Pulmonary Embolism
Complete Nursing Guide & Clinical Management
Table of Contents
Fundamentals
Clinical Assessment
1Introduction to Pulmonary Embolism
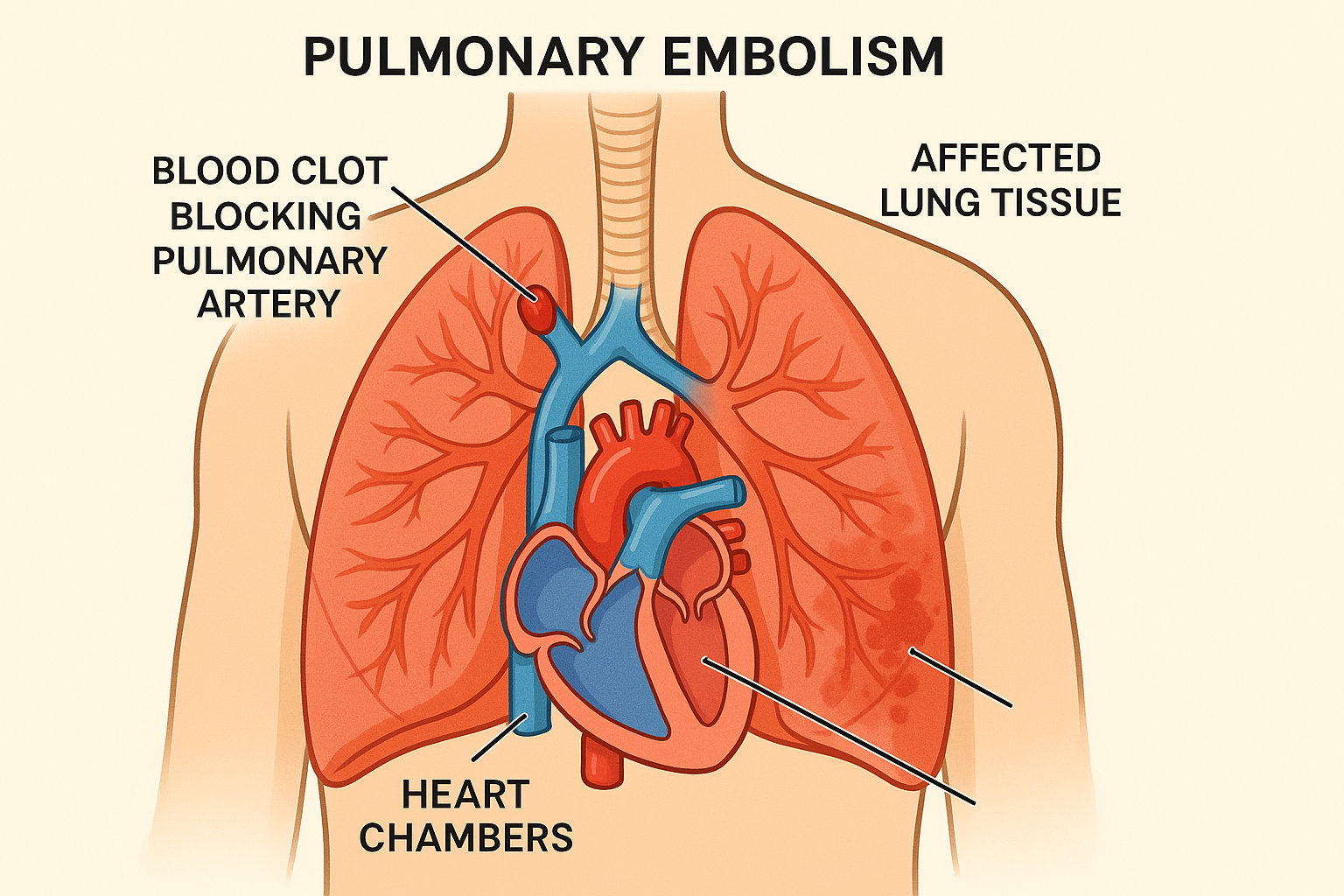
Pulmonary embolism represents one of the most critical cardiovascular emergencies encountered in clinical practice, affecting millions of patients worldwide annually. This life-threatening condition occurs when blood clots, typically originating from deep vein thrombosis, travel through the circulatory system and lodge within the pulmonary arteries, creating potentially fatal blockages that compromise respiratory and cardiovascular function.
