse)
- P – Psychomotor impairment
- I – Irritability (paradoxical reaction)
- N – No abrupt discontinuation
- E – Extreme withdrawal risk
Nursing Considerations
- Assess fall risk, especially in elderly patients
- Monitor for respiratory depression when combined with other CNS depressants
- Evaluate for signs of dependence or tolerance
- Implement safety measures for patients with sedation
- Monitor for paradoxical reactions (agitation, aggression)
- Be aware of benzodiazepine withdrawal syndrome (anxiety, insomnia, irritability, tremor, seizures)
- Assess for memory problems or cognitive impairment
- Use caution with patients who have a history of substance abuse
Patient Education
- Avoid alcohol and other CNS depressants
- Do not drive or operate machinery while taking benzodiazepines
- Take medication exactly as prescribed
- Do not abruptly stop taking medication
- Do not increase dose without medical advice
- Inform healthcare providers of all medications being taken
- Store medication securely away from children
- Be aware of addiction potential with long-term use
- Discuss plans for pregnancy with healthcare provider
Important Warnings
- Benzodiazepine Withdrawal Syndrome: Can be life-threatening; requires gradual tapering (10% reduction every 1-2 weeks)
- Respiratory Depression: Risk increases when combined with opioids, alcohol, or other CNS depressants
- FDA Black Box Warning: Risks when combined with opioid medications
- Pregnancy Category D: Risk of cleft lip/palate and neonatal withdrawal syndrome
- Increased risk of dementia: Long-term use associated with cognitive decline, especially in elderly
Non-Benzodiazepine Anxiolytics
Buspirone (BuSpar)
Mechanism of Action
- Partial agonist at 5-HT1A serotonin receptors
- Weak antagonist at dopamine D2 receptors
- No effect on GABA receptors (unlike benzodiazepines)
- No cross-tolerance with benzodiazepines
- No potential for physical dependence
Clinical Uses
- Generalized anxiety disorder (GAD)
- Anxiety in patients with history of substance abuse
- Augmentation for depression or OCD
- Long-term anxiety management
Key Comparisons
| Property | Buspirone | Benzodiazepines |
|---|---|---|
| Onset | 2-4 weeks | Minutes-hours |
| Sedation | Minimal | Significant |
| Dependence | None | High risk |
| Psychomotor | No impairment | Impaired |
| Alcohol | Safe | Dangerous |
Adverse Effects
- Headache
- Dizziness
- Nausea
- Nervousness or excitement
- Insomnia
- Light-headedness
- Paresthesia
Nursing Considerations
- Educate on delayed onset of action (2-4 weeks)
- Administer with food to decrease GI upset
- Monitor for serotonin syndrome if combined with SSRIs
- Assess therapeutic efficacy regularly
- Not effective for panic attacks or acute anxiety
- Safe in patients with substance use disorders
SSRIs & SNRIs for Anxiety Disorders
Mechanism of Action
SSRIs (Selective Serotonin Reuptake Inhibitors):
- Block serotonin (5-HT) reuptake transporters
- Increase serotonin availability in synaptic cleft
- Downregulate 5-HT receptors with chronic use
- Alter neuronal signaling in anxiety circuits
SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors):
- Block reuptake of both serotonin and norepinephrine
- Dual action may provide broader efficacy
- Different selectivity for transporters depending on specific drug
| Drug Class | Examples | FDA-Approved Anxiety Indications | Common Side Effects |
|---|---|---|---|
| SSRIs | Sertraline (Zoloft) |
|
|
| Paroxetine (Paxil) |
|
||
| Fluoxetine (Prozac) |
|
||
| Escitalopram (Lexapro) |
|
||
| SNRIs | Venlafaxine (Effexor XR) |
|
|
| Duloxetine (Cymbalta) |
|
||
| Desvenlafaxine (Pristiq) |
|
Nursing Considerations
- Monitor for initial worsening of anxiety in first 1-2 weeks
- Full effect may take 4-6 weeks
- Assess suicidal ideation, especially in young adults
- Monitor vital signs (especially BP with SNRIs)
- Watch for serotonin syndrome if combined with other serotonergic agents
- Taper slowly when discontinuing (especially paroxetine and venlafaxine)
- Monitor weight and appetite changes
Patient Education
- Take medication at the same time each day
- Continue medication even when feeling better
- Expect 4-6 weeks for full therapeutic effect
- Do not abruptly discontinue medication
- Report side effects, especially agitation or suicidal thoughts
- Avoid alcohol, which may worsen side effects
- Report signs of serotonin syndrome: agitation, tremor, sweating, diarrhea, high fever
- F – Fatigue/somnolence
- I – Insomnia (paradoxically)
- N – Nausea and GI disturbances
- I – Initial anxiety worsening
- S – Sexual dysfunction (delayed orgasm, decreased libido)
- H – Headache and dizziness
Other Anxiolytics
Beta-Blockers (Propranolol, Atenolol)
Used primarily for performance anxiety and social phobia.
- Mechanism: Block peripheral manifestations of anxiety (tachycardia, tremor)
- Indications: Situational/performance anxiety, stage fright
- Dosing: Propranolol 10-40mg taken 30-60 minutes before anxiety-provoking event
- Contraindications: Asthma, COPD, heart block, bradycardia
Hydroxyzine (Vistaril, Atarax)
First-generation antihistamine with anxiolytic properties.
