Temper Tantrum in Children
Comprehensive Nursing Notes for Identification and Management
Table of Contents
Introduction to Temper Tantrum in Children
Temper tantrums are brief episodes of extreme, unpleasant, and sometimes aggressive behaviors in response to frustration or anger. They are a normal part of childhood development, particularly in toddlers who are developing autonomy but have limited communication skills to express their needs and emotions effectively.
Temper tantrums in children most commonly occur between the ages of 1 to 3 years but can continue until around age 4. They typically manifest as crying, screaming, falling to the floor, kicking, hitting, breath-holding, or throwing objects. These episodes usually last between 30 seconds and 5 minutes, though they may occasionally persist longer.
For nursing students and healthcare professionals, understanding the nature, causes, and appropriate management strategies for temper tantrums is crucial for providing effective care to children and support to families.
Quick Facts
- Prevalence: 87% of 18-24 month-olds, 91% of 30-36 month-olds
- Frequency: Often daily, with 20% of two-year-olds having at least one tantrum per day
- Average Duration: 3 minutes (most common: 0.5-1 minute)
- Gender Difference: No documented differences by gender
- Risk Factors: Fatigue, hunger, illness, frustration

Figure 1: The Arc of a Tantrum showing stages from trigger to recovery
Identification and Diagnosis of Temper Tantrum in Children
Clinical Manifestations
Temper tantrums can present with a variety of behaviors that may include:
Physical Behaviors
- Crying and screaming
- Falling to the floor
- Flailing arms and legs
- Hitting, biting, or kicking
- Holding breath
- Throwing objects
- Going limp
- Head banging (in severe cases)
Emotional Expressions
- Frustration and anger
- Irritability
- Distress
- Emotional overwhelm
- Resistance to comfort
- Quick emotional changes
- Inability to be reasoned with
Common Triggers
Understanding what triggers temper tantrums is essential for both prevention and management. Common triggers include:
Physiological
- Fatigue
- Hunger
- Illness
- Discomfort
Emotional
- Frustration
- Overstimulation
- Feeling misunderstood
- Seeking autonomy
Environmental
- Transitions
- Denied requests
- Limits being set
- Change in routine
Assessment and Diagnosis
To properly assess temper tantrums, nurses should gather comprehensive information through:
Clinical History
Ask the following questions to parents/caregivers:
- When do the tantrums occur? (time of day)
- What circumstances precede the tantrum?
- What specific behaviors occur during episodes?
- How long do tantrums typically last?
- What is the caregiver’s reaction to tantrums?
- How does the caregiver handle the tantrum?
- What is the child’s mood between tantrum episodes?
- Have there been any recent changes at home?
- Has anything scary or upsetting happened recently?
Physical Examination
Physical examination is often normal in children with typical tantrums. Consider:
- Comprehensive health assessment
- Developmental assessment
- Vision and hearing screening
- Signs of anemia if breath-holding occurs
- Language development evaluation
- Assessment for signs of sleep disorders
Red Flags: When to Refer
While most temper tantrums are developmentally normal, the following signs may warrant referral to a specialist:
- Tantrums that last more than 15 minutes