Key Statistics
- Annual Incidence: 600,000 cases in the United States
- Mortality Rate: 10-30% if untreated
- Hospital Admissions: Third leading cause of cardiovascular death
- Recurrence Rate: 5-10% within first year
Critical Recognition
Early recognition and prompt treatment of pulmonary embolism are essential for optimal patient outcomes. Delayed diagnosis significantly increases morbidity and mortality rates, making nursing assessment skills and clinical judgment paramount in emergency situations.
2Pathophysiology of Pulmonary Embolism
Understanding the complex pathophysiological mechanisms underlying pulmonary embolism is crucial for nursing professionals to provide effective care and anticipate potential complications. The condition involves multiple interconnected processes that affect both respiratory and cardiovascular systems.
Embolic Process
- 1. Thrombus Formation: Blood clots develop in deep veins, commonly in lower extremities
- 2. Detachment: Clot fragments break away from original site
- 3. Migration: Emboli travel through venous system to right heart
- 4. Pulmonary Entry: Clots enter pulmonary circulation via pulmonary arteries
- 5. Vascular Obstruction: Emboli lodge in pulmonary vessels causing blockage
Hemodynamic Effects
- Increased Pulmonary Pressure: Vascular resistance rises dramatically
- Right Heart Strain: Elevated workload on right ventricle
- Reduced Cardiac Output: Decreased blood flow to systemic circulation
- Ventilation-Perfusion Mismatch: Impaired gas exchange efficiency
- Potential Cardiac Arrest: Severe cases may lead to circulatory collapse
Memory Aid: “CLOTS” Pathophysiology
- Clot formation in deep veins
- Lodging in pulmonary arteries
- Obstruction of blood flow
- Tissues become hypoxic
- Strain on right heart develops
| Severity Level | Vascular Obstruction | Hemodynamic Impact | Clinical Manifestation |
|---|---|---|---|
| Massive PE | >50% pulmonary circulation | Severe right heart failure | Hemodynamic instability, shock |
| Submassive PE | 25-50% pulmonary circulation | Moderate right heart strain | Normal blood pressure, elevated biomarkers |
| Low-risk PE | <25% pulmonary circulation | Minimal hemodynamic impact | Stable vitals, localized symptoms |
3Risk Factors and Predisposing Conditions
Identifying patients at risk for pulmonary embolism requires comprehensive understanding of predisposing factors. These risk factors often cluster together, creating multiplicative rather than additive risk profiles that nurses must recognize and assess systematically.
Acquired Risk Factors
- • Major surgery (especially orthopedic)
- • Prolonged immobilization
- • Active malignancy
- • Pregnancy and postpartum
- • Hormone replacement therapy
- • Oral contraceptive use
- • Previous thromboembolism
- • Central venous catheters
Inherited Risk Factors
- • Factor V Leiden mutation
- • Prothrombin gene mutation
- • Antithrombin deficiency
- • Protein C deficiency
- • Protein S deficiency
- • Antiphospholipid syndrome
- • Family history of VTE
- • Homocystinuria
Situational Risk Factors
- • Long-distance travel
- • Bed rest >3 days
- • ICU admission
- • Mechanical ventilation
- • Inflammatory conditions
- • Advanced age (>60 years)
- • Obesity (BMI >30)
- • Smoking history
Memory Aid: “THROMBOSIS” Risk Assessment
- Trauma or surgery
- Hormones (estrogen therapy)
- Rest (prolonged immobility)
- Obesity
- Malignancy
- Birth control pills
- Old age
- Smoking
- Inherited thrombophilia
- Surgery (major procedures)
Nursing Assessment Priority
Always conduct comprehensive risk stratification for every patient, particularly those with multiple risk factors. Document risk assessment findings clearly and communicate high-risk status to the entire healthcare team for appropriate prophylactic interventions.