- Mechanism: H₁ receptor antagonist with anticholinergic effects
- Indications: Acute anxiety, insomnia, pruritus
- Benefits: Non-habit forming, can be used PRN
- Side effects: Sedation, dry mouth, blurred vision
- Nursing consideration: Safe alternative to benzodiazepines for patients with history of substance abuse
Clinical Decision-Making: Anxiolytic Selection
Special Population: Elderly
- Start at lower doses (usually 1/2 of adult dose)
- Benzodiazepines increase fall risk and may worsen cognitive function
- Anticholinergic effects of hydroxyzine may cause confusion
- SSRIs preferred for chronic anxiety in elderly
- Monitor for hyponatremia with SSRIs
- Beers Criteria recommends avoiding benzodiazepines in elderly
Special Population: Pregnancy
- Benzodiazepines: Category D – associated with cleft palate when used in first trimester
- SSRIs: Most Category C – paroxetine is Category D due to cardiac defects
- SSRI use in late pregnancy may result in neonatal adaptation syndrome
- Buspirone: Category B – limited human data
- Non-pharmacological interventions should be first-line when possible
- Risk/benefit assessment crucial for all psychotropic medications
Summary and Review
Mood Stabilizers
- S – Serum levels monitoring required (especially lithium)
- T – Teratogenic effects (pregnancy category D or X)
- A – Adverse effects vary by medication
- B – Bipolar disorder (main indication)
- L – Lithium has narrow therapeutic index
- E – Educate patients on adherence importance
- M – Monitor for toxicity signs
- O – Observe for suicidal ideation
- O – Onset of action takes weeks
- D – Drug interactions are common
- S – Slow tapering required for discontinuation
Anxiolytics
- C – Chronic use of benzodiazepines can cause dependence
- A – Acute vs. chronic anxiety guides medication choice
- L – Long-term treatment usually uses SSRIs/SNRIs
- M – Monitoring for side effects is essential
- A – Avoid abrupt discontinuation
- N – Non-benzodiazepines may be preferable
- X – Expect delayed onset with SSRIs/buspirone
- I – Initial worsening of anxiety may occur with SSRIs
- E – Elderly require dose adjustments
- T – Tolerance develops to benzodiazepines
- Y – Young adults have increased suicide risk with SSRIs
Key Nursing Responsibilities
Assessment
- Comprehensive psychiatric history
- Baseline vital signs and physical assessment
- Medication history and potential interactions
- Substance use history
- Risk assessment for suicidal ideation
- Comorbid medical conditions
Monitoring
- Therapeutic and adverse effects
- Drug levels for lithium, valproate, carbamazepine
- Vital signs, especially with SNRIs
- Laboratory tests (CBC, LFTs, electrolytes)
- Weight and metabolic parameters
- Treatment adherence
Patient Education
- Medication purpose, effects, and side effects
- Importance of adherence
- When to seek medical attention
- Avoidance of abrupt discontinuation
- Lifestyle modifications to enhance treatment
- Contraceptive needs with teratogenic medications
References
- 1. Leucht, S., Helfer, B., Dold, M., Kissling, W., & McGrath, J. D. (2015). Lithium for schizophrenia. The Cochrane Database of Systematic Reviews, (10), CD003834.
- 2. Geddes, J. R., & Miklowitz, D. J. (2013). Treatment of bipolar disorder. The Lancet, 381(9878), 1672-1682.
- 3. Cipriani, A., Reid, K., Young, A. H., Macritchie, K., & Geddes, J. (2013). Valproic acid, valproate and divalproex in the maintenance treatment of bipolar disorder. The Cochrane Database of Systematic Reviews, (10), CD003196.
- 4. Malhi, G. S., Tanious, M., Das, P., Coulston, C. M., & Berk, M. (2013). Potential mechanisms of action of lithium in bipolar disorder. Current understanding. CNS Drugs, 27(2), 135-153.
- 5. Baldwin, D. S., Anderson, I. M., Nutt, D. J., Allgulander, C., Bandelow, B., den Boer, J. A., … & Wittchen, H. U. (2014). Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: a revision of the 2005 guidelines from the British Association for Psychopharmacology. Journal of Psychopharmacology, 28(5), 403-439.
- 6. Stahl, S. M. (2021). Stahl’s essential psychopharmacology: Neuroscientific basis and practical applications (5th ed.). Cambridge University Press.
- 7. Bandelow, B., Michaelis, S., & Wedekind, D. (2017). Treatment of anxiety disorders. Dialogues in Clinical Neuroscience, 19(2), 93-107.
- 8. Strawn, J. R., Geracioti, L., Rajdev, N., Clemenza, K., & Levine, A. (2018). Pharmacotherapy for generalized anxiety disorder in adult and pediatric patients: an evidence-based treatment review. Expert Opinion on Pharmacotherapy, 19(10), 1057-1070.
- 9. Bostwick, J. R., Casher, M. I., & Yasugi, S. (2012). Benzodiazepines: A versatile clinical tool. Current Psychiatry, 11(4), 54-64.
- 10. Reinhold, J. A., & Rickels, K. (2015). Pharmacological treatment for generalized anxiety disorder in adults: an update. Expert Opinion on Pharmacotherapy, 16(11), 1669-1681.
Pharmacology Notes
Stimulants, Cognitive Enhancers for Dementia, and Hypnotics & Sedatives
Table of Contents
1. Stimulants
2. Cognitive Enhancers
3. Hypnotics & Sedatives
1. CNS Stimulants
Overview
Central Nervous System (CNS) stimulants are a class of drugs that increase the activity of the brain and nervous system. They elevate levels of catecholamines (particularly dopamine and norepinephrine) in the brain, resulting in increased alertness, attention, and energy.
