Comprehensive Nursing Notes: Understanding Dementia
A complete guide for nursing students on prevalence, classification, assessment, and management of dementia
Table of Contents
Introduction to Dementia
Dementia is a progressive neurological disorder characterized by a decline in cognitive function beyond what is considered a normal part of aging. It affects memory, thinking, orientation, comprehension, calculation, learning capacity, language, and judgment. Dementia is not a specific disease but rather an umbrella term that describes a syndrome associated with a wide range of specific medical conditions.
The impact of dementia extends beyond the affected individual to families, caregivers, and healthcare systems. As global population aging accelerates, dementia has become a significant public health concern and a priority for healthcare professionals, especially nurses who play a crucial role in the comprehensive care of individuals with dementia.
Key Concept
While memory loss is often the most recognized symptom, dementia encompasses a much broader range of cognitive and behavioral changes that significantly impact daily functioning and independence.
Prevalence and Incidence of Dementia
Dementia prevalence has been steadily increasing worldwide, largely due to population aging and increased awareness and diagnosis. Understanding the epidemiological trends of dementia is essential for healthcare planning and resource allocation.
Global and National Statistics (2024)
| Region/Population | Prevalence | Projected Growth |
|---|---|---|
| Global | 57 million people (2021) | 152.8 million by 2050 |
| United States | 6.9 million Americans (65+) | 13.8 million by 2060 |
| Low and middle-income countries | Over 60% of all cases | Fastest growing region |
| Annual new cases | 10 million worldwide | One new case every 3.2 seconds |
Age-Specific Prevalence
- Ages 65-74: Approximately 3% of population
- Ages 75-84: Approximately 17% of population
- Ages 85+: Approximately 32% of population
Note: The risk of developing dementia doubles approximately every 5 years after age 65.
Recent studies have shown possible decreases in age-specific incidence rates in some high-income countries, potentially linked to improved education, better cardiovascular health management, and lifestyle factors. However, the absolute number of cases continues to rise due to the increasing number of older adults in the population.
Classification of Dementia
Dementia can be classified based on etiology, pathophysiology, clinical presentation, or progression pattern. Understanding the various types of dementia is fundamental to accurate diagnosis and appropriate management strategies.
Primary Types of Dementia
| Type | Prevalence | Key Characteristics | Pathology |
|---|---|---|---|
| Alzheimer’s Disease | 60-70% of cases | Gradual onset, progressive memory loss, language difficulties, executive dysfunction | Amyloid plaques, neurofibrillary tangles, neuronal loss |
| Vascular Dementia | 15-20% of cases | Step-wise progression, focal neurological deficits, history of cerebrovascular disease | Multiple infarcts, white matter lesions, cerebrovascular disease |
| Lewy Body Dementia | 5-10% of cases | Visual hallucinations, fluctuating cognition, parkinsonism, REM sleep behavior disorder | Lewy bodies (alpha-synuclein protein deposits) |
| Frontotemporal Dementia | 5-10% of cases | Behavioral changes, language deficits, earlier onset (45-65 years) | Frontal and temporal lobe atrophy, tau or TDP-43 protein aggregates |
| Mixed Dementia | Up to 45% of cases | Features of multiple dementia types, commonly AD and vascular | Multiple pathologies coexisting |
Other Significant Forms of Dementia
Potentially Reversible Causes
- Medication-induced cognitive impairment
- Metabolic disorders (thyroid dysfunction, B12 deficiency)
- Normal pressure hydrocephalus
- Chronic subdural hematoma
- Brain tumors
- Infectious causes (syphilis, HIV)
Rare Forms of Dementia
- Huntington’s disease
- Creutzfeldt-Jakob disease
- Progressive supranuclear palsy
- Corticobasal degeneration
- Posterior cortical atrophy
- Limbic-predominant age-related TDP-43 encephalopathy (LATE)
Classification Based on Progression
Mild Dementia
- Recent memory loss
- Difficulty with time relationships
- Problem-solving challenges
- Still independent with daily activities
Moderate Dementia
- Increased memory deficits
- Confusion/disorientation
- Assistance needed for ADLs
- Behavioral/personality changes
Severe Dementia
- Inability to recognize family
- Complete dependence for ADLs
- Speech limitations
- Physical decline (swallowing, mobility)
Etiology and Pathophysiology of Dementia
The development of dementia involves complex interactions between genetic factors, environmental exposures, and aging processes. Understanding the pathophysiological mechanisms underlying dementia is crucial for developing targeted therapies and preventive strategies.