4Clinical Presentation and Assessment
Pulmonary embolism presents with a wide spectrum of clinical manifestations, ranging from subtle symptoms to life-threatening cardiovascular collapse. The challenge lies in recognizing that many symptoms are nonspecific and can mimic other respiratory or cardiac conditions.
Primary Symptoms
Dyspnea (90% of cases)
Sudden onset shortness of breath, often the first and most common symptom
Chest Pain (75% of cases)
Sharp, stabbing pain that worsens with deep breathing
Tachypnea (70% of cases)
Respiratory rate typically >20 breaths per minute
Secondary Signs
- Tachycardia: Heart rate >100 bpm (compensatory mechanism)
- Hypoxemia: Decreased oxygen saturation, often subtle initially
- Hemoptysis: Coughing up blood (25% of patients)
- Syncope: Fainting episodes, particularly with massive PE
- Anxiety: Feeling of impending doom
- Diaphoresis: Excessive sweating due to physiological stress
| Assessment Category | Findings | Clinical Significance | Nursing Actions |
|---|---|---|---|
| Respiratory | Dyspnea, tachypnea, decreased oxygen saturation | Impaired gas exchange | Monitor respiratory status, administer oxygen |
| Cardiovascular | Tachycardia, hypotension, elevated JVP | Right heart strain | Continuous cardiac monitoring, vital signs |
| Neurological | Anxiety, confusion, syncope | Cerebral hypoxia | Mental status assessment, safety measures |
| Integumentary | Pallor, cyanosis, diaphoresis | Poor perfusion | Skin assessment, temperature monitoring |
Memory Aid: “EMBOLISM” Clinical Presentation
- Exertional dyspnea
- Massive chest pain
- Bleeding (hemoptysis)
- Oxygen desaturation
- Low blood pressure
- Increased heart rate
- Syncope episodes
- Mental status changes
5Diagnostic Methods and Imaging
Accurate diagnosis of pulmonary embolism requires a systematic approach combining clinical assessment, laboratory testing, and advanced imaging techniques. The diagnostic process must balance accuracy with timeliness, as delayed diagnosis can have life-threatening consequences.
Laboratory Tests
- D-dimer: Elevated levels suggest thrombosis
- Arterial Blood Gas: Shows hypoxemia and respiratory alkalosis
- Troponin: May be elevated with right heart strain
- BNP/NT-proBNP: Indicates heart failure
- Complete Blood Count: Baseline values
- Coagulation Studies: PT/PTT for anticoagulation
Imaging Studies
- CT Pulmonary Angiogram: Gold standard diagnostic test
- Chest X-ray: Often normal, rules out other conditions
- Echocardiogram: Assesses right heart function
- Ventilation-Perfusion Scan: Alternative when CT contraindicated
- Duplex Ultrasound: Identifies deep vein thrombosis
- Pulmonary Angiography: Rarely used, invasive gold standard
Physiologic Tests
- Electrocardiogram: Shows signs of right heart strain
- Pulse Oximetry: Monitors oxygen saturation
- Peak Expiratory Flow: Assesses respiratory function
- Capnography: End-tidal CO2 monitoring
- Blood Pressure: May show hypotension
- Heart Rate Variability: Autonomic dysfunction
| Diagnostic Test | Sensitivity | Specificity | Advantages | Limitations |
|---|---|---|---|---|
| CT Pulmonary Angiogram | 95-100% | 95-98% | Rapid, widely available, high accuracy | Contrast allergy, kidney function |
| D-dimer | 95-98% | 35-40% | High negative predictive value | Low specificity, many false positives |
| V/Q Scan | 85-90% | 85-95% | No contrast required | Time-consuming, requires cooperation |
| Echocardiogram | 70-80% | 80-85% | Assesses cardiac function | Indirect signs only |
Diagnostic Algorithm
- 1. Clinical assessment and risk stratification
- 2. D-dimer testing (if low/moderate clinical probability)
- 3. CT pulmonary angiogram (if high probability or positive D-dimer)
- 4. Alternative imaging if CT contraindicated
- 5. Lower extremity ultrasound if PE suspected
6Clinical Assessment Tools and Scoring Systems
Standardized assessment tools provide objective methods for evaluating pulmonary embolism probability and severity. These validated instruments help guide diagnostic decisions and treatment strategies while reducing clinical variability in patient care.