Common CNS Stimulants
- Amphetamines: Adderall, Dexedrine, Vyvanse
- Methylphenidate: Ritalin, Concerta
- Modafinil: Provigil
- Caffeine: Found in coffee, tea, energy drinks
- Nicotine: Found in tobacco products
Classification
- By Structure: Amphetamines, Methylphenidate, Xanthines
- By Effect: Direct-acting vs. indirect-acting
- By Use: Medical (ADHD, narcolepsy) vs. recreational
- By Legal Status: Prescription-only vs. over-the-counter
Mechanism of Action
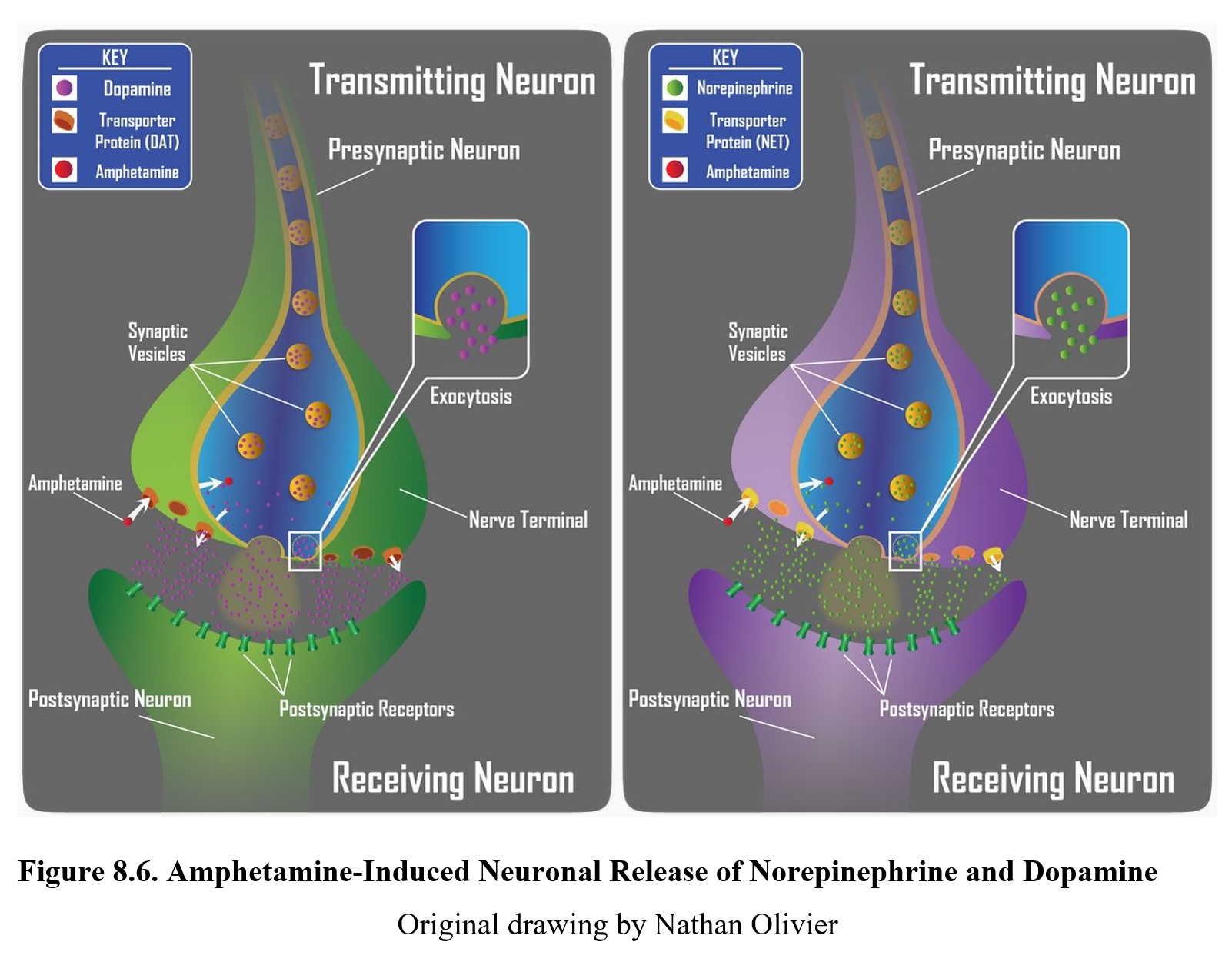
CNS stimulants primarily work by increasing the availability of neurotransmitters, especially dopamine and norepinephrine, in the synaptic cleft. This occurs through several mechanisms:
- Increased Release: Stimulate the release of catecholamines from presynaptic neurons
- Reuptake Inhibition: Block the reuptake transporters (like DAT and NET), preventing removal of neurotransmitters from the synapse
- MAO Inhibition: Some inhibit monoamine oxidase, reducing breakdown of neurotransmitters
- Receptor Agonism: Some act as direct agonists at receptors
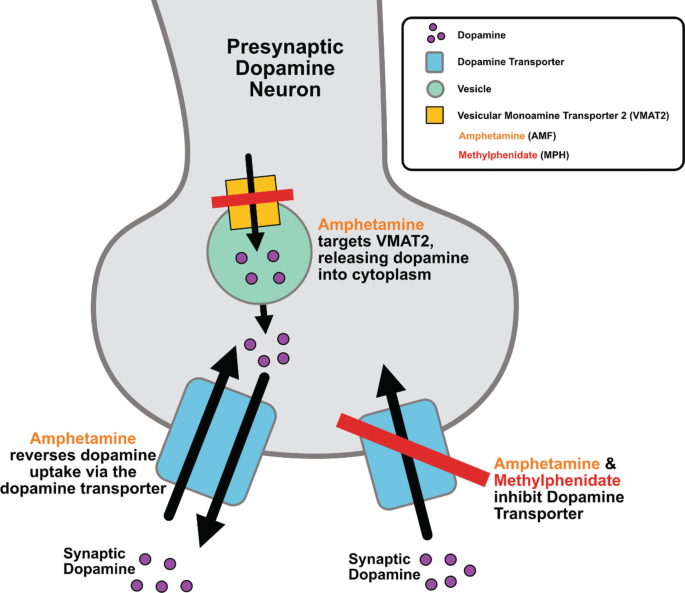
Amphetamines
Amphetamines enter the presynaptic neuron and cause release of dopamine and norepinephrine from storage vesicles. They also inhibit monoamine oxidase (MAO) and block reuptake transporters, resulting in increased neurotransmitter levels in the synapse.
Methylphenidate
Methylphenidate works primarily by blocking dopamine and norepinephrine reuptake transporters (DAT and NET). This prevents the removal of these neurotransmitters from the synapse, thereby increasing their concentration and effects.
Indications
| Indication | Medications | Rationale |
|---|---|---|
| ADHD | Adderall, Ritalin, Concerta, Vyvanse | Improve focus, reduce hyperactivity and impulsivity by enhancing dopamine and norepinephrine signaling in prefrontal cortex |
| Narcolepsy | Modafinil, Adderall, Dexedrine | Promote wakefulness and prevent sleep attacks |
| Depression (treatment-resistant) | Modafinil (adjunctive) | Enhance mood and combat fatigue when traditional antidepressants are insufficient |
| Obesity (short-term) | Phentermine | Suppress appetite and increase metabolic rate |
| Respiratory Depression | Doxapram | Stimulate respiratory center in medulla to increase respiratory rate |
Clinical Pearl
While stimulants are first-line therapy for ADHD, treatment should be individualized based on the patient’s age, symptoms, comorbidities, and potential for abuse. Non-stimulant alternatives (e.g., atomoxetine) may be preferred for patients with substance abuse history or significant anxiety.
