High Risk Newborn: Respiratory Distress
Comprehensive Nursing Notes for Student Nurses
Table of Contents
Introduction to Neonatal Respiratory Distress
Neonatal respiratory distress represents one of the most common and serious challenges in the care of high-risk newborns. Affecting approximately 7% of all neonates, it accounts for about 30% of all neonatal mortality worldwide. The successful management of a newborn with respiratory distress requires prompt recognition, appropriate assessment, and timely intervention.
Respiratory distress in newborns presents as a constellation of clinical signs indicating the baby is struggling to maintain adequate oxygenation and ventilation. The underlying causes can range from transient tachypnea of the newborn to severe conditions like respiratory distress syndrome (RDS) or meconium aspiration syndrome.
Key Concept
Neonatal respiratory distress is a clinical presentation, not a specific disease. It requires both immediate supportive care and treatment of the underlying cause.
Pathophysiology
Neonatal respiratory distress develops when there is a disruption in the normal transition from fetal to neonatal respiration. This transition involves multiple physiological changes:
Fetal-to-Neonatal Transition
- Clearance of fetal lung fluid
- Establishment of regular breathing patterns
- Pulmonary vascular resistance decrease
- Increased pulmonary blood flow
- Surfactant function activation
Disruptions Leading to Distress
- Inadequate clearance of lung fluid
- Surfactant deficiency or dysfunction
- Airway obstruction
- Mechanical restriction of lung expansion
- Central nervous system abnormalities affecting respiration
Respiratory Mechanisms and Adaptations
Neonatal respiratory distress often involves one or more of these pathophysiologic mechanisms:
- Ventilation-perfusion mismatch: Areas of the lung receive inadequate ventilation relative to perfusion
- Diffusion impairment: Thickened alveolar-capillary membrane prevents efficient gas exchange
- Hypoventilation: Inadequate minute ventilation leads to CO2 retention and hypoxemia
- Right-to-left shunting: Deoxygenated blood bypasses the lungs and enters systemic circulation
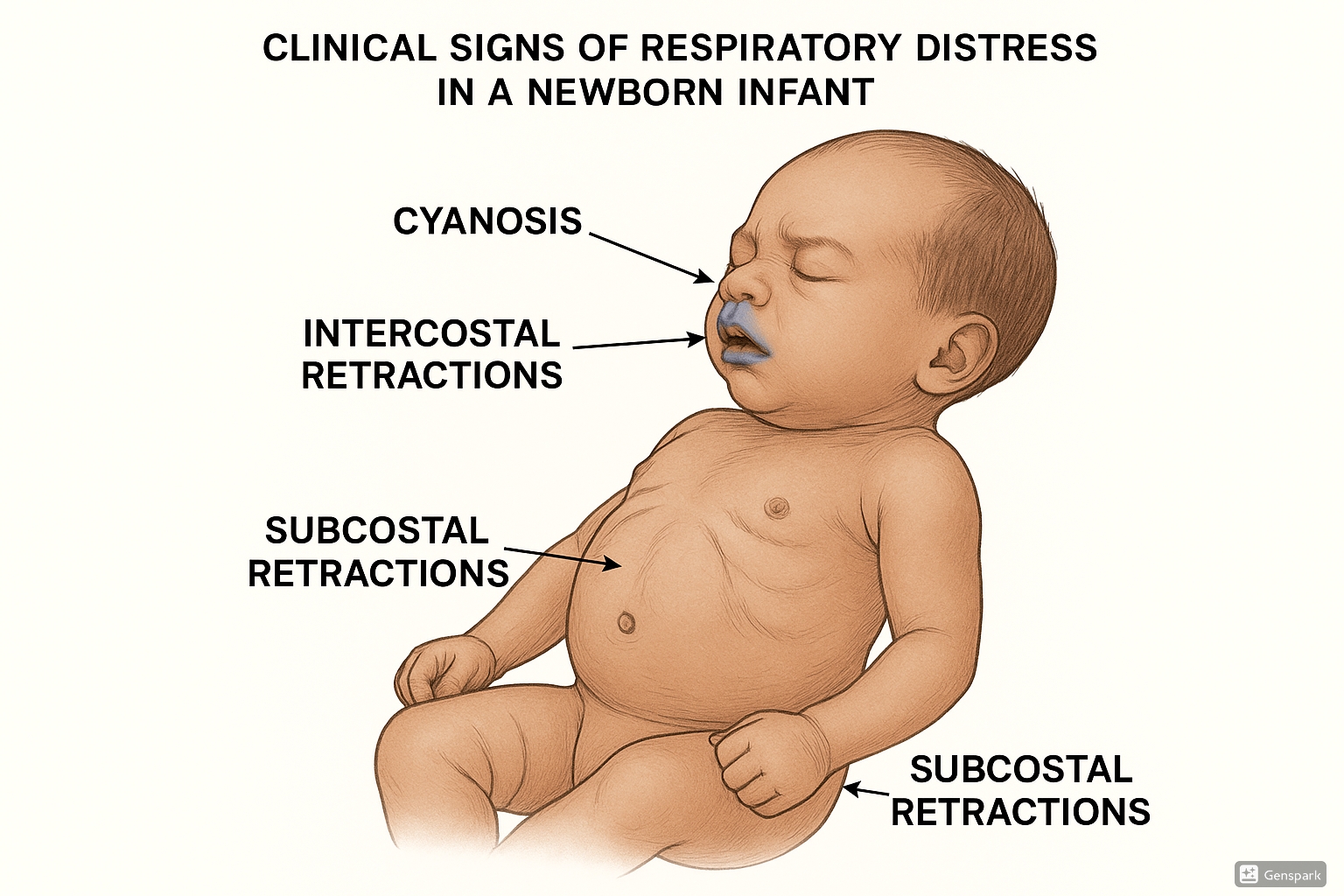
Figure 1: Clinical signs of neonatal respiratory distress including intercostal retractions, subcostal retractions, nasal flaring, and cyanosis
Risk Factors
Various maternal, perinatal, and neonatal factors increase the risk of neonatal respiratory distress:
| Maternal Factors | Perinatal Factors | Neonatal Factors |
|---|---|---|
| Diabetes mellitus | Cesarean delivery (especially without labor) | Prematurity (<37 weeks) |
| Hypertensive disorders | Prolonged labor | Low birth weight (<2500g) |
| Chorioamnionitis | Meconium-stained amniotic fluid | Male gender |
| Substance abuse | Fetal distress | Congenital anomalies |
