Raynaud’s Disease Nursing Care Plan
Comprehensive Guide for Nursing Students
Overview of Raynaud’s Disease
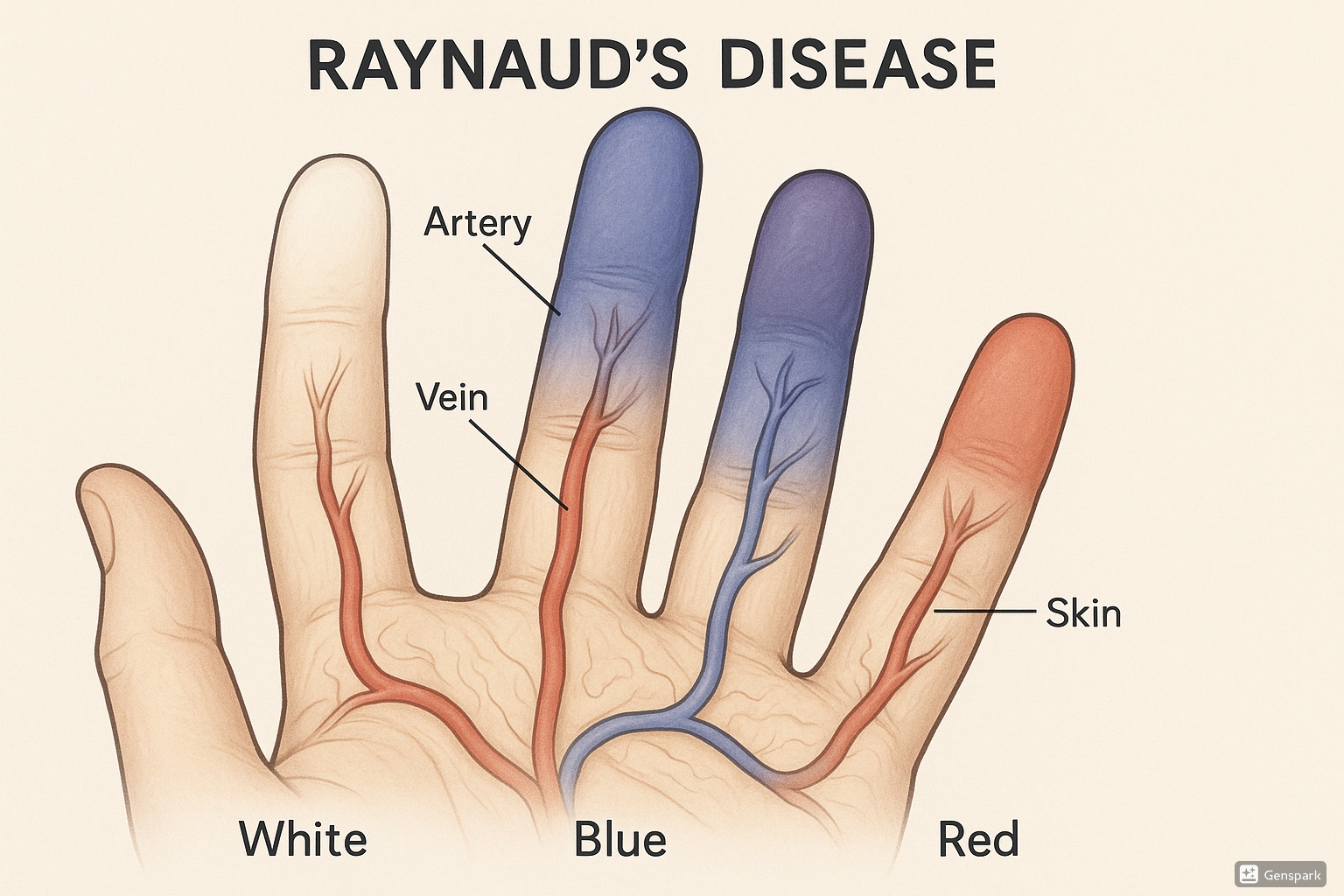
Raynaud’s disease is a disorder that affects small blood vessels in the extremities, primarily the fingers and toes. It is characterized by episodic vasospastic attacks triggered by exposure to cold temperatures or emotional stress. During an attack, the arterioles and capillaries in the affected areas constrict excessively, limiting blood flow and causing a characteristic triphasic color change: white (ischemia), blue (deoxygenation), and red (reperfusion).