Wells Score for PE
| Clinical Feature | Points |
|---|---|
| Clinical signs of DVT | 3.0 |
| PE most likely diagnosis | 3.0 |
| Heart rate >100 bpm | 1.5 |
| Immobilization/surgery in past 4 weeks | 1.5 |
| Previous DVT/PE | 1.5 |
| Hemoptysis | 1.0 |
| Malignancy | 1.0 |
Interpretation:
• Low risk: ≤4 points
• High risk: >4 points
PESI Score (Pulmonary Embolism Severity Index)
Risk Classes:
• Class I-II (≤85): Low risk
• Class III-V (>85): High risk
Memory Aid: “PERC Rule” (PE Rule-out Criteria)
If ALL criteria are negative, PE risk is <1%:
- • Age <50 years
- • Heart rate <100 bpm
- • Oxygen saturation ≥95%
- • No hemoptysis
- • No estrogen use
- • No surgery/trauma in 4 weeks
- • No prior VTE
- • No unilateral leg swelling
7Treatment Options and Therapeutic Interventions
Treatment of pulmonary embolism requires immediate intervention with anticoagulation therapy as the cornerstone of management. The choice of specific treatments depends on the severity of the embolism, patient stability, and individual risk factors for bleeding complications.
Anticoagulation Therapy
Initial Treatment (First 5-10 days)
- Unfractionated Heparin: IV bolus then continuous infusion
- Low Molecular Weight Heparin: Subcutaneous injection
- Direct Oral Anticoagulants: Rivaroxaban, Apixaban
- Fondaparinux: Synthetic Factor Xa inhibitor
Long-term Treatment (3-6 months)
- Warfarin: Target INR 2.0-3.0
- Direct Oral Anticoagulants: Dabigatran, Rivaroxaban
- Extended therapy: Consider for recurrent PE
Advanced Interventions
Thrombolytic Therapy
- Systemic thrombolysis: Alteplase, Streptokinase
- Catheter-directed thrombolysis: Localized delivery
- Indications: Massive PE with hemodynamic instability
Surgical Interventions
- Pulmonary embolectomy: Emergency surgical removal
- IVC filter placement: When anticoagulation contraindicated
- ECMO support: Severe cardiopulmonary failure
| Medication Category | Examples | Mechanism of Action | Nursing Considerations |
|---|---|---|---|
| Unfractionated Heparin | Heparin sodium | Enhances antithrombin activity | Monitor aPTT, assess for bleeding |
| LMWH | Enoxaparin, Dalteparin | Selective factor Xa inhibition | Fixed dosing, monitor platelets |
| Direct Oral Anticoagulants | Rivaroxaban, Apixaban | Direct factor Xa inhibition | Monitor renal function, drug interactions |
| Vitamin K Antagonists | Warfarin | Inhibits vitamin K dependent factors | Monitor INR, dietary education |
Contraindications to Anticoagulation
Absolute Contraindications:
- • Active major bleeding
- • Recent intracranial hemorrhage
- • Severe thrombocytopenia
- • Recent major surgery
Relative Contraindications:
- • History of GI bleeding
- • Severe hypertension
- • Pregnancy (warfarin)
- • Liver disease
8Comprehensive Nursing Care Plans
Nursing care for patients with pulmonary embolism requires vigilant monitoring, comprehensive assessment, and patient-centered interventions. Nurses play a crucial role in early detection of complications and providing supportive care throughout the treatment process.