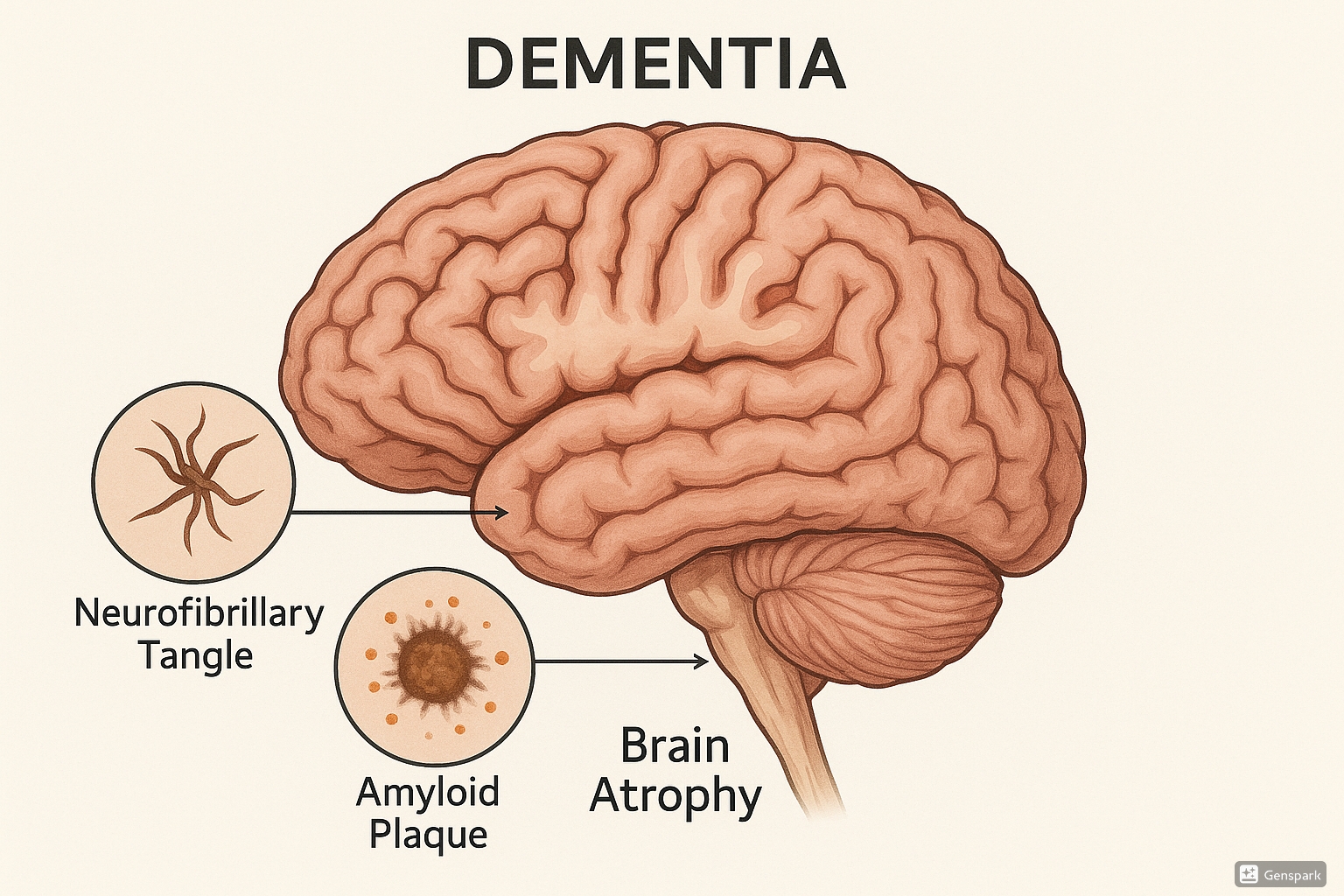
Brain affected by dementia showing neurofibrillary tangles, amyloid plaques, and brain atrophy
General Pathophysiological Mechanisms in Dementia
1. Protein Misfolding and Aggregation
Most neurodegenerative dementias involve abnormal accumulation of misfolded proteins:
- Beta-amyloid: Forms extracellular plaques in Alzheimer’s disease
- Tau protein: Forms intracellular neurofibrillary tangles in AD and other tauopathies
- Alpha-synuclein: Forms Lewy bodies in Lewy body dementia and Parkinson’s disease
- TDP-43: Aggregates in frontotemporal dementia and amyotrophic lateral sclerosis
2. Neuroinflammation
Chronic inflammation contributes to neuronal damage through:
- Microglial activation
- Release of pro-inflammatory cytokines
- Complement activation
- Blood-brain barrier disruption
3. Neurotransmitter Deficits
Alterations in neurotransmitter systems affect neural signaling:
- Acetylcholine: Significant reduction in Alzheimer’s disease
- Dopamine: Depleted in Lewy body dementia and Parkinson’s disease dementia
- Glutamate: Excitotoxicity contributes to neuronal death
- Serotonin: Alterations affect mood and behavior in various dementias
4. Vascular Mechanisms
Cerebrovascular pathology contributes to dementia through:
- Large vessel infarcts
- Small vessel disease and microinfarcts
- Cerebral amyloid angiopathy
- Chronic hypoperfusion
- Blood-brain barrier dysfunction
5. Mitochondrial Dysfunction and Oxidative Stress
Cellular energy production impairment leads to:
- Increased reactive oxygen species
- Oxidative damage to cellular components
- Compromised cellular bioenergetics
- Enhanced susceptibility to apoptosis
Mnemonic: “DEMENTIA” for Assessing Causes
D – Drugs and alcohol
E – Eyes and ears (sensory deficits)
M – Metabolic and endocrine disorders
E – Emotional disorders (depression)
N – Neurological disorders
T – Tumors and trauma
I – Infections
A – Atherosclerosis/vascular disease
Risk Factors for Dementia
Non-Modifiable Risk Factors
- Age: Strongest risk factor, risk doubles every 5 years after age 65
- Genetics: ApoE ε4 allele (Alzheimer’s), MAPT mutations (FTD), etc.
- Family history: First-degree relatives with dementia
- Down syndrome: Early onset Alzheimer’s pathology
Modifiable Risk Factors
- Cardiovascular: Hypertension, diabetes, obesity, smoking
- Lifestyle: Physical inactivity, poor diet, alcohol excess
- Education: Lower cognitive reserve with less education
- Social isolation: Reduced cognitive stimulation
- Hearing loss: Associated with increased dementia risk
- Traumatic brain injury: Repeated concussions
Clinical Features of Dementia
The clinical presentation of dementia encompasses a wide range of cognitive, behavioral, and psychological symptoms that develop over time. While specific features may vary depending on the type of dementia, there are common patterns of symptom progression that assist in recognition and diagnosis.