Raynaud’s disease affects approximately 3-5% of the general population, with a higher prevalence among:
- Women (female to male ratio of 4:1)
- Young adults (onset typically between ages 15-30)
- People living in colder climates
- Those with a family history of the condition
Pathophysiology
The exact pathophysiology of Raynaud’s disease is not fully understood, but it involves:
- Enhanced vascular reactivity: Exaggerated vasoconstriction in response to cold or emotional stress
- Autonomic dysfunction: Imbalance between vasodilatory and vasoconstrictive stimuli
- Endothelial dysfunction: Impaired release of nitric oxide and increased production of endothelin-1 (a potent vasoconstrictor)
- Viscosity abnormalities: Increased blood viscosity and platelet aggregation
- Neurogenic mechanisms: Abnormal sensitivity of alpha-2 adrenergic receptors in the vascular smooth muscle
During a Raynaud’s attack, the sequence typically involves:
- Initial vasoconstriction: Arterioles and small arteries undergo extreme narrowing
- Reduced oxygen delivery: Tissue hypoxia develops in the affected areas
- Color changes: The characteristic white-blue-red color progression
- Sensory symptoms: Numbness, tingling, and pain during the attack
- Hyperemic response: Vasodilation and reactive hyperemia during recovery
Clinical Manifestations
Raynaud’s disease is characterized by episodic attacks with the following features:
| Phase | Color Change | Pathophysiology | Clinical Manifestations |
|---|---|---|---|
| Initial (Ischemic Phase) | White (pallor) | Arterial vasoconstriction with decreased blood flow | Numbness, coolness, and reduced sensation |
| Middle (Cyanotic Phase) | Blue (cyanosis) | Deoxygenation of residual blood in tissues | Pain, tingling, throbbing sensations |
| Recovery (Hyperemic Phase) | Red (erythema) | Reactive hyperemia as blood flow returns | Throbbing pain, burning sensation, swelling |
Other clinical features include:
- Duration of attacks: Usually 15-20 minutes, but can last longer
- Frequency: Varies from several times per day to occasional episodes
- Distribution: Typically bilateral and symmetrical
- Most commonly affected areas: Fingers (especially 2nd and 3rd digits), toes
- Less commonly affected: Nose, ears, lips, nipples
Types of Raynaud’s Disease
| Feature | Primary Raynaud’s (Disease) | Secondary Raynaud’s (Phenomenon) |
|---|---|---|
| Cause | Idiopathic (unknown) | Associated with underlying conditions |
| Age of onset | Usually younger (teens to 30s) | Often after age 40 |
| Gender | Strong female predominance | Less gender disparity |
| Severity | Generally milder symptoms | Often more severe, painful episodes |
| Complications | Rarely causes tissue damage | May lead to ulcers, tissue necrosis, gangrene |
| Associated conditions | None | Autoimmune (scleroderma, lupus, rheumatoid arthritis) Arterial diseases Carpal tunnel syndrome Medications Occupational (vibration exposure, typing) |
Nursing Care Plans for Raynaud’s Disease
The following nursing care plans address the key nursing diagnoses and interventions for patients with Raynaud’s disease.
1. Nursing Care Plan: Ineffective Peripheral Tissue Perfusion
Expected Outcomes:
- Patient will demonstrate improved peripheral tissue perfusion as evidenced by warm extremities, normal skin color, and capillary refill ≤ 3 seconds within 2 hours of interventions.
- Patient will verbalize understanding of measures to improve circulation within 24 hours.
- Patient will report decreased frequency and severity of vasospastic attacks within 1 week.
Nursing Interventions:
- Assess peripheral circulation: Monitor affected extremities for color changes, temperature, capillary refill, and presence of pulses. Document findings to establish baseline and track improvement.
- Promote vasodilation: Apply warm compresses to affected areas during vasospastic episodes. Maintain ambient room temperature between 70-75°F (21-24°C).
- Encourage gentle movement: Teach patient to perform circular movements with hands and feet during attacks to stimulate circulation.