| Inadequate prenatal care | Precipitous delivery | Multiple gestation |
| Maternal age <20 or >35 | Cord prolapse/compression | Perinatal asphyxia |
Clinical Insight
Cesarean section without labor increases neonatal respiratory distress risk by 2-4 times compared to vaginal delivery, primarily due to inadequate clearance of fetal lung fluid.
Clinical Manifestations
Early recognition of neonatal respiratory distress is crucial for prompt intervention. Key clinical signs include:
Primary Signs
- Tachypnea: Respiratory rate >60 breaths per minute
- Nasal flaring: Widening of nostrils during inspiration
- Grunting: Audible expiratory sound as infant attempts to maintain positive end-expiratory pressure
- Retractions: Visible pulling in of tissues between ribs (intercostal), below ribs (subcostal), or above sternum (suprasternal)
- Cyanosis: Bluish discoloration of skin, mucous membranes, or nail beds
Associated Findings
- Seesaw respirations: Paradoxical chest and abdominal movement
- Decreased air entry: Reduced breath sounds on auscultation
- Abnormal breath sounds: Crackles, wheezing, or rhonchi
- Altered mental status: Lethargy or irritability
- Poor feeding: Inability to coordinate sucking, swallowing, and breathing
- Apneic episodes: Pauses in breathing >20 seconds
Severity Assessment
Several scoring systems help evaluate the severity of neonatal respiratory distress. One commonly used system is the Silverman-Andersen score:
| Parameter | 0 Points | 1 Point | 2 Points |
|---|---|---|---|
| Upper chest movement | Synchronized | Lag on inspiration | See-saw motion |
| Lower chest retraction | None | Just visible | Marked |
| Xiphoid retraction | None | Just visible | Marked |
| Nares dilation | None | Minimal | Marked |
| Expiratory grunt | None | Audible by stethoscope | Audible by unaided ear |
Interpretation: 0 = no distress; 1-3 = mild distress; 4-6 = moderate distress; 7-10 = severe distress
Common Causes of Neonatal Respiratory Distress
Mnemonic for Causes: “RESPIRATORY”
- R – Respiratory Distress Syndrome (surfactant deficiency)
- E – Encephalopathy or neurological disorders
- S – Sepsis or pneumonia
- P – Persistent Pulmonary Hypertension of the Newborn (PPHN)
- I – Inhalation of meconium, amniotic fluid, or milk
- R – Retained lung fluid (Transient Tachypnea of Newborn)
- A – Airway malformations or obstruction
- T – Thoracic abnormalities (pneumothorax, diaphragmatic hernia)
- O – Overheating/hypothermia affecting metabolic demand
- R – Rare congenital disorders
- Y – Yielding to cardiac causes (congenital heart defects)
Major Respiratory Conditions
1. Respiratory Distress Syndrome (RDS)
Primarily affects premature infants due to surfactant deficiency. Characterized by progressive respiratory failure, diffuse atelectasis, and hyaline membrane formation.