Core Cognitive Symptoms
| Cognitive Domain | Clinical Manifestations | Functional Impact |
|---|---|---|
| Memory |
– Impaired ability to learn new information – Difficulty recalling recent events – Repetitive questioning – Remote memories often preserved longer |
– Missed appointments – Misplacing items – Forgetting medication – Difficulty following new routines |
| Executive Function |
– Impaired planning and organization – Difficulty with abstract thinking – Poor judgment and decision-making – Reduced problem-solving ability |
– Financial mismanagement – Inability to plan meals – Poor medication management – Safety concerns (e.g., leaving stove on) |
| Language |
– Word-finding difficulties – Decreased verbal fluency – Comprehension problems – Eventually progressing to aphasia |
– Communication barriers – Social withdrawal – Difficulty expressing needs – Misinterpreting instructions |
| Visuospatial Skills |
– Difficulty with navigation – Problems with spatial relationships – Impaired object recognition – Constructional apraxia |
– Getting lost in familiar places – Driving difficulties – Inability to use tools properly – Problems dressing (e.g., orientation of clothes) |
| Attention |
– Reduced concentration – Distractibility – Difficulty with divided attention – Slowed information processing |
– Inability to follow conversations – Difficulty completing tasks – Problems managing multiple stimuli – Increased vulnerability to delirium |
Behavioral and Psychological Symptoms of Dementia (BPSD)
Mood Disturbances
- Depression: Common in early stages, may present as apathy
- Anxiety: Often related to awareness of cognitive decline
- Emotional lability: Rapid mood swings without clear triggers
- Apathy: Reduced motivation and initiative
Psychotic Symptoms
- Delusions: Often persecutory (theft, infidelity, abandonment)
- Hallucinations: Visual most common in LBD, auditory can occur
- Misidentification: Not recognizing familiar people/places
- Capgras syndrome: Believing loved ones are imposters
Behavioral Disturbances
- Agitation: Restlessness, pacing, repetitive actions
- Aggression: Verbal or physical, often during care activities
- Wandering: Purposeless movement, exit-seeking behavior
- Disinhibition: Inappropriate social behavior, loss of filters
- Sundowning: Increased confusion and agitation in late afternoon/evening
Neurovegetative Symptoms
- Sleep disturbances: Fragmented sleep, day-night reversal
- Appetite changes: Usually decreased, sometimes altered food preferences
- Altered sexual behavior: Hypersexuality or diminished interest
- Incontinence: Develops as disease progresses
Mnemonic: “JAMCO” for Assessing Cognitive Changes in Dementia
J
Judgment
A
Affect
M
Memory
C
Cognition
O
Orientation
Clinical Features Specific to Different Dementia Types
| Dementia Type | Early/Prominent Features | Distinguishing Characteristics |
|---|---|---|
| Alzheimer’s Disease |
– Episodic memory impairment – Word-finding difficulties – Spatial disorientation |
– Insidious onset, gradual progression – Early preservation of social skills – Late-stage language, mobility impairment |
| Vascular Dementia |
– Executive dysfunction – Focal neurological deficits – Psychomotor slowing |
– Stepwise deterioration – History of stroke or cardiovascular disease – Early gait disturbances and falls |
| Lewy Body Dementia |
– Visual hallucinations – Fluctuating cognition – REM sleep behavior disorder |
– Parkinsonism (rigidity, bradykinesia) – Severe neuroleptic sensitivity – Early visuospatial impairment |
| Frontotemporal Dementia |
– Personality and behavior changes – Loss of empathy/social awareness – Language variants (semantic, progressive non-fluent) |
– Earlier age of onset (45-65 years) – Relative preservation of memory and visuospatial skills – Disinhibition, compulsive behaviors |
Diagnosis and Differential Diagnosis
Diagnosing dementia requires a systematic approach to identify cognitive impairment, determine its severity, establish its impact on daily function, and identify the underlying cause. Early and accurate diagnosis is essential for appropriate management and planning.