- Tantrums occurring more than 5 times per day
- Extreme aggression during tantrums
- Self-injurious behavior
- Persistent tantrums in children over 5 years of age
- Inability to calm down without assistance
- Physical injury to self or others
- Property destruction
- Negative mood or behavior between tantrums
- Associated sleep disorders or enuresis
Differentiating Normal vs. Pathological Tantrums
| Feature | Normal Tantrums | Potential Pathological Tantrums |
|---|---|---|
| Duration | Usually 0.5-5 minutes | Often >15 minutes |
| Frequency | Once daily or less | Multiple times daily (>5) |
| Age | Common in 1-4 year-olds | Persistent beyond 5 years |
| Aggression | Mild, non-directed | Severe, directed at others |
| Self-injury | Rare | May be present |
| Trigger | Usually identifiable | May occur without clear trigger |
| Between episodes | Normal behavior and mood | May show other behavioral issues |
| Self-regulation | Eventually self-calms | Unable to self-regulate |
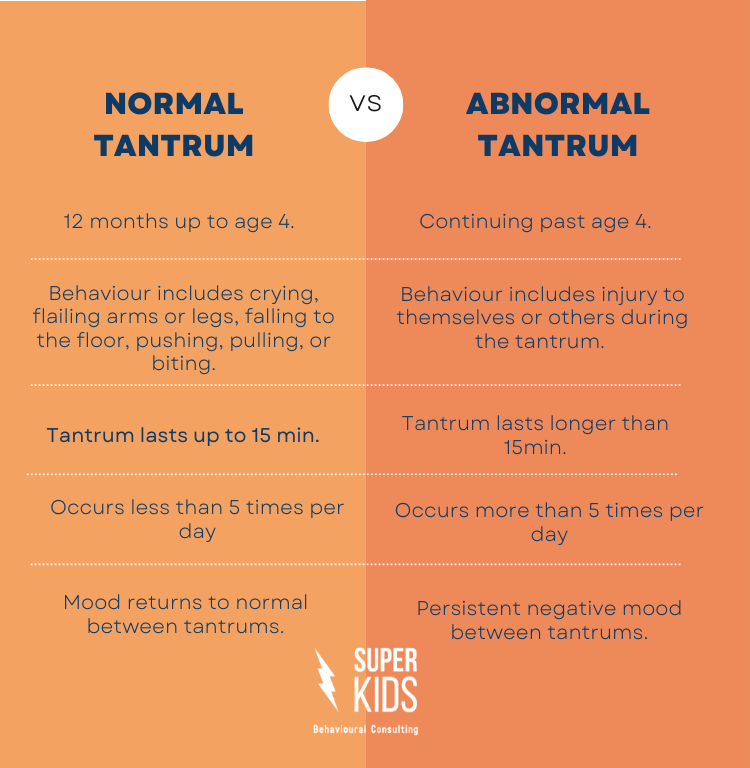
Figure 2: Comparison between normal and abnormal tantrum behaviors
Differential Diagnosis
When assessing a child with frequent or severe tantrums, consider these possible conditions:
- Oppositional Defiant Disorder (ODD) – Persistent pattern of angry/irritable mood and defiant behavior
- Attention Deficit Hyperactivity Disorder (ADHD) – May present with impulsivity and emotional dysregulation
- Autism Spectrum Disorder – May have meltdowns due to sensory overload or communication difficulties
- Disruptive Mood Dysregulation Disorder – Severe, recurrent temper outbursts inconsistent with developmental level
- Language Delays – Frustration due to inability to communicate needs
- Sensory Processing Issues – Meltdowns triggered by sensory overload
Nursing Management of Temper Tantrum in Children in Hospital Settings
When children are hospitalized, they may experience increased stress, fear, and frustration, which can trigger more frequent or intense temper tantrums. Nursing management in the hospital setting requires special consideration of the child’s emotional state while balancing medical needs.
Nursing Assessment
A comprehensive nursing assessment should include:
Initial Assessment
- Baseline behavior and temperament
- Previous tantrum history and patterns
- Parent/caregiver management strategies
- Current stressors (pain, procedures, unfamiliar environment)
- Sleep patterns and disruptions
- Nutritional status and meal schedule
Ongoing Monitoring
- Tantrum triggers within hospital environment
- Effectiveness of interventions
- Duration and intensity of tantrums
- Impact on medical care and treatment
- Parent/caregiver stress levels
- Response to comfort measures
Nursing Diagnosis
| Nursing Diagnosis | Related Factors | Defining Characteristics |
|---|---|---|
| Ineffective Coping |
|
|
| Fear |
|
|
| Interrupted Family Processes |
|
|
| Sleep Pattern Disturbance |
|
|
| Risk for Injury |
|
|
Nursing Interventions
Prevention Strategies
- Maintain routines: Keep meal times, nap times, and bedtime routines as consistent as possible within hospital constraints
- Preparation: Prepare child for procedures using age-appropriate explanations
- Environment: Create a child-friendly environment with familiar items from home
- Choices: Offer appropriate choices when possible (e.g., “Would you like to take your medicine with apple juice or water?”)