Priority Nursing Diagnoses
- 1. Impaired Gas Exchange related to ventilation-perfusion mismatch
- 2. Ineffective Tissue Perfusion related to pulmonary vascular obstruction
- 3. Acute Pain related to pulmonary tissue ischemia
- 4. Risk for Bleeding related to anticoagulant therapy
- 5. Anxiety related to acute illness and fear of death
- 6. Activity Intolerance related to decreased oxygen delivery
Essential Nursing Interventions
- Continuous Monitoring: Vital signs, oxygen saturation, cardiac rhythm
- Oxygen Therapy: Maintain SpO2 >95%, titrate as needed
- Medication Administration: Anticoagulants, analgesics, anxiolytics
- Positioning: Semi-Fowler’s position for optimal breathing
- Bleeding Assessment: Monitor for signs of hemorrhage
- Emotional Support: Provide reassurance and education
| Assessment Parameter | Normal Values | Critical Values | Nursing Actions |
|---|---|---|---|
| Oxygen Saturation | 95-100% | <90% | Increase oxygen, notify physician |
| Heart Rate | 60-100 bpm | >120 bpm or <50 bpm | Continuous monitoring, assess hemodynamics |
| Blood Pressure | 120/80 mmHg | SBP <90 mmHg | Fluid resuscitation, vasopressor support |
| Respiratory Rate | 12-20 breaths/min | >30 or <8 breaths/min | Assess work of breathing, consider ventilation |
Memory Aid: “MONITOR” Nursing Care
- Monitor vital signs continuously
- Oxygen therapy as prescribed
- Note bleeding signs and symptoms
- Increase head of bed for breathing
- Teach about anticoagulation
- Observe for complications
- Report changes immediately
Nursing Care Excellence
Implement evidence-based protocols for PE care including standardized assessment tools, medication reconciliation, and multidisciplinary communication. Document all interventions and patient responses thoroughly to ensure continuity of care and optimal patient outcomes.
9Complications and Emergency Management
Pulmonary embolism can lead to serious complications that require immediate recognition and intervention. Understanding potential complications helps nurses anticipate problems and implement appropriate preventive measures and emergency responses.
Cardiovascular Complications
- Right Heart Failure: Acute cor pulmonale
- Cardiogenic Shock: Severe hemodynamic compromise
- Cardiac Arrest: Sudden cardiac death
- Arrhythmias: Atrial fibrillation, ventricular tachycardia
- Pulmonary Hypertension: Chronic elevated pressures
Respiratory Complications
- Respiratory Failure: Severe hypoxemia
- Pulmonary Infarction: Tissue death from ischemia
- Pleural Effusion: Fluid accumulation
- Pneumothorax: Air leak into pleural space
- ARDS: Acute respiratory distress syndrome
Treatment-Related Complications
- Major Bleeding: Intracranial, GI, retroperitoneal
- Heparin-Induced Thrombocytopenia: HIT syndrome
- Thrombosis Extension: Clot propagation
- Drug Interactions: Anticoagulant complications
- Allergic Reactions: Contrast or medication allergy
Emergency Management Protocol
Immediate Actions (First 5 minutes)
- 1. Assess airway, breathing, circulation
- 2. Apply high-flow oxygen therapy
- 3. Establish IV access (2 large bore)
- 4. Continuous cardiac monitoring
- 5. Vital signs every 15 minutes
Ongoing Management
- 1. Prepare for intubation if needed
- 2. Administer anticoagulation promptly
- 3. Consider thrombolytic therapy
- 4. Prepare for emergency procedures
- 5. Family communication and support
| Complication | Early Warning Signs | Assessment Findings | Emergency Interventions |
|---|---|---|---|
| Massive PE | Sudden onset dyspnea, chest pain | Hypotension, tachycardia, hypoxemia | Thrombolysis, embolectomy, ECMO |
| Right Heart Failure | Increasing dyspnea, fatigue | Elevated JVP, peripheral edema | Diuretics, inotropes, afterload reduction |
| Major Bleeding | Unusual bruising, bleeding | Decreased Hgb, active hemorrhage | Reverse anticoagulation, transfusion |
| Recurrent PE | Return of symptoms | New embolic events on imaging | IVC filter, escalate anticoagulation |
10Prevention Strategies and Risk Reduction
Prevention of pulmonary embolism focuses on identifying high-risk patients and implementing appropriate prophylactic measures. Effective prevention strategies can dramatically reduce the incidence of venous thromboembolism in hospitalized patients and high-risk populations.