Diagnostic Approach to Dementia
Step 1: Comprehensive History
- Cognitive symptoms – onset, progression
- Functional assessment
- Behavioral/psychological symptoms
- Medical history, including vascular risk factors
- Medication review
- Family history
- Social/occupational history
- Collateral history from reliable informant
Step 2: Clinical Examination
- General physical examination
- Neurological examination
- Cognitive assessment using standardized tools
- Mental status examination
- Screening for depression
- Functional assessment
Step 3: Investigations
- Laboratory tests to exclude reversible causes
- Neuroimaging (structural and sometimes functional)
- Advanced biomarker testing (when indicated)
- Electroencephalography (when indicated)
- Neuropsychological assessment
Standardized Cognitive Assessment Tools
| Assessment Tool | Key Features | Score Interpretation | Time to Administer |
|---|---|---|---|
| Mini-Mental State Examination (MMSE) | 30-point questionnaire measuring orientation, registration, attention, calculation, recall, language, and visuospatial ability | ≥24: Normal 19-23: Mild 10-18: Moderate ≤9: Severe |
5-10 minutes |
| Montreal Cognitive Assessment (MoCA) | More sensitive for mild cognitive impairment; assesses executive function and attention in more detail | ≥26: Normal 18-25: Mild 10-17: Moderate ≤9: Severe |
10-15 minutes |
| Clock Drawing Test | Tests visuospatial, executive function, and numerical knowledge; patient draws clock face and sets time | Various scoring systems; assesses planning and execution | 2-3 minutes |
| Mini-Cog | Combines 3-word recall with clock drawing test; useful in primary care | 0-2: Positive screen for dementia 3-5: Negative screen |
3-5 minutes |
| Addenbrooke’s Cognitive Examination (ACE-III) | Comprehensive assessment with 5 cognitive domains; better at differentiating dementia subtypes | ≥88: Normal 82-87: Mild ≤82: Significant impairment |
15-20 minutes |
Laboratory and Neuroimaging Investigations
Standard Laboratory Tests
- Complete blood count
- Blood glucose, electrolytes, renal function
- Liver function tests
- Thyroid function tests (TSH, Free T4)
- Vitamin B12 and folate levels
- Syphilis serology (RPR/VDRL)
- HIV testing (in high-risk populations)
- Inflammatory markers (ESR, CRP)
Neuroimaging
- Structural Imaging:
- CT scan: To exclude mass lesions, hemorrhage, hydrocephalus
- MRI: More sensitive for white matter changes, atrophy patterns
- Functional Imaging (when diagnosis is uncertain):
- FDG-PET: Shows patterns of hypometabolism
- SPECT: Evaluates cerebral perfusion
- Amyloid PET: Detects amyloid plaques in vivo
Differential Diagnosis of Dementia
| Condition | Distinguishing Features | Diagnostic Considerations |
|---|---|---|
| Delirium |
– Acute onset – Fluctuating course – Altered level of consciousness – Inattention is prominent – Often reversible |
– Search for underlying cause (infection, medications, metabolic) – Can coexist with dementia – Confusion Assessment Method (CAM) for diagnosis |
| Depression |
– “Pseudodementia” – Poor effort in cognitive testing – “Don’t know” answers common – Often aware of deficits – Symptoms may be worse in morning |
– Geriatric Depression Scale – History of mood disorders – Response to antidepressant treatment – Can coexist with dementia |
| Mild Cognitive Impairment |
– Cognitive decline greater than expected for age – Preserved activities of daily living – Does not meet criteria for dementia |
– Annual follow-up to monitor progression – Biomarkers may predict progression to AD – 10-15% per year convert to dementia |
| Normal Aging |
– Slower cognitive processing – Mild word-finding difficulties – No functional impairment – Stable over time |
– Careful history taking – Normalized cognitive test scores for age/education – Lack of progression on follow-up |
| Substance-Induced Cognitive Impairment |
– Temporal relationship with substance use – May improve with abstinence – Multidomain cognitive impairment |
– Toxicology screening – Medication review – History of substance use |
Important Clinical Consideration
Always evaluate for potentially reversible causes of cognitive impairment before establishing a diagnosis of irreversible dementia. Up to 10-15% of cases may have contributing factors that are partially or fully reversible, including medication effects, metabolic disorders, infections, normal pressure hydrocephalus, and depression.
Nursing Assessment
Comprehensive nursing assessment is fundamental to developing individualized care plans for patients with dementia. Nurses play a crucial role in identifying cognitive, functional, behavioral, and physical changes, as well as evaluating the patient’s environment and caregiver support systems.
Components of a Comprehensive Nursing Assessment for Dementia
History Taking
- Cognitive Symptoms:
- Memory problems (onset, progression)
- Language difficulties
- Problems with reasoning or judgment
- Spatial/navigational difficulties
- Functional Status:
- Basic Activities of Daily Living (BADLs)
- Instrumental Activities of Daily Living (IADLs)
- Recent changes in independence
- Behavioral and Psychological Symptoms:
- Agitation, aggression, wandering
- Mood changes, anxiety, depression
- Sleep disturbances
- Hallucinations or delusions
- Medication Review:
- Current medications (including OTC)
- Medication adherence
- Potential adverse effects
Physical and Neurological Assessment
- Vital Signs: Including orthostatic blood pressure
- Neurological Assessment:
- Motor function and coordination
- Gait and balance evaluation
- Cranial nerve assessment
- Reflexes and sensory function
- Nutritional Status:
- Weight changes
- Eating difficulties
- Swallowing assessment
- Hydration status
- Physical Function:
- Mobility assessment
- Fall risk evaluation
- Physical limitations
- Continence Assessment:
- Urinary continence
- Bowel function
Standardized Assessment Tools for Nursing Practice
| Assessment Domain | Assessment Tools | Application in Nursing Practice |
|---|---|---|
| Cognitive Function |
– Mini-Mental State Examination (MMSE) – Montreal Cognitive Assessment (MoCA) – Mini-Cog – Six-Item Screener |
– Baseline cognitive assessment – Monitoring disease progression – Evaluating response to interventions – Care planning based on cognitive abilities |
| Functional Status |
– Barthel Index (for BADLs) – Lawton-Brody IADL Scale – Katz Index of Independence in ADL – Functional Assessment Staging (FAST) |
– Determining level of assistance needed – Identifying areas for targeted interventions – Monitoring functional decline – Discharge planning |
| Behavioral Symptoms |