2. Transient Tachypnea of the Newborn (TTN)
Results from delayed clearance of fetal lung fluid. Common after cesarean delivery without labor. Usually self-limiting within 24-72 hours.
3. Meconium Aspiration Syndrome (MAS)
Occurs when a fetus gasps in utero, inhaling meconium-stained amniotic fluid. Causes airway obstruction, chemical pneumonitis, and surfactant inactivation.
4. Pneumonia
Can be congenital (transmitted in utero) or acquired during or after birth. Common pathogens include Group B Streptococcus, E. coli, and Listeria monocytogenes.
5. Persistent Pulmonary Hypertension of the Newborn (PPHN)
A failure of normal pulmonary vascular transition resulting in right-to-left shunting and severe hypoxemia resistant to oxygen therapy.
Assessment
Comprehensive assessment of a newborn with respiratory distress includes history taking, physical examination, and relevant investigations.
History
- Maternal risk factors and conditions
- Gestational age and birth weight
- Mode of delivery
- Apgar scores
- Resuscitation details, if performed
- Onset and progression of respiratory symptoms
Physical Examination
Mnemonic for Physical Assessment: “ABCDE”
- A – Airway: Check patency, position, and secretions
- B – Breathing: Assess rate, rhythm, effort, and breath sounds
- C – Circulation: Evaluate heart rate, pulses, capillary refill, and blood pressure
- D – Disability: Check neurological status, tone, and responsiveness
- E – Exposure: Examine for congenital anomalies, color, and temperature
Respiratory Assessment Details
| Assessment Parameter | Normal Findings | Abnormal Findings |
|---|---|---|
| Respiratory Rate | 40-60 breaths/minute | Tachypnea (>60/min) or bradypnea (<30/min) |
| Respiratory Pattern | Regular, symmetrical | Irregular, paradoxical, or periodic breathing |
| Chest Wall Movement | Synchronized chest and abdomen | Retractions, asymmetry, or see-saw respirations |
| Breath Sounds | Clear and equal bilaterally | Decreased, asymmetrical, or adventitious sounds |
| Color | Pink | Central or peripheral cyanosis, pallor, or mottling |
Diagnostic Tests
Accurate diagnosis of the underlying cause of neonatal respiratory distress requires appropriate diagnostic testing.