Side Effects
Common Side Effects
- Decreased appetite and weight loss
- Insomnia and sleep disturbances
- Irritability and mood changes
- Headache
- Dry mouth
- Nausea
- Increased heart rate
- Increased blood pressure
- Rebound symptoms when drug wears off
Serious Adverse Effects
- Cardiovascular effects (arrhythmias, hypertension)
- Growth suppression in children
- Psychosis or mania
- Serotonin syndrome (with certain combinations)
- Seizures
- Severe cutaneous adverse reactions (rare)
- Physical and psychological dependence
- Sudden cardiac death (rare)
Black Box Warning
Stimulants have a high potential for abuse and dependence, particularly amphetamines. They are classified as Schedule II controlled substances. Prolonged use can lead to tolerance, psychological dependence, and withdrawal symptoms upon discontinuation.
Cardiovascular risks include sudden death in patients with pre-existing cardiac abnormalities or serious heart problems.
Nursing Considerations
Assessment
- Baseline vital signs, especially BP and HR
- Weight and height (for growth monitoring in children)
- Comprehensive cardiac history and examination
- Mental health assessment
- Sleep patterns
- Substance abuse history
- Complete medication review for potential interactions
Monitoring
- Regular monitoring of vital signs
- Weight checks (weekly initially)
- Growth parameters in children
- Mental status changes
- Sleep patterns
- Development of tics or other movement disorders
- Signs of abuse or diversion
Patient Education
- Take medication exactly as prescribed
- Immediate-release formulations typically taken twice daily, after breakfast and in early afternoon
- Extended-release formulations taken once daily, usually in the morning
- Avoid evening doses as they may interfere with sleep
- Monitor for and report concerning side effects
- Avoid abrupt discontinuation
- Avoid caffeine, which may exacerbate side effects
- Store securely to prevent theft or misuse
- Use of drug should be disclosed to all healthcare providers
Contraindications
- Cardiovascular disease
- Moderate to severe hypertension
- Hyperthyroidism
- Glaucoma
- History of substance abuse
- During or within 14 days of MAOI administration
- Known hypersensitivity
Drug Interactions
- MAOIs: Hypertensive crisis, hyperpyrexia
- SSRIs: Increased risk of serotonin syndrome
- Antihypertensives: Reduced effectiveness
- Anticonvulsants: Changed seizure threshold
- Antacids/GI acidifiers: Altered absorption
- Caffeine: Additive stimulant effects
Memory Aids
STIMULANTS Mnemonic
Use this mnemonic to remember common side effects:
- S – Sleep disturbances (insomnia)
- T – Tachycardia
- I – Irritability
- M – Mood changes
- U – Urinary retention
- L – Loss of appetite
- A – Anxiety
- N – Nausea
- T – Tremor
- S – Sweating
DOPAMINE Mnemonic
Remember stimulant mechanism of action:
- D – Decreases reuptake
- O – Opens vesicles to release more
- P – Promotes synthesis
- A – Adrenergic activation
- M – MAO inhibition (some)
- I – Increases neurotransmitter release
- N – NET and DAT blockade
- E – Enhances synaptic concentration
Visual Memory Aid: Stimulants Timeline
Short-Acting
4-6 hours
Methylphenidate IR
Dextroamphetamine IR
Intermediate
6-8 hours
Ritalin SR
Adderall
Long-Acting
8-12 hours
Concerta
Adderall XR
Extended
12-16 hours
Vyvanse
Mydayis
Very Long
>16 hours
Modafinil
Armodafinil
2. Cognitive Enhancers for Dementia
Overview