Pharmacological Prevention
Low-Risk Patients
- Aspirin: 75-100mg daily for medical patients
- Graduated compression stockings: 15-20 mmHg
- Early mobilization: Within 24 hours post-op
High-Risk Patients
- LMWH: Enoxaparin 40mg subcutaneous daily
- Unfractionated Heparin: 5000 units TID
- Fondaparinux: 2.5mg subcutaneous daily
- DOACs: Rivaroxaban 10mg daily post-orthopedic surgery
Non-Pharmacological Prevention
Mechanical Measures
- Sequential compression devices: Intermittent pneumatic compression
- Graduated compression stockings: 15-30 mmHg pressure
- Venous foot pumps: Plantar compression devices
Lifestyle Modifications
- Early ambulation: Progressive mobility protocols
- Leg exercises: Ankle pumps, calf raises
- Hydration: Adequate fluid intake
- Position changes: Avoid prolonged immobility
| Patient Population | VTE Risk Level | Recommended Prophylaxis | Duration |
|---|---|---|---|
| Medical Patients | Moderate to High | LMWH or UFH + mechanical prophylaxis | Length of stay or until mobile |
| General Surgery | Moderate | LMWH or UFH + early mobilization | 5-10 days or until discharge |
| Orthopedic Surgery | High | LMWH, UFH, or DOAC + mechanical | 10-35 days post-operatively |
| ICU Patients | High | LMWH or UFH (if no bleeding risk) | Duration of ICU stay |
Memory Aid: “PREVENT” VTE Strategy
- Prophylaxis for high-risk patients
- Risk assessment on admission
- Early mobilization protocols
- Venous compression devices
- Education for patients and families
- No delay in starting prophylaxis
- Thromboprophylaxis continuation
Quality Improvement Measures
Implement hospital-wide VTE prevention protocols including electronic alerts for high-risk patients, standardized risk assessment tools, and regular audits of prophylaxis compliance rates. Evidence shows that systematic approaches can reduce hospital-acquired VTE by up to 70%.
11Patient and Family Education
Comprehensive patient education is essential for successful management of pulmonary embolism and prevention of recurrence. Patients and families need clear, understandable information about the condition, treatment, and long-term care requirements.