- Eliminate vasoconstrictive stimuli: Instruct patient to avoid cold exposure, emotional stress, nicotine, and caffeine.
- Administer medications: Administer vasodilator medications as prescribed (e.g., calcium channel blockers, alpha-adrenergic blockers) and monitor effectiveness.
- Position extremities appropriately: Teach patient to keep extremities at or slightly above heart level to promote circulation.
- Encourage regular exercise: Recommend moderate physical activity to improve overall circulation while avoiding excessive cooling from outdoor activities in cold weather.
Evaluation:
Patient demonstrates improved peripheral circulation as evidenced by:
- Warm extremities with normal color
- Capillary refill time less than 3 seconds
- Decreased frequency and severity of vasospastic attacks
- Verbalization of understanding of measures to improve circulation
2. Nursing Care Plan: Acute Pain
Expected Outcomes:
- Patient will report pain reduction from 4/10 to 0-1/10 within 30 minutes of intervention.
- Patient will demonstrate use of non-pharmacological pain management techniques within 24 hours.
- Patient will identify factors that trigger or exacerbate pain within 24 hours.
Nursing Interventions:
- Assess pain characteristics: Determine location, quality, intensity (0-10 scale), duration, and alleviating/aggravating factors of pain during Raynaud’s attacks.
- Monitor vital signs: Assess for tachycardia, hypertension, and increased respiratory rate, which may indicate acute pain.
- Provide comfort measures: Apply warm compresses to affected areas, maintain warm environment, and ensure comfortable positioning of affected extremities.
- Teach non-pharmacological pain management: Instruct on relaxation techniques, deep breathing exercises, guided imagery, and distraction methods.
- Administer analgesics: Provide pain medication as prescribed and evaluate effectiveness.
- Support during episodes: Remain with patient during acute pain episodes, provide reassurance, and help implement pain relief measures.
- Document pain patterns: Help patient maintain a pain diary to identify triggers and evaluate effectiveness of interventions.
Evaluation:
Patient demonstrates pain management as evidenced by:
- Reports pain at 0-1/10 following interventions
- Successfully employs non-pharmacological pain management techniques
- Identifies and avoids factors that trigger or worsen pain
- Shows reduced protective behaviors of affected extremities
3. Nursing Care Plan: Risk for Impaired Skin Integrity
Expected Outcomes:
- Patient will maintain intact skin integrity as evidenced by absence of skin breakdown, ulceration, or infection.
- Patient will demonstrate preventive skin care techniques within 24 hours.
- Patient will verbalize understanding of risk factors for skin breakdown within 24 hours.
Nursing Interventions:
- Perform comprehensive skin assessment: Inspect extremities (especially fingertips and toes) for signs of skin breakdown, ulceration, infections, or necrosis. Document findings.
- Implement preventive skin care: Teach patient to keep skin clean, moisturized, and protected. Apply moisturizing lotion after washing (avoid between toes).
- Prevent trauma: Instruct patient to handle sharp objects carefully, wear protective gloves during activities that could cause trauma, and avoid tight jewelry or clothing.
- Promote proper nail care: Teach patient to trim nails straight across and file edges to prevent ingrown nails and injury.
- Encourage daily skin inspection: Teach patient to inspect extremities daily for any changes, especially after Raynaud’s attacks.
- Address skin injuries promptly: Teach immediate cleansing of minor wounds with mild soap and water, application of antibiotic ointment, and proper bandaging techniques.
- Manage existing skin breakdown: For patients with ulcerations, implement appropriate wound care protocols according to facility guidelines.
Evaluation:
Patient maintains skin integrity as evidenced by:
- Intact skin without breakdown, ulceration, or infection
- Demonstration of proper skin care techniques
- Prompt reporting of any skin changes or concerns
- Verbalization of understanding of risk factors for skin breakdown
4. Nursing Care Plan: Anxiety
Expected Outcomes:
- Patient will report decreased anxiety levels within 24 hours of intervention.
- Patient will demonstrate at least two effective coping strategies to manage anxiety within 48 hours.
- Patient will express increased confidence in managing the disease and its symptoms within 72 hours.