Cognitive enhancers, also known as anti-dementia drugs, are medications designed to improve memory, attention, and other cognitive functions in patients with dementia. These drugs do not cure or stop the progression of dementia but may temporarily slow cognitive decline and improve quality of life.
Types of Cognitive Enhancers
- Cholinesterase Inhibitors: Donepezil (Aricept), Rivastigmine (Exelon), Galantamine (Razadyne)
- NMDA Receptor Antagonists: Memantine (Namenda)
- Combination Therapy: Donepezil + Memantine (Namzaric)
- Amyloid-Targeting Therapies: Aducanumab (Aduhelm), Lecanemab (Leqembi)
Dementia Types
- Alzheimer’s Disease: Most common form (60-80% of cases)
- Vascular Dementia: Due to impaired blood flow to the brain
- Lewy Body Dementia: Characterized by protein deposits in nerve cells
- Frontotemporal Dementia: Affects frontal and temporal lobes
- Mixed Dementia: Combination of multiple types
Dementia Pathophysiology
Dementia involves progressive neuronal damage and death, resulting in cerebral atrophy and cognitive impairment. In Alzheimer’s disease, key pathological features include:
- Beta-amyloid plaques outside neurons
- Neurofibrillary tangles (tau protein) inside neurons
- Loss of connections between neurons
- Inflammation and immune system activation
- Neurotransmitter imbalances, particularly reduced acetylcholine
Mechanism of Action
Cognitive enhancers work through different mechanisms to improve neuronal function and communication:
Cholinesterase Inhibitors
These drugs inhibit the enzyme acetylcholinesterase, which is responsible for breaking down acetylcholine in the synaptic cleft. This results in:
- Increased acetylcholine levels in the brain
- Enhanced cholinergic neurotransmission
- Improved cognitive function
Examples: Donepezil (Aricept), Rivastigmine (Exelon), Galantamine (Razadyne)
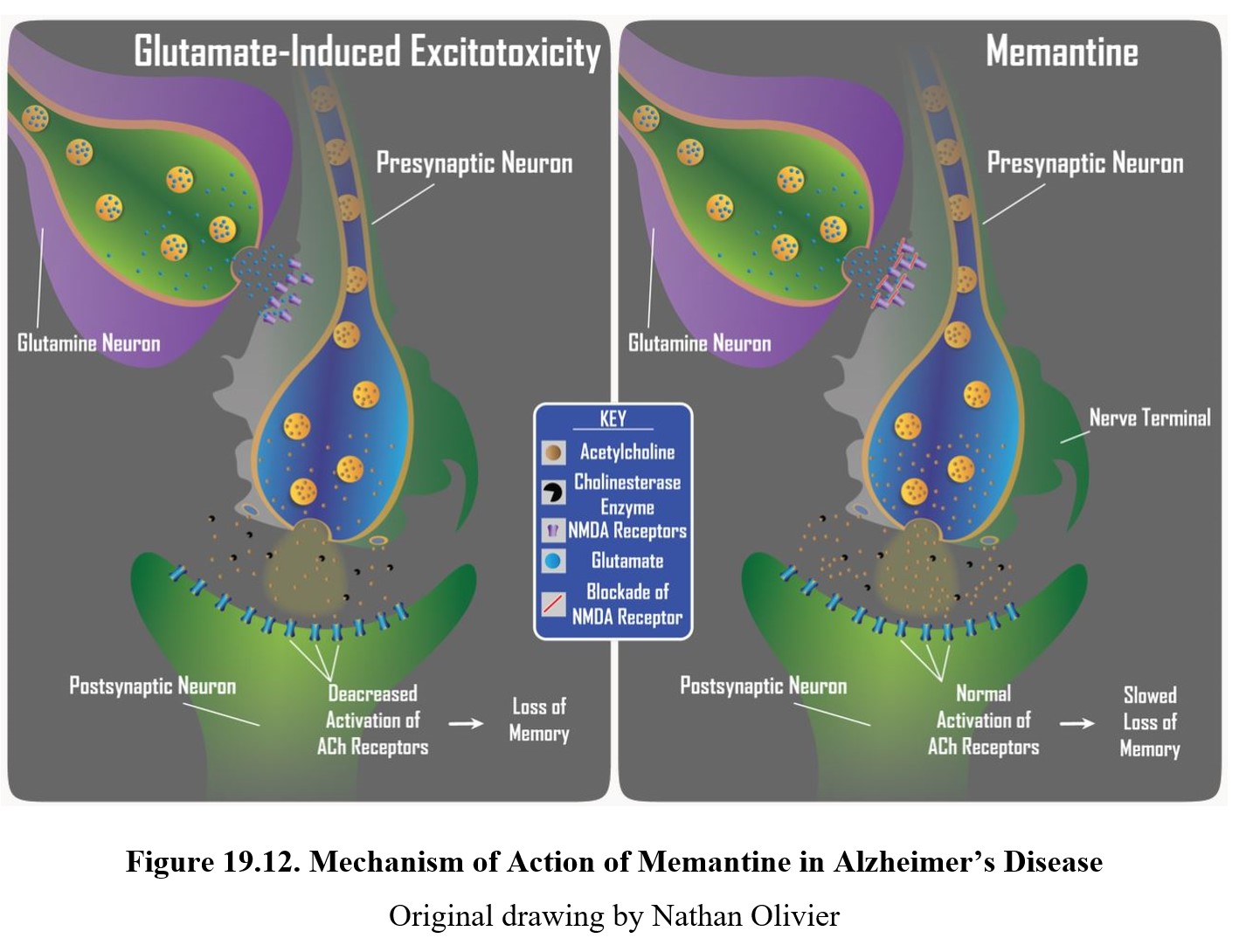
NMDA Receptor Antagonists
Memantine works by blocking NMDA (N-methyl-D-aspartate) glutamate receptors to:
- Prevent excessive glutamate activity
- Protect neurons from excitotoxicity
- Regulate calcium influx into neurons
- Improve signal transmission
Example: Memantine (Namenda)
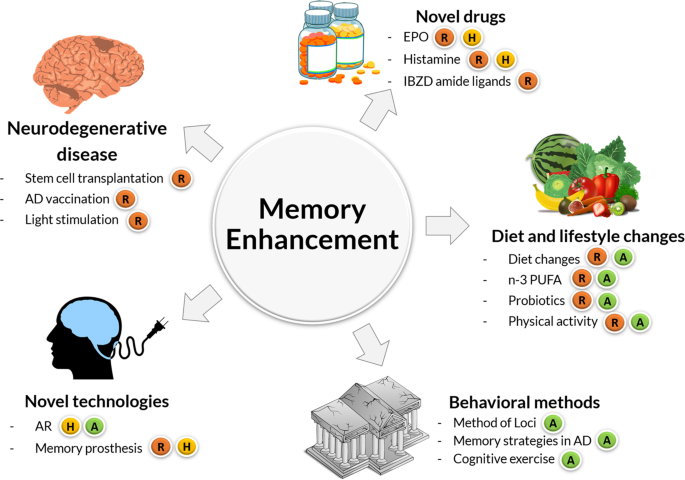
Amyloid-Targeting Therapies
These newer monoclonal antibody therapies target beta-amyloid, a key component in Alzheimer’s pathology:
- Bind to beta-amyloid aggregates in the brain
- Promote clearance of amyloid plaques
- Potentially slow disease progression
Examples: Aducanumab (Aduhelm), Lecanemab (Leqembi)
Indications
| Medication | FDA-Approved Indications | Dementia Stage |
|---|---|---|
| Donepezil (Aricept) | Alzheimer’s Disease | All stages (mild to severe) |
| Rivastigmine (Exelon) | Alzheimer’s Disease, Parkinson’s Disease Dementia | Mild to moderate |
| Galantamine (Razadyne) | Alzheimer’s Disease | Mild to moderate |
| Memantine (Namenda) | Alzheimer’s Disease | Moderate to severe |
| Donepezil + Memantine (Namzaric) | Alzheimer’s Disease | Moderate to severe |
| Aducanumab (Aduhelm) | Alzheimer’s Disease | Early stage (MCI or mild dementia) |
| Lecanemab (Leqembi) | Alzheimer’s Disease | Early stage (MCI or mild dementia) |
Clinical Pearl
While cognitive enhancers are primarily indicated for Alzheimer’s disease, they are sometimes used off-label for other types of dementia. Cholinesterase inhibitors may provide some benefit in Lewy body dementia and Parkinson’s disease dementia, but have limited efficacy in vascular dementia and frontotemporal dementia.