- Distraction: Use therapeutic play, games, or child life specialist services
- Rest periods: Ensure adequate rest between procedures and activities
- Pain management: Assess for pain regularly and provide appropriate interventions
Management During Tantrums
- Safety first: Remove dangerous objects and protect medical equipment
- Remain calm: Use a calm, neutral tone of voice
- Minimize attention: Provide minimal attention to tantrum behavior
- Simple language: Use brief, simple statements
- Physical comfort: Offer comfort without reinforcing tantrum behavior
- Consistency: Follow through with established boundaries
- Documentation: Document tantrum patterns, triggers, and effective interventions
R.I.D.D. Approach for Hospital Tantrums
The R.I.D.D. approach is particularly useful in hospital settings:
- Remain calm: Maintain a calm demeanor regardless of the tantrum intensity
- Ignore the tantrum behavior (when safe to do so)
- Distract the child with an alternative activity when possible
- Do say “yes” to addressing physical and safety needs, but don’t give in to unreasonable demands
Parent/Caregiver Education
Nurses should provide education to parents/caregivers on:
- Normal developmental aspects of tantrums
- How hospitalization may affect tantrum frequency and intensity
- Consistent management strategies between hospital staff and family
- How to identify and avoid tantrum triggers in the hospital environment
- Self-care strategies for parents to manage their own stress
- When to seek assistance from nursing staff during a tantrum
Interprofessional Collaboration
Effective management of temper tantrums in the hospital setting often requires collaboration with:
Child Life Specialists
Can provide specialized interventions to help children cope with hospitalization through therapeutic play and preparation
Pediatric Psychologists
May assist with behavioral interventions for more severe or persistent tantrums
Social Workers
Can support families with resources and coping strategies during hospitalization
Documentation
Proper documentation of temper tantrums in the hospital setting should include:
- Time, duration, and intensity of tantrum
- Identified triggers
- Interventions implemented and their effectiveness
- Parent/caregiver involvement and response
- Safety measures taken
- Impact on medical treatment or procedures
- Follow-up plan
Nursing Management of Temper Tantrum in Children at Home
Home is where most tantrums occur, and nurses play a vital role in educating and supporting parents to manage these behaviors effectively. A comprehensive approach addresses prevention, management during tantrums, and promoting healthy emotional development.
Assessment in Home Setting
When conducting home visits or providing guidance for home management, assess:
Home Environment
- Home routines and structure
- Safety hazards during tantrums
- Family dynamics and responses to tantrums
- Consistency of parental approaches
- Environmental triggers in the home
Family Factors
- Parental stress and coping skills
- Sibling interactions
- Cultural beliefs and practices regarding behavior
- Support systems available to the family
- Parental knowledge of child development
Prevention Strategies for Home
Teaching families the C.A.L.M. mnemonic can help prevent frequent tantrums:
C – Communicate Well
- Model good communication skills
- Avoid yelling and arguing in front of children
- Help children identify and express feelings
- Use visual aids (feelings charts) for younger children
- Teach older children to verbalize emotions
A – Attend to Needs
- Give positive attention regularly
- Read to child, play games together