Nursing Interventions:
- Assess anxiety level: Determine severity of anxiety through observation of behavior, verbal reports, and physiological indicators such as increased heart rate and respiratory rate.
- Establish therapeutic relationship: Develop rapport with patient by demonstrating empathy, active listening, and providing emotional support.
- Provide accurate information: Educate patient about Raynaud’s disease, prognosis, treatment options, and self-management strategies to reduce fear of the unknown.
- Teach stress management techniques: Instruct on relaxation methods such as deep breathing, progressive muscle relaxation, meditation, and guided imagery.
- Encourage expression of feelings: Create opportunities for patient to discuss fears and concerns related to the condition.
- Identify stress triggers: Help patient recognize situations that increase anxiety and develop strategies to minimize their impact.
- Promote control over condition: Teach patient to identify early warning signs of attacks and implement immediate interventions to minimize severity.
- Consider referral: If anxiety is severe or persistent, consult with healthcare provider about possible referral to mental health professional.
Evaluation:
Patient demonstrates reduced anxiety as evidenced by:
- Verbal report of decreased anxiety levels
- Demonstration of effective coping strategies
- Improved ability to discuss condition without increased tension
- Decreased physical manifestations of anxiety
- Expression of increased confidence in disease management
5. Nursing Care Plan: Deficient Knowledge
Expected Outcomes:
- Patient will verbalize accurate understanding of Raynaud’s disease, its triggers, and management within 48 hours.
- Patient will demonstrate proper techniques for managing attacks within 24 hours.
- Patient will identify at least five lifestyle modifications to reduce frequency and severity of attacks within 48 hours.
- Patient will verbalize understanding of when to seek medical attention within 24 hours.
Nursing Interventions:
- Assess knowledge level: Determine patient’s current understanding of Raynaud’s disease, identify knowledge gaps, and correct misconceptions.
- Provide disease information: Explain pathophysiology, triggers, symptoms, and possible complications in simple, understandable terms.
- Teach attack management: Demonstrate techniques to manage acute attacks, including warming methods, stress reduction, and position changes.
- Explain medication regimen: Discuss purpose, dosage, schedule, side effects, and importance of adherence for prescribed medications.
- Instruct on preventive measures: Educate about avoiding triggers such as cold exposure, emotional stress, smoking, and certain medications.
- Demonstrate protective strategies: Teach proper layering of clothing, use of gloves/mittens, hand warmers, and other protective gear.
- Explain warning signs: Clarify symptoms that warrant immediate medical attention, such as prolonged color changes, skin ulcers, or intense pain.
- Provide written materials: Supply educational handouts, reliable websites, and community resources for continued learning.
- Verify understanding: Use teach-back method to confirm patient’s comprehension of key information.
Evaluation:
Patient demonstrates knowledge acquisition as evidenced by:
- Accurate description of Raynaud’s disease, its triggers, and management
- Proper demonstration of techniques for managing attacks
- Identification of appropriate lifestyle modifications
- Clear understanding of when to seek medical attention
- Correction of previous misconceptions about the condition
6. Nursing Care Plan: Risk for Injury
Expected Outcomes:
- Patient will remain free from injury throughout care.
- Patient will demonstrate safety precautions within 24 hours.
- Patient will identify potential hazards in home and workplace within 48 hours.
Nursing Interventions:
- Assess sensory function: Evaluate sensation, temperature perception, and proprioception in affected extremities.
- Evaluate dexterity: Observe patient’s ability to perform fine motor tasks, especially during or after vasospastic episodes.
- Identify environmental hazards: Help patient recognize potential dangers in home and workplace environments, especially related to temperature extremes and sharp objects.
- Teach protective measures: Instruct on wearing protective gloves when handling hot items, sharp objects, or harsh chemicals.
- Promote assistive devices: Recommend tools with larger grips, electric can openers, or other assistive devices for tasks requiring manual dexterity.
- Advise temperature testing: Teach patient to test water temperature with unaffected body part or thermometer before immersion.
- Encourage workspace modifications: Suggest ergonomic adjustments such as padded keyboard rests, heated mouse pads, and proper hand positioning during computer use.
- Recommend home safety measures: Advise installing slip-resistant surfaces in bathrooms, adequate lighting, and keeping walkways clear.