The effects of these medications are modest, and expectations should be managed accordingly. The goal is to temporarily stabilize or slow decline rather than improve cognitive function to pre-disease levels.
Side Effects
Cholinesterase Inhibitors Side Effects
- Gastrointestinal: Nausea, vomiting, diarrhea, anorexia
- Neurological: Headache, dizziness, insomnia
- Cardiovascular: Bradycardia, syncope, hypertension
- Genitourinary: Urinary incontinence, UTI
- Muscular: Muscle cramps, weakness
- Other: Weight loss, fatigue, increased gastric acid secretion
Memantine Side Effects
- Neurological: Dizziness, headache, confusion
- Gastrointestinal: Constipation, vomiting (less common than with cholinesterase inhibitors)
- Cardiovascular: Hypertension
- Other: Fatigue, back pain, somnolence
Amyloid-Related Imaging Abnormalities (ARIA)
Amyloid-targeting therapies like aducanumab and lecanemab can cause ARIA, which includes:
- ARIA-E: Brain edema or swelling
- ARIA-H: Microhemorrhages or superficial siderosis
Symptoms may include headache, confusion, dizziness, vision changes, and nausea. Risk is higher in patients with the ApoE ε4 gene.
Special Precautions
Cholinesterase inhibitors should be used with caution in patients with:
- History of ulcer disease or GI bleeding
- Sick sinus syndrome or other supraventricular cardiac conduction disorders
- History of seizures
- Asthma or COPD
- Urinary outflow obstruction
Nursing Considerations
Assessment
- Complete cognitive assessment using standardized tools (MMSE, MoCA)
- Baseline functional status (ADLs, IADLs)
- Cardiac assessment (ECG if indicated)
- Weight and nutritional status
- Complete medication review
- History of GI problems, seizures, asthma
- For amyloid therapies: MRI and ApoE status
Administration
- Donepezil: Once daily, can be taken at bedtime
- Rivastigmine: Twice daily with food (oral); apply patch once daily to clean, dry skin, rotating sites (transdermal)
- Galantamine: Twice daily with morning and evening meals
- Memantine: Once or twice daily depending on formulation
- Aducanumab/Lecanemab: IV infusion under medical supervision
- Start with low dose and titrate gradually to minimize side effects
Monitoring
- Cognitive function and behavioral symptoms
- Functional abilities
- Weight and nutritional status
- Side effects, especially GI symptoms
- Heart rate and blood pressure
- For amyloid therapies: MRI monitoring for ARIA
- Evaluate effectiveness regularly (typically every 3-6 months)
Patient and Caregiver Education
- Set realistic expectations about treatment benefits
- Report side effects, especially severe GI symptoms or dizziness
- Do not discontinue medication abruptly
- Take with food to minimize GI effects
- Ensure adequate hydration
- Use memory aids and establish routines for medication adherence
- Continue cognitive stimulation activities
- Recognize that effects may be subtle and primarily involve slowing decline
- Report any significant changes in behavior or function
Drug Interactions
- Anticholinergics: Reduce efficacy of cholinesterase inhibitors
- Cholinergic agonists: Additive effects
- Beta-blockers: Increased risk of bradycardia
- NSAIDs: Increased risk of GI bleeding
- CYP450 inducers/inhibitors: Affect metabolism of some agents
- Memantine and NMDA antagonists: Potentially additive effects
Discontinuation Considerations
- Consider discontinuation if:
- Adverse effects outweigh benefits
- No apparent response after 6 months
- Progression to very severe dementia
- Development of contraindications
- Monitor for cognitive decline after discontinuation
- Consider restarting if significant worsening occurs
Memory Aids
DEMENTIA Mnemonic
Use this mnemonic to remember key features of dementia treatment:
- D – Donepezil for all stages
- E – Evaluate cognitive function regularly
- M – Memantine for moderate to severe stages
- E – Expect modest benefits only
- N – Non-pharmacological approaches are essential
- T – Titrate doses gradually
- I – Inform caregivers about realistic expectations
- A – Adverse effects, especially GI, require monitoring
BRAIN Mnemonic for Cognitive Enhancers
Remember the classifications and actions:
- B – Boost acetylcholine (Cholinesterase inhibitors)
- R – Regulate glutamate (Memantine)
- A – Amyloid targeting (newer monoclonal antibodies)
- I – Improve neurotransmission (main mechanism)
- N – No cure, only symptomatic relief
Side Effects Comparison Chart
| Side Effect | Cholinesterase Inhibitors | Memantine |
|---|---|---|
| Nausea/Vomiting | +++ | + |
| Diarrhea | +++ | + |
| Dizziness | ++ | ++ |
| Headache | ++ | ++ |
| Bradycardia | ++ | – |
| Confusion | + | ++ |
| Constipation | + | ++ |
Key: +++ = Common, ++ = Occasional, + = Rare, – = Not typically associated
Cognitive Enhancer Escalation Ladder
3. Hypnotics & Sedatives
Overview
Hypnotics and sedatives are substances that depress central nervous system (CNS) activity, reducing anxiety, promoting calmness, and inducing sleep. While sedatives primarily produce a calming effect, hypnotics specifically induce and maintain sleep. Many drugs serve both functions but at different doses.