– Neuropsychiatric Inventory (NPI) – Cohen-Mansfield Agitation Inventory – BEHAVE-AD – ABC (Antecedent-Behavior-Consequence) Charting |
– Identifying behavioral triggers – Evaluating effectiveness of interventions – Documentation of behavioral patterns – Developing person-centered behavioral care plans |
| Depression/Mood |
– Cornell Scale for Depression in Dementia – Geriatric Depression Scale – Patient Health Questionnaire (PHQ-9) |
– Distinguishing dementia from depression – Identifying comorbid depression – Monitoring response to interventions – Referral for psychiatric consultation when needed |
| Pain Assessment |
– Pain Assessment in Advanced Dementia (PAINAD) – Abbey Pain Scale – DOLOPLUS-2 |
– Identifying pain in non-verbal patients – Monitoring effectiveness of pain management – Addressing behavioral symptoms related to undetected pain |
| Caregiver Assessment |
– Zarit Burden Interview – Caregiver Strain Index – Family Caregiver Alliance Assessment |
– Identifying caregiver burnout and stress – Assessing caregiver education needs – Referral for caregiver support services – Discharge planning considerations |
Mnemonic: “NURSES” for Dementia Assessment
N
Neurological Status
- Cognitive function
- Motor abilities
- Coordination
U
Understanding & Communication
- Comprehension
- Expression
- Language abilities
R
Risk Assessment
- Fall risk
- Wandering
- Self-harm
S
Self-Care Abilities
- ADLs
- IADLs
- Independence level
E
Emotional & Behavioral Status
- Mood
- Agitation
- Psychotic symptoms
S
Social Support
- Caregiver availability
- Home environment
- Community resources
Special Considerations in Nursing Assessment
Communication Strategies During Assessment
- Use simple, direct language
- Ask one question at a time
- Allow sufficient time for responses
- Maintain eye contact
- Minimize background distractions
- Use visual cues when needed
- Observe non-verbal communication
- Validate the patient’s feelings
Environmental Assessment
- Home safety evaluation
- Fall hazards identification
- Wandering risk assessment
- Kitchen safety
- Bathroom accessibility and safety
- Medication management systems
- Orientation cues in the environment
- Assistive device needs
Documentation Tips for Nursing Assessment
- Document specific behaviors rather than general statements (e.g., “Paced the hallway for 30 minutes asking to go home” rather than “Patient is agitated”)
- Note the time of day when behaviors occur to identify patterns
- Record changes from baseline functioning
- Document effectiveness of interventions
- Include both strengths and deficits
- Incorporate information from multiple sources (patient, family, staff observations)
Treatment Modalities for Dementia
While there is currently no cure for most forms of dementia, treatment approaches focus on symptom management, slowing disease progression when possible, and maintaining quality of life. A multidisciplinary approach is essential, combining pharmacological and non-pharmacological interventions tailored to individual needs.
Pharmacological Interventions
| Medication Class | Specific Agents | Mechanism of Action | Clinical Applications | Key Nursing Considerations |
|---|---|---|---|---|
| Cholinesterase Inhibitors |
– Donepezil – Rivastigmine – Galantamine |
Inhibit acetylcholinesterase, increasing acetylcholine availability in synaptic clefts |
– Mild to moderate AD – Lewy body dementia – Parkinson’s disease dementia – Some benefit in vascular dementia |
– Monitor for GI side effects (nausea, vomiting, diarrhea) – Bradycardia risk; assess pulse regularly – Take with food to reduce GI effects – Gradual titration improves tolerability |
| NMDA Receptor Antagonist | – Memantine | Blocks glutamate excitotoxicity by regulating NMDA receptor activity |
– Moderate to severe AD – Can be combined with cholinesterase inhibitors – Some benefit in mixed dementia |
– Better tolerated than cholinesterase inhibitors – Monitor for dizziness, confusion, headache – Dose adjustment needed in renal impairment – May reduce agitation in some patients |
| Antipsychotics |
– Risperidone – Quetiapine – Olanzapine – Aripiprazole |
Block dopamine receptors (D2) and various serotonin receptors |
– Severe agitation/aggression – Psychosis/hallucinations – As last resort when non-pharmacological approaches fail |
– FDA black box warning for increased mortality – Use lowest effective dose for shortest time – Monitor for extrapyramidal symptoms – Increased stroke risk – QT prolongation risk – Contraindicated in Lewy body dementia |
| Antidepressants |
– SSRIs (sertraline, citalopram) – SNRIs (venlafaxine, duloxetine) – Trazodone – Mirtazapine |
Increase serotonin and/or norepinephrine in synaptic cleft |
– Depression in dementia – Anxiety – Agitation (trazodone) – Sleep disturbances (mirtazapine, trazodone) |
– Monitor for hyponatremia with SSRIs – Start low, go slow dosing approach – Assess for serotonin syndrome with multiple agents – Weight gain with mirtazapine |
| Anticonvulsants |
– Valproate/Divalproex – Carbamazepine – Lamotrigine |
Multiple mechanisms including GABA enhancement, sodium channel modulation |
– Agitation/aggression – Impulsivity – When antipsychotics contraindicated |
– Monitor liver function and CBC – Drug interactions common – Therapeutic drug monitoring needed – Risk of sedation, ataxia |
Important Medication Considerations
The use of psychotropic medications in dementia must be carefully considered, with benefits weighed against potential risks. Current guidelines emphasize:
- Non-pharmacological approaches should be first-line for behavioral symptoms
- When medications are necessary, use lowest effective dose for shortest duration
- Regular reassessment of medication benefit and consideration of gradual discontinuation
- Careful monitoring for adverse effects, particularly with antipsychotics
Non-Pharmacological Interventions
Cognitive Interventions
- Cognitive Stimulation Therapy: Structured group activities to engage thinking, memory, and social interaction
- Cognitive Rehabilitation: Individualized strategies to manage specific deficits
- Reality Orientation: Providing cues about time, place, and person
- Reminiscence Therapy: Using past experiences to stimulate memory and improve mood
- Computer-Based Cognitive Training: Specialized programs targeting specific cognitive domains
Sensory Interventions
- Music Therapy: Personalized music to enhance mood, reduce agitation
- Aromatherapy: Essential oils to promote relaxation and reduce stress
- Multisensory Stimulation (Snoezelen): Controlled sensory environment
- Light Therapy: Bright light exposure to regulate circadian rhythms