Initial Tests
- Pulse oximetry: Continuous monitoring of oxygen saturation
- Blood gas analysis: Arterial, capillary, or venous blood gases to assess oxygenation, ventilation, and acid-base status
- Chest radiography: To identify specific patterns associated with different conditions
- Complete blood count: To evaluate for infection or anemia
- Blood cultures: If infection is suspected
Additional Tests as Indicated
- Echocardiography: For suspected congenital heart disease or PPHN
- Cranial ultrasound: For assessment of intraventricular hemorrhage
- CT or MRI: For complex congenital anomalies
- Bronchoscopy: For suspected airway abnormalities
- Genetic studies: For suspected genetic syndromes
Interpretation of Chest X-ray Patterns
| Condition | Radiographic Findings |
|---|---|
| Respiratory Distress Syndrome (RDS) | Diffuse ground-glass appearance, air bronchograms, decreased lung volume |
| Transient Tachypnea of the Newborn (TTN) | Hyperinflation, fluid in fissures, prominent central vascular markings |
| Meconium Aspiration Syndrome (MAS) | Patchy irregular infiltrates, hyperinflation, areas of atelectasis |
| Pneumonia | Focal or diffuse opacities, pleural effusions possible |
| Pneumothorax | Free air in pleural space, mediastinal shift away from affected side |
| Congenital Diaphragmatic Hernia | Bowel loops in thorax, mediastinal shift, lung hypoplasia |
Management
Management of neonatal respiratory distress follows a systematic approach while addressing the specific underlying cause.
General Supportive Measures
- Thermoregulation: Maintain normal body temperature (36.5-37.5°C)
- Fluid and electrolyte management: Ensure adequate hydration and glucose levels
- Minimal handling: Cluster care activities to reduce stress and oxygen consumption
- Positioning: Slight head elevation (15-30°) and neutral neck position
- Continuous monitoring: Heart rate, respiratory rate, oxygen saturation, blood pressure
Respiratory Support
Respiratory support follows a stepwise approach based on severity:
| Support Level | Indication | Description |
|---|---|---|
| Supplemental oxygen | Mild hypoxemia (SpO₂ 90-94%) | Delivered via nasal cannula, oxygen hood, or mask to maintain target SpO₂ 90-95% (preterm) or 92-97% (term) |
| Continuous Positive Airway Pressure (CPAP) | Moderate distress, SpO₂ <90% despite O₂ | Provides positive pressure (5-8 cm H₂O) via nasal prongs or mask; maintains alveolar expansion |
| High-Flow Nasal Cannula (HFNC) | Alternative to CPAP in select cases | Delivers heated, humidified oxygen at high flow rates (4-8 L/min); provides low levels of distending pressure |
| Non-invasive ventilation (NIV) | Apnea, increasing work of breathing despite CPAP | Includes nasal intermittent positive pressure ventilation (NIPPV); provides intermittent breaths |
| Mechanical ventilation | Severe distress, respiratory failure, or refractory hypoxemia | Conventional: pressure or volume-controlled ventilation High-frequency: oscillatory or jet ventilation for severe cases |
Specific Treatments
1. Respiratory Distress Syndrome (RDS)
- Surfactant replacement therapy: Endotracheal administration of exogenous surfactant
- Early CPAP with selective surfactant administration
- Antenatal corticosteroids if preterm delivery anticipated
2. Transient Tachypnea of the Newborn (TTN)
- Supportive care and oxygen as needed
- Usually self-resolving within 24-72 hours
3. Meconium Aspiration Syndrome (MAS)
- Respiratory support as needed
- Surfactant lavage in severe cases
- Antibiotics if secondary infection suspected
- Consider inhaled nitric oxide for PPHN
4. Pneumonia
- Empiric antibiotic therapy
- Respiratory support as needed
- Adjust antibiotics based on culture results
5. Persistent Pulmonary Hypertension of the Newborn (PPHN)
- Optimize oxygenation and ventilation
- Inhaled nitric oxide (iNO)
- Maintain normal blood pressure
- Consider ECMO (Extracorporeal Membrane Oxygenation) in severe cases
Important Caution
Oxygen is a medication and should be titrated carefully. Hyperoxia can lead to oxygen toxicity, particularly in premature infants (retinopathy of prematurity, bronchopulmonary dysplasia).