- Childproof the home to avoid unnecessary “no’s”
- Offer age-appropriate toys and activities
- Set age-appropriate expectations
L – Listen to Feelings
- Allow children to share feelings without judgment
- Validate emotions even when behavior is unacceptable
- Offer choices to provide sense of control
- Practice active listening techniques
M – Make Routines
- Establish consistent mealtimes and bedtimes
- Have healthy snacks available
- Prepare children for transitions and changes
- Create visual schedules for predictability
- Include regular physical activity in daily routine
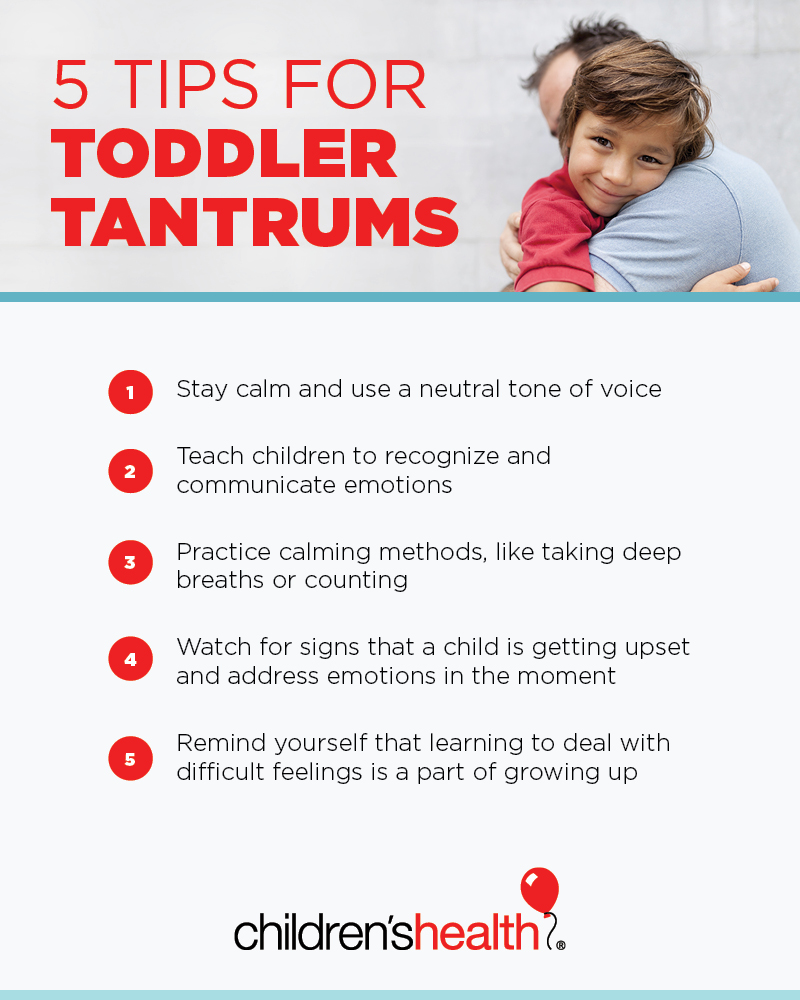
Figure 3: Visual guide for managing toddler tantrums at home
Managing Tantrums at Home
Nurses should educate parents on effective responses during tantrums:
Do’s
- Remain calm and model emotional regulation
- Ensure physical safety
- Use brief, simple language
- Acknowledge feelings (“I see you’re angry”)
- Offer a quiet, safe space to calm down
- Wait until the child is calm before discussing
- Praise recovery and regaining control
Don’ts
- Don’t give in to tantrums (reinforces behavior)
- Avoid lengthy explanations during tantrums
- Don’t use physical punishment
- Don’t shame or ridicule the child
- Avoid threats that won’t be carried out
- Don’t bribe to stop tantrums
- Avoid showing anger or frustration
Teaching Emotional Regulation Skills
A crucial aspect of nursing management is teaching parents how to help children develop emotional regulation skills:
For Toddlers (1-3 years)
- Name emotions for them
- Use picture books about feelings
- Simple calming techniques (deep breaths)
- Redirect to physical activity
- Comfort items (stuffed animal)
For Preschoolers (3-5 years)
- Create a “calm down corner”
- Practice “turtle technique” (slow down, go inside shell, calm down)
- Emotion charts with coping strategies
- Simple problem-solving skills
- Role play appropriate responses
For School-Age (5+ years)
- Teach “stop and think” before acting
- Help identify body cues of emotions
- Practice specific coping strategies
- Self-calming techniques
- Problem-solving conversations
Creating a “Calm Down Kit” for Home
Nurses can help families create a personalized calm-down kit containing:
- Stress ball or sensory items
- Calming images or cards
- Feelings chart
- Favorite small toy or comfort item
- Simple breathing exercise cards
- Emotion-focused picture book
Parent Support and Self-Care
Nurses should emphasize the importance of parental self-care:
- Realistic expectations: Understand that tantrums are normal developmental behavior
- Self-regulation: Parents need to model and practice emotional regulation themselves
- Support systems: Identify friends, family, or parent groups who can provide support
- Self-care: Encourage parents to take breaks and care for their own mental health
- Tag-team approach: When possible, parents can take turns managing difficult behaviors
When to Seek Additional Help
Advise parents to consult healthcare providers if:
- Tantrums are increasing in frequency or intensity despite consistent management
- The child is at risk of harming themselves or others
- Tantrums persist well beyond the typical developmental age (after 4-5 years)
- Parents feel overwhelmed or unable to manage the behaviors
- Tantrums are affecting family functioning or the child’s ability to participate in normal activities
Control Techniques for Temper Tantrum in Children
Controlling temper tantrums involves a multi-faceted approach that combines prevention strategies, in-the-moment management techniques, and long-term behavioral teaching. Nurses can educate families on these evidence-based approaches.