Classes of Hypnotics & Sedatives
- Benzodiazepines: Diazepam, Lorazepam, Temazepam, Midazolam
- Z-drugs: Zolpidem, Zaleplon, Eszopiclone
- Barbiturates: Phenobarbital, Pentobarbital (less commonly used now)
- Melatonin receptor agonists: Ramelteon
- Orexin receptor antagonists: Suvorexant
- Antihistamines: Diphenhydramine, Doxylamine
Clinical Applications
- Insomnia: Difficulty falling asleep or staying asleep
- Anxiety: Acute anxiety episodes, generalized anxiety disorder
- Seizures: Emergency management of status epilepticus
- Procedural sedation: Endoscopy, minor surgeries
- Alcohol withdrawal: Prevention and management of symptoms
- Muscle relaxation: Relief of spasticity and muscle spasms
- Pre-anesthetic medication: Before surgery
Important Concerns
Most hypnotics and sedatives have significant risks, including:
- Potential for dependence and withdrawal
- Risk of tolerance with long-term use
- CNS depression that can compound with other substances
- Risk of falls and accidents, especially in older adults
- Respiratory depression at higher doses
- Many are controlled substances due to abuse potential
Mechanism of Action
Most hypnotics and sedatives exert their effects by enhancing inhibitory neurotransmission in the central nervous system, particularly through the GABA system:

Benzodiazepines
Bind to a specific site on the GABAA receptor:
- Enhance the effect of GABA by increasing the frequency of chloride ion channel opening
- Result in neuronal hyperpolarization, making neurons less excitable
- Produce anxiolytic, sedative, hypnotic, muscle relaxant, and anticonvulsant effects
Z-Drugs
Similar to benzodiazepines but with greater selectivity:
- Bind specifically to the omega-1 (BZ1) receptor subtype of the GABAA receptor
- More selective for sleep effects with fewer anxiolytic and muscle relaxant properties
- Shorter duration of action than most benzodiazepines
Barbiturates
Bind to a different site on the GABAA receptor:
- Increase the duration of chloride ion channel opening
- Can directly activate chloride channels at high doses
- Have a narrower therapeutic index than benzodiazepines
- Higher risk of respiratory depression and overdose
Non-GABA Mechanisms
- Melatonin receptor agonists: Activate MT1 and MT2 receptors to promote sleep onset
- Orexin receptor antagonists: Block wake-promoting orexin signaling in the brain
- Antihistamines: Block H1 histamine receptors, which produces sedation as a side effect
Indications
| Drug Class | Examples | Primary Indications |
|---|---|---|
| Benzodiazepines (short-acting) | Midazolam, Triazolam | Procedural sedation, short-term insomnia |
| Benzodiazepines (intermediate-acting) | Lorazepam, Alprazolam, Temazepam | Anxiety disorders, insomnia, alcohol withdrawal |
| Benzodiazepines (long-acting) | Diazepam, Clonazepam | Anxiety disorders, seizures, muscle spasms |
| Z-drugs | Zolpidem, Zaleplon, Eszopiclone | Insomnia (sleep onset and/or maintenance) |
| Barbiturates | Phenobarbital, Pentobarbital | Seizures, pre-anesthetic, severe insomnia (limited use) |
| Melatonin receptor agonists | Ramelteon | Sleep onset insomnia |
| Orexin receptor antagonists | Suvorexant, Lemborexant | Insomnia (sleep onset and maintenance) |
| Antihistamines | Diphenhydramine, Doxylamine | Mild, occasional insomnia (OTC use) |
Clinical Pearl
The choice of hypnotic/sedative should be based on the specific sleep complaint:
- Sleep onset insomnia: Consider shorter-acting agents (zaleplon, triazolam, ramelteon)
- Sleep maintenance insomnia: Consider intermediate-acting agents (zolpidem, eszopiclone, temazepam)
- Combined onset and maintenance: Consider suvorexant, eszopiclone, or extended-release zolpidem
Non-pharmacological strategies should be first-line treatment for chronic insomnia, with medications as adjunctive therapy for short-term use when possible.
Side Effects
Common Side Effects
- Daytime drowsiness/sedation
- Dizziness and lightheadedness
- Impaired coordination and ataxia
- Cognitive impairment (confusion, memory impairment)
- Headache
- Paradoxical reactions (increased anxiety, agitation)
- Blurred vision
- Nausea or GI disturbances
- Anterograde amnesia
- Complex sleep behaviors with Z-drugs (sleep-walking, sleep-driving)
Serious Adverse Effects
- Respiratory depression (especially with other CNS depressants)
- Tolerance and physical dependence
- Withdrawal syndrome (rebound insomnia, anxiety, seizures)
- Increased risk of falls and fractures, especially in elderly
- Potential for abuse and misuse
- Overdose toxicity (especially with barbiturates)
- Potential for increased dementia risk with long-term use
- Increased risk of motor vehicle accidents
Special Population Concerns
- Elderly: More sensitive to side effects. Use lower doses (typically half the adult dose). Increased risk of falls, cognitive impairment, and delirium.
- Pregnant/breastfeeding women: Risk of neonatal withdrawal, sedation, and potential teratogenicity. Most hypnotics and sedatives should be avoided if possible.
- Patients with respiratory conditions: Increased risk of respiratory depression in those with COPD, sleep apnea, or other respiratory disorders.
- Patients with hepatic impairment: Reduced metabolism leading to drug accumulation and enhanced effects. Dose reduction required.
Benzodiazepine Withdrawal Syndrome
Symptoms can include:
- Rebound anxiety and insomnia
- Irritability and agitation
- Tremors
- Nausea and vomiting
- Hyperacusis (sensitivity to sound)
- Paresthesias
- Perceptual disturbances
- Seizures (in severe cases)
- Psychosis (in severe cases)
Withdrawal is more severe with higher doses, longer duration of use, and shorter-acting agents. Always taper gradually rather than abrupt discontinuation.