Nursing Interventions
Nursing care of the newborn with neonatal respiratory distress is critical for favorable outcomes. Key nursing interventions include:
Mnemonic for Nursing Care: “BREATHE”
- B – Breathing assessment: Continuous monitoring of respiratory status
- R – Respiratory support: Proper implementation and maintenance
- E – Environment: Maintaining thermoneutral environment
- A – Airway clearance: Proper suctioning techniques
- T – Tissue perfusion: Monitoring and maintaining adequate circulation
- H – Handling: Minimal and clustered care
- E – Education: Family support and teaching
Detailed Nursing Interventions
Assessment and Monitoring
- Perform systematic respiratory assessment every 1-4 hours based on condition
- Monitor vital signs, including continuous pulse oximetry
- Assess work of breathing: retractions, nasal flaring, grunting
- Monitor blood gas results and correlate with clinical status
- Assess fluid balance and weight changes
Respiratory Support Management
- Ensure proper fit of respiratory equipment
- Monitor oxygen saturation and titrate oxygen as ordered
- Properly position infant to optimize ventilation
- Maintain patency of respiratory equipment
- Document ventilator parameters and changes
Supportive Care
- Maintain thermoregulation using warming devices
- Position infant with slight neck extension to maintain airway
- Provide oral care and suction as needed
- Implement developmental care principles
- Administer medications as prescribed (surfactant, antibiotics)
- Support nutrition through parenteral or enteral routes as appropriate
Family Support
- Explain equipment and procedures to parents
- Promote bonding through touch and involvement when stable
- Provide emotional support and regular updates
- Teach parents recognition of respiratory distress signs
- Prepare for discharge and follow-up care
Documentation
Thorough documentation is essential for continuity of care and should include:
- Respiratory assessment findings
- Oxygen therapy details (method, concentration, flow rate)
- Ventilator parameters if applicable
- Response to interventions
- Medications administered
- Parental teaching and support provided
Complications
Neonatal respiratory distress can lead to several short-term and long-term complications:
Short-term Complications
- Air leak syndromes: Pneumothorax, pneumomediastinum, pneumopericardium
- Respiratory failure: Progressive deterioration requiring escalation of support
- Pulmonary hypertension: Persistent or secondary
- Metabolic acidosis: Due to tissue hypoxia and increased anaerobic metabolism
- Infection: Nosocomial pneumonia, sepsis
- Necrotizing enterocolitis: Particularly in preterm infants with compromised gut perfusion
Long-term Complications
- Bronchopulmonary dysplasia (BPD): Chronic lung disease following prolonged oxygen and ventilator support
- Neurodevelopmental impairment: Related to hypoxic episodes or complications of prematurity
- Retinopathy of prematurity: Related to oxygen exposure in premature infants
- Growth failure: Due to increased energy expenditure and feeding difficulties
- Reactive airway disease: Increased risk of asthma and recurrent wheezing
- Pulmonary hypertension: Persistent cases may develop chronic pulmonary hypertension
Critical Warning Sign
Worsening respiratory status despite maximal support, decreasing oxygen saturation, or increasing work of breathing may indicate impending respiratory failure requiring immediate intervention.
Prevention Strategies
Several strategies can help prevent or reduce the severity of neonatal respiratory distress:
Prenatal Prevention
- Prenatal care: Regular monitoring to identify high-risk pregnancies
- Antenatal corticosteroids: For women at risk of preterm delivery between 24-34 weeks
- Antibiotics for Group B Streptococcus: For colonized mothers or those with risk factors
- Tocolytic therapy: Short-term delay of preterm birth to allow steroid effect
- Maternal disease management: Control of diabetes, hypertension, and other conditions
Perinatal Prevention
- Delayed cord clamping: For improved cardiopulmonary transition
- Appropriate delivery planning: Based on gestational age and maternal/fetal conditions
- Skilled resuscitation team: Available for high-risk deliveries
- Optimal timing of elective cesarean section: After 39 weeks when possible
Postnatal Prevention
- Early continuous positive airway pressure (CPAP): For preterm infants showing early signs of respiratory distress
- Prophylactic surfactant: For extremely preterm infants at high risk for RDS
- Caffeine therapy: For prevention of apnea of prematurity
- Infection prevention: Hand hygiene and other infection control measures
- Thermoregulation: Preventing cold stress which increases oxygen consumption
Prognosis
The prognosis for newborns with respiratory distress varies widely depending on several factors:
Prognostic Factors
| Favorable Factors | Unfavorable Factors |
|---|---|
| Term or late preterm gestation | Extreme prematurity (<28 weeks) |
| Transient causes (e.g., TTN) | Severe underlying condition (e.g., congenital diaphragmatic hernia) |
| Prompt response to interventions | Persistent hypoxemia despite maximal support |
| Limited duration of mechanical ventilation | Prolonged mechanical ventilation (>14 days) |
| Absence of complications | Development of BPD or other complications |
| Access to advanced neonatal care | Limited resources or specialized care |
Condition-Specific Outcomes
- Transient Tachypnea of the Newborn: Excellent prognosis with complete recovery expected
- Respiratory Distress Syndrome: Generally good outcome with modern therapies, though risk of BPD in severe cases
- Meconium Aspiration Syndrome: Variable prognosis; mild cases recover well, severe cases may have long-term respiratory issues
- Pneumonia: Good outcome with prompt treatment; may be worse if complicated by sepsis
- Persistent Pulmonary Hypertension: Improved outcomes with inhaled nitric oxide; some cases remain challenging
- Congenital anomalies: Depends on specific condition; some may require long-term management
Follow-up Care
Infants with severe or prolonged neonatal respiratory distress should have regular follow-up to monitor for long-term respiratory issues, neurodevelopmental outcomes, growth, and hearing and vision screening.