Preventive Control Techniques
Environmental Modifications
- Childproofing: Keep tempting but off-limits objects out of sight
- Safe spaces: Create designated areas where children can express emotions safely
- Reduce stimulation: Minimize overstimulating environments when children are tired or hungry
- Visual schedules: Use pictures to help children understand daily routines
- Transition warnings: Give 5-minute warnings before activity changes
Physiological Needs Management
- Hunger prevention: Offer regular meals and healthy snacks
- Sleep routine: Ensure adequate sleep and consistent nap schedule
- Physical activity: Provide opportunities for gross motor play daily
- Sensory breaks: Regular sensory activities for children with sensory needs
- Medical needs: Address any underlying medical issues (e.g., treat pain)
Direct Control Techniques During Tantrums
| Technique | Description | When to Use |
|---|---|---|
| Planned Ignoring | Deliberately withholding attention during tantrum behaviors while ensuring safety | Most effective for attention-seeking tantrums; not appropriate for dangerous behaviors |
| Distraction | Redirecting child’s attention to a different activity or topic | Works best at early stages of tantrum or with younger children |
| Time-Out | Brief removal from stimulating environment to calm space (1 minute per year of age) | Effective for children 2+ years; best for specific rule violations |
| Physical Comfort | Offering physical reassurance without reinforcing tantrum behavior | For children who are overwhelmed or scared rather than demanding |
| Minimal Verbal Response | Using few, simple words and neutral tone rather than lectures | Throughout tantrum; children cannot process complex language when upset |
| Feelings Validation | Acknowledging emotions while maintaining boundaries | Most effective when child is beginning to calm; “I see you’re angry” |
| Removal from Situation | Taking child to quieter environment until calm | Public tantrums or when behavior disrupts others |

Figure 4: Strategies for managing temper tantrums effectively
Post-Tantrum Teaching Techniques
After a tantrum, when the child is calm, use these strategies to teach better emotional regulation:
Immediate Post-Tantrum
- Provide positive reinforcement for calming down
- Reconnect emotionally with comfort and reassurance
- Keep post-tantrum discussions brief for young children
- Avoid shaming language or lengthy lectures
Later Teaching Moments
- Role-play alternative ways to handle frustration
- Read books about managing emotions
- Create visual reminders of coping strategies
- Practice calming techniques during non-stress times
Positive Reinforcement System
Establishing a positive reinforcement system can help children develop better emotional regulation:
For Toddlers (1-3 years)
- Immediate praise for calm behavior
- Simple reward system (stickers)
- Extra story time for good behavior
- Focus on “catching them being good”
For Preschoolers (3-5 years)
- Sticker charts for using words instead of tantrums
- Special privileges for demonstrating self-control
- Praise specific behaviors (“I like how you asked calmly”)
- Small rewards for meeting behavioral goals
For School-Age (5+ years)
- Token economy system
- Behavior contracts with defined goals