- Animal-Assisted Therapy: Interaction with trained animals to improve mood and engagement
- Art Therapy: Creative expression through various artistic media
Behavioral Approaches
- Person-Centered Care: Tailoring care to individual preferences, history, and needs
- ABC Analysis: Identifying Antecedents, Behaviors, and Consequences
- Validation Therapy: Accepting the person’s emotional reality
- Structured Routine: Consistent daily schedule to reduce confusion
- Redirection: Gently shifting focus from problematic situations
- Environment Modification: Adapting surroundings to reduce stress and enhance function
Physical Health Interventions
Exercise and Physical Activity
- Benefits in Dementia:
- Improved cognition
- Enhanced mood and reduced depression
- Better sleep quality
- Reduced fall risk
- Maintained functional abilities
- Reduced behavioral symptoms
- Recommended Activities:
- Walking programs
- Chair-based exercises
- Tai Chi and gentle yoga
- Dance therapy
- Resistance training (with supervision)
Nutrition and Dietary Approaches
- Nutritional Support:
- Regular nutritional assessment
- High-calorie, nutrient-dense foods for weight loss
- Modified food textures for swallowing difficulties
- Finger foods for independence
- Colorful plates and contrasting colors
- Dietary Considerations:
- Mediterranean diet associated with reduced risk
- MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay)
- Omega-3 fatty acids
- Adequate hydration
Evolving Treatment Approaches
Emerging Pharmacological Approaches
- Disease-Modifying Therapies:
- Aducanumab (Aduhelm) – Anti-amyloid monoclonal antibody
- Lecanemab – Anti-amyloid antibody in clinical trials
- Donanemab – Targets specific forms of beta-amyloid
- Anti-inflammatory Approaches:
- Microglial modulators
- Targeted cytokine inhibitors
- Metabolic Approaches:
- Intranasal insulin
- Ketogenic supplements (medium-chain triglycerides)
Technology-Based Interventions
- Assistive Technologies:
- GPS tracking devices
- Medication management systems
- Smart home technologies
- Virtual assistants and reminder systems
- Digital Therapeutics:
- Virtual reality therapy
- Therapeutic games and apps
- Social robots and companions
- Telehealth Approaches:
- Remote monitoring
- Virtual cognitive assessment
- Caregiver support platforms
Nursing Management of Dementia
Nursing management of dementia is comprehensive and multifaceted, addressing cognitive, functional, behavioral, and psychosocial aspects of care. Nurses play a pivotal role in coordinating care, implementing interventions, educating caregivers, and advocating for patients across healthcare settings.
Common Nursing Diagnoses for Patients with Dementia
| Nursing Diagnosis | Related Factors | Key Nursing Interventions | Expected Outcomes |
|---|---|---|---|
| Chronic Confusion |
– Progressive cognitive impairment – Neurological changes – Sensory deprivation |
– Consistent environment with orientation cues – Simple, clear communication – Reality orientation as appropriate – Validation of feelings and perceptions |
– Demonstrates reduced anxiety in surroundings – Responds to reorientation – Maintains optimal cognitive function |
| Risk for Injury |
– Impaired judgment – Wandering behavior – Sensory-perceptual alterations – Impaired physical mobility |
– Environmental safety modifications – Regular safety assessments – Supervised mobility and transfers – Wandering precautions – Identification bracelets |
– Remains free from injury – Maintains safe environment – Returns to safe location if wandering occurs |
| Self-Care Deficit |
– Cognitive impairment – Executive function deficits – Apraxia – Memory loss |
– Establish consistent ADL routines – Break tasks into simple steps – Use visual cues and demonstration – Provide assistance as needed – Maintain dignity and privacy |
– Participates in self-care activities – Maintains highest level of independence – Experiences satisfaction with appearance |
| Disturbed Sleep Pattern |
– Circadian rhythm disturbances – Neurological changes – Environmental factors – Anxiety and agitation |
– Establish consistent sleep-wake schedule – Daytime activity and light exposure – Evening relaxation routines – Comfortable sleep environment – Limit caffeine and daytime napping |
– Increased hours of nighttime sleep – Reduced nocturnal awakenings – Decreased daytime sleepiness |
| Impaired Social Interaction |
– Communication difficulties – Altered behavior – Cognitive impairment – Social withdrawal |
– Facilitate appropriate social activities – Adapt communication techniques – Encourage family visits and involvement – Provide sensory-appropriate stimulation – Use reminiscence to promote interaction |
– Demonstrates interest in social activities – Engages in meaningful interactions – Shows positive affect during social contact |
| Caregiver Role Strain |
– Progressive care demands – Inadequate support systems – Insufficient knowledge – Prolonged caregiving |
– Assess caregiver stress and coping – Provide education on dementia care – Connect to community resources – Encourage respite care – Support groups referral |
– Caregiver verbalizes decreased stress – Utilizes appropriate resources – Demonstrates effective coping strategies |
Communication Strategies for Dementia Care
Verbal Communication Techniques
- Approach from the front, establish eye contact
- Introduce yourself and address patient by preferred name
- Speak slowly in a calm, low-pitched voice
- Use short, simple sentences and concrete terms
- Ask one question at a time, provide ample response time
- Avoid asking “Do you remember…?” questions
- Use yes/no questions when open-ended questions overwhelm
- Provide step-by-step instructions for tasks
- Avoid arguing or correcting misperceptions directly
- Validate feelings behind confused statements
Non-Verbal Communication Strategies
- Use gentle touch to gain attention (if culturally appropriate)
- Maintain a relaxed, open body posture
- Position yourself at eye level
- Use visual cues and demonstrations
- Pay attention to your facial expressions
- Model the behavior you want the patient to perform
- Use gestures to enhance verbal communication
- Reduce background distractions
- Maintain appropriate physical distance
- Be mindful of how your body language affects the patient
Managing Challenging Behaviors in Dementia
Behavioral and Psychological Symptoms of Dementia (BPSD) can be understood as expressions of unmet needs or responses to environmental triggers. Using a person-centered approach focused on understanding the meaning behind behaviors can lead to more effective interventions.