Global Best Practices
Around the world, various approaches and innovations are helping improve outcomes for newborns with respiratory distress:
Notable International Approaches
1. Kangaroo Mother Care (KMC)
Originally developed in Colombia, KMC involves skin-to-skin contact between mother and baby, exclusive or nearly exclusive breastfeeding, and early discharge with close follow-up. Studies show KMC reduces mortality and respiratory morbidity in stable preterm infants.
2. Bubble CPAP in Low-Resource Settings
Pioneered in Malawi and other developing countries, bubble CPAP provides low-cost respiratory support without mechanical ventilation. This approach has significantly reduced mortality in settings where ventilators are unavailable.
3. The MIST Technique (Sweden)
Minimally Invasive Surfactant Therapy (MIST) allows administration of surfactant without intubation, reducing ventilator-associated complications. This technique involves inserting a thin catheter into the trachea while the infant breathes spontaneously.
4. Japanese Approach to Gentle Ventilation
Japanese NICUs have pioneered gentler ventilation strategies emphasizing minimal pressure, permissive hypercapnia, and early weaning, resulting in lower rates of BPD.
5. European “Golden Hour” Protocol
Standardized approach to the first hour of life for preterm infants, focusing on temperature control, respiratory management, infection prevention, and glucose monitoring. Implementation has improved outcomes in multiple European NICUs.
Future Directions
- Artificial intelligence: For early prediction of respiratory deterioration
- Lung-protective ventilation strategies: Further refinement to prevent ventilator-induced lung injury
- Novel surfactant delivery methods: Aerosolized surfactant and other non-invasive approaches
- Precision medicine: Genetic and biomarker-guided therapies
- Telemedicine: Supporting management of respiratory distress in remote settings
References
American Academy of Pediatrics. (2021). Textbook of Neonatal Resuscitation (8th ed.). American Academy of Pediatrics.
Bancalari, E., & Walsh, M. (2021). Bronchopulmonary dysplasia and surfactant. In Avery’s Diseases of the Newborn (10th ed., pp. 678-710). Elsevier.
Edwards, M. O., Kotecha, S. J., & Kotecha, S. (2019). Respiratory distress of the term newborn infant. Paediatric Respiratory Reviews, 15(1), 29-37.
Hibbard, J. U., Wilkins, I., Sun, L., et al. (2018). Respiratory morbidity in late preterm births. Journal of the American Medical Association, 304(4), 419-425.
Kumar, A., & Bhat, B. V. (2019). Epidemiology of respiratory distress of newborns. Indian Journal of Pediatrics, 83(1), 44-49.
Martin, R. J., Fanaroff, A. A., & Walsh, M. C. (2020). Fanaroff and Martin’s Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant (11th ed.). Elsevier.
Sweet, D. G., Carnielli, V., Greisen, G., et al. (2019). European consensus guidelines on the management of respiratory distress syndrome – 2019 update. Neonatology, 115(4), 432-450.
World Health Organization. (2022). WHO recommendations on interventions to improve preterm birth outcomes. Retrieved from https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/preterm-birth-highlights/en/