- Self-monitoring charts
- Earning privileges through consistent emotional control
Ineffective Techniques to Avoid
Nurses should advise against these ineffective or potentially harmful approaches:
- Physical punishment: Can increase aggression and model poor emotional regulation
- Shaming or ridiculing: Damages self-esteem and parent-child relationship
- Threatening: Empty threats undermine parental authority
- Bribing: Reinforces tantrum behavior
- Inconsistency: Giving in sometimes but not others confuses children
- Over-reasoning: Long explanations during tantrums are ineffective
Special Considerations
Some situations require modified approaches to tantrum management:
Children with Special Needs
- Adapt techniques based on developmental level, not chronological age
- For autism spectrum disorders, identify sensory triggers
- For communication disorders, use visual supports
- May require more structure and consistency
- Consider consultation with developmental specialists
Public Tantrums
- Have an exit strategy planned in advance
- Prepare small distraction items to carry
- Identify quiet areas in public places
- Ignore judgmental onlookers
- Consider timing outings around naps and meals
Breath-Holding Episodes
Some children may have breath-holding spells during intense tantrums:
- Usually occur in children 6 months to 5 years old
- May cause brief loss of consciousness
- Ensure child’s safety during episode
- Do not reinforce behavior with excessive attention
- Consider screening for iron deficiency anemia
- Reassure parents that episodes typically resolve on their own
Helpful Mnemonics and Tools for Managing Temper Tantrum in Children
Mnemonics and visual tools can help healthcare providers, parents, and children remember strategies for preventing and managing temper tantrums. These can be taught by nurses during patient education sessions.
Mnemonics for Nurses and Parents
R.I.D.D. – Managing Active Tantrums
- Remain calm with neutral tone and expression
- Ignore the tantrum behavior when safe to do so
- Distract the child with another activity
- Do say “yes” to physical needs but not demands
C.A.L.M. – Preventing Tantrums
- Communicate well and model good communication
- Attend to child’s needs with positive attention
- Listen to feelings and validate emotions
- Make routines consistent and predictable
S.T.O.P. – Parent Self-Regulation
- Stop and take a deep breath
- Think about your response
- Observe your child’s needs
- Proceed with a calm approach
P.E.A.C.E. – After Tantrum Approach
- Praise child for calming down
- Emotional reconnection with comfort
- Acknowledge feelings that triggered tantrum
- Coach better ways to express feelings
- Encourage practice of new skills
Child-Friendly Tools
The Turtle Technique
A popular technique to teach children emotional regulation:
- Recognize feeling upset (angry turtle)
- Stop your body (go in turtle shell)
- Take 3 deep breaths (inside shell)
- Think of a better choice (come out calmly)
Particularly effective for preschoolers
Feelings Thermometer
Visual tool showing emotion intensity levels:
- Blue/Green: Calm, happy, okay
- Yellow: Getting upset, frustrated
- Orange: Very upset, angry
- Red: Out of control, tantrum
Each level has corresponding calming strategies
Calming Strategy Cards