Evaluation:
Patient demonstrates injury prevention as evidenced by:
- Absence of injuries related to sensation or dexterity deficits
- Consistent use of protective measures during daily activities
- Identification and modification of potential hazards in environment
- Appropriate use of assistive devices when needed
7. Nursing Care Plan: Disturbed Body Image
Expected Outcomes:
- Patient will express increased acceptance of body changes within 1 week.
- Patient will demonstrate positive coping strategies for dealing with visible symptoms within 72 hours.
- Patient will maintain social interactions without undue concern about appearance within 1 week.
Nursing Interventions:
- Assess body image concerns: Explore patient’s feelings about visible manifestations of Raynaud’s disease and their impact on self-concept.
- Validate feelings: Acknowledge patient’s concerns as legitimate without minimizing them.
- Provide emotional support: Create a non-judgmental environment where patient can openly discuss body image issues.
- Explore adaptive responses: Help patient identify positive ways to cope with visible symptoms, such as focusing on strengths and capabilities rather than appearance.
- Discuss camouflage techniques: When appropriate, suggest strategies such as gloves, mittens, or nail polish to minimize the visibility of symptoms in social situations.
- Connect with support resources: Provide information about support groups, online communities, or counseling services for people with Raynaud’s disease.
- Emphasize normal aspects: Help patient recognize that symptoms are temporary and that between episodes, appearance is typically normal.
- Encourage social engagement: Support continued participation in valued activities and relationships despite concerns about appearance.
Evaluation:
Patient demonstrates improved body image as evidenced by:
- Expressions of increased acceptance of body changes
- Decreased negative comments about appearance
- Reduced tendency to hide affected areas
- Maintenance of social interactions without undue focus on appearance
- Use of positive coping strategies when facing body image challenges
8. Nursing Care Plan: Ineffective Thermoregulation
Expected Outcomes:
- Patient will maintain comfortable body temperature with appropriate interventions within 24 hours.
- Patient will demonstrate effective warming techniques within 24 hours.
- Patient will verbalize understanding of thermoregulation strategies within 48 hours.
Nursing Interventions:
- Assess temperature sensitivity: Determine patient’s threshold for cold-induced symptoms and responses to various environmental temperatures.
- Maintain environmental warmth: Ensure comfortable room temperature (70-75°F/21-24°C) and minimize exposure to drafts or air conditioning.
- Teach layering techniques: Instruct on proper clothing layering to trap body heat, with focus on core warmth to promote peripheral circulation.
- Recommend specialized clothing: Suggest thermal gloves, mittens, socks, and battery-operated heated garments designed for people with cold sensitivity.
- Demonstrate warming methods: Teach safe techniques for warming affected extremities, such as placing hands under armpits or using lukewarm (not hot) water.
- Caution against extreme temperatures: Advise against direct exposure to heat sources like radiators or heating pads, which may damage insensitive skin.
- Suggest core warming strategies: Recommend warm beverages and regular meals to maintain internal body temperature.
- Advise transition planning: Teach patient to prepare for temperature changes when moving between environments (e.g., wearing gloves before entering cold areas).
Evaluation:
Patient demonstrates effective thermoregulation as evidenced by:
- Maintenance of comfortable body temperature with appropriate interventions
- Proper use of warming techniques and protective clothing
- Decreased frequency of cold-induced vasospastic episodes
- Verbalization of understanding of thermoregulation strategies
- Proactive measures to prevent cold exposure
9. Nursing Care Plan: Impaired Comfort
Expected Outcomes:
- Patient will report improved comfort within 1 hour of interventions during vasospastic episodes.
- Patient will demonstrate use of at least three comfort enhancement techniques within 48 hours.
- Patient will express satisfaction with comfort measures within 72 hours.
Nursing Interventions:
- Assess comfort status: Evaluate nature of discomfort, including location, quality, intensity, and factors that improve or worsen it.
- Create comfortable environment: Maintain appropriate temperature, reduce noise, provide adequate lighting, and ensure comfortable positioning.
- Apply warming techniques: Use warm compresses, warming mitts, or tepid water soaks for affected extremities during episodes.
- Recommend comfortable clothing: Suggest loose-fitting, soft garments that don’t constrict circulation and provide adequate warmth.