The DICE Approach to Behavioral Management
- D – Describe:
- Document specific behaviors
- Note time, location, people present
- Identify antecedents (triggers)
- Document consequences following behavior
- I – Investigate:
- Assess for physical causes (pain, infection, etc.)
- Evaluate medication effects
- Consider environmental factors
- Examine caregiver approach
- C – Create:
- Develop person-centered care plan
- Address underlying causes
- Modify environment as needed
- Train caregivers in approach
- E – Evaluate:
- Assess effectiveness of interventions
- Adjust plan as needed
- Document outcomes
- Continue successful strategies
Specific Behavioral Interventions
| Behavior | Potential Interventions |
|---|---|
| Wandering |
– Provide safe walking paths – Use identification bracelets – Disguise exits with visual barriers – Regular supervised walking – Consider GPS tracking devices |
| Agitation/Aggression |
– Identify and address triggers – Use distraction techniques – Create calm environment – Maintain consistent routines – Assess for pain or discomfort |
| Repetitive Questions/Actions |
– Respond with calm reassurance – Use memory aids (calendars, signs) – Distract with meaningful activities – Recognize anxiety underlying behavior |
| Sundowning |
– Maintain active mornings, quiet evenings – Reduce environmental stimulation – Avoid caffeine and sugar in evening – Use night lights to reduce shadows |
Environmental Adaptations for Dementia Care
Safety Considerations
- Secure medications and toxic substances
- Install grab bars in bathrooms
- Remove or secure trip hazards (rugs, cords)
- Install door alarms or monitoring systems
- Secure sharp objects and dangerous tools
- Use temperature regulators on faucets
- Install stove safety controls
- Provide adequate lighting, especially at night
Orientation Enhancement
- Large, visible clocks and calendars
- Clear signage with words and pictures
- Color-coding of rooms and important areas
- Memory boxes or photos on doors
- Consistent furniture arrangement
- Day/night lighting patterns
- Visual cues for daily routines
- Personal items and photos in living space
Stimulation Management
- Reduce unnecessary background noise
- Avoid overly complex patterns in decor
- Create quiet spaces for retreat
- Use contrasting colors for important objects
- Provide multisensory stimulation areas
- Create spaces for meaningful activities
- Consider acoustic management
- Balance stimulation to prevent under/over stimulation
Mnemonic: “CARE” for Dementia Nursing Management
C
Communication
- Clear, simple language
- Consistent approach
- Compassionate attitude
- Calm environment
A
Assessment
- Analyze behavior patterns
- Assess physical needs
- Address pain promptly
- Attentive to changes
R
Routine
- Regular schedule
- Reassuring environment
- Redirect when agitated
- Recognize personhood
E
Engagement
- Encourage participation
- Ensure safety
- Empower through choices
- Employ meaningful activities
Follow-up and Home Care Rehabilitation
As dementia is a progressive condition, ongoing follow-up, home care, and rehabilitation are essential components of comprehensive management. The primary goals are to support optimal functioning, enhance quality of life, maintain dignity, and provide appropriate support to both the individual with dementia and their caregivers.