Picture cards showing calming techniques:
- Deep breathing exercises
- Counting to 10 slowly
- Squeezing a stress ball
- Asking for a hug
- Drawing feelings
Child selects a strategy when upset
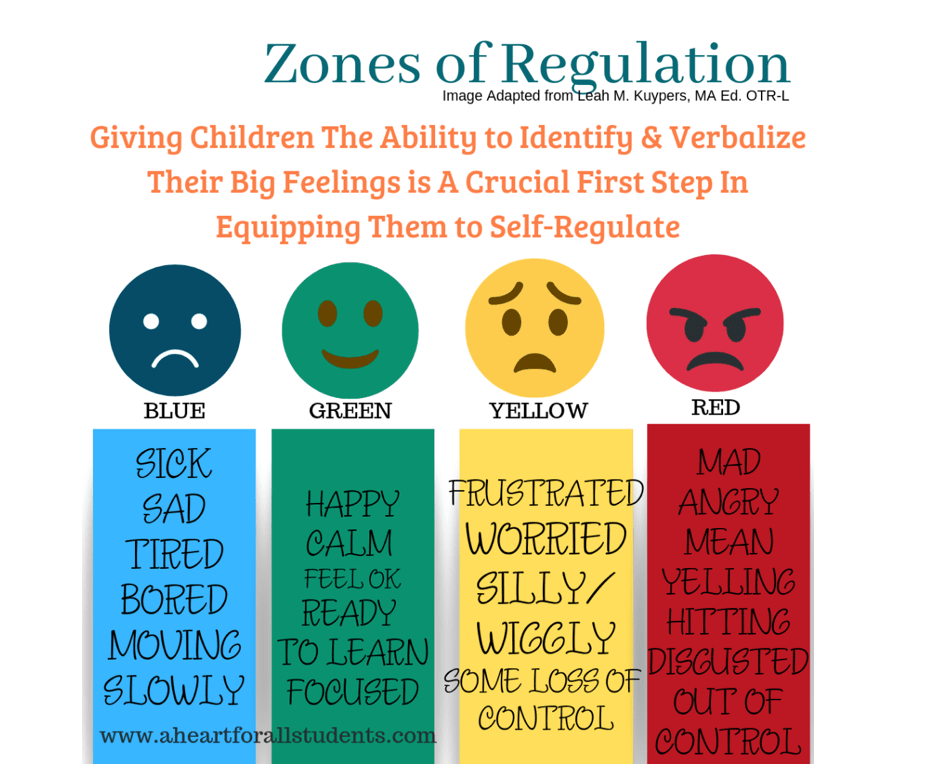
Figure 5: Zones of Regulation for teaching emotional awareness and management
Visual Supports for Home and School
Nurses can help families create and implement these visual supports:
Visual Schedule
A chart showing the daily routine with pictures representing each activity.
Benefits:
- Provides predictability
- Prepares children for transitions
- Reduces anxiety about what comes next
- Can include visual timer for transitions
Calm Down Corner
Designated space with calming tools and visual supports.
Components:
- Comfort items (pillows, stuffed animals)
- Visual calming sequence
- Emotion cards for identification
- Timer for self-regulation practice
- Calming sensory items
Documentation Tools for Nurses
These tools help nurses systematically document tantrum behavior:
ABC Behavior Chart
Documents:
- Antecedent – What happened before
- Behavior – Specific tantrum behaviors
- Consequence – What happened after
Helps identify patterns and triggers
Tantrum Tracking Log
Records:
- Date and time
- Duration of tantrum
- Intensity (scale 1-5)
- Triggering factors
- Interventions used
- Effectiveness of interventions
Teaching Tool: The Tantrum Arc
Educate parents about the typical progression of a tantrum:
- Triggering phase: Child encounters frustration or limitation
- Escalation phase: Emotions intensify, rational thinking decreases
- Peak phase: Most intense emotional expression
- De-escalation phase: Energy depletes, child begins to calm
- Recovery phase: Return to baseline behavior and emotion
Different intervention strategies are appropriate for each phase of the tantrum arc.
Case Studies: Temper Tantrum in Children
The following case studies illustrate nursing approaches to various tantrum scenarios, demonstrating assessment, intervention, and evaluation.
Case Study 1: Hospital Setting
Patient
Tyler, 3-year-old male, hospitalized for pneumonia.
Situation
Tyler has been having increasingly frequent tantrums during his hospital stay, particularly before vital sign checks and medication administration. Tantrums include screaming, kicking, and trying to hide under the bed. Parents report tantrum behavior is much more frequent than at home.
Nursing Assessment
- Sleep disrupted by hospital environment and nursing checks
- Fear and anxiety related to medical procedures
- Loss of normal routine and environment
- Parents increasingly stressed and responding inconsistently
- Pain assessment: 2/10 when calm
Nursing Interventions
- Created visual schedule of daily hospital activities
- Consolidated care when possible to minimize disruptions
- Implemented medical play with child life specialist before procedures
- Taught parents consistent approach using R.I.D.D. technique
- Added comfort items from home to environment
- Incorporated consistent bedtime routine
Outcomes
After two days of implementing interventions, Tyler’s tantrums decreased from 6-7 daily to 2-3, with shorter duration. Parents reported feeling more confident in managing outbursts, and Tyler showed improved cooperation with vital checks when using the visual schedule as preparation.