- Teach massage techniques: Demonstrate gentle massage of unaffected areas to promote relaxation and overall comfort.
- Encourage distraction methods: Suggest engaging activities that divert attention from discomfort, such as reading, listening to music, or conversation.
- Provide emotional support: Offer reassurance during uncomfortable episodes and acknowledge the legitimacy of the patient’s experience.
- Administer medications: Provide prescribed medications for symptom management and evaluate effectiveness.
Evaluation:
Patient demonstrates improved comfort as evidenced by:
- Verbal reports of increased comfort following interventions
- Decreased restlessness and irritability during attacks
- Effective use of comfort enhancement techniques
- Expression of satisfaction with comfort measures
- Improved ability to engage in daily activities despite occasional symptoms
10. Nursing Care Plan: Activity Intolerance
Expected Outcomes:
- Patient will report increased ability to perform daily activities within 1 week.
- Patient will demonstrate adaptive techniques for activity completion within 72 hours.
- Patient will identify activities that trigger symptoms and develop appropriate modifications within 48 hours.
Nursing Interventions:
- Assess activity limitations: Determine specific activities affected by Raynaud’s symptoms and their impact on daily functioning.
- Identify triggers: Help patient recognize activity-related triggers for vasospastic episodes (e.g., grasping cold objects, repetitive hand movements).
- Plan activity timing: Suggest scheduling demanding activities during periods when symptoms are typically less severe.
- Teach energy conservation: Demonstrate techniques such as pacing, priority setting, and planned rest periods to minimize fatigue.
- Recommend adaptive equipment: Suggest tools such as jar openers, easy-grip utensils, or button hooks to compensate for decreased dexterity.
- Encourage regular exercise: Promote appropriate exercise that improves circulation without exacerbating symptoms, such as indoor walking or swimming in heated pools.
- Demonstrate activity modifications: Show alternative ways to perform challenging tasks that reduce stress on affected extremities.
- Suggest preventive measures: Advise warming extremities before activity and wearing appropriate protective gear during tasks.
Evaluation:
Patient demonstrates improved activity tolerance as evidenced by:
- Increased participation in daily activities
- Decreased reports of activity-related fatigue
- Successful use of adaptive techniques and equipment
- Appropriate modification of activities to prevent symptom exacerbation
- Expression of increased confidence in ability to manage activities
11. Nursing Care Plan: Ineffective Coping
Expected Outcomes:
- Patient will demonstrate at least three effective coping strategies within 1 week.
- Patient will express increased confidence in ability to manage disease within 72 hours.
- Patient will identify personal and community resources for ongoing support within 48 hours.
Nursing Interventions:
- Assess coping patterns: Evaluate current coping mechanisms, their effectiveness, and areas needing improvement.
- Facilitate expression of feelings: Encourage verbalization of frustrations, fears, and challenges related to living with Raynaud’s disease.
- Normalize emotional responses: Reassure patient that feelings of frustration or discouragement are common reactions to chronic conditions.
- Teach stress management: Instruct in techniques such as deep breathing, progressive muscle relaxation, and mindfulness to reduce stress that can trigger symptoms.
- Promote problem-solving: Help patient identify specific challenges and develop practical solutions, such as planning ahead for weather changes.
- Encourage self-efficacy: Recognize and reinforce patient’s successful management of symptoms to build confidence.
- Identify support systems: Explore personal and community resources available for ongoing support and assistance.
- Suggest peer connection: Provide information about support groups or online communities for people with Raynaud’s disease.
- Consider referral: If coping difficulties persist, discuss potential benefit of counseling or psychological support.
Evaluation:
Patient demonstrates effective coping as evidenced by:
- Use of appropriate coping strategies when facing challenges
- Decreased expressions of frustration and helplessness
- Improved problem-solving related to disease management
- Increased confidence in ability to handle symptom flares
- Engagement with support resources when needed
- Adaptive integration of disease management into daily life
12. Nursing Care Plan: Self-Care Deficit
Expected Outcomes:
- Patient will perform self-care activities independently or with minimal assistance within 1 week.
- Patient will demonstrate use of adaptive equipment and techniques for self-care within 72 hours.