Educational Priorities
Understanding the Condition
- • What is pulmonary embolism and how it develops
- • Risk factors and predisposing conditions
- • Signs and symptoms to recognize
- • Importance of immediate medical attention
Treatment Compliance
- • Importance of taking medications as prescribed
- • Understanding anticoagulation therapy
- • Regular monitoring requirements
- • Duration of treatment expectations
Warning Signs Education
When to Seek Emergency Care
- • Sudden onset severe shortness of breath
- • Sharp chest pain that worsens with breathing
- • Coughing up blood or bloody sputum
- • Fainting or near-fainting episodes
- • Severe leg pain or swelling
Bleeding Complications
- • Unusual or excessive bruising
- • Blood in urine or dark-colored urine
- • Blood in stool or black, tarry stools
- • Severe headaches or vision changes
- • Uncontrolled bleeding from cuts
Discharge Planning Checklist
Medication Management
- ☐ Anticoagulant medication reconciliation
- ☐ Proper injection technique if applicable
- ☐ Drug interaction awareness
- ☐ Laboratory monitoring schedule
- ☐ Prescription refill planning
Lifestyle Modifications
- ☐ Activity restrictions and progression
- ☐ Travel precautions and guidelines
- ☐ Dietary considerations
- ☐ Follow-up appointment scheduling
- ☐ Emergency contact information
| Education Topic | Key Teaching Points | Teaching Methods | Evaluation Criteria |
|---|---|---|---|
| Anticoagulation Safety | Bleeding prevention, drug interactions | Verbal instruction, written materials | Patient demonstrates understanding |
| Activity Modification | Gradual increase, avoid prolonged sitting | Demonstration, return demonstration | Patient verbalizes activity plan |
| Symptom Recognition | Warning signs of recurrence/bleeding | Case scenarios, discussion | Patient identifies when to seek care |
| Follow-up Care | Appointment scheduling, lab monitoring | Written schedule, reminder systems | Patient keeps all appointments |
Memory Aid: “TEACH” Patient Education
- Tell patients about their condition and treatment
- Explain warning signs and when to seek help
- Assess understanding through teach-back methods
- Clarify any questions or concerns
- Help establish support systems for ongoing care
12Global Best Practices and Innovation
Healthcare systems worldwide have developed innovative approaches to prevent, diagnose, and treat pulmonary embolism. These evidence-based practices and technological advances are improving patient outcomes and reducing healthcare costs globally.
United States Innovations
- PERT Teams: Pulmonary Embolism Response Teams for rapid intervention
- Electronic Alerts: EMR-based VTE risk assessment tools
- Quality Metrics: Hospital-acquired VTE prevention measures
- Telemedicine: Remote monitoring of anticoagulation therapy
- AI Integration: Machine learning for PE prediction
European Excellence
- ESC Guidelines: Comprehensive European Society of Cardiology protocols
- Standardized Pathways: Unified care protocols across EU countries
- Mobile PE Units: Specialized emergency response vehicles
- Patient Registries: Long-term outcome tracking systems
- Nurse-Led Clinics: Specialized anticoagulation management
Asia-Pacific Advances
- Robotic Surgery: Minimally invasive embolectomy techniques
- Point-of-Care Testing: Rapid D-dimer and troponin assays
- Community Education: Population-wide VTE awareness programs
- Genetic Screening: Thrombophilia testing protocols
- Digital Health: Smartphone apps for medication compliance
Award-Winning Programs
Mayo Clinic PERT Program (USA)
Multidisciplinary rapid response teams that have reduced PE mortality by 50% through coordinated care protocols and 24/7 availability for high-risk cases.
NHS Scotland VTE Prevention (UK)
National implementation of mandatory VTE risk assessment achieving 95% compliance rates and 40% reduction in hospital-acquired VTE events.
| Innovation | Location | Impact | Implementation |
|---|---|---|---|
| AI-Powered Risk Assessment | Johns Hopkins, USA | 30% improvement in PE prediction | Machine learning algorithms in EHR |
| Mobile Stroke Units for PE | Berlin, Germany | 25% reduction in door-to-treatment time | Specialized ambulances with CT capability |
| Pharmacogenomic Testing | Singapore | 50% reduction in bleeding complications | Genetic testing for warfarin dosing |
| Virtual Reality Training | Tokyo, Japan | 40% improvement in diagnostic accuracy | VR simulation for medical education |
Future Directions
Emerging technologies including artificial intelligence, wearable sensors for early detection, personalized medicine approaches, and novel anticoagulants are revolutionizing PE care. These innovations promise to further improve outcomes while reducing healthcare costs and patient burden.
Conclusion
Pulmonary embolism remains a critical healthcare challenge requiring comprehensive understanding, rapid recognition, and evidence-based management. As nursing professionals, our role in preventing, identifying, and managing this life-threatening condition is paramount to improving patient outcomes and saving lives. Through continued education, clinical excellence, and adoption of innovative practices, we can make a significant difference in the fight against venous thromboembolism.
© 2025 Advanced Medical Education – Pulmonary Embolism Nursing Guide
Evidence-Based • Patient-Centered • Excellence in Care