Case Study 2: Home Setting
Patient
Mia, 2.5-year-old female, seen in pediatric clinic for well-child visit.
Situation
Mother reports Mia has daily tantrums, usually around transitions or when denied something she wants. Tantrums include crying, screaming, and throwing herself on the floor. Parents have been giving in to demands to end tantrums. Mother is pregnant with second child and worried about managing two children.
Nursing Assessment
- Typical development for age
- Normal physical examination
- Tantrums typical in duration (2-3 minutes)
- Parents inconsistent in responses to tantrums
- Tantrum triggers: transitions, denied requests, bedtime
- Recent changes: mother pregnant, moved to new bedroom
Nursing Interventions
- Educated parents on normal development and tantrum patterns
- Taught C.A.L.M. prevention strategies
- Recommended consistent bedtime routine
- Advised against giving in to demands during tantrums
- Created visual routine chart for transitions
- Set up rewards for positive behavior (sticker chart)
- Scheduled follow-up phone call in 2 weeks
Outcomes
At two-week follow-up, mother reported tantrums reduced to 1-2 per day. Parents were consistently implementing strategies and using visual supports. Mia had responded well to the sticker chart and was learning to use words instead of tantrums. Parents requested continued support in preparation for new sibling.
Case Study 3: Atypical Tantrums
Patient
Aiden, 5-year-old male, referred to pediatric nurse practitioner by kindergarten teacher for concerning tantrum behaviors.
Situation
Aiden has multiple tantrums daily at school and home, lasting 15-20 minutes. Tantrums include physical aggression toward others, throwing objects, and self-injurious behaviors (head banging). School reports difficulty reintegrating him into activities after tantrums.
Nursing Assessment
- Duration, frequency, and intensity of tantrums atypical for age
- History of speech delay and sensory sensitivities
- Difficulty with transitions and changes in routine
- Limited ability to identify and express emotions
- Parents exhausted and feeling helpless
- Red flags: age, duration, self-injury, aggression
Nursing Interventions
- Immediate safety planning for self-injurious behaviors
- Referral to developmental pediatrician
- Taught parents modified calming techniques
- Recommended speech and language evaluation
- Connected family with parent support group
- Communicated with school about consistent approaches
- Implemented visual supports and social stories
Outcomes
Developmental evaluation revealed autism spectrum disorder with sensory processing differences. With appropriate diagnosis, specialized interventions, and consistent approaches between home and school, Aiden’s tantrum frequency and intensity gradually decreased. Parents reported feeling more equipped to understand and support their child’s needs.
Case Study Analysis
These case studies demonstrate key principles in nursing management of temper tantrums:
- Individualized assessment: Each child’s tantrum behavior must be evaluated in context
- Differentiation: Distinguishing typical from atypical tantrum patterns
- Environmental factors: Considering how setting influences behavior
- Parental support: Teaching consistent, evidence-based strategies
- Appropriate referral: Recognizing when specialized evaluation is needed
- Collaborative approach: Working with families, schools, and specialists
Conclusion
Temper tantrums in children are a normal part of development, particularly between the ages of 1 and 3 years. Understanding the triggers, progression, and appropriate management strategies is essential for nurses providing care to children and education to families.
As healthcare professionals, nurses play a vital role in helping families navigate this challenging aspect of child development. Through proper assessment, evidence-based interventions, and family education, nurses can help transform tantrums from frustrating experiences into opportunities for teaching emotional regulation skills that will benefit children throughout their lives.
The management of temper tantrums in children requires a multifaceted approach that includes prevention strategies, consistent responses during tantrums, and teaching skills for emotional expression. By empowering parents with effective tools and techniques, nurses contribute significantly to healthy child development and positive family functioning.
Key Takeaways
- Temper tantrums are a normal developmental behavior in young children
- Prevention is the most effective management strategy
- Consistent, calm responses during tantrums are essential
- Teaching emotional regulation skills supports long-term development
- Atypical tantrums require specialized evaluation and intervention
- Family education and support is a core nursing responsibility