- Patient will verbalize strategies for managing self-care during symptomatic episodes within 48 hours.
Nursing Interventions:
- Assess self-care abilities: Evaluate specific areas of difficulty in activities of daily living, particularly those requiring manual dexterity.
- Promote independence: Encourage patient to perform self-care activities to the fullest extent possible while providing assistance as needed.
- Teach adaptive techniques: Demonstrate modified approaches to challenging tasks, such as using palms instead of fingers for certain activities.
- Recommend assistive devices: Suggest tools such as button hooks, zipper pulls, elastic shoelaces, and easy-grip handles for personal care items.
- Modify clothing choices: Advise selection of clothing with simple closures (Velcro, large buttons, slip-ons) that are easier to manage during episodes.
- Arrange environment: Suggest organization of living space to promote accessibility and minimize need for fine motor skills (e.g., pre-opening containers).
- Develop symptom management plan: Create strategies for completing essential self-care during symptomatic periods, including preparation and timing.
- Consult occupational therapy: Consider referral for specialized assessment and recommendations for adaptive techniques.
Evaluation:
Patient demonstrates improved self-care ability as evidenced by:
- Independent performance of self-care activities with minimal assistance
- Effective use of adaptive equipment and techniques
- Decreased frustration during personal care tasks
- Successful management of self-care during symptomatic episodes
- Verbalization of satisfaction with level of independence
Home Care Advice for Patients with Raynaud’s Disease
The following home care recommendations will help patients manage Raynaud’s disease effectively and prevent complications:
Temperature Management
- Home climate control: Maintain indoor temperature between 70-75°F (21-24°C). Use programmable thermostats to prevent temperature drops at night.
- Layered clothing: Wear multiple thin layers rather than one thick layer. This traps warm air between layers and provides better insulation.
- Extremity protection: Keep hands and feet warm at all times. Wear insulated gloves, mittens, or socks even when indoors if necessary.
- Core warmth: Focus on keeping your core warm to promote circulation to extremities. Wear thermal underwear, vests, and scarves.
- Hand and foot warmers: Use chemical or rechargeable hand and foot warmers inside gloves and shoes during cold weather or when planning outdoor activities.
- Warm baths and showers: Use lukewarm (not hot) water for bathing to improve circulation without damaging sensitive skin.
Practical Daily Living Tips
- Transition planning: Wear gloves when taking items from the refrigerator or freezer. Carry gloves to use in air-conditioned buildings.
- Grocery shopping: Bring gloves to wear in frozen food aisles. Consider wearing gloves with grip when handling cold shopping carts.
- Meal preparation: Run warm water over frozen foods before handling. Use oven mitts or pot holders when reaching into refrigerator.
- Vehicle preparation: Start and warm car before traveling in cold weather. Consider a remote starter or heated steering wheel cover.
- Work environment: Use a space heater (if permitted), fingerless gloves for typing, and ergonomic equipment to reduce strain.
- Sleep environment: Use electric blankets (pre-heat bed before sleeping), flannel sheets, and keep warm sleepwear nearby for nighttime bathroom trips.
Attack Management at Home
- Early intervention: Act at the first sign of an attack. Warm the affected area immediately to minimize symptom severity.
- Warming techniques: Place hands under armpits, against warm skin of abdomen, or in lukewarm (not hot) water.
- Movement: Perform gentle arm swinging, finger wiggling, or circular arm movements to stimulate circulation.
- Stress reduction: Practice deep breathing or quick relaxation techniques at the onset of symptoms.
- Immediate environment change: Move to a warmer area, away from air conditioning vents or cold drafts.
Skin and Wound Care
- Daily inspection: Check fingers, toes, and other affected areas daily for cuts, cracks, or changes in appearance.
- Moisturizing: Apply hypoallergenic moisturizer to hands and feet after bathing while skin is still slightly damp (avoid between toes).
- Gentle cleaning: Wash with lukewarm water and mild soap. Pat dry gently rather than rubbing.
- Nail care: Trim nails carefully and straight across. File rough edges to prevent catches and tears.
- Minor injury care: Clean cuts or scrapes promptly with mild soap and water. Apply antibiotic ointment and appropriate bandage.