Follow-up Care Considerations
Medical Follow-up
- Regular Assessment Schedule:
- Cognitive reassessment (every 6-12 months)
- Medication review and adjustment
- Monitoring for comorbidities
- Behavioral symptom evaluation
- Key Assessment Areas:
- Disease progression
- Medication efficacy and side effects
- Functional status
- Nutritional status and weight
- Behavioral and psychological symptoms
- Care Coordination:
- Communication between providers
- Electronic health record documentation
- Transitions of care management
Nursing Follow-up
- Community Nursing Support:
- Home health nursing visits
- Telehealth monitoring
- Nurse case management
- Specialized dementia care nurses
- Nursing Assessment Focus:
- Medication management
- Safety assessments
- Caregiver education and support
- Symptom management
- Care plan adjustments
- Documentation and Reporting:
- Changes in condition
- Response to interventions
- Updated care recommendations
Home Care Strategies for Dementia
Daily Care Routines
- Personal Hygiene:
- Establish consistent bathing routine
- Prepare environment before activities
- Provide step-by-step guidance
- Consider privacy and dignity
- Use adaptive equipment as needed
- Dressing:
- Simplify clothing choices
- Use adaptive clothing (Velcro, elastic)
- Lay out clothes in order of dressing
- Allow extra time
- Nutrition:
- Regular meal times
- Simple table settings
- Adaptive utensils when needed
- Monitor for swallowing difficulties
Medication Management
- Organization Systems:
- Pill organizers with time divisions
- Medication reminder alarms
- Electronic dispensing systems
- Color-coding systems
- Administration:
- Ensure proper timing and dosage
- Monitor for side effects
- Maintain medication list
- Consider alternative forms (liquid)
- Safety Measures:
- Secure storage of medications
- Prevent overdosing
- Regular medication reconciliation
- Dispose of unused medications
Activity Planning
- Meaningful Activities:
- Match to abilities and interests
- Use past occupations/hobbies
- Simple crafts and projects
- Music and memory activities
- Daily Structure:
- Balance activity and rest
- Include physical exercise
- Visual schedule/routine board
- Consistent timing for activities
- Engagement:
- Focus on process, not outcome
- Provide appropriate stimulation
- Use life story in activities
- Celebrate small successes
Rehabilitation Approaches in Dementia
While traditional rehabilitation may need adaptation for dementia, maintaining function and quality of life remain central goals. Rehabilitation in dementia focuses on optimizing remaining abilities, compensating for deficits, and supporting both the individual and their environment.
| Rehabilitation Domain | Approaches and Interventions | Nursing Role |
|---|---|---|
| Cognitive Rehabilitation |
– Spaced retrieval training – Errorless learning techniques – External memory aids – Reality orientation therapy – Cognitive stimulation therapy – Computerized cognitive training |
– Integrate cognitive techniques into daily care – Reinforce strategies used in therapy – Provide consistent cognitive stimulation – Monitor for frustration during activities – Document cognitive responses |
| Physical Rehabilitation |
– Gait and balance training – Strength and endurance exercises – Fall prevention programs – Mobility assistance devices – Transfer training – Tai Chi and adapted physical activities |
– Encourage daily physical activity – Ensure proper use of assistive devices – Monitor for pain during movement – Implement fall prevention strategies – Collaborate with physical therapy |
| Occupational Therapy |
– ADL training with adaptive techniques – Environmental modification – Assistive technology assessment – Energy conservation strategies – Purposeful activity program – Caregiver training |
– Maintain consistent use of adaptive equipment – Reinforce compensatory strategies – Support maximum independence in ADLs – Document functional abilities and changes – Educate caregivers on techniques |
| Speech-Language Therapy |
– Communication strategies – Alternative/augmentative communication – Swallowing assessment and interventions – Memory books and communication aids – Word retrieval exercises – Group communication therapy |
– Use recommended communication techniques – Implement swallowing precautions – Monitor for aspiration risk – Maintain communication tools and aids – Support social communication opportunities |
| Psychological Support |
– Validation therapy – Behavior management programs – Reminiscence therapy – Counseling for depression/anxiety – Support groups – Life review therapy |
– Recognize emotional needs – Provide consistent emotional support – Use empathic listening techniques – Monitor for depression or anxiety – Document behavioral responses to interventions |
Caregiver Support and Education
Caregiver Education Components
- Disease Education:
- Understanding dementia progression
- Recognizing symptoms and changes
- Medication management
- When to seek medical help
- Care Skills Training:
- Personal care techniques
- Managing difficult behaviors
- Communication strategies
- Safe transfer techniques
- Managing nutrition and hydration
- Safety Planning:
- Home safety assessments
- Wandering prevention
- Emergency response plans
- Driving safety considerations
Caregiver Support Strategies
- Self-Care Promotion:
- Respite care options
- Stress management techniques
- Setting realistic expectations
- Maintaining personal health
- Support Services:
- Support groups (in-person and online)
- Individual counseling
- Family therapy resources
- Community resources and agencies
- Long-term Planning:
- Advanced care planning
- Legal and financial considerations
- Long-term care options
- End-of-life care discussions
Signs of Caregiver Burnout
Nurses should be alert for signs of caregiver burnout, including:
- Social withdrawal
- Increased anxiety, irritability, or depression
- Exhaustion and sleep problems
- Neglect of personal health
- Increased alcohol or medication use
- Feelings of hopelessness or helplessness
Early intervention for caregiver burnout can prevent negative outcomes for both the caregiver and the person with dementia.
Palliative and End-of-Life Care Considerations
As dementia progresses to advanced stages, palliative care approaches become increasingly important to maintain comfort and dignity. Nursing care shifts to emphasize comfort, symptom management, and support for both the individual and family.
Advanced Dementia Care Priorities
- Physical Comfort:
- Pain assessment and management
- Skin integrity and pressure injury prevention
- Respiratory comfort measures
- Management of dysphagia
- Gentle positioning and touch
- Symptom Management:
- Agitation and restlessness
- Respiratory secretions
- Fever management
- Seizure prevention and management
- Psychosocial Support:
- Continued presence and companionship
- Sensory stimulation (music, gentle touch)
- Familiar religious/cultural practices
- Dignity-preserving care
End-of-Life Decision Making
- Advance Care Planning:
- Early discussions while capacity exists
- Documentation of wishes (advanced directives)
- Designation of healthcare proxy
- POLST/MOLST forms
- Treatment Decisions:
- Artificial nutrition and hydration
- Antibiotic use for infections
- Cardiopulmonary resuscitation preferences
- Hospitalization vs. home care
- Hospice Involvement:
- Criteria for hospice in dementia
- Benefits of hospice services
- Interdisciplinary team approach
- Bereavement support for families