Nursing Considerations
Assessment
- Complete sleep history and pattern disturbances
- Screen for substance use disorders
- Evaluate for underlying medical, psychiatric, or environmental causes of sleep disturbance
- Respiratory status, especially in patients with COPD or sleep apnea
- Liver and kidney function
- Comprehensive medication review for potential interactions
- Mental status and cognitive function
- Risk for falls, especially in elderly patients
Administration
- Administer at appropriate time before desired sleep onset
- Ensure 7-8 hours of potential sleep time after administration
- Z-drugs should be taken immediately before bedtime
- Some medications should be taken on an empty stomach for faster onset (e.g., zolpidem)
- Ensure patient remains in bed after taking medication
- Implement safety precautions (bed in low position, side rails as appropriate, call bell within reach)
- Monitor for paradoxical reactions, especially in elderly
Monitoring
- Level of sedation and response to medication
- Respiratory status, especially when combined with other CNS depressants
- Mental status and cognitive function
- Signs of dependence or tolerance (requesting higher doses or more frequent administration)
- Paradoxical reactions, especially in elderly patients
- Effectiveness in improving sleep quality and duration
- Side effects (morning drowsiness, dizziness, confusion)
- Fall risk, especially in hospitalized patients
Patient Education
- Take medication exactly as prescribed
- Do not drive or operate machinery after taking medication
- Avoid alcohol and other CNS depressants
- Do not abruptly discontinue after prolonged use
- Use the medication for the shortest time necessary
- Practice good sleep hygiene in addition to medication
- Report any unusual side effects or complex sleep behaviors
- Store medication securely away from children and individuals with substance use disorders
- Discuss plans for gradual discontinuation with healthcare provider
Sleep Hygiene Education
- Maintain regular sleep and wake times
- Create a comfortable sleep environment (dark, quiet, cool)
- Avoid caffeine, alcohol, and nicotine near bedtime
- Limit screen time before bed
- Engage in relaxing bedtime routines
- Exercise regularly, but not close to bedtime
- Limit daytime napping
- Use the bed only for sleep and intimacy
- If unable to fall asleep within 20 minutes, get up and do a relaxing activity until sleepy
Drug Interactions
- CNS depressants: Additive effects with alcohol, opioids, antipsychotics, antihistamines
- CYP450 inhibitors: May increase levels of benzodiazepines and Z-drugs
- CYP450 inducers: May decrease effectiveness of some agents
- Grapefruit juice: Can increase levels of some benzodiazepines
- Proton pump inhibitors: May affect absorption of some agents
- Antacids: May decrease absorption if taken concurrently
Memory Aids
BENZODIAZEPINES Mnemonic
Remember key side effects and concerns:
- B – Balance disturbances and falls
- E – Elderly are more sensitive
- N – Never abruptly discontinue
- Z – Zonked (oversedation) risk
- O – Overdose potential (especially with other CNS depressants)
- D – Dependence and tolerance
- I – Impaired coordination and cognition
- A – Amnesia (anterograde)
- Z – Zzz’s (rebound insomnia upon discontinuation)
- E – Extended use problematic
- P – Paradoxical reactions possible
- I – Interactions with other medications
- N – No driving or hazardous activities
- E – Euphoria (potential for abuse)
- S – Scheduled medications (controlled substances)
SLEEP Mnemonic for Sedative Selection
Factors to consider when selecting a hypnotic:
- S – Specific sleep complaint (onset vs. maintenance)
- L – Length of treatment (short-term preferred)
- E – Elderly status (lower doses, avoid long-acting)
- E – Existing conditions (respiratory, hepatic, mental health)
- P – Previous response or side effects to sleep medications
Benzodiazepine Comparison Chart
| Agent | Onset | Duration | Primary Use |
|---|---|---|---|
| Midazolam | Very rapid | Short (2-4h) | Procedural sedation |
| Triazolam | Rapid | Short (3-5h) | Sleep onset insomnia |
| Alprazolam | Intermediate | Intermediate (6-12h) | Anxiety, panic |
| Lorazepam | Intermediate | Intermediate (10-20h) | Anxiety, insomnia |
| Temazepam | Slow | Intermediate (8-20h) | Insomnia |
| Diazepam | Rapid | Long (20-80h) | Anxiety, muscle spasms |
| Clonazepam | Intermediate | Long (18-50h) | Seizures, anxiety |
Z-Drugs vs. Benzodiazepines
- Advantages of Z-drugs:
- Less daytime sedation
- Less cognitive impairment
- Lower risk of dependence
- Less effect on sleep architecture
- Less rebound insomnia
- Disadvantages of Z-drugs:
- Complex sleep behaviors
- Still have abuse potential
- Still cause tolerance over time
- Amnesia still possible
Tapering Visual Aid
For long-term benzodiazepine discontinuation:
* Taper schedule should be individualized based on patient response
Updated Black Box Warnings for SSRIs/SNRIs: Reassessing Impact and Implications
In recent years, significant attention has been directed toward the black box warnings placed on selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs). These stringent warnings, originally implemented by the FDA in 2004 and expanded in 2007, were intended to alert healthcare providers and patients about potential increased risks of suicidal thoughts and behaviours in young people taking these medications.
However, mounting evidence suggests these warnings may have had unintended negative consequences. A systematic review published in Health Affairs examined data spanning from 2003 to 2022, analysing the effects of these warnings on treatment patterns and patient outcomes. The findings revealed “significant unintended reductions” in mental health care following the implementation of black box warnings, with antidepressant prescribing dropping by 20-50% in various populations. More alarmingly, researchers found correlations between these warnings and increased psychotropic drug poisonings and suicide deaths among young people.
“The sudden, simultaneous, and sweeping effects of these warnings—reduction in depression treatment and increase in suicide—are documented across 14 years of strong research,” stated Stephen Soumerai, Harvard Medical School professor of population medicine at the Harvard Pilgrim Health Care Institute. “The consistency in observed harms and absence of observed benefits after the black-box warnings indicates this is not a coincidence.”
The warnings advised closer monitoring of patients initiated on these medications, yet studies indicated that fewer than 5% of pediatric patients received the recommended monitoring. This suggests that rather than enhancing vigilance, the warnings may have deterred treatment altogether.
Parallel to these concerns, regulatory bodies worldwide update warnings about other risks associated with these medications. For instance, the Australian Therapeutic Goods Administration recently aligned Product Information documents for all SSRIs and SNRIs to reflect the risk of sexual dysfunction persisting after drug cessation. While previously acknowledged during treatment, the persistence of sexual side effects after discontinuation, potentially lasting weeks to years, wasn’t uniformly disclosed across all medications in this class.
Despite these concerns, antidepressants remain important treatment options for many patients with depression and anxiety disorders. The challenge lies in balancing appropriate caution with the need to ensure those who could benefit from treatment aren’t deterred by warnings that may overstate risks or understate benefits.
In response to these findings, researchers have recommended that the FDA reconsider the black box warnings for antidepressants—either by incorporating them into routine warnings that pose fewer barriers to appropriate treatment or potentially removing them entirely. The FDA has acknowledged that “the evaluation of product safety is an ongoing and continuous process,” indicating openness to reviewing existing evidence.
For healthcare providers, these developments underscore the importance of individualised benefit-risk discussions with patients and families, acknowledging both the potential risks of medication and the substantial risks of untreated depression and anxiety. As our understanding of these medications continues to evolve, so too should the regulatory framework that governs their use, always with the ultimate goal of optimising patient outcomes.