- Ulcer prevention: Protect vulnerable areas with padded bandages or liquid bandage products before activities that might cause trauma.
Lifestyle Modifications
- Smoking cessation: Quit smoking and avoid secondhand smoke, as nicotine causes vasoconstriction.
- Caffeine moderation: Limit caffeine intake, which can trigger vasospasm in some people with Raynaud’s.
- Regular exercise: Engage in regular physical activity to improve overall circulation. Choose indoor activities during cold weather.
- Stress management: Practice regular stress reduction techniques such as meditation, yoga, or deep breathing.
- Diet considerations: Maintain a heart-healthy diet rich in omega-3 fatty acids, which may help improve circulation.
- Hydration: Drink adequate fluids to maintain proper blood volume and circulation.
Medication Management
- Medication adherence: Take prescribed medications regularly and as directed, even when symptoms are minimal.
- Medication timing: For medications taken to prevent attacks, establish a routine that ensures consistent blood levels.
- Side effect monitoring: Track and report any side effects or changes in symptom patterns to healthcare provider.
- Over-the-counter awareness: Check with healthcare provider before using OTC cold or allergy medications, as some contain vasoconstrictors.
- Medication organization: Use pill organizers or smartphone reminders to maintain consistent medication schedule.
When to Seek Medical Attention
- Prolonged attacks: Seek medical care if color changes last more than 2-3 hours despite warming efforts.
- Skin ulcers: Contact healthcare provider if you develop sores or ulcers on fingers or toes.
- Infection signs: Seek attention for increased pain, warmth, redness, swelling, or discharge from any skin breaks.
- Severe pain: Report pain that is unusually severe or unresponsive to usual management techniques.
- Tissue discoloration: Seek emergency care for persistent black or dark blue discoloration that doesn’t resolve.
- New symptoms: Contact provider if you develop new or changing symptoms that might indicate progression or complications.
Patient Education Resources
Effective education is crucial for patients with Raynaud’s disease to manage their condition successfully. Healthcare providers should direct patients to reliable resources for ongoing learning and support.
Educational Topics to Cover
- Basic understanding of Raynaud’s disease pathophysiology
- Distinction between primary and secondary Raynaud’s
- Common triggers and how to avoid them
- Early recognition of attacks and immediate interventions
- Proper use of medications and potential side effects
- Warning signs that require medical attention
- Skin care and wound prevention strategies
- Adaptive techniques for daily activities
- Emotional coping strategies
- Available community resources and support groups
Teaching Methods
- Provide written materials with key information for reference
- Demonstrate techniques for warming and protecting extremities
- Use visual aids to explain the disease process
- Employ teach-back method to confirm understanding
- Schedule follow-up education sessions to reinforce learning
- Include family members or caregivers in education when appropriate
References
- Mayo Clinic. (2024). Raynaud’s disease – Diagnosis and treatment. https://www.mayoclinic.org/diseases-conditions/raynauds-disease/diagnosis-treatment/drc-20363572
- Cleveland Clinic. (2023). Raynaud’s Syndrome: Symptoms, Causes & Treatment. https://my.clevelandclinic.org/health/diseases/9849-raynauds-phenomenon
- Nursing Times. (2003). Raynaud’s syndrome. https://www.nursingtimes.net/respiratory/raynauds-syndrome-22-07-2003/
- Raynaud’s Association. (2015). Advice to Nurses on Treating Raynaud’s. https://www.raynauds.org/2015/06/07/advice-to-nurses-on-treating-raynauds/
- NurseTogether. (2025). Ineffective Tissue Perfusion Nursing Diagnosis & Care Plans. https://www.nursetogether.com/ineffective-tissue-perfusion-nursing-diagnosis-care-plan/
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2019). Nurse’s pocket guide: Diagnoses, prioritized interventions, and rationales (15th ed.). F.A. Davis Company.
- Ackley, B. J., Ladwig, G. B., Makic, M. B. F., Martinez-Kratz, M., & Zanotti, M. (2020). Nursing diagnosis handbook: An evidence-based guide to planning care (12th ed.). Elsevier.
- Carpenito, L. J. (2017). Nursing diagnosis: Application to clinical practice (15th ed.). Wolters Kluwer.
